Abstract
This study addressed the effect of CPOE implementation on chest pain ordering patterns for patients in the emergency department. Retrospective order data was collected to assess the implementation. 300 randomly selected, time matched patients with a chief complaint of chest pain were selected in a before/after study. Patient demographics, treatment and disposition data were collected on clinical orders. Order volume, completeness and completion times were assessed before and after implementation. Overall order volume increased significantly from 11.6 pre-CPOE to 19.9 post-implementation (p<.01). Order documentation deficiencies were noted pre-implementation with 35.6% containing all order elements. Order completion times were unchanged; however, laboratory completion times increased for admitted patients post-implementation. Order volume increased after CPOE implementation, likely due to improved ED-based admission order capture for admitted patients. Order completeness improved significantly including standing order documentation. Overall, CPOE implementation is associated with improved clinical documentation with limited effect on clinical testing turn-around times.
Introduction
Computerized provider order entry (CPOE) provides a common starting point for initiating requests for clinical tests and treatments with potential to improve the safety and efficiency of patient care. CPOE has been associated with reducing clinical care errors, [1,2] decreasing medication errors and lowering medication costs [3,4,5]. CPOE can enhance clinical workflows, create efficiencies and decrease hospital length of stays by reducing redundant laboratory testing, enhancing adherence to clinical pathways and promoting order timeliness [6,7,8,9,10,11]. Although studies have demonstrated considerable benefits with implementing CPOE systems, some have raised questions about their impact on clinical errors, providing evidence that implementing CPOE systems may lead to unintended consequences [12,13,14]. CPOE implementation requires a multi-factorial approach that addresses provider resistance and work efficiency, and may necessitate changes in clinical workflows [15,16,17,18]. Healthcare institutions face many challenges when implementing CPOE and it is not surprising that the number of hospitals that have implemented CPOE systems remain moderate at an estimated implementation rate ranging between 8% and 15% [19,20].
The impact of CPOE systems has been examined in the outpatient and inpatient settings; however, implementing CPOE in the Emergency Department (ED) setting presents distinct challenges that have been evaluated infrequently [21]. The challenges within an ED setting include the mix of outpatient and inpatient care, the time sensitive nature of care delivery, national metrics for care quality, and the need to manage multiple patients simultaneously [22,23]. A previous evaluation of adherence to acute coronary syndrome guidelines in the ED did not show improvement after implementing a commercial CPOE system [24]. Given the rapid pace of diagnostic decisions and the need for triage capabilities, the efficiency of clinical workflow and the impact on patient care is an important aspect. In the ED, implementing CPOE reduced the need to clarify orders, and laboratory turn-around times decreased when CPOE was combined with the implementation of a pneumatic tube system [25,26]. However, prior time study data from this CPOE implementation had indicated that the effect of computerized order entry was to increase the time commitments by clinical providers based on workflow analysis and time study data [30]. In the intensive care setting, a similar time critical environment, the timeliness of stat orders improved after CPOE implementation [27].
Given the limited experience with implementing CPOE in the ED setting, there is a need to assess the impact of CPOE on patient care and operational processes. This study assessed the impact of implementing a CPOE system on order volumes, order completeness, and the clinical laboratory and diagnostic exam turn-around times among ED patients who presented with a chief complaint of chest pain.
Methods
Study design:
This was a retrospective cohort study before and after implementing a CPOE system in the ED. The study was reviewed and approved by local Institutional Review Board.
Study Setting and Population:
The adult ED of Vanderbilt University Medical Center is an urban, academic, level 1 trauma center with an annual volume of >50,000 patients. In March 23, 2004 the ED implemented an in-house developed, inpatient CPOE system (WizOrder), which was adapted to the requirements of the ED setting [28]. The CPOE system is currently distributed as Horizon Expert Order (McKesson®). The ED was already using information technology applications for patient care, including a longitudinal electronic medical record and an electronic patient tracking system [29]. A computerized ED order tracking application was developed and implemented with the CPOE system. The order tracking application supports the ED staff in managing all ED orders electronically. Prior to CPOE implementation, orders were processed using traditional paper order forms. The post-CPOE workflow requires physicians to enter orders into the CPOE system, while other supporting personnel have the ability to enter verbal orders. Through the patient tracking application a provider gains access to the CPOE system where order entry screens group order sets together according to the presenting complaints of the patient providing typical ED diagnostic and treatment order options.
Patients were eligible to be included if the presenting chief complaint was “chest pain” as identified with an ICD-9 coded chief complaint in the patient tracking board. As part of the patient triage process, the nurse selects an ICD-9 coded chief complaint from a list of about 140 different chief complaints in the patient tracking board. During a 4-month study period (September 1, 2003 to December 31, 2003) before CPOE implementation we randomly selected 150 patients among all 931 eligible patients with chest pain. During a 4-month study after CPOE implementation period (September 1, 2004 to December 31, 2004) we randomly selected 150 patients among all 965 eligible patients with chest pain.
Study Protocol:
We obtained patient and order information from multiple sources including the electronic ED patient tracking system, the CPOE system, paper charts, and electronic medical records. The electronic data was validated with database table cross-checks across the available sources to insure data reliability with validation of patient identifiers and dates of service. All orders placed in the ED, paper and electronic were recorded and categorized by service area including radiological orders, lab tests, respiratory, nursing care, pharmacy and other orders. Specific elements were assessed including time stamps, the orders written and the presence of a provider signature. Cardiac testing was considered as a service area and included electrocardiograms, treadmill studies, echocardiograms, stress echocardiograms and Holter monitors. To make the results comparable between pre- and post-CPOE period decomposing laboratory panel orders into core elements was necessary. For example, the order of a single coagulation laboratory panel, which included three individual tests, was decomposed into three separate laboratory orders in both phases to assure that order volumes were comparable in both phases. Laboratory and diagnostic exam turn-around times for the this study reflected the time interval between the patient arrival time in the ED (registration time) and the time when the results (for laboratory exams) or the diagnostic exam findings (for imaging studies and ECG) were available to the clinicians in the electronic systems during both the pre-and post-CPOE implementation. For each of the 150 patients in the pre- and post-implementation phases turn-around time information was obtained from reviewing the longitudinal electronic medical record for the laboratory, cardiac and radiological exam data completed during each patient’s ED visit and data were abstracted into a Microsoft® Access database.
An internal medicine trained resident physician (PGY-3) systematically reviewed and abstracted data from the paper charts of the 150 pre-implementation patients. The independent reviewer was not affiliated with the ED clinical practice at the study site, the ED providers, or the CPOE development and implementation team. The chart review used a standard process of identifying orders from the paper-based order sheets during the pre-CPOE period, identified each discernable written order, and assessed the completeness of orders, including the order description, timestamp and signature. All three order elements were required for the order documentation to be considered complete. Other elements of the paper chart were reviewed for supporting documentation of clinical orders including nursing notes, medication administration records and disposition. During the post-CPOE period the review of orders relied on electronic queries of the CPOE system.
Measures:
Chest pain patient specific outcome data were collected including a) order volumes; b) order placement completeness, i.e., presence of order description, time stamp, and provider signature; and c) the order turn-around times which measured the differences between patient ED registration to the time to when the result of an order was available for provider interpretation which was assessed from the electronic medical record time stamp which was operational in the ED in both phases of the study.
Order Volume:
Order volume data were obtained in the pre-implementation phase by completing paper chart reviews to evaluate the order type, departmental origin and order quantity. Order volume subset analysis was also completed for the patients admitted to the hospital and for the patients treated and discharged from the ED using the same chart abstraction process. Patients who were admitted to the hospital but were boarded in the ED because of lack of hospital bed availability continued to accrue orders designated as “ED” orders since they remained in the care of the ED both pre- and post-implementation. Post-implementation order data were obtained from a CPOE order database to assess order type, department origin and order quantity. The total number of reported laboratory results and diagnostic exams for each patient were also assessed for typical high frequency chest pain diagnostic tests including chest x-rays, electrocardiograms, complete blood counts, basic metabolic panels and cardiac enzymes using an electronic medical record review in both phases. Department origin order data were also assessed in both phases to better describe the types of orders present in each phase.
Order Placement:
Order placement completeness was assessed by reviewing the paper and electronic charts for the presence of required order descriptors, order time, and signatures. Orders lacking any of the required elements were considered incomplete and the presence or absence of all of the 3 core components was abstracted; however, even if orders only had an order descriptor they were included in the order volume total. In addition, each ED based laboratory, cardiac and radiological test result was compiled for every patient from the electronic patient record and assessed for the presence of a corresponding order to assess for missing order documentation in both phases of the study.
Laboratory and Diagnostic Turn-Around Times:
The turn-around times for cardiac, radiological and laboratory assessments were assessed for orders based on the time stamp data (as represented in the electronic medical record) including chest x-rays, electrocardiograms, complete blood counts, basic metabolic panels and cardiac enzymes. In both study periods the turn-around time for results and exam availability was defined as the difference between the patient’s registration time and the result availability time, i.e., when the result was available to the providers in the electronic medical record. The average time between ED registration and result or exam availability time were calculated for all patients, and separately for patients who were hospitalized and patients who were discharged home from the ED.
ED Length of Stay:
In addition to the order data, the ED length of stay was assessed in a multivariate regression analysis to assess for potential confounders in addition to CPOE that may have affected patient length of stay. Key variables included age, gender, acuity (Emergency Severity Index), inpatient admission status, ED consultation, weekend and afterhours variables.
Data Analysis:
Data analyses included descriptive statistics, Student t-test, Fisher’s exact test and Wilcoxon signed rank were completed where appropriate using JMP version 7 software. 95% confidence intervals, median values and inter-quartile ranges were obtained. Normality testing was completed to assess the distributions of the variables. Linear regression analysis included independent variable interaction terms and a log transformation of the dependent variable. A p-value < 0.05 was considered statistically significant.
Results
Patient demographics are summarized in table I. The demographic characteristics of the pre- and post-CPOE patient cohorts did not differ statistically, except for the length of stay for patients who were treated and released from the ED. The patients who were treated and released had a longer length of stay before CPOE implementation (6.6 hours versus 5.0 hours; p=0.01). For patients admitted to the hospital, the length of stay before implementation was 7.8 hours and 6.4 hours after implementation (p=0.45). For the patients admitted to the hospital, the patient boarding times (time from hospital admission time to actual ED discharge time) was averaged 3.3 hours before versus 2.6 hours after CPOE implementation (p = 0.62).
Table I:
Patient Demographic Characteristics
| Study Group | Pre-CPOE (N=150) | Post-CPOE (N=150) | p-value |
|---|---|---|---|
| Age, years | 48.1 (45.5–50.8) | 46.9 (44.2–49.5) | 0.44 |
| Female gender (%) | 54.0 | 55.3 | 0.45 |
| Length of stay (hours) | 7.1 (3.5–8.6) | 5.5 (3.2–6.7) | 0.01 |
| Consult (%) | 24.0 | 22.0 | 0.68 |
| Admitted (%) | 43.3 | 36.7 | 0.24 |
The patient length of stay was assessed in a multivariate regression analysis using a log transformed length of stay with the results noted in Table II. Several statistically significant results were associated with length of stay and reflected a percentage change in the length of stay due to the log transformed dependent variable reflected in the coefficient terms. Longer lengths of stay were associated with cardiac enzyme orders (+32%), inpatients admission (boarding) (+84%), and patients with an ESI (Emergency Severity Index) acuity level of 2 (+40%). Shorter lengths of stay were associated with CPOE (−15%) and the interaction between patient age and inpatient status (−1%). Age, patient ESI acuity level 1 and 3, female gender, consult status, weekend and after hours ED admissions were not statistically significant in the regression model with an overall R-squared: 0.20.
Table II:
Multivariate Regression of Log Length of Stay
| Source | DF | Sum of Squares | Mean Square | F Ratio |
| Model | 12 | 25.28314 | 2.10693 | 5.6818 |
| Error | 275 | 101.97545 | 0.37082 | Prob > F |
| C. Total | 287 | 127.25859 | <.0001 | |
| Term | Coefficient | t Ratio | Prob>|t| | |
| Intercept | 0.7257553 | 3.58 | 0.0004 | |
| Age | 0.0057802 | 1.52 | 0.1288 | |
| Cardiac enzymes | 0.3208774 | 2.69 | 0.0076 | |
| Inpatient | 0.8360759 | 3.08 | 0.0023 | |
| Age*Inpatient | −0.014991 | −2.92 | 0.0038 | |
| CPOE | −0.153692 | −2.08 | 0.0382 | |
| ACUITY[1] | −0.365331 | −1.48 | 0.1392 | |
| ACUITY[2] | 0.3954799 | 2.83 | 0.0049 | |
| ACUITY[3] | 0.2489901 | 1.61 | 0.1094 | |
| Female gender | 0.133984 | 1.78 | 0.0760 | |
| Consult | 0.160915 | 1.75 | 0.0805 | |
| Weekend | 0.0008133 | 0.01 | 0.9928 | |
| AfterHours | 0.0287627 | 0.37 | 0.7109 | |
| RSquare | 0.198675 | F Ratio | 5.6818 | |
| RSquare Adj | 0.163708 | |||
| Observations | 288 | Prob > F | <.0001 | |
Order volume:
Order volume assessment demonstrated a substantial increase in the number of documented orders placed after CPOE implementation. The average number of documented orders per patient increased significantly after CPOE implementation with an average of 11.6 (95% CI: 9.0–13.1) orders per patient in the pre-CPOE phase and 19.9 (17.9–22.0) orders per patient in the post-CPOE phase (p < 0.01). For hospital admitted patients the pre-CPOE average order volume was 14.0 (12.7–15.2) as compared with 33.9 (28.6–39.1) orders post-CPOE (p<0.01). For patients treated and released from the ED the average order volume was 8.8 (7.7–10.0) orders pre-CPOE and 11.9 (10.5–13.3) orders post-CPOE (p<0.01).
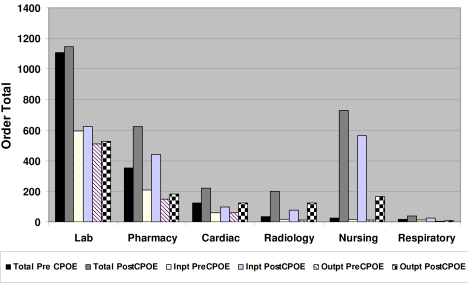
The composition of the aggregate order data is further clarified in Figure 1. Laboratory data were the largest component of the aggregate order volume followed by pharmacy, cardiac testing and radiology, nursing and respiratory prior to CPOE implementation (Pre CPOE in Figure). After implementation (Post CPOE in Figure) the numbers of all documented order types increased with the largest percentage increase for nursing (2700%), radiology (519%), respiratory (106%), cardiology (80%) and pharmacy (76%). Figure 1 displays the results from the subgroup analysis of patients who were admitted to the hospital and for those treated and released from the ED. The results are similar for both the admitted patients and the treat and release patients. However, the admitted patients appeared to have a proportionally larger increase in nursing orders and pharmacy orders after CPOE versus the treat and release patients
Figure One:
Order Totals by Service Department
The documented cardiac ED diagnostic test orders for chest pain patient were similar except for electrocardiograms and chest x-rays. For the laboratory tests the total tests completed before and after CPOE were similar: complete blood counts (112 before, 116 after), basic metabolic panels (120 before, 113 after) and cardiac enzymes (144 before, 147 after). There was an increase in the number of documented orders for both electrocardiograms (105 before, 204 after) and chest x-rays (18 before, 135 after) with CPOE implementation. The low relative number of documented ECGs and chest x-ray orders may reflect standing orders, which were not documented in the ED paper order sheet. In the case of chest x-rays, 18 orders were placed and 132 chest x-ray exams were completed pre-CPOE. With electrocardiograms, 105 orders were placed and 194 were available pre-CPOE. The differences between placed orders and availability of results or exams are most likely due to standing orders for chest pain patients. The ECG and chest x-rays represents 203 of the 261 orders identified but not documented on the ED chart pre-CPOE.
Order placement completeness:
Order placement completeness assessed each order for the presence of an order descriptor, order time-stamp and provider signature. The assessment of order placement completeness noted significant paper chart order deficiencies. Of completed ED orders identified, 84.6% had a discernable documented written order in the paper chart (15.4% without any order documentation) which likely reflected the lack of documentation of standing orders in the paper chart for chest x-rays and electrocardiograms. The evaluation of order placement completeness noted that only 35.6% of pre-CPOE paper orders contained all order elements (order time, order date and signature completion) in the paper record. The majority of the missing data elements were the time stamp with only 36.1% of orders having a time stamp present. In the post-CPOE phase all orders reviewed contained all elements since the data are automatically collected with the computerized CPOE process.
Laboratory and Diagnostic Exam Turn-Around Times:
Time studies for laboratory results, radiology exams and ECG turn-around times were completed for several typical ED chest pain diagnostic studies with the median times noted in Table III for the key cardiac tests. No statistically significant differences were noted with CPOE implementation for the laboratory and diagnostic exam turn-around times in the overall evaluation or the hospital admission and treat-and-release patients.
Table III:
Laboratory and Diagnostic Test Turn-Around Times
| Clinical Study1 | Overall Results (Interquartile Range) | Hospital admitted patients (Interquartile Range) | Treat-and-release patients (Interquartile Range) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-CPOE (N=150) | Post-CPOE (N=150) | p-value | Pre-CPOE (N=65) | Post-CPOE (N=55) | p-value | Pre-CPOE (N=85) | Post-CPOE (N=95) | p-value | |
| CBC | 51 (33–75) | 56 (40–89) | 0.22 | 48 (30–69) | 56 (40–95) | 0.10 | 63 (38–89) | 59 (40–86) | 0.74 |
| EKG | 27 (19–39) | 29 (18–41) | 0.43 | 24 (16–34) | 26 (16–37) | 0.89 | 30 (20–51) | 32 (19–55) | 0.52 |
| CXray | 55 (34–89) | 59 (37–89) | 0.57 | 44 (25–80) | 50 (32–75) | 0.54 | 63 (45–100) | 64 (40–94) | 0.83 |
| BMP | 53 (35–75) | 55 (39–85) | 0.62 | 48 (30–69) | 55 (40–88) | 0.17 | 62 (44–89) | 54 (38–83) | 0.34 |
| C Enz | 52 (33–75) | 55 (40–87) | 0.37 | 47 (29–68) | 55 (40–88) | 0.07 | 63 (44–89) | 55 (39–85) | 0.48 |
CBC=Complete Blood Count EKG=Electrocardiogram CXray=Chest Xray BMP=Basic Metabolic Panel, C Enz=Cardiac Enzymes
Discussion
The implementation of CPOE in the ED setting provided substantial changes by increasing documented order volumes and improving order placement completeness with no overall effect on laboratory and diagnostic exam turn-around times. The increase volume of documented orders provided better documentation of care delivered in the ED since more order data was captured after CPOE implementation. Specific order placement components improved with CPOE implementation including an increased collection of dates and times of order writing and enhanced documentation of standing orders. CPOE consistently produced a time stamp and electronic audit trail that were often incomplete in the paper record. Laboratory and diagnostic exam turn-around times remained unchanged suggesting a limited effect of CPOE on clinical order processing times of ED-based orders. The overall ED length of stay was lower after implementation; however, there are several potential confounders in the workflow changes during CPOE implementation, including diversion status and ED census data, which were unavailable with the retrospective chart review and may potentially account for the observed reduction in length of stay.
The increase in documented order volume has not been previously noted with implementation of CPOE in the ED setting. The order volumes were significantly increased in both admitted and treat-and-release patients, but the magnitude of order expansion was larger in the subset of admitted patients. The order types with the largest increases in documented order volumes were nursing, radiology, pharmacy and cardiac testing. Nursing order volumes likely increased due to improvements in order documentation and in the care transition from the ED to the hospital. The documentation of previous standing orders, particularly with radiology (chest x-rays) and cardiac testing (electrocardiograms), may explain why some of the order volume increased but did not provide a clear explanation for the near doubling of overall order volumes. For the boarding patients in the ED, CPOE potentially improved continuity of care through the availability of pre-admission orders that were entered from the receiving teams during the ED encounter which was unavailable prior to CPOE implementation.
Some of the increase in documented order volume post-CPOE may be explained by inpatient admission care being recorded in the ED setting and reflecting better information on where patient care resources are physically being delivered. In the pre-CPOE setting, inpatient clinical orders were written and recorded in the patient’s hospital admission order set and the hospital admission orders were activated at the time of patient arrival in the hospital. The actual care provided to these transitional patients may have included some inpatient care interventions provided in the ED but actually recorded in the inpatient order record. As a result, the increased overall order volume after CPOE implementation is likely partially explained by the presence of previously designated inpatient care orders being documented as ED care after CPOE implementation, particularly for patients in transition from the ED to the hospital. However, for the treat-and-release patients who were not affected by dual inpatient and outpatient order entry documentation, there was still a significant increase in documented orders.
Order placement documentation quality with CPOE provided a more complete picture of order timing that was not always available in the pre-implementation paper record. The inclusion of time stamps and ordering provider information was always available after implementation due to the automated data collection with CPOE. The improvement in order placement completeness has potential operational implications. The ability to obtain accurate and complete order data in the post-implementation setting provides the potential for better workflow timing analysis which was much more difficult prior to CPOE due to inconsistent time stamp data. In addition, improved order placement information may be helpful to collect accurate care quality metric data.
With CPOE implementation, improved documentation occurred without an impact on laboratory and diagnostic exam turn-around times. Previous published results have shown improved timeliness of orders with the use of CPOE when utilized in conjunction with a pneumatic tube system [26] and when implemented for treating stroke patients in the ED setting [11] and for pathology turn-around times [32]. CPOE has also been shown to improve the timeliness of “stat” laboratory and imaging studies in the time critical ICU setting [27]. The lack of improvement in completion times with CPOE implementation may have been affected by increased patient laboratory testing volumes or by the increased time for computer login with each patient. Laboratory volumes may impact the completion times, however these data were not directly available. There was an increase in chest pain patients by 3.7% post-CPOE (931 pre-CPOE compared to 965 post-CPOE), but the effect of the increase would likely be limited. In addition, the time for workstation log-in and subsequent order entry can potentially contribute to longer completion times when compared to paper forms and has been noted on a prior analysis of the ED implementation which indicated an increased workload for providers post-CPOE [30]. If workstation log-in times were to be the primary cause of diagnostic delay, then the standing order testing should be the most affected by CPOE implementation; however, the turn-around times for completion of the chest x-rays and electrocardiograms were not significantly affected.
CPOE implementation was associated with an overall reduction in the length of stay for this cohort of chest pain patients. Hwang et al. found a reduced inpatient length of stay with the use of CPOE [9]. Although a reduction in the ED length of stay was noted in this study, the overall hospital length of stay was not evaluated for those admitted to the hospital. The expected effect of CPOE on length of stay is mixed. The need for computer login and entry has the potential to increase the time for order placement, however, CPOE also has the potential to reduce order fulfillment times by streamlining order sets, allowing the combination of common order elements on a single page in a context sensitive fashion, and directing orders to the appropriate services, such as radiology exam requests.
With expanded use of CPOE there may be additional efficiencies realized with triage workflows, diagnostic choices and treatment selections which could help optimize clinical care. In patients with chest pain, time critical decision making depends on the rapid availability of diagnostic information and treatment modalities as in the patients with needs for cardiac intervention. In this subset of chest pain patients, it is important to optimize door-to-catheterization laboratory time for patients for clinical care as well as for quality assessment and adherence to treatment guidelines [23]. Previous work by Asaro et al., which evaluated the effect of CPOE on a local acute coronary syndrome guideline and order set utilization with a mixed paper and CPOE implementation process, showed no improvements in guideline adherence, but was associated with increased order set usage [24]. This study computerized the order entry process, leading to full order set use since it became the only way to input orders after implementation and avoided the potential challenges of a dual paper-electronic ordering process.
Beyond the effects on order processing efficiency, there are several other potential benefits to CPOE use in the ED. Prior to implementation, patients in the ED had inpatient orders (in the inpatient CPOE system) queued but not activated until they were admitted to the hospital which limited the ability to start inpatient order processing. By having the ED using the same order entry system as the hospital, inpatient care delivery can more easily start prior to the patient’s transfer to the inpatient unit assuring continuity of care from a CPOE perspective. The allied health providers and clerical staff spend less time reading, confirming and processing handwritten orders, providing the potential for cost savings by labor reduction [30]. The improvements in documentation provides the potential to better measure exact timing of clinical ordering decisions which can provide enhanced data for quality initiatives. In addition, CPOE systems may help reduce the risk missing test results which could potentially improve patient safety [31].
Limitations:
The study had several limitations including the involvement of a single center, the focus of the patient population (chest pain) and potential for documentation bias. The single center retrospective design could be improved with the use of a prospective analysis at multiple institutions; however, the evaluation of CPOE is generally challenging since each clinical setting is distinct as is the technology implementation in that setting. In addition, each CPOE implementation is also unique given the differences in information systems, organizational structures and technologic capabilities. The implementation in this study took place at a facility with existing electronic medical records and electronic tracking systems in the ED, which limits the ability to generalize these results to other sites. A reduced ED length of stay was observed after implementation; however, there are a number of other potential organizational changes that occurred with CPOE implementation that are difficult to adjust for and may contribute to the improvements in length of stay, such as workflow assessment and standardization that occur with CPOE assessment and implementation. In addition, since the study was retrospective there were limits on the ability to obtain important data on patient occupancy, diversion status and staffing since they were not available in both phases of the study resulting in limited ability to control for pertinent factors associated with length of stay.
Chest pain was selected since it was a prototypical patient population which requires time sensitive evaluation due to risk of cardiac complications and sudden death in the ED setting. However, outside the typical diagnostic tests provided to most chest pain patients where the results are clearly documented in the electronic medical record in both study phases, the ability to differentiate actual care delivered versus the documented orders provided is somewhat difficult to differentiate. It may be possible that patients received exactly the same nursing care before and after implementation, yet the lack of order placement documentation in the pre-CPOE phase limits the ability to accurately assess the actual care provided. Further evaluation of other specific types of patients or a broader and generalized survey of patients could provide additional insight of the effect of CPOE. The effect of documentation bias is also a potential concern given the retrospective chart review design of the study. In addition, the data were abstracted systematically by a single chart reviewer and was not assessed for inter-rater reliability which provides some potential for bias. Though no differences were found in turn-around times for lab results and diagnostic exams, the times were an indirect measure which relied on the patient registration time, since many pre-CPOE orders lacked needed time stamps to assess more direct measures of order placement times.
Conclusions
The implementation of CPOE in the ED setting was able to provide better documentation of the orders that were placed. Compared to paper records the documentation of order placement was improved with CPOE, the ED length of stay was reduced, and the impact on laboratory and diagnostic turn-around times was unchanged. The increase in documented orders after implementation including previously uncharted standing orders and inpatient care provided in the ED. The use of CPOE allowed better documentation of inpatient orders executed in the ED. The overall order numbers were increased significantly by accurately documenting ED clinical activities. Given the improvements in order capture and increased timing data provided by CPOE, the implementation of quality assurance and quality improvement programs are likely more feasible with CPOE. In this study, CPOE implementation seems to have provided potential benefits without delays on the turn-around times of results or exams, and a possible reduction in ED length of stay.
Bibliography
- 1.Institute of Medicine To err is human: building a safer health system. Washington: National Academy Press; 1999. [Google Scholar]
- 2.To err is human: building a safer health system. Washington: National Academy Press; 2000. [PubMed] [Google Scholar]
- 3.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. Jama. 1998 Oct 21;280(15):1311–1316. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 4.Overhage JM, Tierney WM, Zhou XH, McDonald CJ. A randomized trial of “corollary orders” to prevent errors of omission. J Am Med Inform Assoc. 1997 Sep-Oct;4(5):364–375. doi: 10.1136/jamia.1997.0040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma’Luf N, Boyle D, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999 Jul-Aug;6(4):313–321. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bates DW, Kuperman GJ, Rittenberg E, Teich JM, Fiskio J, Ma’luf N, Onderdonk A, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med. 1999 Feb;106(2):144–150. doi: 10.1016/s0002-9343(98)00410-0. [DOI] [PubMed] [Google Scholar]
- 7.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000 Oct 9;160(18):2741–2747. doi: 10.1001/archinte.160.18.2741. [DOI] [PubMed] [Google Scholar]
- 8.Teich JM, Glaser JP, Beckley RF, Aranow M, Bates DW, Kuperman GJ, Ward ME, et al. The Brigham integrated computing system (BICS): advanced clinical systems in an academic hospital environment. Int J Med Inform. 1999 Jun;54(3):197–208. doi: 10.1016/s1386-5056(99)00007-6. [DOI] [PubMed] [Google Scholar]
- 9.Hwang JI, Park HA, Bakken S. Impact of a physician’s order entry (POE) system on physicians’ ordering patterns and patient length of stay. Int J Med Inform. 2002 Nov 12;65(3):213–223. doi: 10.1016/s1386-5056(02)00044-8. [DOI] [PubMed] [Google Scholar]
- 10.Kaushal R, Jha AK, Franz C, Glaser J, Shetty KD, Jaggi T, Middleton B, et al. Return on investment for a computerized physician order entry system. J Am Med Inform Assoc. 2006 May-Jun;13(3):261–266. doi: 10.1197/jamia.M1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nam HS, Han SW, Ahn SH, Lee JY, Choi HY, Park IC, Heo JH. Improved time intervals by implementation of computerized physician order entry-based stroke team approach. Cerebrovasc Dis. 2007;23(4):289–293. doi: 10.1159/000098329. [DOI] [PubMed] [Google Scholar]
- 12.Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of computerized physician order entry systems in facilitating medication errors. Jama. 2005 Mar 9;293(10):1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 13.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of Unintended Consequences Related to Computerized Provider Order Entry. J Am Med Inform Assoc. 2006 Jun;13(5):547–56. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han YY, Carcillo JA, Venkataraman ST, Clark RS, Watson RS, Nguyen TC, Bayir H, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005 Dec;116(6):1506–1512. doi: 10.1542/peds.2005-1287. [DOI] [PubMed] [Google Scholar]
- 15.Langberg ML. Challenges to implementing CPOE: a case study of a work in progress at Cedars-Sinai. (CPOE).(computerized physician order entry system) Modern Physician. 2003;7(2):S21. (22). [Google Scholar]
- 16.Wright MJ, Frey K, Scherer J, Hilton D. Maintaining excellence in physician nurse communication with CPOE: A nursing informatics team approach. J Healthc Inf Manag. 2006 Spring;20(2):65–70. [PubMed] [Google Scholar]
- 17.Murff HJ, Kannry J. Physician satisfaction with two order entry systems. J Am Med Inform Assoc. 2001 Sep-Oct;8(5):499–509. doi: 10.1136/jamia.2001.0080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee F, Teich JM, Spurr CD, Bates DW. Implementation of physician order entry: user satisfaction and self-reported usage patterns. J Am Med Inform Assoc. 1996 Jan-Feb;3(1):42–55. doi: 10.1136/jamia.1996.96342648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Usage of CPOE steadily increasing, leapfrog says. Healthcare Benchmarks Qual Improv. 2006 Mar;13(3):33–34. [PubMed] [Google Scholar]
- 20.Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized physician order entry in U.S. hospitals: results of a 2002 survey. J Am Med Inform Assoc. 2004 Mar-Apr;11(2):95–99. doi: 10.1197/jamia.M1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Handler JA, Feied CF, Coonan K, Vozenilek J, Gillam M, Peacock PR, Jr, Sinert R, et al. Computerized physician order entry and online decision support. Acad Emerg Med. 2004 Nov;11(11):1135–1141. doi: 10.1197/j.aem.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto LG, Khan AN. Challenges of electronic medical record implementation in the emergency department. Pediatr Emerg Care. 2006 Mar;22(3):184–191. doi: 10.1097/01.pec.0000203821.02045.69. quiz 192. [DOI] [PubMed] [Google Scholar]
- 23.Pham JC, Kelen GD, Pronovost PJ. National study on the quality of emergency department care in the treatment of acute myocardial infarction and pneumonia. Acad Emerg Med. 2007 Oct;14(10):856–863. doi: 10.1197/j.aem.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 24.Asaro PV, Sheldahl AL, Char DM. Embedded guideline information without patient specificity in a commercial emergency department computerized order-entry system. Acad Emerg Med. 2006 Apr;13(4):452–458. doi: 10.1197/j.aem.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 25.Banet GA, Jeffe DB, Williams JA, Asaro PV. Effects of implementing computerized practitioner order entry and nursing documentation on nursing workflow in an emergency department. J Healthc Inf Manag. 2006 Spring;20(2):45–54. [PubMed] [Google Scholar]
- 26.Guss DA, Chan TC, Killeen JP. The impact of a pneumatic tube and computerized physician order management on laboratory turnaround time. Ann Emerg Med. 2008 Feb;51(2):181–185. doi: 10.1016/j.annemergmed.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Thompson W, Dodek PM, Norena M, Dodek J. Computerized physician order entry of diagnostic tests in an intensive care unit is associated with improved timeliness of service. Crit Care Med. 2004 Jun;32(6):1306–1309. doi: 10.1097/01.ccm.0000127783.47103.8d. [DOI] [PubMed] [Google Scholar]
- 28.Miller RA, Waitman LR, Chen S, Rosenbloom ST. The anatomy of decision support during inpatient care provider order entry (CPOE): empirical observations from a decade of CPOE experience at Vanderbilt. J Biomed Inform. 2005 Dec;38(6):469–485. doi: 10.1016/j.jbi.2005.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aronsky D, Jones I, Lanaghan K, Slovis CM. Supporting patient care in the emergency department with a computerized whiteboard system. J Am Med Inform Assoc. 2008 Mar-Apr;15(2):184–194. doi: 10.1197/jamia.M2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piasecki JK, Calhoun E, Engelberg J, Rice W, Dilts D, Belser D, Aronsky D, et al. Computerized provider order entry in the emergency department: pilot evaluation of a return on investment analysis instrument. AMIA Annu Symp Proc; 2005. p. 1081. [PMC free article] [PubMed] [Google Scholar]
- 31.Callen JL, Paoloni R, Georgiou A, Prgomet M, Westbrook J. The rate of missed test results in an Emergency Department. An evaluation using an electronic test ordering and viewing system. Methods of Information in Medicine. 2010;1:37–43. doi: 10.3414/ME09-01-0011. 49. [DOI] [PubMed] [Google Scholar]
- 32.Westbrook JI, Georgiou A, Rob MI. Test turnaround times and mortality rates 12 and 24 months after the introduction of a computerised provider order entry system. Methods of Information in Medicine. 2009;48(2):211–215. doi: 10.3414/ME9219. [DOI] [PubMed] [Google Scholar]