Abstract
Cancer patients often need to manage care-related information when they are away from home, when they are experiencing pain or treatment side effects, or when their abilities to deal with information effectively are otherwise impaired. In this paper, we describe the results from a four-week evaluation of HealthWeaver Mobile, a mobile phone application that we developed to support such “unanchored” patient information activities. Based on experiences from nine cancer patients, our results indicate that HealthWeaver Mobile can help patients to access care-related information from anywhere, to capture information whenever a need arises, and to share information with clinicians during clinic visits. The enhanced ability to manage information, in turn, helps patients to manage their care and to feel more confident in their ability to stay in control of their information and their health.
Background
Health information technology plays an important role in helping cancer patients to become active participants in their care. Self-management systems, such as CHESS1 and WebChoice2, provide patients with effective tools for tracking their symptoms, engaging in self-care, and finding high quality information. For example, CHESS, an early self-management system originally focused on breast cancer, enables patients to communicate with other patients and health professionals, to get vetted answers to questions about their illness, and to clarify their priorities and create treatment and self-care action plans. WebChoice, a more recent self-management system for cancer, provides symptom assessment tools with self-management advice tailored to reported problems, links to reliable online health resources, and forums in which patients can interact with other patients and have their questions answered by nurses. Such self-management tools can positively impact patient care. For example, an RCT that examined the use of CHESS by breast cancer patients3 found that the intervention group had significantly higher information competence, involvement in care, and levels of social support.
Personal health records (PHRs)4,5 and patient portals6 enable patients to store, view, and share their lab results, medical histories, allergies, and prescriptions, which helps patients to track their health information and to communicate with their healthcare providers. In many health domains such systems have been found to have significant benefits for patients. A review of studies of patient portals in diabetes care7, for instance, found that the use of patient portals improved physician-patient communication and satisfaction with care and enhanced disease management and health outcomes. Similarly, Detmer and colleagues6 have argued that integrated PHRs can increase the availability of care-relevant information and free the appointment time typically spent on routine data collection for addressing patients’ problems, concerns, and treatment priorities. While the evidence for the effectiveness of PHRs in cancer care is equivocal, a recent review found that cancer patients are largely positive about PHRs.8
Although PHRs and self-management tools can be effective for improving patient care and engagement, they are typically complex, web-based systems that are intended to be used when patients have sufficient time and attention to devote to health information management. However, cancer patients often need to deal with information for their care when they are away from home, are in pain or are experiencing other treatment side effects, and when their abilities to manage information effectively are otherwise impaired. In our previous work we found that such “unanchored information work”9 is a critical aspect of what cancer patients do to manage their treatment. For example, to avoid a long phone tag with the clinic, patients often need to take phone calls and schedule care while they are away from home. Similarly, to make sure their concerns are addressed during important but infrequent appointments with their oncologists, patients need to keep track of their questions—often over several weeks—writing them down when they first think of them and collecting and triaging the notes before and after the appointment. Although traditional PHRs and self-management systems provide valuable help when patients can sit down at their computers, these systems are not designed to support such important unanchored patient work.
Existing mobile applications for cancer patients do not fully address patients’ unanchored needs either. Systems such as WHOMS10 and ASyMS11 enable patients to track symptoms and quality of life and report them to their clinical teams and, in the case of ASyMS, to instantly receive tailored self-care advice for managing chemotherapy side effects. However, these systems do not support many other common unanchored activities that cancer patients do, such as keeping track of questions and accessing an up-to-date medication list. Although patients sometimes appropriate general purpose applications on their mobile phones—such as notes and audio recording—to deal with these other aspects of unanchored work such strategies often lead to fragmentation of patients’ information.9
To support unanchored patient work, we have developed a smartphone application called HealthWeaver Mobile,12 which runs on the Android operating system. HealthWeaver Mobile tightly integrates with HealthWeaver, our web-based system for helping patients to manage information during cancer care. In this paper, we present the results from a four-week field study that examined how HealthWeaver Mobile supports cancer patients’ information management work. We found that a key contributor to the difficulties our participants experienced with managing care-related information was a lack of effective systems they could use at the clinic, out and about, and during the day when they needed to capture or access care-related information. In spite of its usefulness to patients—chiefly by providing them with a single location where their care-related information could be organized—the HealthWeaver website alone was not enough to provide support in such situations. With HealthWeaver Mobile, on the other hand, participants were able to access their information throughout the day, enabling them to look up and update their calendars, log symptoms, medications, and other information when their needs arose. This support increased participants’ confidence in their ability to manage their care effectively.
In what follows, we first give a brief overview of HealthWeaver, including both web and mobile components, and describe our study methods. We then discuss how a lack of effective information management systems contributed to our participants’ difficulties with unanchored work, and how HealthWeaver addressed those difficulties. We conclude by discussing the importance of systems that provide patients with mobile access to their health information and how such applications can enhance patients’ abilities to take active roles in their care.
HealthWeaver
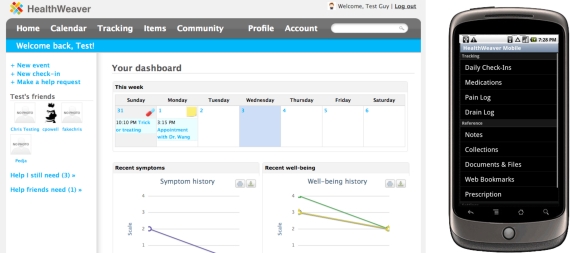
The HealthWeaver system was designed based on extensive fieldwork with, and design input from, over 50 cancer patients. It includes a web component and a mobile component. The HealthWeaver website (Figure 1, left) enables patients to manage a broad range of personal and health information that they need during treatment. It provides (1) a calendar to manage health-related events, such as appointments, (2) functionality for organizing notes, lists, bookmarks, and care-related files, (3) a system, called self check-ins, for tracking symptoms, pain, and wellbeing with automatic graphing, and (4) logs for medications, supplements, and the care of post-surgery wounds. All this information can be searched using a fast full text search system. To make access to needed information easier, patients can create links among any pieces of HealthWeaver information to make collections of information for specific purposes or to quickly access related information from an existing object. Finally, HealthWeaver enables patients to keep their social networks informed of their progress by selectively sharing care-related information with family and friends, as well as by asking for and coordinating help with rides, research, household chores, and other tasks with which the patients need assistance.
Figure 1:
The HealthWeaver website (left) and the HealthWeaver Mobile phone application (right)
HealthWeaver Mobile (Figure 1, right) provides access from a smartphone to the information stored on the HealthWeaver website and a set of unique features of its own. Using the phone application, patients can create, edit, and view the full range of information stored in HealthWeaver. In addition, patients can create photo, audio, and text notes to quickly capture information and they can immediately link those notes to related upcoming appointments. These links can make it easier for patients to find the notes, in context, later when they need them. Finally, HealthWeaver Mobile synchronizes the HealthWeaver calendar to the phone’s native calendar application, providing patients with an up-to-date view of their care appointments and access to HealthWeaver information they have linked to them. The calendar also lets patients see their care events alongside their other commitments (e.g., work). Although the version of HealthWeaver Mobile used in this study runs only on the Android operating system, the architecture of the application makes it easy to port it to other smartphone platforms, such as the iPhone.12
Methods
Between July and December of 2010, we conducted a four-week study of HealthWeaver Mobile with nine breast cancer patients undergoing active treatment. The study was reviewed and approved by the University of Washington’s Institutional Review Board. We describe the study procedures and data analysis next.
Study design and procedures
To understand how HealthWeaver Mobile supports unanchored work in comparison with the HealthWeaver website, the study used a cross-over design. Four of the participants used only the website for the first two weeks of the study. Then, they “crossed over” to the other study arm and used both the website and the mobile application for the second two weeks. To minimize order effects, the other five participants used both the web and mobile component of the system during the first two weeks and used only the web component during the second two weeks. Each participant was also interviewed during an in-person session at the start of the study, after two weeks of in situ use when they crossed over into the other study arm, and at the end of the four week study.
During the first in-person session, participants completed demographic and experience with technology questionnaires and were interviewed about their experiences with managing information during treatment for breast cancer. After the interview, we gave the participants the technology appropriate to their study arm and instructed them in its use by walking them through common tasks that HealthWeaver supports. To run HealthWeaver Mobile, the participants were given a Nexus One Android phone with the HealthWeaver Mobile application pre-installed and pre-configured to access their HealthWeaver account. The study phones were equipped with unlimited data service.
During in-situ use, the participants were asked to use the HealthWeaver system (appropriate to their study arm) to manage their care-related information during their day-to-day life. Specifically, the participants were asked to (1) use the system to prepare for an upcoming medical appointment of their choosing; (2) track at least one symptom or wellbeing parameters of their choosing (e.g., pain, stress, energy level, etc.); and (3) use the system at least three times per week to ensure sufficient experience with the study technology. Participants completed two weeks of in situ use for each study arm.
During second and third in-person sessions (at 2 weeks and 4 weeks), participants were interviewed about their experiences using HealthWeaver. We asked what participants did with the system, what they found valuable and frustrating, and in what kinds of situations they used the system. During the second session, each participant was crossed over to the other study arm. Participants were compensated $125 for their participation. All participants were allowed to continue using the HealthWeaver website beyond the end of the study.
Data analysis
We created a comprehensive set of notes for each participant that included a description of the participant’s background and a summary, with quotes, of all major discussion points from each in-person session. We then used thematic analysis to code the notes. Coding was done iteratively, and the coding categories were informed by our analysis of unanchored work9 and focused on participants’ use of the system, difficulties with information management, and sense of competence and control.
Results
In this section, we give an overview of our participants’ characteristics and discuss our results in three main areas: mitigating the challenges of unanchored work with the consistent use of an information management system, supporting unanchored work with the HealthWeaver website and the limitations of that support, and supporting unanchored work with the HealthWeaver Mobile phone application.
Participants
Nine breast cancer patients, all women, participated in the study. A tenth patient, P9, began the study but became overwhelmed with her cancer experience and chose to withdraw. The participants ranged in age from 48 to 68 (mean=57.6, median=57). At the start of the study all participants were undergoing active treatment for cancer. Four participants had Stage I disease, one had Stage II, three had Stage III, and one was a metastatic patient with Stage IV illness. Two participants began the study right before surgery, two were in chemotherapy, two in radiation therapy, two were beginning aromatase inhibitor treatment, and one was preparing for a reconstruction surgery. Two participants had a recurrence after being cancer-free for several years; the other seven had cancer for the first time.
The participants came from a wide range of occupational backgrounds. Two participants were retired (one was formerly a nurse and the other a director for a school district), one was a homemaker, and one was a freelance writer receiving disability. All other participants were employed full time. Their professions included a minister, an IT project manager, a technical writer, a postal worker, and a mental health counselor. All participants but one had a college degree and three participants had graduate degrees (two had a PhD and one a Masters degree).
All participants owned a home computer and a mobile phone and used both devices several times a week or more often. During the study, all participants used the HealthWeaver website at least three times a week, as required, and seven participants used it almost daily. None of the participants reported significant problems with using the website, regardless of their prior experience with technology. The phone component was used nearly every day by five participants, three times a week by one participant, and once or twice a week by three participants, all of whom were recovering at home and did not need to manage care information outside the house very often. One 68-year-old participant had substantial problems with using HealthWeaver Mobile due to tremors. Other participants were able to use the phone application without significant difficulties and reported only minor usability issues.
Mitigating challenges of unanchored work with consistent use of an information management system
One of our key findings is that an information management system that patients use consistently throughout the day—independent of the sophistication of the system—can mitigate the difficulties of unanchored information work. For participants who lacked such a system, managing care-related information—including calendaring, capturing of notes, and accessing information at the clinic—was very challenging. For participants who had even a simple, paper-based system that they could use throughout the day (e.g., a notebook for tracking questions for appointments), the aspects of care-related information work covered by that system were made substantially easier.
At the time of the study, P2 lacked any consistent system to help her manage information. For her, all aspects of care-related information management were frustratingly hard. Difficulties with capturing notes were a good example of this. P2 explained: “I say I will have a consistent place to put notes, but I don’t. I write them at the edge of books, I put them in my jeans and I wash my jeans, all sorts of things.” This lack of a consistent system made it difficult for P2 to hold on to any information she captured:
The fact that there is no single tool that I always have with me, paper and pen... [my partner] has an iTouch [sic.] which I occasionally use, I email things to myself all the time so they would show up in my [inbox], but I still don’t necessarily notice it… Even in my house it’s not stored in one logical place and so even if I called and said [partner’s name], please find this for me, it wouldn’t be easily accessible for her so it’s not easy to take with me to have it either.
Lack of a consistent system made tracking questions for physicians challenging as well. For example, P4 wrote her questions on notes that she later lost or forgot to integrate with her other questions, leading her to jog her memory for issues to discuss while sitting in the waiting room right before the appointment. P6 had similar difficulties. If a question occurred to her while she was at work, she wrote it on a piece of paper that she put in her pocket. Getting back to this information worked “maybe 75% of the time. Most of the time I remember to take it and put it beside my computer so I remember to put it in doctor piles I have on my desktop but sometimes I forget. Sometimes I look at it and I wrote it in code…and then I can’t remember what the code means.” P10 echoed this difficulty as well. When she collected information for appointments, she often jotted it on the closest piece of paper which easily got lost: “If I have a piece of paper somewhere, I write it down, but then you are back to those little pieces of paper that get lost, so yeah, that is a problem.” Without a consistent system, capturing notes, questions for physicians, and other information was difficult, as was the retrieval of that information later.
Our participants experienced similar problems with calendaring. P3 used a paper calendar that she kept losing. P2 did not have a calendar when she started the study and when people asked her when she was free she would “stare at them because I have no idea.” If her partner was not with her, scheduling was impossible. Similarly, P10 recalled that for a while she tried to keep her schedule in her head and that she constantly ended up double-booking herself.
Scheduling could be challenging even for participants who used a calendar. P8 used two paper calendars, one for work and one for personal appointments. Until she became sick this separation worked well for her, but “this year it’s been ghastly because I have to put cancer information on both of them. It’s ridiculous.” She sometimes double-booked herself because she had not put an appointment on both of her calendars. P5 kept her main calendar in a Microsoft Word document on her computer and just carried a small post-it note that listed the upcoming things she needed to do. Scheduling on the spot was hard because the calendar she carried was incomplete. Lastly, participants who used a paper calendar—P3, P8, P9, and P10—complained about the need to make frequent revisions and needing to use a pencil to write on the calendar so that they could erase and correct changed information.
Even a simple, paper-based system helped a great deal with unanchored information management if that system was consistently used. P1, P3, and P8 all used a single notebook where they wrote all of their care-related notes. P1 used hers to take detailed notes during appointments, keep track of her question lists, and keep copies of important test results. Most importantly, she always had the notebook with her in her purse or close at hand at home, making it easy for her to note any new information in the notebook. P3 and P8 used their notebooks in a similar way. As P8 described it, the notebook “lives with me.” Questions and answers from every appointment were in the notebook, as were her list of medications and cancer resources that other people had given her. Because of this system, these three participants didn’t experience as much trouble with the capture and retrieval of notes as did the participants who relied on more haphazard methods. P1, P3, and P8 always had their system with them, and they knew that if they needed to get back to their notes, there would be only one place where the notes could be.
A regularly used system also helped with calendaring. P1 had a paper calendar, which she used for many years. P7 used the calendar on her Blackberry, which synchronized with her online calendar. For both these participants, scheduling was not experienced as being difficult. However, for it to ease unanchored work, a system needed to be both consistent and adequate to the information needs of cancer care. P8’s system of maintaining separate work and personal calendars worked well before she got sick but it broke down when she needed to keep both calendars up to date with her myriad cancer appointments. She sometimes failed to do so, resulting in scheduling conflicts.
A consistently used information system that they could use throughout the day thus emerged as a major factor that mediated how challenging our participants experienced unanchored care-related information management. Only a handful of participants had well-established systems, and even those systems only covered a subset of frequent care-related information activities. That even such partial systems could help patients manage their care information suggests that providing patients with a system that addresses a range of care-related information management needs could be an effective way of supporting unanchored work. To this topic we now turn.
Supporting unanchored information management with the HealthWeaver website
All study participants used the web version of HealthWeaver throughout the four-week study. Overall, the HealthWeaver website was very positively received and participants thought that it helped them gain better control of their information. One feature emerged as being particularly important in this regard: providing a single location where patients’ care-related information could be organized.
Nearly all participants commented that one of the most valuable things for them about using HealthWeaver was that the system provided them with a single location for their care-related information. P3, for example, said that having her health calendar, clinical contacts, and all her medication and drain-care tracking in one place was essential: “to have it all in one place, without shuffling my papers” was extremely important to her. Even over the first two weeks of the study, HealthWeaver became “the easiest place to go” for P3 to find her information, from a phone number to the last time she took a painkiller. P6 echoed this sentiment. She stated that she felt much more organized knowing that everything was in one place so that she didn’t have to go through her folders looking for things. As she told us, “I definitely feel more empowered. Instead of having 50 pieces of paper all over, I have it all right in front of me.”
A key aspect of this benefit of HealthWeaver was that information was better organized than in the systems that the participants previously used. P3, for example, stated that HealthWeaver was far better organized than her binder: “here [in HealthWeaver] it’s filed properly because there are particular places to put [information]. An appointment is on the calendar, it will not be on a list, so it forces you to organize.” One effect of this built-in organization structure was that participants felt it was easier for them to access information when they needed it. P1, P3, and P8 all used the comment field in HealthWeaver calendar events to keep track of important points that were discussed during appointments. Doing this allowed them to quickly find these appointment notes just by opening the calendar event, without needing to flip through pages and pages in their notebooks to find where they wrote them. Similarly, P2 used the notes field on her self check-ins extensively. It was important to her to know that she could just scan through the first few words of those notes to get back to her reflections on how her health situation was evolving. By providing a unified and organized place for their information, the HealthWeaver website made it possible for participants to quickly get back to care-related information—thus supporting an important aspect of unanchored patient information work.
Unifying information in HealthWeaver also had a positive psychological effect: it gave participants greater confidence than they had before that they were in control of their information. P3 described this well:
And then, there was a lot of confidence that if I put it there, it would be there when I went back. And there was not a lot of confidence that when I went back to my paper file that it would still be there. Because sometimes I would take it out and take it to the telephone in another room, and then I would have to put it back, and then put it back in a similar place. So there was a lot of time I spent with my binder tearing everything out, going through it looking for something that might not even be there. [With HealthWeaver,] I would have confidence that it would still be there.
In spite of the benefits of unification and organization of information, however, the HealthWeaver website turned out to be insufficient to fully support effective management of care-related information. A number of situations occurred during the study when the website provided insufficient support for participants’ unanchored information activities. This was the case both for participants who used the website first—and who did not know about HealthWeaver Mobile until after the second interview—and the participants who used HealthWeaver Mobile first and used only the website during the second part of the study. We briefly describe these situations next.
One type of situation for which the website proved insufficient was during clinical appointments. P3, a participant who was in the web-only arm during the first half of the study, started her second interview with the following:
[I made] a list of questions for the oncologists, I then printed them out, and then I left the paper at home. So when you asked [last time] have you ever been out somewhere and not have your information, I said ‘oh I always have my trusted binder’, but if I had my iPhone I could have looked up all my questions, but I didn’t, so I didn’t have my questions.
P3 thought she remembered most of the questions, but said that “I would have been more confident if I have had them in front of me.” Similarly, P1 went to see her oncologist and forgot to print the medication list with the antibiotic that her dentist had prescribed. She noted that had she been able to use HealthWeaver there she could have just printed the list and handed it to the clinic staff. Without access to a computer at the clinic, the information these participants prepared to use during their appointments, but then forgot, was not available.
Another situation when the website did not provide sufficient support was when participants needed to be away from home for several days. During the second part of the study, after she returned the phone, P2 went for a long weekend camping trip. While on the trip she had symptoms she wanted to record, but by the time she got back “a million things have happened that normally don’t happen and I have forgotten about it.” P7 had a similar thing happen when away on an out-of-town trip. By the time she came back, she had forgotten the details of what she wanted to record in HealthWeaver.
Finally, there were situations when the participants wanted to record information they needed to get back to but did not have the right tools to do so. P2 gave a good example of this situation. Thinking back about the second part of the study when she didn’t have the phone, she said that “I spent a whole bus ride to my doctor in thinking of things and forgetting them, and thinking of things and forgetting them, and writing them down on little pieces of paper that I then can’t find when I get there, so even that, just having them in one place where I wouldn’t forget is very nice.”
These examples confirm that care-related information needs arise in situations when desktop or web-based systems are not enough to support effective information management. Although HealthWeaver provided support for certain aspects of unanchored work—such as quick retrieval of care-related information—unanchored needs that arose when participants were away from home were not addressed by the HealthWeaver website. When the website was unavailable the system could not be used consistently. The phone portion of the study provided evidence that a mobile tool can better support such information needs. To this topic we now turn.
Supporting unanchored information management with HealthWeaver Mobile
For two of the four weeks of the study, participants had access not only to the HealthWeaver website but also to the mobile component of the system, HealthWeaver Mobile. Their experiences with HealthWeaver Mobile supplement the findings reported in the last section and indicate that a mobile application can play an important role in helping patients manage their care-related information. In particular, participants found that HealthWeaver Mobile provided an effective way to access information at the clinic, to keep their health calendars up to date, and to record and look up information throughout the day. In addition, HealthWeaver Mobile enabled participants to manage health information when it was most convenient for them to do so. A key outcome of using HealthWeaver Mobile in these ways was that the participants felt more confident overall in their ability to manage their care-related information.
Managing information at the clinic
One type of use for which participants saw HealthWeaver Mobile as very helpful was to access information at the clinic. P2 used the phone extensively for this purpose. She used the phone to look up her self check-ins during appointments with her oncologist in order to tell her when her restless leg started and to show her the graphs of her worsening hip pain. P2 thought that having this data made her doctor take her symptoms more seriously: “I think that the fact I had it [data] for day after day after day and I could show her what was going on make her actually take it more seriously.” P8 saw a similar benefit of using the phone at the clinic. She thought that having “evidence” and showing it to the physician would make it easier for the physician to acknowledge a problem than if P8 relied on her memory to describe how her symptoms had changed over the previous two months.
HealthWeaver Mobile was used at the clinic for more than sharing of symptom data, however. P2 also used the phone to facilitate her conversation with her oncologist about her chemotherapy regimen. She explained that she was receiving Taxol and Avastin but that she had recently seen an article in New York Times that Avastin was not effective for breast cancer and that the FDA was recommending alternative treatments. This really upset P2 and she wanted to talk to her oncologist about the article. She saved the article in HealthWeaver and then used the phone to show it to the oncologist during her next appointment. P2 described the experience as follows:
It worked great. She [the oncologist] read a couple of paragraphs to make sure she understood the gist of it and handed it back to me and we talked about it and it was perfect. Because other times I have described things I’ve read, thinking she’d know about them, and sometimes she has but other times she hasn’t, and I haven’t remembered enough of the gist to have a conversation about it. So that part was great.
Similarly, P3 thought that HealthWeaver Mobile could be particularly helpful for answering physicians’ questions during appointments. Since HealthWeaver was better organized than her binder, she thought that accessing the needed information on the phone would be faster than paging through her binder.
Finally, for P7, the weight of the phone was a crucial factor for its usefulness at the clinic. As she was finishing the study, P7 was transferring her care from a local cancer center to another cancer center in another state. She explained that she was taking her laptop with her, but that the computer was too heavy for her to carry all day while she was making care arrangements at the new hospital. She planned to leave the laptop at her hotel and use her personal phone to access HealthWeaver at the clinic.
Calendaring
P2, P3, P5, and P8 used HealthWeaver Mobile for calendaring a great deal. They used the calendar at the clinic, in their cars, and on the bus. A chief benefit of being able to enter events on the phone was that the participants didn’t have to rely on their memory to enter appointment slips and other new commitments into the HealthWeaver calendar on the web when they got home—an activity that was made more difficult to do consistently due to stress and symptoms. P3 recalled that she was extremely alarmed when she realized, days later, that she had not entered the appointments she received on a printout from the clinic scheduler into her HealthWeaver calendar. The HealthWeaver calendar had become essential to her—“if it’s not there, I am not going to show up”—so keeping it accurate was very important. To avoid this problem happening again, during the second half of the study she used the phone to enter new events while she was out, as soon as she made a new time commitment. P2 made a similar point: “I really liked having the calendar with me and being able to add to it when I was out and about and not try to remember when I got home.”
Another benefit of the phone calendar was that participants could attach other related information to their calendar appointments through HealthWeaver’s linking feature. For example, P2 and P5 both attached the directions to appointments they had not gone to before (for a psychiatric oncologist and a cancer support group, respectively) so that they would have the directions quickly accessible while they were on the way to the appointment. Similarly, P8 entered notes from each clinical appointment into the comment field in the calendar event for that appointment. She was able to use the phone to refer to these notes when she was giving her friends an update on her health situation. Having the health calendar on the phone, therefore, both helped the participants to keep their calendar up to date and quickly access information related to their health events.
Ad-hoc recording and access to care-related information
HealthWeaver Mobile also made it possible for patients to access and record care-related information in situations when an information need arose unexpectedly. For example, P2 went for a weekly urine test only to find out that the lab did not have her on the schedule that week. She got upset thinking that her test wouldn’t be done in time for her next appointment, and she used the phone to look for her doctor’s phone number in HealthWeaver so she could resolve the issue. It turned out that the lab’s schedule was correct and that the test was not needed that week. Similarly, P8 was having a discussion with a friend about her symptoms and used the phone to look up notes that she took about her symptoms.
The participants occasionally used the phone to enter care-related information into HealthWeaver as well. For example, P3 took notes on the phone while she and her husband were driving back from an appointment and were discussing what had taken place. As she explained, “it’s invaluable to capture that immediately [because] I would forget things that were said.” Although P3’s husband often remembered things that she forgot, sometimes both of them didn’t remember the details after some time passed and keeping that information was important for them to make treatment decisions. The phone helped P3 to immediately capture a few key terms that she could later use to reconstruct the conversation and remember the main points she needed to record.
Managing care information at the most convenient times
In addition to supporting acute unanchored information needs, HealthWeaver Mobile turned out to have an additional benefit: mobility afforded by the phone application made it possible for participants not only to manage information when specific needs arose, but also at times when managing care-related information best fit into their daily schedules. For example, P1 often used the phone to enter self check-ins even while she was at home, when her computer was readily available. She explained:
Maybe it’s how I operate. I will organize myself in the morning. Get up, drink some coffee to get awake, read the newspaper, discuss it with my husband, and then I will pick up my calendar and while I am doing that, I would use the little computer system, the HealthWeaver system on the phone when I did the organizational things. It just became a part of what I did in the morning.
P1 explained that using the phone enabled her to enter check-ins in the dining room, where she spent the mornings with her husband, rather than having to go to the library where her computer was plugged in. The phone, she said, “was easier to access and faster, and because of that I was more consistent.”
Similarly, P6 used the phone to enter notes while she was on the ferry during her commute to appointments at the cancer center, taking advantage of this time to work on her health information. She also wanted to use the phone to work on her information during her lunch breaks, but the place where she worked did not have good cellular coverage and she was not able to use HealthWeaver Mobile for that reason. P8 made a similar point about the convenience of access. The phone made it possible, she said, to work on her health information during the few minutes of free time between appointments with her counseling clients and other short breaks during her work day. “If I have 15 minutes, if I’m waiting for something, I’ll do it then…I live a really busy life with not very much time. So, this was great, if I had any little time I could do stuff on it that I wanted to do.” Although a longer study is needed to determine how patients incorporate HealthWeaver Mobile into their daily routines, these results suggest that smooth integration of health information management with other aspects of patients’ lives might be a major benefit of such mobile applications.
Supporting patients’ sense of information management competence
Our study data suggest that an important outcome of the support that HealthWeaver Mobile provides for unanchored information management is patients’ enhanced sense of competence during care. Several participants discussed issues of confidence and control related to their experiences with using the mobile system. Reflecting on her experiences in the study, P2 said that she felt that using the system helped her become more involved in her care:
I don’t know that I’ve felt more competent, but I’ve been a little more involved. That’s half of my problem, I just want to give it to my partner to do and I need to do a little more of it myself...I honestly think that working with that Android calendar that I thought I should give Google Calendar another try. So, if nothing else, you drove me back to calendaring, which is good. I felt that I knew what was coming up the next day, which is good.
While the phone provided P2 with awareness of what was coming up, helping her become more engaged with her care, the phone gave P3 and P8 confidence that they would always have the information they needed. P3 explained: “I think this [phone] could be really key, to take with you, just to have the confidence that anything they ask you, you can look up.” P8 made a similar point. When asked in the final interview what was the most valuable aspect for her of having access to HealthWeaver, she replied: “number one, it really makes me feel like I have more control over the information I need and it really has helped me feel that way. It feels more organized to me and I know where to go looking for information I need and that I’ll find it.” But the phone was an important part of this: “the phone definitely contributed to that. It just meant that I could always look up stuff if I needed to.”
The participants also indicated that just knowing that they had a backup if they forgot something or an unexpected need arose was helpful to them. P2 was very explicit about this point. Talking about the need to review her symptom logs before her next appointment after the completion of the study, she said: “the odds that I will leave the house on Friday without having reviewed it or having printed it out, however, are overwhelmingly high. I am a very forgetful person. I really did love having the mobile connection so that even if I did leave the house without looking at it, I would be able to look at it there.” Similarly, when she forgot her question list when she went to an oncologist appointment, P3 recognized that having access to HealthWeaver from the phone would have enabled her to pull her list up and have confidence that she would be able to ask all her questions.
Comments such as those of P3 and P8 indicate that having a backup afforded by mobile access to their collection of health information gives peace of mind even to patients who are typically very organized. For patients who are not as prepared, such as P2, mobile systems for health information management might provide even a greater benefit.
Discussion and conclusions
An important finding of this study was that even simple information management systems that participants used regularly throughout the day, such as a spiral notebook, could substantially ease the challenges of unanchored patient work. In light of this, it is not surprising that the participants that seemed to benefit the most from having access to HealthWeaver Mobile were those who did not have a good system prior to the study. P2, who prior to the study lacked any consistent systems, found HealthWeaver Mobile extremely helpful. However, even those participants who had systems for managing care-related information on the go typically only used a partial system. P3 was good about taking notes in her spiral notebook, but had trouble with keeping a calendar. P1 and P8 used both a notebook for notes and a paper calendar, but neither had a good way of tracking their symptoms and medications. And some systems just plainly didn’t work very well—like P8’s use of two paper calendars.
For these reasons, HealthWeaver and HealthWeaver Mobile turned out to be valuable even to participants who previously tried to stay on top of their information. The HealthWeaver website gave participants a way to organize a larger portion of their care-related information and the confidence that they would know where to look for it when they needed that information again. However, in a number of situations that our participants experienced even during this short study, they did not have access to the website when they needed their care information. Thus, the phone played a key role in supporting participants’ information management efforts, both by facilitating specific unanchored activities—e.g., looking up information at the clinic, capturing a note during a drive back from an appointment, etc.—and by giving participants the confidence that if an expected need arose or they forgot to bring something to the clinic, they could get back to the needed information. In addition, by enabling them to work with their health information at times when it was convenient, such as on the ferry or between appointments, the mobile application helped participants to actively engage with their health information—and by extension, with their care.
Active engagement in care and patients’ sense of competence and autonomy are both related to positive health outcomes.13–15 Thus, our findings provide preliminary evidence that mobile applications that enable patients to manage their health and care-related information can support these important psychosocial outcomes beyond the support provided by web-based health information management tools, such as PHRs.
Our data on the unifying and organizational value of the HealthWeaver website also suggest that mobile applications for personal health information management should not be standalone systems but should be tethered to a larger system, such as a PHR, that can serve as a master repository for patients’ information. In fact, our findings indicate that access to a mobile system can facilitate patients’ involvement with the tethered website, increasing the consistency and frequency with which the website is used and, consequently, its value to patients. Providing mobile access thus might be another way to attack the problem of PHR adoption.
In all, these findings suggests that adding robust mobile access to patient portals and third party PHRs should be an important goal for organizations that develop or leverage these products. At the same time, the variety of data that our participants needed to manage for their care—from calendaring information to questions, bookmarks, and notes—do not currently fit comfortably in the data model that most PHRs use. Expanding the range of information that can be stored in PHRs—and supporting these new information types through mobile applications—would greatly increase the usefulness of such systems to patients.
Mobile health applications are not new. Applications for tracking symptoms, for logging diet and exercise, and for remote monitoring of patients with serious health risks are widely available. However, mobile applications that provide PHR-type functionality have not seen the same level of development. Our findings indicate that such applications can be greatly beneficial to patients. By supporting unanchored information work, applications like HealthWeaver Mobile can help patients to manage their information effectively and take control of their health.
References
- 1.Gustafson DH, Hawkins RP, Boberg EW, et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. Int J Med Inform. 2002;65(3):169–177. doi: 10.1016/s1386-5056(02)00048-5. [DOI] [PubMed] [Google Scholar]
- 2.Moore SM, Ruland CM, Jeneson A, Andersen T, Andersen R, Slaughter L, Bente-Schjødt-Osmo Designing tailored Internet support to assist cancer patients in illness management. AMIA Annual Symposium Proceedings; American Medical Informatics Association; 2007. pp. 635–639. [PMC free article] [PubMed] [Google Scholar]
- 3.Gustafson D, Hawkins R, Pingree S, et al. Effect of computer support on younger women with breast cancer. Journal of General Internal Medicine. 2001;16(7):435–445. doi: 10.1046/j.1525-1497.2001.016007435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim MI, Johnson KB. Personal health records: evaluation of functionality and utility. J Am Med Inform Assoc. 2002;9(2):171–180. doi: 10.1197/jamia.M0978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Detmer D, Bloomrosen M, Raymond B, Tang P. Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak. 2008;8:45. doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osborn CY, Mayberry LS, Mulvaney SA, Hess R. Patient web portals to improve diabetes outcomes: a systematic review. Curr. Diab. Rep. 2010;10(6):422–435. doi: 10.1007/s11892-010-0151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gysels M, Richardson A, Higginson IJ. Does the patient-held record improve continuity and related outcomes in cancer care: a systematic review. Health Expect. 2007;10(1):75–91. doi: 10.1111/j.1369-7625.2006.00415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klasnja P, Civan Hartzler A, Unruh KT, Pratt W. Blowing in the wind: Unanchored patient information work during cancer care. Proceedings of the 28th international conference on Human factors in computing systems; Atlanta, GA. ACM Press; 2010. pp. 193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bielli E, Carminati F, La Capra S, et al. A Wireless Health Outcomes Monitoring System (WHOMS): development and field testing with cancer patients using mobile phones. BMC Med Inform Decis Mak. 2004;4:7. doi: 10.1186/1472-6947-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kearney N, McCann L, Norrie J, et al. Evaluation of a mobile phone-based, advanced symptom management system (ASyMS©) in the management of chemotherapy-related toxicity. Support Care Cancer. 2008;17:437–444. doi: 10.1007/s00520-008-0515-0. [DOI] [PubMed] [Google Scholar]
- 12.Klasnja P, Hartzler A, Powell C, Phan G, Pratt W. HealthWeaver Mobile: Designing a mobile tool for managing personal health information during cancer care. AMIA Annual Symposium Proceedings; American Medical Informatics Association; 2010. pp. 392–396. [PMC free article] [PubMed] [Google Scholar]
- 13.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA. 1996;275(2):152–156. [Google Scholar]
- 14.Bárez M, Blasco T, Fernández-Castro J, Viladrich C. A structural model of the relationships between perceived control and adaptation to illness in women with breast cancer. J Psychosoc Oncol. 2007;25(1):21–43. doi: 10.1300/J077v25n01_02. [DOI] [PubMed] [Google Scholar]
- 15.Watson M, Homewood J, Haviland J, Bliss JM. Influence of psychological response on breast cancer survival: 10-year follow-up of a population-based cohort. Eur. J. Cancer. 2005;41(12):1710–1714. doi: 10.1016/j.ejca.2005.01.012. [DOI] [PubMed] [Google Scholar]