Abstract
This paper presents preliminary outcomes associated with an experimental, longitudinal study of a Multiple Family Group (MFG) service delivery approach set within thirteen urban outpatient clinics serving children and their families living in inner-city, primarily African American and Latino communities. Specifically, this paper focuses on parent reports of child oppositional behavior and parenting stress over time. MFG is a flexible, protocol-driven approach designed to address the most common reason for referral to outpatient child mental health clinics, childhood behavioral difficulties. The MFG also aims to enhance family-level engagement and retention in ongoing care. Further, the service delivery model was collaboratively developed with intensive input from parents rearing children with conduct difficulties, parent advocates, community-based child mental health providers and services research staff in order to ultimately expand the number of effective service models that can be situated within “real world,” urban child mental health settings.
Each year, billions of dollars are spent responding to the legal, correctional, educational and psychological needs of disruptive youth (Burke, Loeber, & Birmaher, 2002; Foster & Jones, 2005). Nationwide, oppositional or aggressive behaviors are found among 5 to 10% of 8 to 16 year olds and account for one-third to one-half of all youth mental health referrals (Angold & Costello, 2001; Frick, 1998; Frick & Muñoz, 2006; Rowe, Maughan, Pickles, Costello, & Angold, 2002). However, within urban, low-income communities, significantly higher prevalence rates of childhood conduct related difficulties, ranging from 24 to 40%, have been found (Gorman–Smith, Tolan, Henry & Florsheim, 2000). Thus, addressing urban child conduct difficulties is a serious public health need. Further, emerging evidence suggests that despite recent advancements in the development of effective child mental health service models, there continues to be serious barriers in connecting the most vulnerable of children and their families with care. Therefore, the development of effective interventions associated with high engagement and retention of youth and families residing in urban, low income communities is greatly needed.
A disproportionate number of children with mental health problems do not receive adequate mental health care (National Institute of Mental Health, 2001; Ringel & Sturm, 2001; US Department of Health and Human Services, 2010; US Public Health Service, 2000, 2001). Specific to minority youth, addressing the serious disparities regarding receipt of appropriate, quality mental health service has also been urgently emphasized (Garland, Lau, Yeh, McCabe, Hough, & Landsverk, 2005; Kataoka, Zhang, Wells,2002; Padgett et al., 1994a,b). This is particularly important since urban minority youth are most deeply affected by the stressors that exist within inner-city communities, notably poverty, community violence, inadequate child-serving resources, under supported schools and substance abuse (Attar, Guerra, & Tolan 1994; Gorman-Smith, Tolan, & Henry, 1999; Grant et al., 2005; Hess & Atkins, 1999; Weist, Acosta, Youngstrom, 2001). Further, the number of children in need of care within urban communities far outstrips the availability of services and the number of service providers. Waiting lists for care within inner-city communities can extend up to six months (Brown, 2002). Accordingly, there appears to be a need for a comprehensive mental health service model capable of addressing the most common reason for referrals, barriers to services for urban children and serious service capacity issues.
Thus, the current paper presents preliminary outcomes of a study involving a Multiple Family Group (MFG) service delivery strategy tested in collaboration with thirteen urban outpatient clinics set within primarily African American and Latino communities. MFG is a protocol-driven approach designed to address oppositional defiant and conduct difficulties (Franco, Dean-Assael, & McKay, 2008; Gopalan & Franco, 2009). In addition, the MFG was specifically designed to enhance engagement and retention in outpatient child mental health care, as well as to contribute to the number of effective services that can be situated within “real world,” urban child mental health settings.
Multiple Family Groups (MFG) for Children with Behavioral Difficulties
The multiple family group service delivery strategy targets school-age, inner-city children (7 to 11 years of age) meeting diagnostic criteria for Oppositional Defiant (ODD) or Conduct Disorders (CD) and their families (including adult caregivers and siblings between the ages of 6 to 18 years). MFG consists of a 16-week series of group meetings with 6 to 8 families present in each group, and the intervention protocol which guides each group meeting was designed in collaboration with urban parents in previous studies to strengthen specific aspects of parenting skills and family relationship processes (e.g., child management skills, parental discipline practices, family communication, within family support and positive parent/child interaction) (McKay, Gonzales, Quintana, Kim, & Abdul-Alil, 1999; McKay, Gonzales, Stone, Ryland, & Kohner,1995; McKay, Harrison, Gonzales, Kim, & Quintana, 2002; see Franco, Dean-Assael, & McKay, 2008 for an earlier published version of the intervention protocol). In addition, intervention sessions were designed to target factors (e.g., parental stress, use of emotional and parenting support resources, and stigma associated with mental health care) which potentially impact inner-city child mental health service use and outcomes. See Tables 1 and 2 for a summary of empirically supported intervention targets and session goals.
Table 1.
Summary of empirically supported family-level influences on ODD and CD
| MFG target | Family process or parenting skill linked with youth conduct problems or associated with positive youth behavioral outcomes |
|---|---|
| Rules | 1) family organization; 2) consistent non harsh discipline practices, including clear behavioral limits, appropriate consequences and reinforcement; 3) parental monitoring and supervision skills |
| Responsibility | 1) family interconnectedness; 2) positive behavioral expectancies for youth |
| Relationships | 1) family warmth and attachment; 2) within family support and; 3) time spent together |
|
Respectful Communication |
1) family communication; 2) family conflict; 3) parent/child interaction |
| Stress | 1) parenting hassles;2) parenting stress; 3) life stressors, 4) socio-economic disadvantage |
| Social support | Social isolation |
Table 2.
Summary of MFG intervention targets
| MFG target | MFG session |
MFG goals |
|---|---|---|
| Rules | 3 & 9 | 1) Families clarify the set of rules that are operate in the family 2) Rules are more clearly identified for children 3) Parents examine their own behavior in relation to rules 4) Consequences for not following the rules are clarified 5) Rewards and giving praise for following the rules is increased 6) Parents come to understand link between behavioral success at home and in school or community |
| Responsibility | 4 & 10 | 1) Roles of parents and children are clarified 2) Each family member is given credit for the contribution that they already make to the family 3) Expectations for children are clarified 4) Parents identify areas where they need additional support and problem solve about ways to obtain necessary resources |
| Relationships | 5 & 11 | 1) Families develop a consistent time to spend together 2) Families schedule fun activities, promoting positive relations |
| Respectful communication |
6 & 12 | 1) Parents develop enhanced abilities to communicate with children so that they will attend and understand 2) Parents develop enhanced ability to listen to their children and be more available to them 3) Children become able to discuss concerns with their parents; 4) Children are able to more carefully attend to parent communication |
| Stress | 7 & 13 | 1) Families can identify the stressors that hinder the 4 R’s 2) Families will feel support from the group and have the opportunity to share experiences that have been stressful in their lives 3) Parents and kids will become more aware of the stressors each one faces 4) Families will have the opportunity to practice supporting and communicating with each other in hopes of alleviating stress |
| Social support | 8 & 14 | 1) Parents see themselves as supports for each other 2) Kids see their parents as supports for them 3) Families identify the need for building supports in their lives 4) To be able to identify times when support is needed |
Involving the entire family in a series of group meetings was based upon strong existing evidence for a set of family-level risk factors related to the occurrence and persistence of serious conduct problems during childhood (see Table 1). More specifically, poor levels of parental discipline, monitoring, family communication, within family support, family interactions and bonding, and family disorganization, stressors, and conflict have been associated with conduct problems (Burke et al., 2002; Grant et al., 2005; Gutman, McLoyd, & Tokoyawa, 2005; Keiley, 2002; Kimonis & Frick, 2010; Kumpfer & Alvarado, 2003; Shaw, Vondra, Hommerding, Keenan, & Dunn, 1994; Alexander, Robbins, & Sexton, 2000; Dishion, French & Patterson, 1995; Kilgore, Snyder, & Lentz, 2000). For families living in more disadvantaged environments, specific factors affect parenting and influence the development of behavioral difficulties, such as poverty, social isolation, high stress and lack of social support (Kazdin & Whitley, 2003; Kazdin, 1995; Kotchick, Dorsey, & Heller, 2005; Wahler & Dumas, 1989).
Furthermore, the stressors that parents experience in their role as parents may impact parenting practices, and in turn, child mental health. A number of internal (e.g., parent’s mental health) and external factors (e.g., neighborhood context, child temperament) contribute to parental stress (Copeland & Harbaugh, 2005; McPherson, Lewis, Lynn, Haskett, & Behrend, 2009; Misri, Reebye, Milis, & Shah, 2006; Ostberg & Hagekull, 2000; Sheinkopf et al., 2006). Through its’ effect on parenting practices, parenting stress has been associated with poor parent-child interaction, and child disruptive behaviors (Crnic & Low, 2002; Deater-Deckard, 2004; Grant et al., 2003; Kazdin & Whitley, 2003; Morgan, Robinson, & Aldridge, 2002). Thus, supporting families and reducing the effect of each of these family factors is the basis for MFG.
Multiple Family Groups with Other Populations
Over the last three decades, evidence has emerged that supports the use of MFG with a range of populations. More specifically, the MFG modality has been developed and most frequently used within inpatient psychiatric settings with adults with serious mental illness (Anderson et al., 1986; McFarlane, 2002). In fact, strong empirical evidence suggests that family involvement in multiple family groups is significantly associated with improved adult outcomes, rehabilitative and vocational success, medication compliance, and reduced psychiatric hospitalizations (Dyck, Hendryx, Short, Voss, & McFarlane, 2002; Dyck et al., 2000; Lukens & Thorning, 1998). These particular multiple family groups rely upon psychoeducational models that provide both the adult and their families with information about mental illness within a group context that decreases stigma while offering support, suggestions for coping and opportunities to problem solve (Goldstein & Mikloitz, 1995; Hogarty et al., 1991; McFarlane, 2002).
In addition, the use of MFG has been described with battered women and their children (Rhodes & Zelman, 1986), urban families (Aponte, Zarski, Bixentine, & Cibik, 1991; McDonald et al., 2006), clients of family service agencies (Gritzer & Okun, 1983), families with difficulties in parent-child relationships (Cassanno, 1989), African American families (Boyd-Franklin, 1993), juvenile offenders and their families (Caldwell, Horne, Davidson, & Quinn, 2007) and with adopted adolescents and their families (Lang, 1993). Further, MFG has been described as being potentially effective with families experiencing a range of difficulties, including depression (Lemmens et al., 2009; Robinson, Berman, Neimeyer, 1990); drug abuse (Wermuth & Scheidt, 1986); chronic or life threatening illness (Steinglass, 1998); and children at risk of placement (Meezan & O’Keefe, 1998). In relation to use with children experiencing mental health disorders, there is evidence of their impact on youth mood disorders (Fristad, Gavazzi, & Mackinaw-Koons, 2003; Fristad, Goldberg-Arnold, & Gavazzi, 2002). Thus, pursuing a MFG service delivery model as a potentially effective option within the field of child mental health appears promising based on this growing body of knowledge.
Methods
The current study examined the preliminary impact of the MFG service delivery approach on two outcomes: 1) youth oppositional behavior and 2) parent stress over time.
Outcomes associated with the MFG are currently being examined via a 2 group (random assignment of youth and their family members to either the MFG or comparison condition consisting of standard outpatient child mental health care) by 5 assessments (baseline, 8 weeks (midway through the MFG) posttest (16 weeks), 6 and 18 month follow-up) research design as part of a R01-level study funded by the National Institute of Mental Health granted to the first author. Only data from the first four assessment periods are included here as the longitudinal study is still ongoing.
Data from thirteen participating outpatient community-based clinics are included. Data from the first 321 participating youth and their families were available for analyses at the time that this paper was prepared. All adult caregivers provided active informed consent and all youth participants provided assent. IRB approval was secured for this study.
Participants were randomly assigned within clinics to study one of two study conditions, MFG or standard care. Randomization procedures were as follows. The first 6–8 families whose children were screened and met eligibility criteria were enrolled in the experimental condition. The next 3–4 families who were successfully screened and met eligibility criteria were then assigned to the comparison condition (see details regarding eligibility and procedures in next sections of this paper).
Sample
To date, the study has involved 321 youth (ages 7 to 11 years) and their families (including adult caregivers and siblings between the age of 6 and 18 years) nested within child outpatient mental health clinics (n=13) that serve low income, African American and Latino children. See Table 3 for description of participating youth and their families.
Table 3.
Demographic Characteristics of Participants
| Total (n = 321) |
Experimental (n = 224) |
Control (n = 97) |
||||
|---|---|---|---|---|---|---|
| Characteristic | n | %a | n | %a | n | %a |
| Caregiver Ethnicity: | ||||||
| White/Caucasian | 30 | 9.35 | 21 | 6.54 | 9 | 2.80 |
| Black/African American | 96 | 29.91 | 62 | 19.31 | 34 | 10.59 |
| Hispanic/Latino | 169 | 52.65 | 119 | 37.07 | 50 | 15.58 |
| Native American | 3 | 0.93 | 2 | 0.62 | 1 | 0.31 |
| Asian/Pacific Islander | 2 | 0.62 | 1 | 0.31 | 1 | 0.31 |
| Other | 13 | 4.05 | 12 | 3.74 | 1 | 0.31 |
| Child Ethnicity: | ||||||
| White/Caucasian | 25 | 7.79 | 16 | 4.98 | 9 | 2.80 |
| Black/African American | 95 | 29.60 | 65 | 20.25 | 30 | 9.35 |
| Hispanic/Latino | 157 | 48.91 | 112 | 34.89 | 45 | 14.02 |
| Native American | 8 | 2.49 | 3 | 0.93 | 5 | 1.56 |
| Asian/Pacific Islander | 1 | 0.31 | 0 | 0.00 | 1 | 0.31 |
| Other | 21 | 6.54 | 15 | 4.67 | 6 | 1.87 |
| Primary Caregiver: | ||||||
| Mother | 253 | 78.82 | 175 | 54.52 | 78 | 24.30 |
| Father | 6 | 1.87 | 5 | 1.56 | 1 | 0.31 |
| Mother and Father | 24 | 7.48 | 21 | 6.54 | 3 | 0.93 |
| Grandparent | 14 | 4.36 | 6 | 1.87 | 8 | 2.49 |
| Other | 14 | 4.36 | 9 | 2.80 | 5 | 1.56 |
| Caregiver Marital Status: | ||||||
| Single | 137 | 42.68 | 86 | 26.79 | 51 | 15.89 |
| Married or Cohabiting | 106 | 33.02 | 80 | 24.92 | 26 | 8.10 |
| Divorced | 14 | 4.36 | 7 | 2.18 | 7 | 2.18 |
| Separated | 44 | 13.71 | 34 | 10.59 | 10 | 3.12 |
| Widowed | 7 | 2.18 | 4 | 1.25 | 3 | 0.93 |
| Other | 4 | 1.25 | 4 | 1.25 | 0 | 0.00 |
| Family Income: | ||||||
| Less than $9,999 | 125 | 38.94 | 91 | 28.35 | 34 | 10.59 |
| $10,000 to $19,999 | 81 | 25.53 | 55 | 17.13 | 26 | 8.10 |
| $20,000 to $29,999 | 47 | 14.64 | 32 | 9.97 | 15 | 4.67 |
| $30,000 to $39,999 | 23 | 7.17 | 14 | 4.36 | 9 | 2.80 |
| $40,000 to $49,999 | 5 | 1.56 | 3 | 0.93 | 2 | 0.62 |
| Over $50,000 | 17 | 5.30 | 13 | 4.05 | 4 | 1.25 |
| Caregiver Education Status: | ||||||
| 8th Grade or Less | 32 | 9.97 | 27 | 8.41 | 5 | 1.56 |
| Some High School | 91 | 28.35 | 60 | 18.69 | 31 | 9.66 |
| Completed H.S./G.E.D. | 77 | 23.99 | 51 | 15.89 | 26 | 8.10 |
| Some College | 71 | 22.12 | 48 | 14.95 | 23 | 7.17 |
| Completed College | 21 | 6.54 | 16 | 4.98 | 5 | 1.56 |
| Some Grad/Prof. School | 6 | 1.87 | 5 | 1.56 | 1 | 0.31 |
| Competed Grad/Prof. School | 14 | 4.36 | 9 | 2.80 | 5 | 1.56 |
| Caregiver Employment Status: | ||||||
| Employed Full-Time | 75 | 23.36 | 54 | 16.82 | 21 | 6.54 |
| Employed Part-Time | 54 | 16.82 | 40 | 12.46 | 14 | 4.36 |
| Student | 18 | 5.61 | 13 | 4.05 | 5 | 1.56 |
| Retired | 8 | 2.49 | 3 | 0.93 | 5 | 1.56 |
| Disabled | 37 | 11.53 | 26 | 8.10 | 11 | 3.43 |
| Unemployed | 104 | 32.40 | 71 | 22.12 | 33 | 10.28 |
| Other | 16 | 4.98 | 10 | 3.12 | 6 | 1.87 |
| Caregiver age (mean ± SD) | 310 | 36.43 ± 8.74 | 215 | 35.74 ± 8.41 | 95 | 37.99 ± 9.30 |
| Child age (mean ± SD) | 299 | 8.87 ± 1.41 | 208 | 8.88 ± 1.45 | 91 | 8.85 ± 1.33 |
Note: Numbers may not add up to n=321 due to missing data
% is out of Total sample size (n = 321)
Description of Participating Outpatient Child Mental Health Clinic Research Sites
The 13 outpatient child mental health clinics involved share common characteristics. All the sites included in the study provide a range of mental health services to youth and their families living in the New York City metropolitan area. Further, the vast majority of youth served at each site are low income. Generally, youth and families at each of the sites are members of minority groups with the largest proportion of youth being Latino (with ties to Puerto Rico, Dominican Republic or Mexico) or African American.
Recruitment and Informed Consent Procedures
Providers at each site received information about the study and were given printed materials to provide to their clients about participation. Recruitment strategies included: 1) a strong on-site presence at each of the clinics; 2) on-going reminder telephone contact with clinic supervisor to encourage planning to introduce the study to families scheduled for intake appointments; 3) presentation at staff meetings to problem solve any obstacles to recruitment; 4) meetings with families took place during after school and evening hours and concerted efforts to follow-up immediately with the family immediately upon their expression of interest were made.
Potentially eligible youth and their families (based on an intake diagnosis of ODD and CD made by clinical service providers) were informed of the study by their providers. Then, if the family was interested in learning more about the study, they were contacted by a member of the research staff. Informed consent materials were provided to the family by the research staff. If the adult caregiver provided consent and the youth provides assented, then the research staff administered two screening instruments to confirm the presence of clinically significant disruptive behavior difficulties to determine study eligibility. Over ninety percent of youth screened eligible for the study. If the youth and family were screened as eligible, then the family was immediately assigned to one of the two study conditions.
Description of Multiple Family Group Intervention Protocol
The MFG service delivery strategy is a 16-week series of meetings guided by a protocol (McKay, Gonzales et al., 1995). Groups are held weekly and are facilitated by mental health providers and parent advocates. Groups consist of six to eight families involving adult caregivers and all children over six years of age in the family. Each session follows the same procedures and proceeds through five stages: 1) creating social networks; 2) information exchange; 3) group discussions; 4) individual family practice and; 5) homework assignment. Each group begins with an opportunity for families to interact. Snacks are provided. The informational portion of the group lasts approximately 30 minutes. Next, the remainder of the time is divided equally between group discussions, family practice exercises and explanation of the homework assignment (Tolan & McKay, 1996).
Content of the MFG focuses on helping families to strengthen four aspects of family life that have been empirically linked to childhood behavioral disorders. Specifically, the intervention focuses on the 4 “Rs” of family life: 1) Rules; 2) Responsibilities; 3) Relationships and; 4) Respectful communication. In addition, four specific weeks are devoted to expanding support for parenting and reducing stressors (see Tables 1 and 2).
Multiple Family Group Delivery
At each of the clinics involved in the study, agency administrators and clinical supervisors were enlisted to identify potential MFG facilitators. A group meeting with providers was organized by agency leadership. Training of MFG service providers consisted of group learning and individual teaching modalities at the agency sites. Training consisted of information related to childhood conduct difficulties, family level factors that have been linked to child mental health outcomes, strategies to enhance engagement and motivation, group facilitation skills and processes specific to MFGs. In addition, participating providers reviewed training videotapes and engaged in practice activities and role plays. Providers also received at least two hours per week of ongoing supervision which included on-site supervision and group supervisory conferences across research sites. Approximately 75 providers have been trained thus far.
Fidelity assessments were conducted by independent raters fifteen of the thirty-five MFGs completed thus far. Across sessions, raters indicated 94% fidelity to core intervention content, discussion questions and practice activities.
Description of the Comparison Condition
Standard outpatient care served as the comparison condition of the study. In each of the agencies included in this study, a range of individualized youth treatment, family involved services or family therapy, medication and evaluation services are available. There are some groups being offered, however, they were exclusively child only groups or parent support groups at the clinics. No multiple family groups were offered at any of the research sites other than those offered as part of this study.
Data Collection Procedures and Instruments
Data was collected at baseline, 8 weeks (midway through MFG) posttest (16 weeks), 6, and 18 months following the program. For the current study, we examine preliminary results from the first four waves of assessment (baseline, mid-test, post-test, and 6 month follow-up). We used self-administered questionnaires with read-aloud procedures to address issues of literacy. The study instruments for parents were translated into Spanish using well-accepted procedures for adapting assessment instruments into non-English equivalents (Oquendo et al., 2000).
Instruments
Outcomes
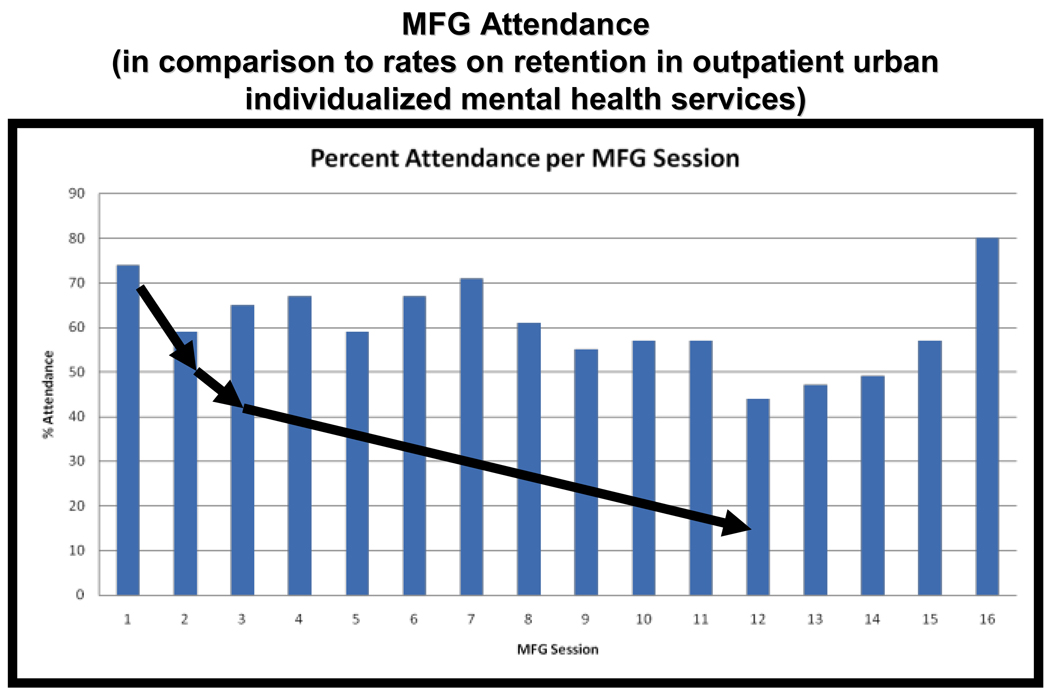
MFG Attendance
Group facilitators indicated whether families attended each session (i.e., “Yes” or “No”). While most participants attended groups lasting 16 sessions, a subset (n = 45) received only 12 sessions due to requests to shorten the intervention by clinic providers. Consequently, the percentage of sessions attended was computed based upon scheduled sessions.
Connors Rating Scale (IA Crs)
The IA Crs measure is a 10 item parent self-report measure of childhood disruptive behavior problems, with subscales assessing for inattentiveness and oppositional behavior (Waschbusch & Willoughby, 2008). For this study, only data from the five item oppositional behavior subscale was be used. Respondents were asked to rate on a 0 to 3 scale (ranging from Not at All to Very Much) how often their child displays these various oppositional behaviors, such as “Defiant” and “Quarrelsome.” Possible scores range from 0 to 15, with higher scores indicating greater levels of child disruptive behavior. Cronbach alphas for baseline, mid-test, post-test and six month follow-up are, respectively, .80, .83, .86 and .88.
Parent Outcomes
Parent Stress Index (PSI)
The PSI is a 36 item, parent self-report measure of parenting stress and social isolation. Five subscales exist within this measure, including: parental distress, parent-child dysfunctional interaction, difficult child, Haskett childrearing stress and defensive responding (Abidin, 1995). Respondents are asked to rate on a 1 to 5 scale (ranging from Strongly Disagree to Strongly Agree) about how they feel such as, “I don’t enjoy things as I used to” or “My child rarely does things for me that make me feel good.” Possible scores range from 36 to 180 and higher scores indicate higher levels of parenting stress. Cronbach alphas for baseline, mid-test, post-test and six month follow-up are, respectively, .91, .92, .94, and .94.
Data Analysis
Random coefficient modeling was performed on data related to child oppositional behavior and parenting stress over time using the SuperMix program for mixed effects regression models (Hedeker, Gibbons, du Toit, & Cheng, 2008). Time was modeled as months from baseline using measurements from 4 time points: baseline, mid-test (mid-way through intervention), post-test (following intervention), and 6 month follow-up. Maximum Likelihood Estimation was utilized to compute model measurements over time within cases. For the current study, participants were nested by the hierarchies of their individual ID, with time treated as a random effect. Also known as hierarchical linear modeling or multilevel linear modeling, this form of analysis: (1) allows parameters (intercepts and slopes) for measurements over time within cases to vary between cases, (2) accounts for correlation between measurements within cases, (3) allows for different times and numbers of measurements within people, which is appropriate for modeling longitudinal change involving data where there is attrition over time, and (4) assumes the missing data is ignorable (i.e., at least missing at random), which is a reasonable assumption with this data.
In order to test differences in child oppositional behavior and parenting stress index between control and experimental group participants, a dichotomous variable for group (experimental vs. control) was included in the full model predicting each outcome. In addition, product terms for group were multiplied by time (i.e. months from baseline) to test whether there was a significant difference (interaction effect) between the groups regarding outcomes. Intercepts were allowed to vary randomly within each model, further enabling calculation of the intra-class correlation coefficient (ICC), a measure of the percentage of variance between people compared to the total variance.
Results
Preliminary results are summarized in Figures 1, 2 and 3 and Tables 4 and 5 presented next. First, Figure 1 already published in McKay et al., 2010 summarizes rates of attendance for MFG participants relative to families enrolled in standard care comparison group. Notably, 80% of families brought their children to the last MFG session (at 4 months following the beginning of the MFG service).
Figure 1.
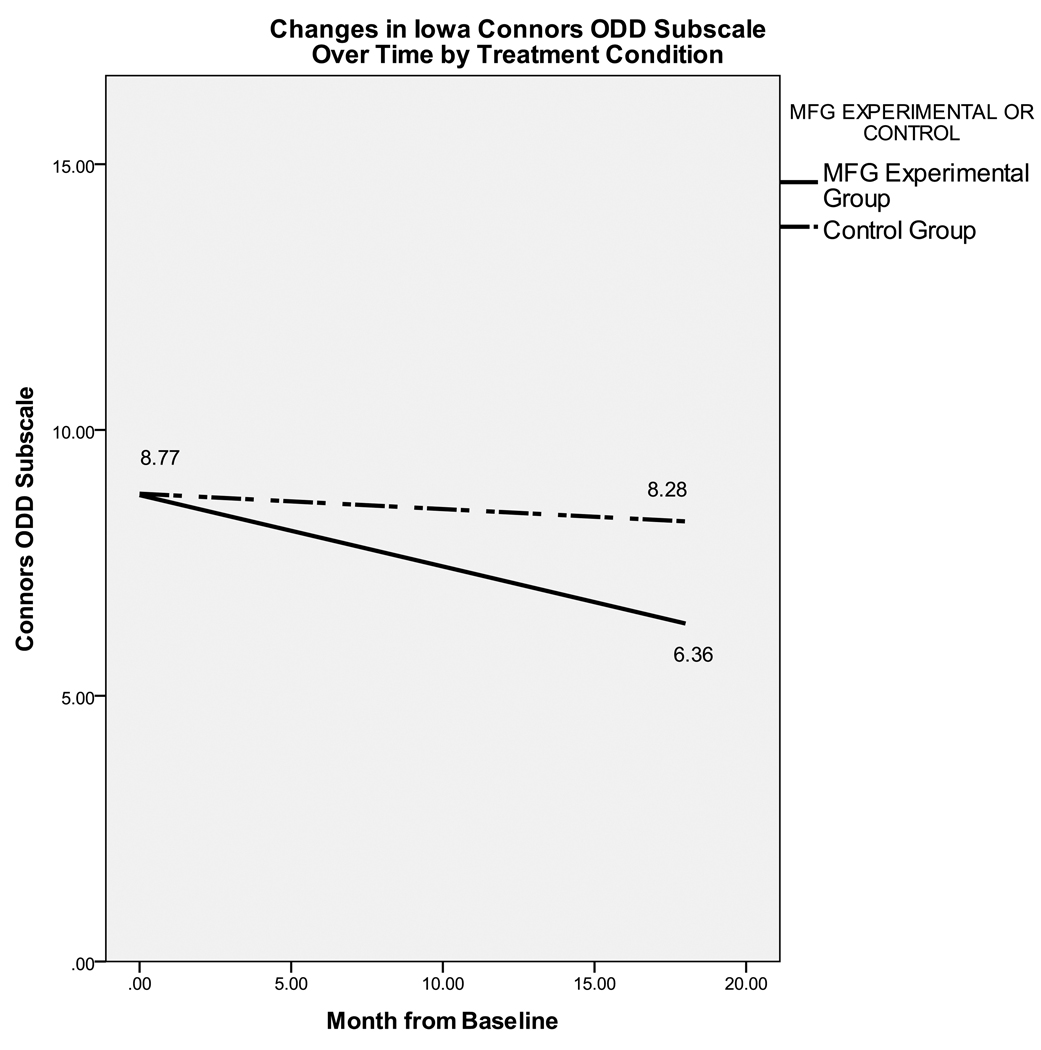
Figure 2.
Multivariate analyses comparing Child Oppositional Behavior over time by treatment group
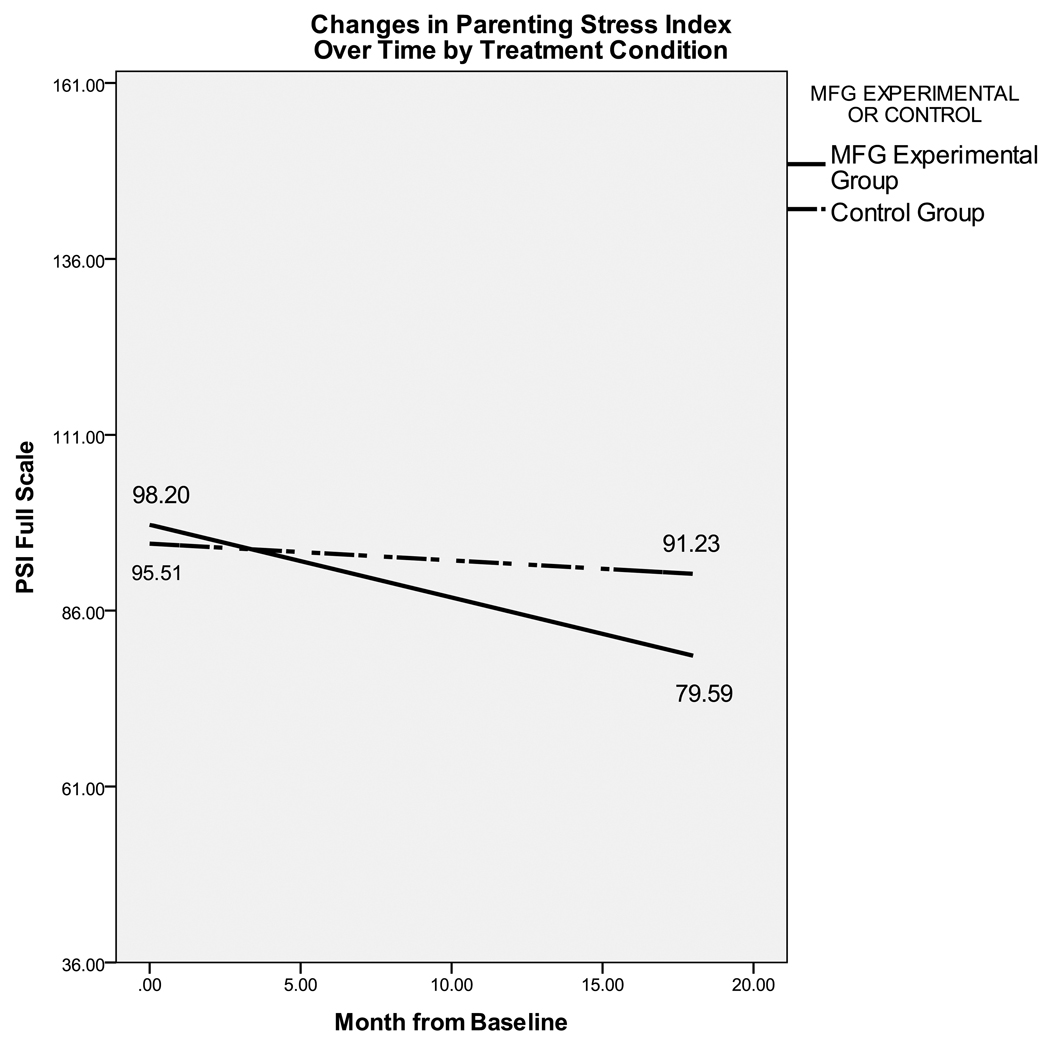
Figure 3.
Multivariate analyses comparing Parenting Stress over time by treatment group
Table 4.
Multivariate analyses comparing Child Oppositional Behavior over time by treatment group
| Variable | β | SE | Z | p-value |
|---|---|---|---|---|
| intercept | 8.77 | 0.22 | 39.87 | 0.00 ** |
| Treatmenta | 0.03 | 0.40 | 0.07 | 0.95 |
| Time | -0.13 | 0.03 | -4.82 | 0.00 ** |
| Treatment X Time | 0.11 | 0.05 | 1.97 | 0.049 * |
p < .01
p < .05
Treatment Group indicator: 0 = Experimental, 1 = Services as Usual
Table 5.
Multivariate analyses comparing Parenting Stress over time by treatment group
| Variable | β | SE | Z | p-value |
|---|---|---|---|---|
| intercept | 98.20 | 1.49 | 65.96 | 0.00 ** |
| Treatment | −2.69 | 2.68 | −1.00 | 0.31 |
| Time | −1.03 | 0.15 | −6.79 | 0.00 ** |
| Treatment X Time | 0.80 | 0.29 | 2.76 | 0.006 ** |
p < .01
p < .05
Treatment Group indicator: 0 = Experimental, 1 = Services as Usual
Next, Table 4 and Figure 2 summarize preliminary multivariate results comparing child oppositional defiant symptoms over time by treatment condition.
The coefficient for Treatment (0 = Experimental, 1 = Services as usual), is not significant, indicating at time = 0 (i.e. baseline) there are no statistically significant differences between treatment groups (β = 0.03, SE = .40, p = .95). Moreover, as seen in Table 4, there is a significant interaction between treatment and time for child oppositional behavior. This suggests that participants in the experimental condition improved in terms of child oppositional behavior at a significantly different rate than those in the comparison condition (β = 0.11, SE = 0.05, p = .049). At the 6 month follow-up (approximately 10 months from baseline), the corresponding effect size is d = .29. As seen in Figure 1, there is little if any change in ODD symptoms for participants in the comparison condition while substantial decrease for experimental group participants. Post-hoc analyses of overall means confirms that there is little change in ODD symptoms from baseline (Mean = 8.99, SD = 3.71) to follow-up (Mean = 8.30, SD = 4.15) for control group participants, while there is substantial drop in ODD symptoms from baseline (Mean = 9.32, SD = 3.35) to follow-up (Mean = 7.45, SD = 3.91).
Similarly, Table 5 (see Figure 3 for graphic display) also indicates that the coefficient for Treatment is not significant (β = −2.69, SE = 2.68, p = .32), indicating that at baseline, the amount of caregiver-reported parenting stress is not significantly different between the treatment groups. There is a significant difference in the rate at which parenting stress decreases between treatment groups over time (β = 0.80, SE = 0.29, p = .006). At the 6 month follow-up (approximately 10 months from baseline), the corresponding effect size is d = .22. Figure 2 indicates that participants in the experimental group manifest a greater decrease in parenting stress over time than comparison group participants. Post-hoc analyses of overall means further indicates that a greater decrease in parenting stress from baseline (Mean = 100.17, SD = 22.98) to follow-up (Mean = 86.53, SD = 25.83) for experimental group participants, than the decrease from baseline (Mean = 95.33, SD = 21.38) to follow-up (Mean = 89.05, SD = 24.58) for comparison group participants.
Discussion and Implications
The multiple family group is a family-centered, group delivered, evidence-informed service delivery approach that has been designed based upon research related to factors that impact the engagement and retention of children and families, specifically: 1) seeking services is often associated with stigma (Alvidrez, 1999; McKay et al., 2001); 2) parents of children with mental health difficulties have reported fears of being blamed for their child’s problems and these fears may in turn influence decisions to continue in services over time (McKay et al., 1996), and; 3) mutual support and normalization of family struggles with child mental health needs could create more receptivity to treatment and potentially offer encouragement for family-level change needed to reduce child disruptive behavioral difficulties (Brannan et al., 2003; Koren et al., 1997).
Further, the MFG capitalizes on: 1) empirically supported, family-focused approaches consistently associated with reductions in child disruptive behavior (Bank et al., 1991; Kumpfer & Alvarado, 2003; Webster-Stratton, 1985; 1990; Sexton & Alexander, 2002); 2) a protocol driven approach that has been developed with maximum input from youth, adult caregivers and providers and successfully implemented by “real world” service providers across a diverse array of outpatient clinic settings (McKay et al., in press; McKay et al., 1998; McKay, Harrison et al., 2001) and; 3) accumulated data supporting an association between MFG service involvement and improvements in engagement and child/family-level outcomes (McKay et al., in press; Fristad et al., 2003; 2002; McKay, Harrison et al., 2001; McKay, Quintana et al., 1998; Stone & McKay, 1996).
Finally, the MFG service delivery model has been specifically designed to target a set of weakness, namely insufficient capacity and high inefficiency within the current delivery system (Atkins et al., in press; Atkins et al., 2004; McKay et al., 2004). Even the current number of children and their families approaching the public mental health service system far outstrips the availability of services and the number of service providers. It is not unusual for waiting lists for care within communities across the US to extend for months (Brown et al., 2002). Thus, MFGs are meant to specifically expand opportunities to receive care within provider organizations that struggle with service capacity and adequate levels of funding and which also have no reasonable expectation for additional resources to expand service slots in the near term.
Acknowledgments
Funding from R01 MH072649 (PI: McKay) and F32 MH090614 (PI: Gopalan) is gratefully acknowledged. In addition, the significant contributions of the members of the multiple family group collaborative working group, including parents, parent advocates, child mental health providers and research staff are also recognized.
Footnotes
This study was previously presented at the Stockholm Conference on Outcome Studies of Social, Behavioral, and Educational Interventions, on February 8th, 2011. It was invited and accepted at the discretion of the Editor.
References
- Alexander JF, Robbins MS, Sexton TL. Family-based interventions with older, at-risk youth: From promise to proof to practice. Journal of Primary Prevention. 2000;21:185–206. [Google Scholar]
- Anderson CM, Griffin S, Rossi A, Pagonis I, et al. A comparative study of the impact of education vs. process groups for families of patients with affective disorders. Family Process. 1986;25:185–205. doi: 10.1111/j.1545-5300.1986.00185.x. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. The epidemiology of disorders of conduct: Nosological issues and comorbidity. In: Hill J, Maughan B, editors. Conduct disorders in childhood and adolescence. New York: Cambridge University Press; 2001. pp. 126–168. [Google Scholar]
- Aponte HJ, Zarski J, Bixenstene C, Cibik P. Home/community based services: A two-tier approach. American Journal of Orthopsychiatry. 1991;61:403–408. doi: 10.1037/h0079270. [DOI] [PubMed] [Google Scholar]
- Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events, and adjustment in urban elementary-school children. Journal of Clinical Child Psychology. 1994;23:391–400. [Google Scholar]
- Boyd-Franklin N. Black families. In: Walsh F, editor. Normal family process. New York: Guilford Press; 1993. pp. 361–376. [Google Scholar]
- Brown AW. The state of mental health services for children and adolescents: An examination of programs, practices and policies. In: Miller SD, editor. Disability and the black community. New York: Haworth Press; 2002. pp. 139–153. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1275–1293. doi: 10.1097/00004583-200211000-00009. [DOI] [PubMed] [Google Scholar]
- Caldwell C, Horne A, Davidson B, Quinn W. Effectiveness of a multiple family group intervention for juvenile first offenders in reducing parent stress. Child-Family Studies. 2007;16:443–459. [Google Scholar]
- Cassano DR. The multi-family therapy group: Research on patterns of interaction -Part II. Social Work with Groups. 1989;12:15–39. [Google Scholar]
- Copeland D, Harbaugh BL. Differences in parenting stress between married and single first time mothers at six to eight weeks after birth. Issues in Comprehensive Pediatric Nursing. 2005;28:139–152. doi: 10.1080/01460860500227556. [DOI] [PubMed] [Google Scholar]
- Crnic KA, Low C. Everyday stresses and parenting. In: Bornstein M, editor. Handbook of parenting: Practical issues in parenting. Mahwah, NJ: Erlbaum; 2002. pp. 243–267. [Google Scholar]
- Deater-Deckard K. Parenting stress. New Haven: Yale University Press; 2004. [Google Scholar]
- Dishion TJ, French DC, Patterson GR. The development and ecology of antisocial behavior. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Vol. 2: Risk, disorder, and adaptation. Oxford, England: John Wiley & Sons; 1995. pp. 421–471. [Google Scholar]
- Dyck DG, Hendryx MS, Short RA, Voss WD, McFarlane WR. Service use among patients with schizophrenia in psychoeducational multiple-family group treatment. Psychiatric Services. 2002;53:749–754. doi: 10.1176/appi.ps.53.6.749. [DOI] [PubMed] [Google Scholar]
- Dyck DG, Short RA, Hendryx MS, Norell D, Myers M, Patterson T, McDonell MG, Voss WD, McFarlane WR. Management of negative symptoms among patients with schizophrenia attending multiple-family groups. Psychiatric Services. 2000;51:513–519. doi: 10.1176/appi.ps.51.4.513. [DOI] [PubMed] [Google Scholar]
- Foster EM, Jones DE. The high cost of aggression: Public expenditures resulting from conduct disorder. American Journal of Public Health. 2005;95:1767–1772. doi: 10.2105/AJPH.2004.061424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frick PJ. Conduct disorders and severe antisocial behavior. New York: Plenum Press; 1998. [Google Scholar]
- Frick PJ, Muñoz L. Oppositional defiant disorder and conduct disorder. In: Essau CA, editor. Child and adolescent psychopathology: Theoretical and clinical implications. New York: Routledge/Taylor & Francis Group; 2006. pp. 26–51. [Google Scholar]
- Fristad MA, Gavazzi SM, Mackinaw-Koons B. Family psychoeducation: An adjunctive intervention for children with bipolar disorder. Biological Psychiatry. 2003;53:1000–1008. doi: 10.1016/s0006-3223(03)00186-0. [DOI] [PubMed] [Google Scholar]
- Fristad MA, Goldberg-Arnold JS, Gavazzi SM. Multifamily psychoeducation groups (MFPG) for families of children with bipolar disorder. Bipolar Disorders. 2002;4:254–262. doi: 10.1034/j.1399-5618.2002.09073.x. [DOI] [PubMed] [Google Scholar]
- Franco LM, Dean-Assael KM, McKay MM. Multiple family groups to reduce youth behavioral difficulties. In: LeCroy C, editor. Handbook of Evidence-Based Child and Adolescent Treatment Manuals. New York: Oxford University Press; 2008. pp. 546–590. [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. American Journal of Psychiatry. 2005;162:1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Goldstein MJ, Miklowitz DJ. The effectiveness of psychoeducational family therapy in the treatment of schizophrenic disorders. Journal of Marital and Family Therapy. 1995;21:361–376. [Google Scholar]
- Gopalan G, Franco LM. Multiple family groups to reduce disruptive behaviors. In: Gitterman A, Salmon R, editors. Encyclopedia of Social Work with Groups. New York: Haworth Press; 2008. [Google Scholar]
- Gorman-Smith D, Tolan PH, Henry D. The relation of community and family to risk among urban poor adolescents. In: Cohen P, Slomkowski C, et al., editors. Historical and geographical influences on psychopathology. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 1999. pp. 349–367. [Google Scholar]
- Gorman-Smith D, Tolan PH, Henry D, Florsheim P. Patterns of family functioning and adolescent outcomes among urban African American and Mexican American families. Journal of Family Psychology. 2000;14:436–457. doi: 10.1037//0893-3200.14.3.436. [DOI] [PubMed] [Google Scholar]
- Grant KE, McCormick A, Poindexter L, Simpkins T, Janda CM, Thomas KJ, Taylor J. Exposure to violence and parenting as mediators between poverty and psychological symptoms in urban African American adolescents. Journal of Adolescence. 2005;28:507–521. doi: 10.1016/j.adolescence.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Gritzer PH, Okun HS. Multiple family group therapy. In: Wolman BB, Stricker G, editors. Handbook of Family and Marital Therapy. New York: Plenum Press; 1983. pp. 315–342. [Google Scholar]
- Gutman LM, McLoyd VC, Tokoyawa T. Financial strain, neighborhood stress, parenting behaviors, and adolescent adjustment in urban African American families. Journal of Research on Adolescence. 2005;15:425–449. [Google Scholar]
- Hess LE, Atkins MS. Victims and aggressors at school: Teacher, self, and peer perceptions of psychosocial functioning. Applied Developmental Science. 1999;2:75–89. [Google Scholar]
- Hogarty GE, Anderson CM, Reiss DJ, Kornblith SJ, et al. Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia: II. Two-year effects of a controlled study on relapse and adjustment. Archives of General Psychiatry. 1991;48:340–347. doi: 10.1001/archpsyc.1991.01810280056008. [DOI] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among US children: Variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Conduct disorders in childhood and adolescence. 2nd edition. Thousand Oaks, CA: Sage Publications, Inc.; 1995. [Google Scholar]
- Kazdin AE, Whitley MK. Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. Journal of Consulting and Clinical Psychology. 2003;71:504–515. doi: 10.1037/0022-006x.71.3.504. [DOI] [PubMed] [Google Scholar]
- Keiley MK. Attachment and affect regulation: A framework for family treatment of conduct disorder. Family Processes. 2002;41:477–492. doi: 10.1111/j.1545-5300.2002.41312.x. [DOI] [PubMed] [Google Scholar]
- Kilgore K, Snyder J, Lentz C. The contribution of parental discipline, parental monitoring, and school risk to early-onset conduct problems in African American boys and girls. Developmental Psychology. 2000;36:835–845. doi: 10.1037//0012-1649.36.6.835. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Frick PJ. Etiology of oppositional defiant disorder and conduct disorder: Biological, familial, and environmental factors identified in the development of disruptive behavior disorders. In: Murrihy RC, Kidman AD, Ollendick TH, editors. Clinical handbook of assessing and treating conduct problems in youth. New York: Springer; 2010. pp. 49–76. [Google Scholar]
- Kotchick BA, Dorsey S, Heller L. Predictors of parenting among African American single mothers: Personal and contextual factors. Journal of Marriage and Family. 2005;67:448–460. [Google Scholar]
- Kumpfer KL, Alvarado R. Family strengthening approaches for the prevention of youth problem behaviors. American Psychologist. 2003;58:457–465. doi: 10.1037/0003-066X.58.6-7.457. [DOI] [PubMed] [Google Scholar]
- Lang LR. A multi-family group intervention to facilitate open communication between adopted adolescents and their adoptive parents. Dissertation Abstracts International. 1993;54:1672. [Google Scholar]
- Lemmens GMD, Eisler I, Buysse A, Heene E, Demyttenaere K. The effects on mood of adjunctive single-family and multi-family group therapy in the treatment of hospitalized patients with major depression. Psychotherapy and Psychosomatics. 2009;78:98–105. doi: 10.1159/000201935. [DOI] [PubMed] [Google Scholar]
- Loeber R, Burke JD, Lahey BB, et al. Oppositional defiant and conduct disorder: A review of the past 10 years, part I. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1468–1484. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Lukens E, Thorning H. Psychoeducation and severe mental illness: Implications for social work practice and research. In: Williams J, Ell K, editors. Breakthrough in mental health research. Washington, DC: NASW Press; 1998. [Google Scholar]
- McDonald L, Moberg DP, Brown R, Rodriguez-Espiricueta I, Flores NI, Burke MP, Coover G. After-school multifamily groups: A randomized controlled trial involving low-income, urban, Latino children. Children & Schools. 2006;28:25–34. [Google Scholar]
- McFarlane WR. Multifamily groups in the treatment of severe psychiatric disorders. New York: Guilford Press; 2002. [Google Scholar]
- McKay M, Harrison M, Gonzales J, Kim L, Quintana E. Multiple family groups for urban children with conduct difficulties and their families. Psychiatric Services. 2002;53:1467–1469. doi: 10.1176/appi.ps.53.11.1467. [DOI] [PubMed] [Google Scholar]
- McKay M, Gonzales J, Quintana E, Kim L, Abdul-Alil J. Multiple family groups: An alternative for reducing disruptive behavioral difficulties of urban children. Research on Social Work Practice. 1999;9:414–428. [Google Scholar]
- McKay M, Gonzales J, Stone S, Ryland D, Kohner K. Multiple family therapy groups: A responsive intervention model for inner city families. Social Work with Groups. 1995;18:41–56. [Google Scholar]
- McPherson AV, Lewis KM, Lynn AE, Haskett ME, Behrend TS. Predictors of parenting stress for abusive and nonabusive mothers. Journal of Child and Family Studies. 2009;18:61–69. [Google Scholar]
- Meezan W, O'Keefe M. Evaluating the effectiveness of multifamily group therapy in child abuse and neglect. Research on Social Work Practice. 1998;8:330–353. [Google Scholar]
- Misri S, Reebye P, Milis L, Shah S. The impact of treatment intervention of parenting stress in postpartum depressed mothers: A prospective study. American Journal of Orthopsychiatry. 2006;76:115–119. doi: 10.1037/0002-9432.76.1.115. [DOI] [PubMed] [Google Scholar]
- Morgan J, Robinson D, Aldridge J. Parenting stress and externalizing child behavior. Child and Family Social Work. 2002;7:219–225. [Google Scholar]
- National Institute of Mental Health. Blueprint for Change: Research on Child and Adolescent Mental Health. Rockville, MD: U.S. Department of Health and Human Services Administration, Center for Mental Health Services, National Institutes of health, National Institute of Mental Health; 2001. [Google Scholar]
- Ostberg M, Hagekull B. A structural modeling approach to the understanding of parenting stress. Journal of Clinical Child Psychology. 2000;29:615–625. doi: 10.1207/S15374424JCCP2904_13. [DOI] [PubMed] [Google Scholar]
- Padgett DK, Patrick C, Burns BJ, Schlesinger HJ. Women and outpatient mental health services: Use by Black, Hispanic, and White women in a national insured population. Journal of Mental Health Administration. 1994a;21:347–360. doi: 10.1007/BF02521354. [DOI] [PubMed] [Google Scholar]
- Padgett DK, Patrick C, Burns BJ, Schlesinger HJ. Ethnicity and the use of outpatient mental health services in a national insured population. American Journal of Public Health. 1994b;84:222–226. doi: 10.2105/ajph.84.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RM, Zelman AB. An ongoing multifamily group in a women's shelter. American Journal of Orthopsychiatry. 1986;56:120–130. doi: 10.1111/j.1939-0025.1986.tb01548.x. [DOI] [PubMed] [Google Scholar]
- Ringel JS, Sturm R. National estimates of mental health utilization and expenditures for children in 1998. Journal of Behavioral Health Services Research. 2001;28:319–333. doi: 10.1007/BF02287247. [DOI] [PubMed] [Google Scholar]
- Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: A comprehensive review of controlled outcome research. Psychological Bulletin. 1990;108:30–49. doi: 10.1037/0033-2909.108.1.30. [DOI] [PubMed] [Google Scholar]
- Rowe R, Maughan B, Pickles A, Costello E, Angold A. The relationship between DSM-IV oppositional defiant disorder and conduct disorder: Findings from the Great Smoky Mountains Study. Journal of Child Psychology and Psychiatry. 2002;43:365–373. doi: 10.1111/1469-7610.00027. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Vondra JI, Hommerding KD, Keenan K, Dunn M. Chronic family adversity and early child behavior problems: A longitudinal study of low income families. Journal of Child Psychology and Psychiatry. 1994;35:1109–1122. doi: 10.1111/j.1469-7610.1994.tb01812.x. [DOI] [PubMed] [Google Scholar]
- Sheinkopf SJ, Lester BM, LaGasse LL, Seifer R, Bauer CR, Shankaran S, et al. Interactions between maternal characteristics and neonatal behavior in the prediction of parenting stress and perception of infant temperament. Journal of Pediatric Psychology. 2006;31:27–40. doi: 10.1093/jpepsy/jsj026. [DOI] [PubMed] [Google Scholar]
- Steinglass P. Multiple family discussion groups for patients with chronic medical illness. Families, Systems, & Health. 1998;16:55–70. [Google Scholar]
- U.S. Department of Health and Human Services. The National Survey of Children’s Health 2007. Rockville, Maryland: U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau; 2010. [Google Scholar]
- U.S. Public Health Service. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: Department of Health and Human Services; 2000. [Google Scholar]
- U.S. Public Health Service. Youth Violence: A report of the surgeon general. Washington, DC: Department of Health and Human Services; 2001. [Google Scholar]
- Wahler RG, Dumas JE. Attentional problems in dysfunctional mother-child interactions: an interbehavioral model. Psycholical Bulletin. 1989;105:116–130. doi: 10.1037/0033-2909.105.1.116. [DOI] [PubMed] [Google Scholar]
- Weist MD, Acosta OM, Youngstrom EA. Predictors of violence exposure among inner-city youth. Journal of Clinical Child Psychology. 2001;30:187–198. doi: 10.1207/S15374424JCCP3002_6. [DOI] [PubMed] [Google Scholar]
- Wermuth L, Scheidt S. Enlisting family support in drug treatment. Family Process. 1986;25:25–33. doi: 10.1111/j.1545-5300.1986.00025.x. [DOI] [PubMed] [Google Scholar]