Abstract
Aims: This is a Stage I open pilot to develop a new intervention, Mentorship for Alcohol Problems (MAP), for individuals with alcohol-use disorders in community treatment programs. Methods: Ten mentors participated for 6 months until 30 mentees received MAP for 12 weeks. Behavioral and biological measures were conducted in addition to fidelity measures. Four focus groups were held with participants and clinician feedback surveys were completed. Results: Feasibility and acceptance data in the domains of patient interest, safety and satisfaction were promising. Mentees reduced their alcohol and substance use and the majority of mentors sustained abstinence. Fidelity measures indicated that mentors adhered to the delivery of treatment. Conclusion: MAP shows promise to be incorporated into professionally run outpatient alcohol treatment programs to assist in the reduction of alcohol and substance use.
Peer mentorship to treat alcohol-use disorders has been widely utilized in 12 step sponsorship programs and therapeutic communities with positive outcomes (Azrin et al., 1982; Miller et al., 1999; Meyers and Miller, 2001). More recently, it has been utilized successfully through many recovery initiatives within clinics to assist treatment (Smith Meyers and Miller, 2001). However, within this recent surge of interest, less attention has been paid to formalizing and testing peer mentorship programs to develop a standardized treatment that could be utilized broadly across treatment programs (Walters, 2002; Harris et al., 2003;Tracy et al., 2010).
The foundation for the utilization of peer mentorship in the treatment of alcohol and substance use disorders is rooted within the Community Reinforcement Approach (CRA). CRA has demonstrated the importance of valued social roles in maintaining abstinence (Hunt and Azrin, 1983; Meyers and Smith, 1995). Having a relationship based on abstinence not only provides reinforcement for the mentee who often has limited relationships outside of those based on alcohol/substance use in early recovery, but also provides a valued social position for the mentor who is seen as a role model to help achieve and sustain abstinence.
We implemented a Stage I pilot to develop a new intervention, Mentorship for Alcohol Problems (MAP), for individuals with alcohol-use disorders in community treatment programs by pilot/feasibility testing, manual writing, training program development and adherence/competence measure construction. This work was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (R01AA016160).
METHODS
In an uncontrolled pilot of MAP, 10 mentors participated for 6 months until 30 mentees received MAP for 12 weeks. Participants were recruited from the Alcohol Dependency Clinic (ADC) at Bellevue Hospital Center. The ADC provides outpatient alcohol/substance abuse treatment for individuals who abuse alcohol and a wide range of other substances. It has over 10,000 visits annually and offers outpatient group therapy and counseling, while maintaining close ties to other community programs and the Bellevue Hospital Shelter for referrals and comprehensive treatment.
Mentors met the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) diagnosis for alcohol abuse or dependence and were 6 months abstinent from alcohol and other substances documented through treatment. Mentees met the same criteria, but were actively using alcohol. Treatment was delivered in two cohorts. Within each cohort, a pool of five available mentors was formed and engaged in individual and group mentoring activities until 15 mentees who were newly admitted to the alcohol treatment facility had participated in MAP for 12 weeks. Mentees were assigned mentors during the first 3 months of alcohol treatment when vulnerability to relapse and drop out is high. Mentors are not paid for providing this support. Where possible, mentorship pairs were same gender; however, when mentorship load became a concern, on occasion pairs were not the same gender in order to permit work load being equally distributed across mentors. Behavioral and biological measures were conducted at baseline, weekly, monthly and termination of the pilot for both mentors and mentees. Adherence and competence measures were constructed and delivered throughout the treatment. Four focus groups were held with MAP participants and clinician feedback surveys were completed with each of the participant's clinicians to obtain satisfaction and additional feasibility data on the intervention. This study was approved by the governing institution's human subjects review board prior to the initiation of the project. MAP has four key components: (a) Mentorship Training, (b) Weekly Mentorship Group, (c) Individual Pair Contact and (c) Supervision. We developed a working manual for MAP and adherence/competence measures based on concepts of social learning theory which was implemented in the pilot. The main focus of the mentoring is the development of a relationship based on abstinence by building rapport. The mentor helps the mentee to develop and achieve abstinence goals using harm reduction strategies which are monitored through modified goal attainment scaling (GAS) (Kiresuk and Sherman, 1968; Kiresuk, 1973; Cytrynbaum et al., 1979; Beidel et al., 1983; Shefler et al., 2001). Abstinence goals may include a wide range of goals (e.g. reduction in alcohol use, changing social networks) seen as contributing to the mentees' ability to remain abstinent and achievements and set backs are recognized incrementally corresponding to the GAS ratings as detailed in the manual.
Mentorship training
The Mentorship Training includes the mentors participating in a 4 week training which meets for 1 h two times per week prior to providing mentorship. In the training, they learn the characteristics of being a good mentor and learn to embody these characteristics while working within a structure of GAS. Rather than condensing the training to one day of training, we chose to have potential mentors come twice a week for 4 weeks to begin to allow for a commitment to the process. If individuals are unable to keep these scheduled appointments, it is likely that a similar occurrence would happen when making commitments to the mentee. The potential mentor must attend all trainings. One emergency excuse may occur, but the potential mentor must provide a urine toxicology and breathalyzer sample within 24 h. In addition, we wanted to have an opportunity to obtain bi-weekly breathalyzer and urine toxicology tests to have assurance that we are connecting mentees to a mentor who is abstinent from alcohol and other substances. Any positive result excludes potential mentor from finishing the training and providing mentoring to a mentee.
Mentorship group
The Mentorship Group includes a weekly group that lasts 1 h and is held with the mentors, mentees and supervisory clinician. The groups are designed to provide a framework for the mentors and mentees to further work on issues outside of group in the Individual Mentorship Contacts. Entailed in the group are discussions of development of GAS recovery plans, monthly formal mentee presentations of the progress on these plans and weekly discussions to receive guidance and support from mentors and the other members of the group to achieve goals of these plans. These groups are facilitated by the supervisory clinician in conjunction with the mentors and provide an additional venue for mentors to provide support to mentees as well as another structure for supervision of mentors and the mentorship process. They are based on a progression of role development and change supported by comradeship.
Individual mentorship contact
Individual Mentorship Contact consists of the mentor working with the mentee outside of the treatment setting to provide a supportive relationship to the mentee and prepare the mentee's GAS recovery plan that aids the mentee in achieving abstinence goals. The goal for the mentor is to attempt to achieve at least 1–4 h of mentoring per week. This may be by phone or in-person contact based on the particular issues surrounding each mentorship pair's availability. In-person individual contacts may include non-substance using social activities (e.g. going for coffee, home visitation, going to the movies, attending family social functions) or treatment-related activities [e.g. attending Alcoholics Anonymous (AA), taking to treatment appointments, assisting with housing searches]. Each week, a contact log form which includes the amount of time spent is submitted prior to the group meeting.
Supervision
Supervision occurs throughout the program to ensure ethical standards are being held. To address any problems which may be occurring, there is a weekly Mentorship Supervisory Group which occurs 1 h prior to the weekly Mentorship Group; informal supervisory interaction during the ongoing weekly Mentorship Group; review of mentorship delivery adherence/competence rating forms; mid-point meetings with the Supervisory Clinician and mentor; and supervision on an ad hoc basis if any problems emerge needing immediate attention.
Adherence competence measures
The following psychotherapy process measures were constructed in the Stage I pilot of MAP to document adherence, competence and critical dimensions of the behavior change process: (a) Mentorship Adherence and Competence Scale (MACS), (b) Mentorship Contact Log (MCL), (c) Mentor Rating Scale (MRS)—Mentor and Mentee Versions, (d) Mentor Supervisory Review (MSR).
The MACS was utilized to rate the adherence and competence of the mentor's delivery of MAP during the tape recorded Introductory Mentorship Pair Meeting. The MACS was modified and adapted for MAP from the Yale Adherence and Competence Scale (Carroll et al., 2000). There are 14 items in the scale resulting from the rating of 7 items for both adherence and competence of the mentor's delivery of the MAP treatment using a likert scale from 1 (not at all) to 5 (extensively).
The MCL is used to record the mentors/mentees contact outside of the group. It captures the date of contact, type, location, amount of time spent and contents. It was completed weekly throughout the treatment.
The third form of fidelity measures, the MRS, was developed from modifying a validated mentorship scale utilized in therapeutic communities for assessment within MAP (Guida et al., 2002). It has 28 items and asks the rater to indicate with a 4-point likert scale how much they agree with statements related to the mentor's delivery of MAP treatment in the following areas: MAP activities, ability to rely on mentor, role modeling and awareness of alcohol/substance use and actions. It was completed by both the mentor and mentee weekly throughout treatment.
The MSR has 17 items and asks the supervisor to indicate with a 4-point likert scale how much they agree with statements related to variables that are thought to contribute to a successful mentoring: communication and impact of actions, initiator, motivator for abstinence and emotional control. This scale was adapted from a validated instrument for rating the delivery of mentorship treatment with alcohol/substance abuse populations within therapeutic communities (Guida et al., 2002). Initially it was completed beginning, mid, and end of the study to isolate the most useful time to deliver scale during the pilot treatment.
FINDINGS
The MAP feasibility and acceptance data in the domains of patient interest, safety and satisfaction for both mentors and mentees were very promising. In addition, participants in MAP showed a reduction in alcohol and substance use.
Participants
Sixty-seven patients were approached to be in the program and 52 (78%) patients signed informed consent with 40 (77%) participants entering the study. Patients who did not proceed further in the process were excluded due to not meeting the entry criteria for the study. Fifteen (38%) of the participants were females. Sixteen participants (40%) were African American or Black, 15 (38%) White and 9 (22%) Hispanic. Ages ranged from 19 to 70 years with a mean of 50.3, SD = 9.97. Table 1 presents a comparison of demographic and diagnostic variables by mentees and mentors.
Table 1.
Comparison of demographic variables by mentor and mentee
| Mentees (n = 30) | Mentors (n = 10) | |
|---|---|---|
| Gender | ||
| Females | 11 (37%) | 4 (40%) |
| Males | 19 (63%) | 6 (60%) |
| Age | M = 48.9, range 19–70 | M = 54.5, range 48–63 |
| Ethnicity | ||
| African American or Black | 13 (43%) | 3 (30%) |
| Caucasian or White | 11 (37%) | 4 (40%) |
| Latino | 6 (20%) | 3 (30%) |
| Psychiatric disorder | ||
| Mood | 20 (66%) | 9 (90%) |
| Anxiety | 10 (33%) | 2 (20%) |
| Substance use disorder | ||
| Alcohol | 30 (100%) | 10 (100%) |
| Cannabis | 16 (53%) | 5 (50%) |
| Cocaine | 18 (60%) | 7 (70%) |
| Opioid | 13 (43%) | 6 (60%) |
| Homeless | 9 (30%) | 2 (20%) |
Forty participants (100%) had a diagnosis of past or current alcohol abuse or dependence. All mentors had lifetime diagnoses. Twenty-nine participants (73%) had an alcohol abuse or dependence diagnoses in addition to a co-occurring mood disorder diagnosis and 12 (30%) had a co-occurring anxiety disorder diagnosis. There was a broad range of other substance use disorders, 25 (62%) cocaine, 21 (53%) cannabis, 19 (48%) opioid, 10 (25%) poly, 1 (2%) sedative hypnotics and 1 (2%) other substances.
All participants were enrolled in an outpatient day treatment program that has patients in similar stages of their recovery receiving similar treatment each day. Participants attended relapse prevention groups, cognitive behavioral-based groups, creative arts groups and individual counseling as needed on a daily basis. Within out-patient treatment, on average participants spent the following hours per week in individual treatment with their primary therapist M = 0.83, SD = 0.65, n = 305 and with any other therapist M = 0.29, SD = 0.23, n = 48. In addition, participants spent the following hours per week in group treatment within the clinic M = 12.9, SD = 2.3, n = 277. Participants were permitted to attend AA groups outside of the treatment facility. Due to this being a feasibility pilot, we did not formally assess involvement in AA or other outside the treatment center activities. However, within the pilot some participants indicated that they engaged in AA; so, our future studies will more rigorously measure AA involvement.
Attrition and attendance
Of the 40 participants who entered the study, there were only four who dropped out yielding a 90% retention rate. All drop outs were mentees. Of those who dropped out two relapsed and were lost to follow-up, one moved out of state and another was a victim of a crime that left her with injuries and physical limitations which prevented her from participating in the study. We had a high 87% (208) attendance rate to weekly Mentorship Supervisory Groups throughout the mentor's 6-month term and also a high 70% (252) attendance rate to the Mentorship Group, which is very positive and uncommon given the early stages of treatment for mentees.
Safety
There was only one adverse event that occurred in the study and it was not study related. Unanimously, 100% (10) of the mentors trained stated the training helped prepare them adequately for providing mentorship responsibilities in MAP. There were no boundary problems, cultural diversity issues, inappropriate handling of crisis situations or lack of appropriate support regarding sobriety or mental health issues witnessed or reported by participants, clinic staff, other patients or study staff.
Alcohol/substance abuse
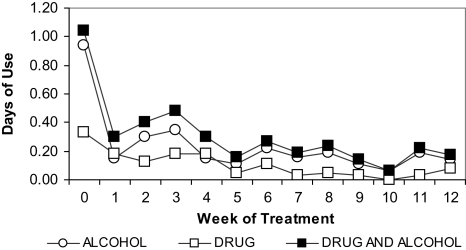
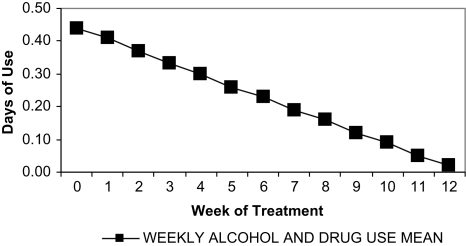
We assessed change in alcohol and drug use with all participants (n = 40) by running random effect regression analyses which indicated that frequency of alcohol use (P < 0.01), drug use (P < 0.01), and both alcohol and drug use (P < 0.01) significantly decreased by week from baseline to week 12 for all participants (see Figs. 1 and 2). All of the mentors remained abstinent from alcohol and drugs throughout their 6-month participation with the exception of one mentor who used alcohol in her 20th week for one day. Her mentee was immediately re-assigned and she was allowed to continue in the study as a mentee. She quickly resumed abstinence which sustained through the end of the study.
Fig. 1.
Days per week of alcohol, drug, drug and alcohol use throughout treatment.
Fig. 2.
HLM mean alcohol and dug use throughout treatment.
Satisfaction and feedback on feasibility
We evaluated participant satisfaction with MAP from the data resulting from the MAP satisfaction assessment collected during the four pilot participant focus groups and the clinician feedback surveys using descriptive statistics.
Focus groups
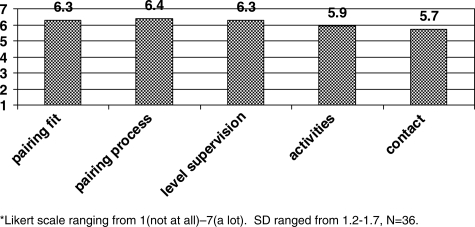
Within the focus groups, there was a strong positive response from the participants regarding the impact of MAP on their lives and its structure. Using a Likert scale from 1 (not at all) to 7(a lot), participants indicated overall that they were very satisfied with MAP (M = 6.25, SD = 1.23, n = 36). Impact on participants—participants also stated MAP helped them to take steps toward becoming or remaining abstinent (M = 6.19, SD = 1.35), managing or reducing psychiatric symptoms (M = 5.22, SD = 2.13), reaching work-related goals (M = 5.94, SD = 1.43), treatment connection (M = 5.97, SD = 1.50) and improved social support networks (M = 6.06, SD = 1.31). Program structure—participants indicated satisfaction with the mentor/mentee pairing being overall ‘good fits’, pair selection process, level of supervision provided, mentorship activities and frequency and quantity of mentorship contact (Fig. 3). In addition, 92% (33) found the GAS process helpful and 89% (32) found the mentorship rating scales to be helpful. About half of the participants, 53% (19), thought the groups were structured enough, with the other half discussing within the focus group a want for more parameters around not letting people into the group after 10 min and not allowing people to leave the group and come back even if they have a legitimate reason. However, they reported being satisfied with the content of the group. In discussing what could be added to the group, 70% (25) indicated that they would like the mentorship contact reviewed at the beginning of the group.
Fig. 3.
Participant satisfaction with map program structure.
Clinician feedback surveys
We also had strong positive feedback on the clinician feedback surveys and a 95% survey completion rate (n = 38) from clinicians whose patients were in the MAP program. The only two that were not able to be completed were from a clinician who left his position and was no longer at the clinic. On a likert scale from 1(not at all) to 7(a lot), clinicians indicated they were overall satisfied with MAP and its interaction with their patient/s (M = 5.8, SD = 1.8) and that MAP provided benefits to their patient/s (M = 5.8, SD = 1.8). Patient impact—additionally, they indicated that MAP helped their patients to remain abstinent from alcohol (M = 5.4, SD = 1.7) and other substances (M = 5.5, SD = 1.6), improved their quality of life (M = 5.3, SD = 1.9) and improved their patient's level of non-substance use social contact (M = 5.4, SD = 1.3), self-efficacy (M = 5.7, SD = 1.2) and coping (M = 5.2, SD = 1.8). Program Structure—In addition, clinicians felt that MAP did not interfere with the treatment they were delivering with the patient/s when asked to indicate the level of interference using the same likert scale (M = 1.7, SD = 1.3).
Adherence competence measures
Mentors adhered to the delivery of the MAP treatment. The overall mean on the MACS was M = 4.36, SD = 0.83, n = 30, adherence M = 4.36, SD = 0.82 and competence M = 4.36, SD = 0.84. We conducted Cronbach's alpha reliability coefficients for the scale which indicated good internal consistency of the items. The coefficient alpha for the full scale of 14 items is 0.98, seven adherence items 0.96, and seven competence items 0.95.
We found the MCL to be reliable between mentor and mentee ratings with a significant Pearson's correlation, r(358) = 0.64, P < 0.01. Utilizing this fidelity measure, we were able to obtain pertinent information regarding the mentorship relationship. On average mentors met the goal in engaging in individual pair mentorship activities at least 1–3 h a week outside of group with mean hours contact M = 1.14, SD = 0.99, n = 720 with a range of contact from 0 to 5 h per week. Approximately 50% of the contacts were in person and 50% over the phone.
Although the MRS scale had positive results in therapeutic communities, we found it to be less useful in an outpatient clinic setting as a fidelity measure. The overall intra-class correlation coefficients for the mentee and mentor ratings was ICC = 0.48. Section I, MAP activities, had the highest agreement between raters ICC = 0.63, and will be retained and utilized in future MAP trials during weekly ratings, because it provides useful information for the Supervisory Clinician on the availability of the mentor. However, the remainding sections appear to be useful from only an investigational standpoint to understand perspectives on the mentorship relationship and its impact on outcome warranting less frequent completion during MAP trials.
We found the last fidelity measure, the MSR to be useful as a base for discussion in the mid point evaluation with the mentors. To test where to best assess the mentor within the process using this measure, we initially attempted to perform this assessment at beginning, mid and end points of the mentor's participation. However, we found that not enough was known about the mentor's ability and style early in the mentoring process to accurately make a beginning assessment. Also, utilizing this assessment later in the mentor's term was not useful for supervisory purposes, because it was at the end of the mentor's providing support to the mentee, so any feedback to improve delivery could not be implemented. In addition, mentors felt they were receiving enough supervision through the supervisory weekly group and ad hoc as needed. They found adding three additional supervisory meetings on top of the mentorship activities already in place and their own treatment made it difficult to orchestrate scheduling. Given the nature of the intervention being peer driven instead of the therapist driven, it is important to not only have the adequate level of fidelity measures, but also to do so in a way that makes our treatment user-friendly and easily adopted in clinical settings.
IN SUM
MAP formalizes client-to-client mentorship relationships as an adjunct to standard outpatient alcohol treatment to aid in the treatment of alcohol-use disorders. It comprises selection, training and supervision procedures to enable successful recovering patients to serve as mentors for clients who are early in the recovery process and is conceived as an optional module that can be incorporated into professionally run outpatient treatment programs based on a wide range of treatment philosophies.
The MAP feasibility and acceptance data in the domains of patient interest, safety and satisfaction for both mentors and mentees were very promising. Patient interest was high demonstrated by high agreement to participate in the study, low attrition and high attendance rates. There were no reported problems within the program regarding boundaries or inappropriate interactions between mentors and mentees and no adverse events related to the study. Mentees who were newly admitted patients with alcohol-use disorders, who typically are vulnerable to relapsing at high rates so early in treatment, reduced their alcohol and substance use during their participation in MAP. In addition, mentors maintained abstinence from alcohol and other substances with only one relapse where abstinence was quickly achieved and sustained. Both mentors and mentees as well as clinicians within the treatment program where MAP was run reported being satisfied with MAP and the intervention's impact on participants and its program structure with no mean satisfaction rating falling below 5 on a 7-point likert scale with seven indicating highest satisfaction. Also, adherence and competence ratings demonstrated that mentors adhered to guidelines in the delivery of the MAP intervention in a competent manner.
Additionally, MAP appears to be a cost-effective treatment. For limited amounts of clinician time per week, multiple patients receive multiple hours of contact from mentors both within the treatment setting and community. Often contact in the community for formal treatment is limited to crisis management situations that are costly. Within peer mentorship programs, the mentor has the ability to connect with the mentee early when the mentee is struggling with an issue or problem in their setting often circumventing a further decline in the mentee's functioning due to lack of support. Because mentors also benefit from the participation, training and supervision can be charged as regular treatment session. Training and supervision provides an additional venue for the mentor to work out any current or past issues. Support is given to help the mentor view him/herself from a position of strength and learn how to manage their triggers to use while interacting with or helping others.
Lastly, MAP is conceived as an augmentation to formal treatment rather than a replacement and is suggested to be delivered simultaneously with formal treatment. We chose delivery within the first few months of treatment when vulnerability to relapse is high to help mentees during this critical time period. However, based on population and clinic needs, alternative time periods could be considered.
In summary, MAP appears to be a feasible treatment that has much promise to assist in the treatment of individuals with alcohol-use disorders. Follow-up studies including a larger sample size utilizing a randomized trial are needed to further substantiate results from this pilot.
Funding
This work was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (R01AA016160).
Acknowledgements
We mourn the loss of Dr Bruce Rounsaville, a true mentor and friend whose contributions made this work possible.
REFERENCES
- Azrin NH, Sisson RW, Meyers R, et al. Alcoholism treatment by disulfiram and community reinforcement therapy. J Behav Ther Exp Psychiat. 1982;13:105–12. doi: 10.1016/0005-7916(82)90050-7. [DOI] [PubMed] [Google Scholar]
- Beidel D, Turner SM, Bellack AS, et al. Using the goal attainment scale to measure treatment outcome in schizophrenia. Int J Partial Hosp. 1983;2:33–41. [Google Scholar]
- Carroll KM, Nich C, Sifry RL, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–38. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Cytrynbaum S, Ginath Y, Birdwell J, et al. Goal attainment scaling: a critical review. Eval Q. 1979;3:5–40. [Google Scholar]
- Guida F, De Leon G, Monahan K. 2002. Measuring peer interaction in the Therapeutic Community. Paper presented at the American Psychological Association Convention. 110th Annual Convention, August 22–25, Chicago, IL. [Google Scholar]
- Harris J, Best D, Gossop M, et al. Prior alcoholics anonymous (AA) affiliation and the acceptability of the twelve steps to patients entering UK statutory addiction treatment. J Stud Alcohol. 2003;64:257–61. doi: 10.15288/jsa.2003.64.257. [DOI] [PubMed] [Google Scholar]
- Hunt GM, Azrin NH. A community-reinforcement approach to alcoholism. Behav Res Ther. 1983;11:91–4. doi: 10.1016/0005-7967(73)90072-7. [DOI] [PubMed] [Google Scholar]
- Kiresuk TJ. Goal attainment scaling at a county mental health service. Eval Monogr. 1973;1:12–8. [Google Scholar]
- Kiresuk TJ, Sherman RE. Goal attainment scaling: a general method for evaluating comprehensive community mental health programs. Community Ment Health J. 1968;4:443–53. doi: 10.1007/BF01530764. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Miller WR. A Community Reinforcement Approach to Addiction Treatment. Cambridge, UK: Cambridge University Press; 2001. [Google Scholar]
- Meyers RJ, Smith JE. Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach. New York, NY: Guilford Press; 1995. [Google Scholar]
- Miller WR, Meyers RJ, Hiller-Sturmhöfel S. The community reinforcement approach. Alcohol Health Res W. 1999;22:116–21. [PMC free article] [PubMed] [Google Scholar]
- Shefler G, Canetti L, Wiseman H. Psychometric properties of goal-attainment scaling in the assessment of Mann's time-limited psychotherapy. J Clin Psychol. 2001;57:971–79. doi: 10.1002/jclp.1063. [DOI] [PubMed] [Google Scholar]
- Smith JE, Meyers RJ, Miller WR. The community reinforcement approach to the treatment of substance use disorders. Am J Addict. 2001;10:51–9. doi: 10.1080/10550490150504137. [DOI] [PubMed] [Google Scholar]
- Tracy K, Burton M, Miescher A, et al. It takes two: teamwork set to improve recovery from alcohol abuse. Int Innov Health. 2010;4:94–6. [Google Scholar]
- Walters GD. Lessons learned from the project MATCH. Addict Disord Treat. 2002;14:135–9. [Google Scholar]