Abstract
Purpose
This study describes the alignment between the need for AAC among a group of young children with cerebral palsy (CP) who had clinical communication disorders and the speech-language goals/objectives being targeted in the IEPs of these children.
Method
22 children with CP who had clinical communication disorders were classified into groups according to their need for AAC based on prospective assessment data. Individualized Education Plans (IEPs) in place at the time of the assessment were analyzed to characterize the type of speech-language goals/objectives being addressed for each child.
Results
95% of children with CP in this sample could benefit from some form of AAC. Among these, 62% had at least some functional speaking ability. Among all children who could benefit from AAC, 57% had AAC-focused speech-language goals/objectives in the IEP. Children who had any functional speaking ability were less likely to have AAC-focused speech language goals/objectives than children who were unable to speak.
Conclusions
Results suggest that a majority of young children with CP and communication disorders would benefit from some form of AAC, however these children seemed to be under-served with regard to AAC interventions, particularly those who had any functional speaking ability. Additional pre-service and in-service training for speech language pathologists and other professional is necessary to ensure that children with CP receive the AAC-focused speech-language services they need.
Keywords: AAC, cerebral palsy, speech-language therapy, early intervention
Children with cerebral palsy (CP) are at considerable risk for communication problems, which can arise from deficits in speech-motor control, cognition, language, sensation / perception, or a combination of these. Recent data from a large population-based sample in Europe indicate that 60% of children with CP have some type of communication problem (Bax et al., 2006); however the exact nature of the communication problems and the functional implications of those problems has not been comprehensively studied. Early intervention to address communication challenges and to prevent communication-related social isolation is critical for maximizing outcomes in children with CP.
Augmentative and alternative communication (AAC) systems and strategies are an important avenue to enhance communication development and social participation for any child who cannot use speech to meet all communication needs (Beukelman & Mirenda, 2005). AAC systems can range from low-tech, involving simple photographs or paper-based communication books and boards, to high-tech, involving sophisticated voice output computers. AAC can play a variety of roles in a child’s communication repertoire and can serve as an important means to support, rather than replace natural speech and language abilities. In this paper, we present a framework for considering the role that AAC can play in the multimodal communication repertoire of children with CP. In this framework, the relationship between AAC and natural speech is conceptualized as a complementary one, with the role of AAC varying based on functional speech capability, considered within the individual communicative contexts of the child’s life. Toward this end, the functionality of speech is considered along with the role that AAC systems and strategies could play to enhance overall communication performance and social participation. Categories of children are as follows:
Category A: Children who are able to meet all communication needs across partners and contexts using speech alone. Speech, language, and communication skills of these children may or may not be “normal”; however, the child is able to use speech to participate at a developmentally appropriate level in his or her life without any compensatory communication strategies.
Category B: Children who can meet most communication needs across partner and settings using speech alone, but have mildly reduced intelligibility and / or speech subsystem involvement that sometimes results in difficulty in adverse communication situations (e.g. competing for the floor in groups, in noisy or reverberant environments, in breakdown situations). These children benefit from AAC as a back-up strategy to supplement speech, and it is used primarily in situations where communication difficulties arise or are expected to arise. Speech is the primary mode of communication for these children; AAC is a secondary, supporting mode.
Category C: Children who can meet some communication needs across partners and contexts using speech alone, but have moderately reduced intelligibility. These children may have speech that is functional with intimately familiar communication partners or in quiet one-on-one situations, but may have difficulty with less familiar partners (i.e. teachers, other children, support staff), or in real-life noisy situations. For these children, preliminary data suggest that as language development advances and length of utterance increases, speech intelligibility tends to decrease (Hustad et al., 2008), likely because the speech motor system is increasingly taxed by the more intensive production demands placed on it. AAC serves as an important support to enhance speech intelligibility for these children and may be used simultaneously with natural speech (Hanson et al., 2004; Hustad et al., 2003a). AAC plays an important role in supporting social participation at school and may even be a primary communication strategy in specific settings where there is less tolerance for communication breakdown. For these children AAC and speech can both be considered primary modes of communication, depending on the partner and the setting.
Category D: Children who can meet few or no communication needs across all partners and contexts using speech alone. These children may be able to produce a few idiosyncratic words or vocalizations that very familiar communication partners can interpret; they also may be able to communicate to some extent using facial expressions, gestures, and vocal intonation, but their communication using these modes is extremely limited. For these children comprehensive AAC systems are necessary for nearly all communication interaction to enable social and educational participation.
At present, there is currently no way to predict which children with CP will develop functional speaking abilities that are sufficient to meet their communication needs across all contexts and settings (Category A), and which children will have difficulty with functional communication without some type of AAC (Categories B, C, D). For children who are at-risk for communication challenges, such as those with CP, Romski and Sevcik (2005) suggest that AAC interventions should be introduced before communication failure occurs, as a means to prevent failure. AAC interventions can provide an important foundation for language development (Romski & Sevcik, 2005), a tool for social participation (Light et al., 2002), and can serve to facilitate development of natural speech (Cress & Marvin, 2003; Hustad et al., 2002; Hustad & Shapley, 2003b; Millar et al., 2006). Thus, even if a child with CP eventually develops speech that is adequate for meeting all communication needs, AAC intervention can have interim educational and developmental benefits.
In the present study, we sought to examine the need for AAC among young children with CP who had clinically diagnosed communication disorders. We also sought to examine how many children with CP were receiving speech-language services targeting AAC systems and strategies. The following specific research questions were addressed:
How many children with CP who have a need for speech and language services also have a need for AAC intervention? For those who could benefit from AAC, what is the nature of the need?
How many children with CP who have a need for AAC intervention have speech-language goals/objectives in the IEP that target AAC? What are the other speech-language goals/objectives being targeted for children who do and do not need AAC?
Are children with particular types of AAC needs more or less likely to receive AAC-focused speech-language services?
Method
Participants
Participants in this study were selected from a cohort of children with CP who were participating in a 4-year prospective longitudinal study of communication development. Criteria for inclusion in the present study required that children with CP: 1.) have a speech and / or language delay or disorder as determined by our research-based speech-language evaluation; 2.) have completed a data collection session at an average age of 54 months (+ / − 6 months); and 3.) have hearing abilities within normal limits as documented by either formal audiological evaluation or distortion product otoacoustic emission screening.
To address our research questions, two sources of data were employed: 1.) research-based assessment data on communication abilities of the children with CP who had a speech and / or language delay or disorder; and 2.) the Individualized Education Plans (IEPs) that were in place at the time of the research-based assessment for each participant.
A total of 26 children from the larger study met inclusion criteria. The mean age across children was 54.3 months (SD 1.9). The sample was comprised of 13 boys and 13 girls. Of the children who met inclusion criteria, IEPs were not available for four children; therefore, those children were excluded from the study. Of the remaining 22 children, 11 were girls and 11 were boys. The mean age of children was 54.3 months (SD 1.9); the mean age at implementation for the IEPs reviewed in this study was 47.0 months (SD 2.2). In addition, children attended school in 18 different districts across the upper-midwest region of the United States. IEPs were written by at least 18 different speech language pathologists.
Procedures and Analyses
Characterizing the communication challenges and needs of children with CP
All children included in this study were seen for research-based speech-language evaluation sessions during the same school year as the IEP that was analyzed for this study. Children were identified as having a speech and / or language delay or disorder if one or more of the following were present: 1.) speech motor involvement as defined by clinically observable evidence of motor impairment affecting musculature of any one or more of the speech subsystems (articulation, phonation, resonation, respiration) that could be perceptually observed at rest, during vegetative movement, during speech, or during feeding; or 2.) language or cognitive involvement as defined by standard scores on one or more language measures that were more than one standard deviation below the mean.1
The need for AAC was determined for each child based on parent responses to questionnaires addressing functional communication in the context of daily life, and based on each child’s observed communication strengths and challenges during parent-child interaction and clinician-child interaction segments of the data collection session. Using expert opinion, data from these sources were triangulated by two different individuals, each with more than 10 years of clinical experience in AAC, and children were assigned to one of the four mutually exclusive functional AAC groups described above. Agreement for classification of children into functional AAC groups between the two expert raters was 95%. Cohen’s Kappa was .93, indicating excellent inter-rater agreement.
Characterizing speech and language services
Speech-language goals/objectives as documented in each child’s IEP were analyzed using a qualitative methodology to identify and code content categories of goals/objectives (Bogdan & Biklen, 1992; Creswell, 2003; McNaughton et al., 2002; McNaughton et al., 2003). The following steps were employed:
All goals/objectives implemented by each child’s speech-language pathologist were located in the IEP and transcribed, verbatim, into a database.
Across all children, goals/objectives were pooled and then each goal/objective was organized into one mutually exclusive category that was established based on within-category conceptual similarities.
Categories were then named based on similarities among goals/objectives.
Operational definitions for each category of goals/objectives were developed and goals/objectives were re-coded into the conceptual categories by the same researcher.
Using the operational definitions, a second researcher was trained to code the goals/objectives, and that researcher then coded all goals/objectives into the operationally defined categories.
The first and second researcher compared and discussed results. Inter-rater coding agreement, defined as the number of categorical agreements divided by agreements plus disagreements, was 79.1%. For each goal/objective where there was a discrepancy in coding between researchers, consensus procedures were used to reach agreement. Operational definitions for goal/objective categories were refined as necessary.
Each of the two researchers then independently recoded all goals/objectives into the categories using the refined operational definitions. Inter-rater agreement, defined as the number of categorical agreements divided by agreements plus disagreements, was 92%. Intra-rater agreement, defined as the number of categorical agreements divided by agreements plus disagreements, was 92%.
From this process, 10 categories of goals/objectives emerged. These were a.) expressive / receptive language; b.) pragmatics / social communication; c.) cognitive development; d.) articulation; e.) motor speech; f.) intelligibility; g.) aided AAC; h.) unaided AAC; i.) oral-motor skills; and j.) miscellaneous. Categories and operational definitions are provided in Table 2.
Table 2.
Operational descriptions of speech-language goal / objective categories obtained from our pilot study.
| Goal area | Operational definition |
|---|---|
| Receptive language | Goals/objective targeting the ability to understand or express spoken language using a verbal (speech) modality. This category includes goals related to expressive or receptive vocabulary, syntax, semantics, and morphology, concepts (e.g. under, more, big), questions, directives, comprehension and production of objects/labels, and classification. Examples include increasing length of utterance, increasing vocabulary (including vocalizations and/or vocal play), telling a sequential/cohesive story, and increasing use or comprehension of grammatical morphemes. Use of aided or unaided AAC is specifically EXCLUDED from this category. All goals in this category imply or directly state that speech is the target modality of expression. |
| Pragmatics / social communication | Goals/objectives targeting the ability to use language (appropriately and functionally) in multiple settings and with a variety of communication partners. This category includes goals that address social communication in some type of meaningful context. Examples include initiating social interactions, participating in group activities, responding appropriately to others in various social settings, engaging in complex play schemes with peers and /or other communication partners, participating in cooperative and/or parallel play, maintaining eye contact, attending to communication partners, and increasing the frequency and duration of social exchanges. This category also includes pragmatic goals, such as sharing relevant information, staying on topic, understanding figurative language, story cohesion, etc. Use of aided or unaided AAC is specifically EXCLUDED from this category. |
| Cognitive development | Goals/objectives targeting the ability to coordinate and use attention, memory, problem solving, and executive functioning skills in various aspects of communication. This category includes goals related to object awareness, object discrimination, development of cause and effect, visual tracking, appropriate play with objects, and consistent response to stimuli and/ or communication partners. Use of aided or unaided AAC is specifically EXCLUDED from this category. |
| Phonology / Articulation | Goals/objectives targeting the ability to produce speech sounds either in isolation or in spoken words or utterances. This category includes goals related to improvement in speech production at the phoneme, syllable, word, sentence, or conversational level. This category may include goals related to increasing the number of phonemes in a repertoire, correct placement of articulators during speech production, and or correct production /approximation of target phonemes in the repertoire. This category may also include goals related to phonological awareness. Goals related to speech intelligibility are specifically EXCLUDED from this category. |
| Motor speech / Speech physiology | Goals/objectives targeting the ability to maintain and control various aspects of respiration, phonation, resonance, and motor planning required for production of speech. Goals in this category differ from oral motor goals in that speech tasks are used to address the problem areas. Goals include improving breath support for speech, reducing hypernasality, increasing loudness, or increasing prosodic variation. Articulation goals and goals that specifically mention intelligibility are EXCLUDED from this category. |
| Intelligibility | Goals/objectives targeting the ability to produce intelligible speech. Goals related to improving overall understandability of speech and those related to consistent production and/or approximations of expressive vocabulary (not target phonemes) are included within this category. Goals that address articulation with the end goal being to improve understandability of productions (rather than to achieve adult-like or perfect productions) are also included. |
| Aided AAC | Goals/objectives targeting the ability to use alternative and/or supplemental communication system(s) to advance functional communication abilities. The use of aided communication modalities other than speech automatically qualifies a goal for inclusion within this category. Examples include low-technology boards, switches, high-technology devices, and other aided communication modalities. Any mention of specific AAC devices or strategies qualifies a goal for inclusion within this category. |
| Unaided AAC | Goals/objectives targeting the ability to use alternative and/or supplemental communication system(s) to advance functional communication abilities. The use of unaided communication modalities other than speech automatically qualifies a goal for inclusion within this category. Examples include facial expression, sign, eye gaze, and gestures. Any mention of specific unaided AAC methods or strategies within a goal qualifies a goal for inclusion within this category; however, any mention of an aided AAC device is specifically EXCLUDED from this category. |
| Oral motor skills | Goals/objectives targeting the ability to develop and/or increase strength, range of motion, sensation, or coordination of oral muscles using non-speech tasks (i.e. tongue exercises, blowing exercises, passive stimulation activities). Goals that mention the use of oral-motor exercises or tolerating different kinds of oral stimulation are included here. Also goals that address blowing, sucking (for non-nutritive purposes), etc. are included here. |
| Miscellaneous | Goals/objectives targeted by speech-language pathologists that are 1) not directly related to any of the other categories; and 2) are included in the speech/language portion of a child’s IEP are included here. Examples include participating in structured learning tasks, imitating activities or actions, increasing vocal play, reducing aversive behaviors. |
Results
Because this study was designed to be descriptive in nature, inferential statistics were not employed. Data reported are based on descriptive statistics (means) and refer to general tendencies within the data.
Need for AAC
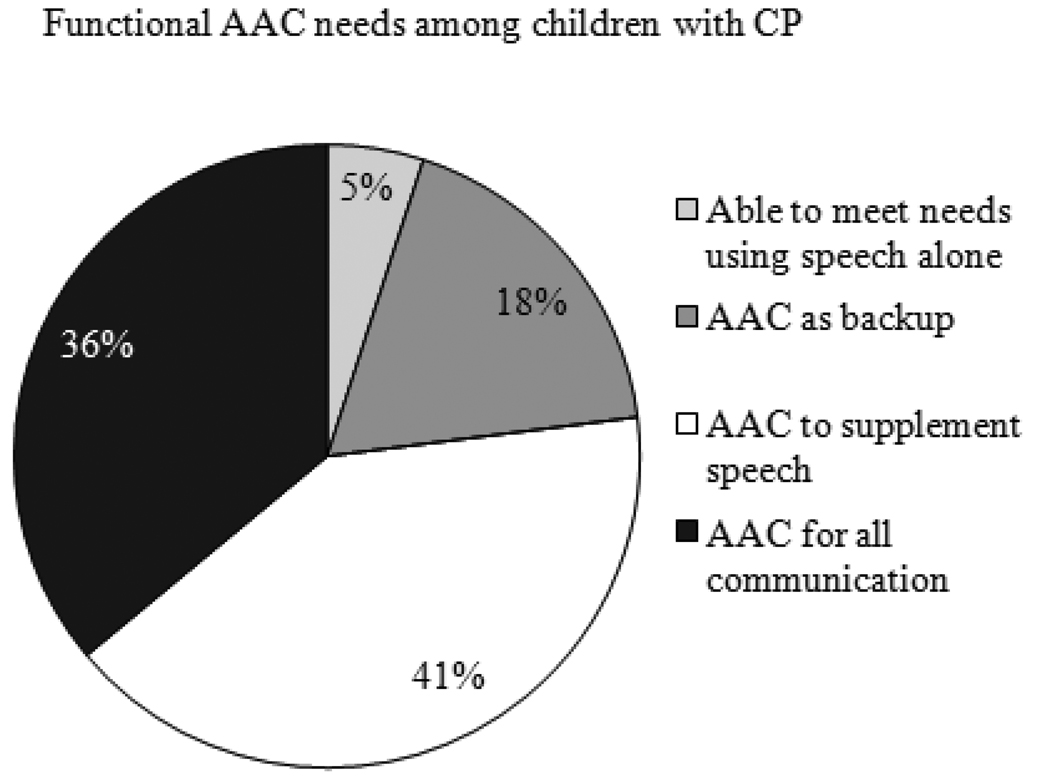
Of the 22 children with CP who had a communication disorder, 21 (95%) were identified as needing some form of AAC, while one child (5%) was able to meet all communication needs using speech alone. In addition, 4 children (18%) could benefit from AAC as a back-up strategy for natural speech (Category B), 9 (41%) could benefit from AAC to supplement or support speech (Category C), and 8 (36%) required AAC for all communication (Category D). See Figure 1.
Figure 1.
Speech-language goals
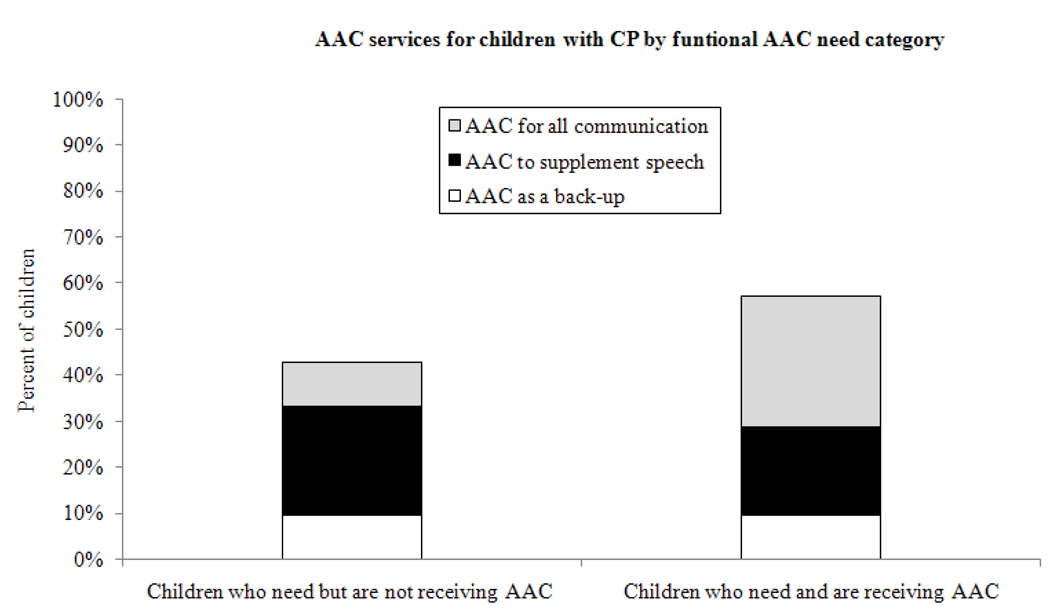
Of the 21 children identified as needing some form of AAC, 12 children (57%) had at least one AAC-focused speech-language goal/objective within their IEPs; 8 children (38%) did not have any AAC-focused speech-language goals/objectives within their IEPs; and 1 child (5%) did not have any speech-language goals/objective identified in the IEP. See Figure 2.
Figure 2.
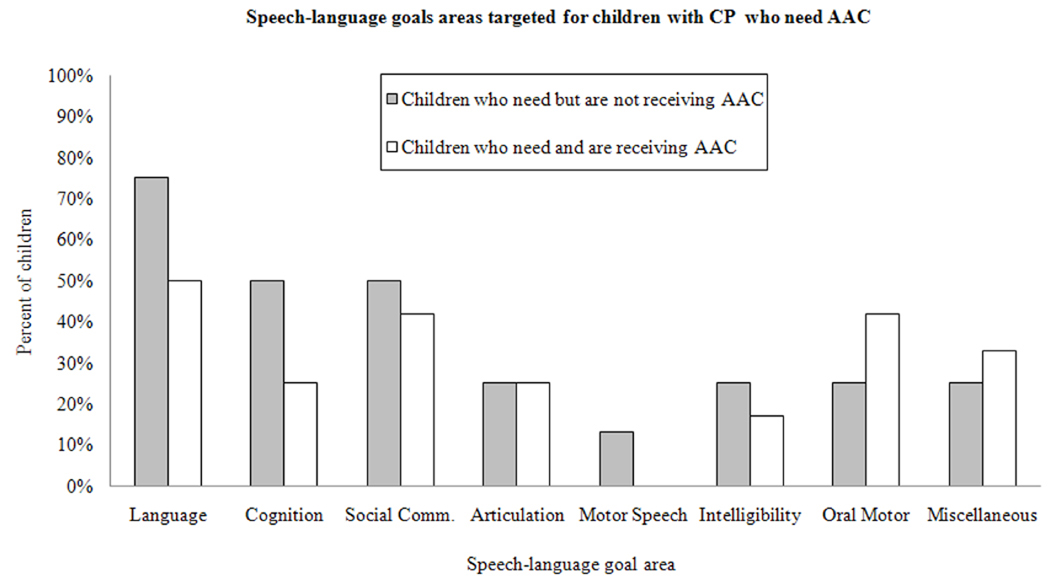
Descriptive findings suggested that there were differences between the children who were and were not receiving AAC intervention with regard to the proportions of children with goals/objectives in the different speech-language categories. In general, a greater percent of children who were not receiving AAC had goals/objectives targeting language development, cognitive development, social communication, speech-motor control, and intelligibility. The percent of children with goals/objectives targeting articulation was the same among children who were and were not receiving AAC. Finally, the percent of goals/objectives targeting oral-motor development and miscellaneous developmental milestones was higher for children who were receiving AAC than for those who were not. See Figure 3.
Figure 3.
Category of AAC need and AAC goals/objectives
When the presence / absence of AAC goals/objectives in the IEP was examined by category of AAC need identified for each child, descriptive data indicated that none of the children who were able to meet all communication needs using speech alone were receiving AAC services. Of the 4 children who could benefit from AAC as a back-up strategy (Category B), 2 (50%) were receiving AAC services. Of the 9 children who could benefit from AAC to support speech, 4 (44%) were receiving AAC services. Finally, of the 8 children who required AAC for all communication, 6 (75%) were receiving AAC services. See Table 1 and Figure 2.
Table 1.
Functional communication categories among children with CP.
| Category | Relationship between AAC and Speech | Number of children |
Number of children with AAC Goals |
|---|---|---|---|
| A. | Children who can meet all communication needs across partners and contexts using speech alone. | 1 | 0 |
| B. | Children who can meet most communication needs across partner and settings using speech alone, but benefit from AAC as a back-up strategy to supplement speech when communication difficulties arise. Speech is the primary mode of communication; AAC is a secondary, supporting mode. | 4 | 2 |
| C. | Children who can meet some communication needs using speech alone, but benefit from AAC to enhance speech intelligibility with some partners and in some contexts. AAC and speech can both be considered primary modes of communication. | 9 | 4 |
| D. | Children who can meet few or no communication needs across all partners and contexts using speech alone. Comprehensive AAC systems are required for nearly all communication. | 8 | 6 |
| Total | 22 | 12 |
Discussion
This study examined the alignment between need for and provision of AAC services to a group of pre-school aged children with CP who had clinical speech-language disorders. The study included 22 children with CP and employed both a direct evaluation component to determine the need for AAC and an analysis of the speech-language goals documented in each child’s IEP.
Results indicated that 95% (21 of 22) of the children with CP who had speech-language disorders in this study could benefit from some form of AAC, while 5% were able to meet all communication needs using speech alone. For each child who was unable to meet all communication needs using speech alone, the need for AAC was further classified into one of three mutually exclusive functional AAC categories to characterize the roles of AAC and speech for each child. Findings indicated that of the children who could benefit from AAC, 19% were able to use speech to meet most communication needs, but could benefit from AAC as a back-up strategy for adverse environments or to manage communication breakdown situations (Category B). In addition, 43% of the children were able to use speech to meet some communication needs, but could benefit from AAC as a means to supplement or enhance speech (Category C). Finally, 38% of children were unable to use speech to meet communication needs and required comprehensive AAC systems to enable functional communication (Category D). From this analysis, it is interesting to note that over half of the children with CP who needed AAC (62%) were able to use speech functionally to some extent (Categories B and C), but still could benefit from AAC as a back-up strategy or to enhance speech intelligibility.
When speech-language goals/objectives targeted in each child’s IEP were examined, results indicated that just over half of children with CP who needed AAC had AAC-focused speech-language goals/objectives in their IEPs. Thus, children with CP appear to be underserved with regard to AAC services in preschool. When AAC services were examined according the specific nature of AAC need, a more detailed picture emerged. Specifically, of the 62% of children with CP who were able to use speech in any capacity (Categories B and C), fewer than half had speech-language goals/objectives targeting AAC in their IEP. However, of the 38% of children with CP who were unable to use speech functionally, two-thirds had AAC-focused speech-language goals/objectives in their IEP. These results suggest that not only are children with CP under-served with regard to AAC services in preschool, but there appears to be a systematic bias against providing AAC-focused speech-language services to children who have any speaking ability. In considering this finding, it important to note that the 22 children included in the study represented 18 different school districts and speech language pathologists. Thus, although findings may reflect regional trends, they do not reflect the trends of one particular school district or municipality.
One key explanation for the findings of this study lies in the knowledge and skills, or lack thereof, of the speech-language pathologists who serve children with CP in the public schools. Studies have documented a consistent need for more and better pre-professional instruction in AAC among speech-language pathology training programs (Koul & Lloyd, 1994; Ratcliff & Beukelman, 1995). Although research suggests that academic preparation in AAC has improved in recent years, there remains a critical need for more academic and clinical training in AAC (Ratcliff et al., 2008). Research examining professional preparation of speech-language pathologists has focused primarily on surveys of graduate programs and courses offered. However, results of this study provide another form of evidence that suggests that practicing speech-language pathologists may have insufficient knowledge and skills in AAC, or at least a limited view of the roles that AAC can play to support speech and multimodal communication. Efforts to provide pre-service and in-service education to speech-language pathologists and students regarding the different roles that AAC can play for children with different speaking capabilities are critical to reduce the number of children who require or could benefit from AAC that are overlooked. Education on the benefits of AAC as a means to prevent communication failure and as a means to scaffold or support speech and language development for children with CP is also important. In addition, it should be emphasized to students and professionals in speech language pathology that AAC and speech are not mutually exclusive communication options. AAC can provide a valuable means, in conjunction with residual speaking capabilities, to support educational and social participation.
Limitations and Clinical Implications
Results of this study suggest that the majority of children with CP who have communication disorders would benefit from speech-language intervention that incorporates AAC. However, our findings indicate that nearly half of children with CP who require AAC are not receiving speech-language services that target AAC, at least as document in their IEPs. Results further suggest that there may be a general bias against targeting AAC goals/objectives with children who are able to use speech as a communication modality (Categories B and C). Children who are stereotypical candidates for AAC (i.e. those who are unable to speak (Category D)) tend to be most likely to have AAC-focused speech-language goals/objectives. These findings are disturbing and suggest that additional pre-service or in-service education regarding AAC is necessary in order to help professionals understand the complementary role that AAC can play with regard to supporting speech and language.
Findings of this study are limited because of the small number of children who were included. In addition, the extent to which our sample represents all children who have CP and communication disorders is unclear. Finally, this study examined only the IEPs and not the actual services provided to the children with CP and communication disorders. As such, it is possible that some children may have been receiving AAC-related interventions that were not documented in their IEPs. Similarly, it is possible that children who were supposed to be receiving AAC-related interventions as specified in their IEPs may not have actually received those interventions. However, if findings of the present study are representative of practices in elementary school, they could have an important detrimental impact on educational and social participation at school and on longer-term outcomes for children with CP. Additional research including a larger number of children who are school-aged as well as children of different ages is necessary to extend the findings of this preliminary study.
Acknowledgements
We thank the children with CP and their families who participated in this study. We also thank Emily McFadd, who provided valuable contributions to coding of goals and objectives. This research was funded by grant R01DC009411from the National Institute on Deafness and Other Communication Disorders, National Institutes of Health, USA.
Footnotes
Note that none of the children had language impairment as their only communication disorder. All children who had language impairment also had speech motor involvement.
References
- Bax M, Tydeman C, Flodmark O. Clinical and MRI correlates of cerebral palsy: The European cerebral palsy study. Journal of American Medical Association. 2006;296(13):1602–1608. doi: 10.1001/jama.296.13.1602. [DOI] [PubMed] [Google Scholar]
- Beukelman DR, Mirenda P. Augmentative and Alternative Communication: Supporting Children and Adults with Complex Communication Needs. 3rd Ed. Baltimore, MD: Paul H. Brookes; 2005. [Google Scholar]
- Bogdan RC, Biklen SK. Qualitative research for education: An introduction to theory and methods. Boston: Allyn & Bacon; 1992. [Google Scholar]
- Cress CJ, Marvin C. Common questions about AAC Services in early intervention. Augmentative and Alternative Communication. 2003;19(4):254–272. [Google Scholar]
- Creswell JC. Research design: Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Hanson EK, Yorkston KM, Beukelman DR. Speech supplementation techniques for dysarthria: A systematic review. Journal of Medical Speech-Language Pathology. 2004;12(2):ix–xxix. [Google Scholar]
- Hustad KC, Gorton KL, McCourt K, Wycklendt T. American Speech Language and Hearing Association Annual Convention. Chicago, IL: 2008. Longitudinal development of speech intelligibility in children with cerebral palsy who have speech motor impairment. [Google Scholar]
- Hustad KC, Jones T, Daily S. Implementing speech supplementation strategies: Effects on intelligibility and speech rate of individuals with chronic severe dysarthria. Journal of Speech, Language, and Hearing Research. 2003a;46:462–474. [PubMed] [Google Scholar]
- Hustad KC, Morehouse TM, Gutman M. AAC strategies for enhancing the usefulness of natural speech in children with severe intelligibility challenges. In: Reichle J, Beukelman D, Light J, editors. Exemplary Practices for Beginning Communicators: Implications for AAC. Baltimore: Paul H. Brookes; 2002. pp. 433–452. [Google Scholar]
- Hustad KC, Shapley KL. AAC and natural speech in individuals with developmental disabilities. In: Light JC, Beukelman DR, Reichle J, editors. Communicative Competence for Individuals who use AAC. Baltimore: Paul H. Brookes; 2003b. pp. 147–162. [Google Scholar]
- Koul R, Lloyd L. Survey of pre-professional preparation in augmentative and alternative communication in speech-language pathology and special education programs. American Journal of Speech-Language Pathology. 1994;3:13–22. doi: 10.1044/1058-0360(2008/005). [DOI] [PubMed] [Google Scholar]
- Light JC, Parsons AR, Drager K. There's more to life than cookies: Developing interactions for social closeness with beginning communicators who use AAC. In: Reichle J, Beukelman D, Light J, editors. Exemplary Practices for Beginning Communicators: Implications for AAC. Baltimore: Paul H. Brookes; 2002. pp. 187–218. [Google Scholar]
- McNaughton D, Light J, Arnold K. Getting your "wheel" in the door: The successful full-time employment experiences of individuals with cerebral palsy who use augmentative and alternative communication. Augmentative and Alternative Communication. 2002;18:59–76. [Google Scholar]
- McNaughton D, Light J, Gulla S. Opening Up a 'whole new world': Employer and co-worker perspectives on working with individuals who use augmentative and alternative Communication. Augmentative and Alternative Communication. 2003;19(4):235–253. [Google Scholar]
- Millar DC, Light JC, Schlosser RW. The impact of augmentative and alternative communication intervention on the speech production of individuals with developmental disabilities: A research review. Journal of Speech, Language, and Hearing Research. 2006;49:248–264. doi: 10.1044/1092-4388(2006/021). [DOI] [PubMed] [Google Scholar]
- Ratcliff A, Beukelman D. Pre-professional preparation in augmentative and alternative communication: State of the art report. Augmentative and Alternative Communication. 1995;11:61–73. [Google Scholar]
- Ratcliff A, Koul R, Lloyd L. Preparation in augmentative and alternative communication: An update for speech-language pathology training. American Journal of Speech-Language Pathology. 2008;17:48–59. doi: 10.1044/1058-0360(2008/005). [DOI] [PubMed] [Google Scholar]
- Romski M, Sevcik RA. Augmentative communication and early intervention: Myths and realities. Infants and Young Children. 2005;18(3):174–185. [Google Scholar]