Abstract
During the last decade, significant scientific research efforts have led to a significant growth in understanding of cancer at the genetic, molecular, and cellular levels providing great opportunities for diagnosis and treatment of cancer diseases. The hopes for fast cancer diagnosis and treatment were significantly increased by the entrance of nanoparticles to the medical sciences. Nanoparticles are attractive due to their unique opportunities together with negligible side effects not only in cancer therapy but also in the treatment of other ailments. Among all types of nanoparticles, surface-engineered superparamagnetic iron oxide nanoparticles (SPIONs) have been attracted a great attention for cancer therapy applications. This review covers the recent advances in the development of SPIONs together with their opportunities and challenges, as theranosis agents, in cancer treatment.
Keywords: Cancer, tumor, nanoscience, nanotechnology, nanoparticle, superparamagnetic iron oxide nanoparticles, SPIONs, coatings, surfaces, targeted drug delivery, controlled drug release, anticancer drugs, chemotherapy, radiotherapy, thermotherapy
Introduction
In 2008, it has been recognized that more than 1 million of Americans and more than 10 million people worldwide were expected to be diagnosed with cancer [1]; however, in 2010 it was expected that the average percentage of people who suffer from some sorts of cancer would be 31% (according to the recent U.N. organized surveys performed in multiple countries). This considerable increase in cancer incidence may relate to the fact that determination of the cancer is strongly dependent upon the development of new diagnostic technologies. However, what is of great importance is that cancers are going to be a significant cause of human death in near future. Thus, intense scientific research was focused on the diagnosis and treatment of cancer.
Due to the dysregulated cell growth in the human body, large groups of different diseases occurred which became recognized as cancer. The uncontrollable cell-cycles not only can form malignant tumors but also can be spread to other parts of the body through the lymphatic system or bloodstream, which is called “metastasis". Although there are numerous available anti-cancer drugs, the main problems currently associated with systemic drug administration include the general systemic distribution of therapeutic drugs, the lack of drug specificity towards a pathological site, the necessity of a large dose to achieve high local concentration, non-specific toxicity and other adverse side effects [2]. Therefore, using modern drug delivery systems are essential for high-yield cancer therapy.
The term “drug delivery” refers to the pharmaceutical agents of interest which are entrapped within, or attached to, an organic polymer matrix or inorganic particles, and in that case, drug safety and efficacy can be greatly improved and new targeted therapies are possible [2]. The strategy for drug delivery can be approached by many methods: (1) drug modification by chemical means [3, 4]; (2) drug encapsulated in vesicles [5-7] or inorganic hollow nanoshells [8-10]; (3) controlled release system such as polymer-based [11-13] and hydrogel-based vectors [14-16], and (4) small-scale integrated systems such as microchip systems [17-20]. The delivery routes are also an important issue for systemic delivery of drugs due to the systemic circulation. Intravenous [21, 22], intra peritoneal [23], pulmonary [24], transdermal [25-27], nose [28, 29], vaginal [30] and eye [31, 32] routes of administration are the approaches designed to improve the selectivity of chemotherapy.
Although there are significant improvements in targeted drug delivery systems, there is a great deal of commonly pursued, desirable qualities for such efficient drug delivery devices, which are not necessarily guidelines. The crucial areas of potential that powerful drug delivery systems should have are: (1) long circulation (i.e. long half-life), (2) high levels of bioavailability and specific targeting, (3) intracellular/organelle delivery, (4) stimuli responsiveness (i.e. efficacy), (5) reporting/imaging, and (6) biodegradation.
In recent years, the fabrication of nanoparticles and exploration of their unusual properties have attracted the attention of physicists, chemists, biologists and engineers. Interest in nanoparticles arises from the fact that the mechanical, chemical, electrical, optical, magnetic, electro-optical and magneto-optical properties of these particles are different from their bulk properties and depend on the particle size. Entrance of nanoparticles in the medical field caused significant hopes for early diagnosis and treatment of catastrophic diseases such as cancer. Nanoparticles are typically referred to as microscopic particles that are between 1 nm and 100 nm in size. Using nanoparticles, delivery systems have the potential to target drugs to specific sites of the body or precisely control drug release rates for prolonged times according to body reaction of chemicals microenvironment [2]. More specifically, nanoparticles as drug carriers in targeted delivery systems in cancer therapies can provide desired and precise penetration of therapeutic and diagnostic substances within for example tumor sites/tissues/cells while their corresponding side effects are much lower in comparison to conventional cancer therapies [2].
Nanoparticles, as smart drug delivery systems, have strong capability to overcome numerous challenges that still exist including the targeting of drugs to specific cells, the creation of novel vaccine delivery approaches, and the development of cell-based delivery systems. Nanoscale drug delivery devices that are stimuli responsive respond dynamically to changes in the environment. These stimuli could be in the form of changes in temperature [33], light [16], pH [15, 34, 35], ultrasound [35-37], or magnetic fields [38, 39]. Disease processes which upset homeostasis can lead to environmental changes that can be exploited by stimuli-responsive therapeutics. Thus, in recent years, significant efforts have been devoted to develop nanotechnology for drug delivery since it offers a suitable means of delivering small molecular weight drugs [40], as well as macromolecules such as proteins, peptides [41] or genes [42, 43] by either localized or targeted delivery to the tissue of interest. It is also worthwhile to mention that nanoparticles may have promise for biomolecular imaging [44]; thus, another potentially important facet of nanoparticles and its application in cancer research could be its capability to probe underlying mechanisms in cancer.
In order to increase the efficiency of drug delivery, magnetic nanoparticles are defined as a promising candidate not only due to capacity of antibodies to attach to their surfaces, but also due to achieve targeting ability by using external magnetic guidance [45, 46]. Among different types of magnetic particles, superparamagnetic iron oxide nanoparticles (SPIONs), with a mean diameter as low as 10 nm and superior magnetic properties, have proven to be among the most capable candidates [47]. In the field of drug delivery, SPIONs particles are considered as small, thermally agitated magnets in carrier liquids, which are called “ferrofluids". A distinguishing feature of SPIONs for drug delivery is their applicability for both alternatives (i.e. magnetic properties and antibody attachment) and consequently developing a targeting capability [2]. Superparamagnetism essentially acts as an activation mechanism because once the external magnetic field is removed, the magnetization disappears, and thus the agglomeration, and hence the possible embolization of the capillary vessels can be avoided [48].
SPIONs also have capability to be used as multifunctional agents [49-51]. The surfaces of SPIONs are engineered to have several simultaneous biomedical-related functions such as drug carrier properties, magnetic resonance imaging (MRI) contrast agents, and local heat induction (hyperthermia) capacity. More recently, a field called “molecular imaging” has appeared, this technique allows the in vivo visualization of molecular events occurring at the cellular level and needs the development of high affinity ligands and their grafting to SPIONs [44]. SPIONs are also good substrates for bioconjugation, they are used as reporters for many physiologic processes and have a lot of clinical applications such as liver and spleen imaging, inflammation, apoptosis, and cardiovascular disease [45, 52, 53].
SPIONs can be accumulated in a biological site by passive or active targeting mechanism. In passive targeting, contrast agents are concentrated in the phagocytic cells (e.g. Kupffer's cells and macrophages) and corresponding organs (e.g. liver, spleen, and lymph nodes) that are responsible for clearance from the body. For example, SPIONs coated with dextran, carboxy-dextran have been used for passive targeting [54-56]. In active targeting, contrast agents need conjugation to a specific ligand to target a site of interest. Typical ligands include antibodies, peptides, sugars, aptamers, etc. which are molecules that can be linked to SPIONs covalently or non-covalently [52, 57, 58].
For biological applications, nanoparticles must be highly stable in aqueous ionic solutions at physiological pH. Vectors grafted on their surface must be able to recognize the target cells or tissues. Particles must be non-toxic and remain in the circulation for a sufficient amount of time to allow targets to be reached. Intensive research are currently undertaken to develop specific contrast agents in targeted cancer imaging. For example, αvβ3 integrin targeted SPIONs have been used for the specific MRI detection of small regions of angiogenesis associated with solid tumors [59, 60].
In summary, SPIONs can be used as theranosis agent in the context of cancer, in other words it can serve as both a diagnostic and therapeutic agent. In this review, the main protocols for the grafting of vectors to SPIONs are reported and some applications are described. In addition, we discuss various in vitro and in vivo studies using surface engineered SPIONs for diagnosis and treatment of cancer diseases.
Synthesis and stabilization of SPIONs
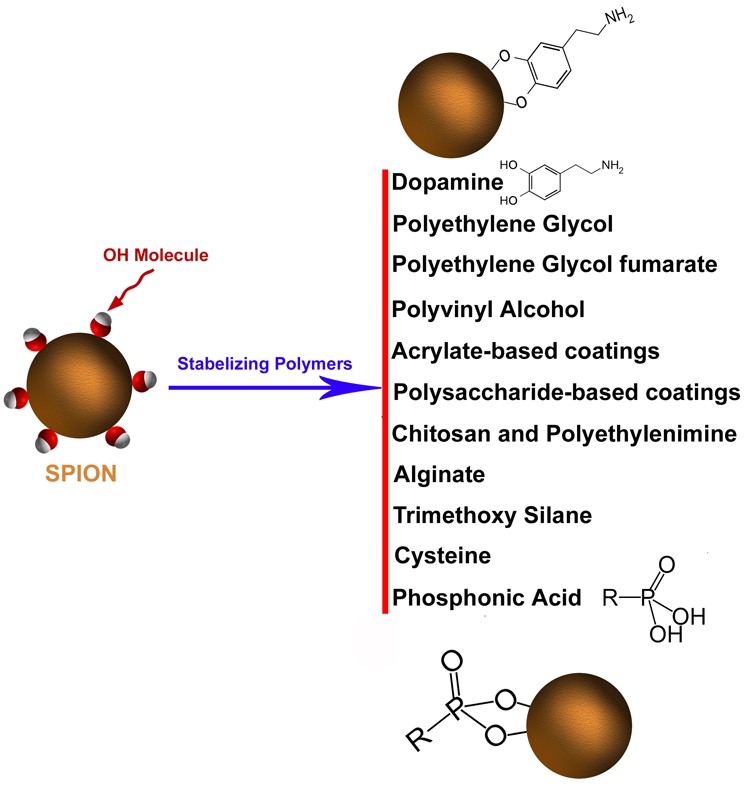
Several methods for chemical synthesis of SPIONs have been described. The most commonly used are summarized in Table 1. Amongst these methods, co-precipitation of Fe2+ and Fe3+ ions in a basic aqueous media (e.g. NaOH or NH4OH solutions) is the simplest way, but usually nanoparticles are polydispersed and poorly crystallized [48]. To avoid these disadvantages, thermal decomposition methods have been employed to produce SPIONs with monodispersity and uniform crystalline [61]. Subsequently, the hydrophobic iron oxide nanoparticles can be coated with phospholipids, silica, or amphiphilic polymers as shells to display good solubility and biocompatibility in vivo (Figure 1).
Table 1.
Principal preparation methods of SPIONs
| Synthetic method | Advantages | Disadvantages | References |
|---|---|---|---|
| Coprecipitation | Rapid synthesis with high yield | Problem of oxidation and aggregation | [48, 62] |
| Hydrothermal reactions | Narrow size distribution and good control, scalable | Long reaction times | [63, 64] |
| High temperature decomposition | Good control of size and shape, High yield | Furthers steps needed to obtain water stable suspension | [61, 65, 66] |
| microemulsion | Control of particle size | Poor yield and large amounts of solvent required, excess of surfactant to eliminate | [51, 67, 68] |
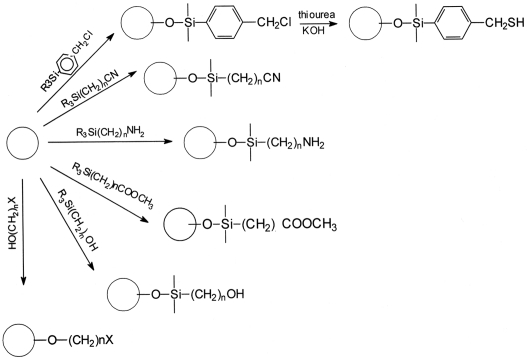
Figure 1.
Scheme showing representative groups that can be used to stabilize the SPIONs.
SPIONs can be coated in situ during the nucleation and growth of the magnetic core (this simultaneous process is often referred to as the “one -pot” method) or after the synthesis following the final application. Monomeric organic stabilizers, polymers and inorganic coatings can also be used to stabilize nanoparticles in aqueous solutions [46, 69]. Organic surfactants are frequently used for the stabilization and coating of magnetic nanoparticles. Fatty acids can stabilize the aqueous fluids by the formation of a surface bilayer with a chemisorbed fatty acid primary layer and an interpenetrating second layer, the latter is physisorbed onto the primary layer with the hydrophilic head-groups pointing outwards [70].
Coating agents which are physically adsorbed (by electrostatic interactions or hydrogen binding) show limited stability in comparison to coating agents which are chemically adsorbed. The stability of the coating grafting also depends on the quantity of the chemical interaction that each molecule or macromolecule can establish with the SPION surface. The most common coatings for biocompatible iron oxide suspensions are polymers [71] such as derivatives of dextran [72, 73] (dextran, carboxymethylated dextran, carboxydextran), arabinogalactan, glycosami-noglycan, starch, polyethyleneglycol, siloxane, sulphonated styrene-divinylbenzene, poly(lactic acid), poly(ε-caprolactone) or polyalkyl-cyanoacrylate [74-76].
Due to their good solubility in water and biocom-patibility, polysaccharides are among the most commonly used coating for the stabilisation of SPIONs. Dextran -SPION can be prepared using co-precipitation method with in situ coating by polysaccharide [77]. Molday and MacKenzie used ferrous and ferric chloride under basic condition in the presence of dextran. Dextran-coated SPIONs with surface functionalities were also developed for specific applications: carboxydextran for cell labeling [78] or aminodextran for grafting with DNA [79]. The chemical modifications of dextran have showed that reduction of terminal sugars can have a significant effect on particle size and coating stability [80]. Particles prepared with carboxydextran yielded a more stable coating [71, 81]. Considering the dextran-coated particles, no evidence of strong chemical adsorption was observed by FTIR (Fourier transform infrared spectroscopy) and SSIMS (statistic secondary ion mass spectra) analysis [82]. The nature of the interactions between the dextran and the SPION surface and its evolution with temperature has been investigated by thermogravimetric and differential thermal analyses and by coupling these data with FTIR analysis [83]. Noteworthy, these dextran-coated iron oxide particles do not show any toxicity [84-87].
Other surface-modifying agents have been explored to increase stability of magnetic nanoparticles. In order to obtain a strong conjugation of dextran to the maghemite surface, Mornet et al. [88] have described a synthetic route consisting of surface modification of SPIONs by silanation of the iron core with aminopropylsilane groups and covalent conjugation with partially oxidized dextran and subsequent reduction of the shiff base [89].
The bonding nature of organosilanes to iron surfaces can be analyzed by FTIR and secondary ion mass spectroscopy (ToF-SIMS). The Si-O-Fe bond is commonly described as covalent [90]. Such systems are ordered molecular assemblies formed by the adsorption of an active molecule (e.g. siloxane, carboxylates, thiolates, and phosphate) on a solid surface (as iron oxide) with different terminal groups (usually -OH, -COOH, and -NH) [91, 92]. This coating can present terminal groups allowing further function-alization by chemical reactions. These functionalities are also frequently incorporated in various polymers where attachment of species on the surface is desired. The stability depends basically on the affinity of the active molecule for the substrate (solid surface), pH and ionic strength of the environment.
Dextran-coated superparamagnetic iron oxide particles can also form stable complexes with transfection agents. Moreover, such complexes can be internalized by endosomes/lysosomes, and have been utilized for tell labeling and in vivo MRI tell tracking [93]. Alginate, another polysaccharide, has also been used for the coating and stabilization of magnetic nanoparticles [51]. Starch-coated SPIONs, obtained via co -precipitation in the presence of starch were also investigated for targeting of brain tumors in rats [94]. Chitosan, a biocompatible and biodegradable polymer, is of particular interest for coating magnetic nanoparticles [95, 96]. It has been reported that oleic acid-coated SPIONs can be easily dispersed in chitosan, producing stable ferrofluids with a typical hydrodynamic diameter of approximately 65 nm [97].
Polylactic acid, another biodegradable polymer, has been used to prepare stable biocompatible ferrofluids with different ferromagnetic particle sizes, ranging from 10 to 180 nm [98]. Polylactic acid-coated nanoparticles can also be loaded with anticancer drugs (e.g., tamoxifen), which allows their use in simultaneous tumor imaging, drug delivery and the real-time monitoring of therapeutic effects [99]. Similar biocompatible nanoparticles have also been prepared via an in situ controlled co-precipitation of magnetite from aqueous solutions containing suitable Fe2+ and Fe3+ salts, in a polymeric starch matrix. This process resulted in starch-coated SPIONs that demonstrated good potential for the imaging of nerve tells and the brain [94].
One very successful strategy for the preparation of stable and biocompatible nanoparticles is to graft polyethylene glycol (PEG) onto the surface (a process known as PEGylation). PEG is not only biocompatible but also has favorable chemical properties and solubility. In this situation, the stabilization is due primarily to steric interactions, while PEGylation can be used to further enhance the pharmacokinetic properties and improve the blood circulation times [100, 101]. For example, an increased image contrast in MRI was achieved by using polymeric micelles formed from SPIONs encapsulated in biocompatible, biodegradable poly(ε-caprolactone)-β-PEG copolymers. These materials have demonstrated significantly improved r2 relaxivities and a good sensitive MRI detection [102]. Copolymers of PEG were also used to stabilize the SPIONs [51, 62].
Aside from the extended half-life that it can provide, one of the great advantages of PEG coating is that it can also be easily conjugated to antibodies or to peptides to achieve a specific targeted delivery. For example, in a recent report, biocompatible water-soluble magnetite nanocrystals were fabricated via the thermal decomposition of ferric triacetylacetonate in 2-pyrrolidone in the presence of monocarboxyl-terminated PEG (MPEG-COOH) [103]. The car-boxylic acid groups on the surface of the particles were conjugated with a cancer-targeting anti-carcinoembryonic antigen (CEA) monoclonal antibody, via a carbodiimide coupling reaction. The resultant materials were assessed for their ability to label cancer tissues in vivo, for subsequent MRI detection [2]. PEG-coated iron oxide nanoparticles may also be conjugated to specific targeting peptides and receptors such as chlorotoxin [104], transactivator protein (Tat) of HIV-1 [105], and integrins [59].
The high temperature decomposition process, known to give nanoparticles a better control of particle size and monodispersity, was described as a one-pot method by decomposition of Fe (acac)3 in 2-pyrolididinone in the presence of MPEG-COOH [103]. Another way to introduce PEG onto SPIONs is to use PEG-silane [106]. This involves reaction of the triethoxysilane group with the hydroxyl group of the SPION surface. Sun et al showed that SPIONs can be treated successively with a bifunctional silane PEG trifluoroethylester linker, ethylenediamine and folic acid (FA). The specificity of these vectorized SPIONs was demonstrated by an increased nanoparticle uptake and a significant contrast enhancement of tumor cells. An alternative protocol to prepare SPION-PEG-FA involved the reaction of FA with tertbutyl-oxycarbonyl (t-BOC) and N-hydroxysuccinimide (NHS), followed by the reaction of (t-boc)folate-NHS with amino-PEG-carboxyl [107]. The resultant (t-boc)folate-PEG-carboxyl was then reacted with SPION with have NH2 groups obtained by reaction with 3-aminopropyl-trimethoxysilane. Finally, the t-boc protective group was removed. Recently, another anchor, dopamine (DPA) has been proposed due to its high affinity for the iron oxide nanoparticle surface and the possibility of functionalization with other molecules through amide bonds [108].
Other polymers and copolymers, which have been used to coat magnetic nanoparticles, include PVP), polyethylenimine (PEI), polyvinyl alcohol (PVA), polysodium-4-styrene sulfonate, poly(trimethylammonium ethylacrylate methyl sulfate)-poly-(acrylamide), polyvinylbenzyl-O-beta -D-galactopyranosyl D-gluconamide (PVLA), poly-caprolactone, and gummic acid [51, 62]. In addition, several stable and biocompatible magnetic fluids have been prepared by coating magnetic nanoparticles with proteins, such as human serum albumin (HSA), avidin, and Annexin AS (anxA5)-VSOP [109, 110].
Dicarboxylic or tricarboxylic acids (citric, tartaric or dimercaptosuccinic acids) [111, 112] are also used for the surface functionalization and stabilization of SPIONs. Some of the functional groups can bind to the surface of the iron oxide, while the remaining carboxylate groups provide negative charges (depending on the pH) and improve the hydrophilicity of the SPION surface. Several studies are reported and demonstrated that phosphonates and phosphates bind efficiently to iron oxide particle surfaces and can serve as potential alternatives to fatty acids [92, 113, 114]. Functionalized phosphonate and phosphate seems to have an acceptable bio-compatibility [115] and it is possible to suggest their utilization as coating agents of magnetic nanoparticles in medical applications [116]. Phosphonates are molecules that contain one or more R-PO(OH)2 Lewis acid groups. The P-C bond is very stable toward oxidation or hydrolysis. These compounds possess a very high ability to form strong complexes with transition metals in aqueous solution and show a large affinity for the metal oxide surfaces [117].
The mechanism of adsorption of dimercaptosuccinic acid (DMSA) has been studied by conductimetric measurements and adsorption isotherms curves. DMSA is oxidized during the coating process in tetrameric polysulfide chains [DMSAox]4 which are absorbed by the carboxylate moiety on the particles after alkalisation and neutralisation. The obtained particles are stable particles at pH = 7 [118, 119].
Among the inorganic coatings, silica, carbon, precious metals (e.g., Ag and Au), or metal oxides are the most frequently used [69]. The silica coating significantly improves the stability of magnetic nanoparticles, protecting them from oxidation, and reduces any potential toxic effects of the nanoparticles [62]. Silica coating can be achieved by using several different approaches; the most popular is the sol-gel process with tetraethyl orthosilicate (TEOS) (known as the Stober method) [120, 121]. Silica shell formation is achieved by the hydrolysis of TEOS in the presence of ammonia and SPIONs, the thickness of the silica coating can be controlled by varying the concentration of ammonium and the ratio of TEOS to water. Amino-silane coatings were activated using glutaralde-hyde, which served as a linker for the binding of a monoclonal antibody directed against cancer. This process resulted in new immunomagnetic nanoparticles for the targeted MRI of cancer [122].
Strategies of vectorization of magnetic nanomaterials for targeted imaging
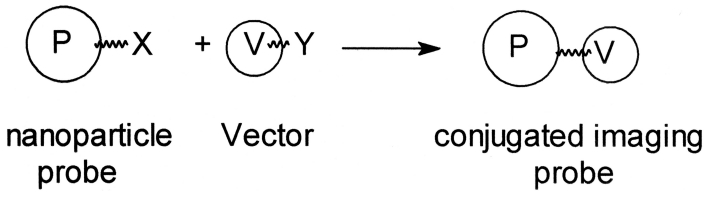
Targeted cellular labeling and molecular imaging require further functionalization in order to provide molecular recognition for specific biological sites. Vectorization is also critical for the further stabilization of nanoparticles, to improve their biocompatibility, and to reduce their potential toxicity. The main vectorization strategies include: (i) the noncovalent grafting of bio-molecules (e.g., antibodies or proteins) via ionic bonding or adsorption; and (ii) the covalent conjugation of biomolecules via strong chemical bonding [123]. Typical examples of the noncovalent approach include the preparation of streptavidin-coated iron oxide nanoparticles [124-126]. Although the noncovalent methods are relatively easy to undertake, the results are very often not reproducible and the response of the materials may be very difficult to control. In addition, noncovalently functionalized nanocomposites are sometimes unstable in variable biological media, and may lose their biological coating and undergo precipitation. Therefore the development of a covalent approach has attracted much more attention during recent years. This involves the formation of linkages between vectors and nanoparticles (see Figure 2).
Figure 2.
Covalent grafting of vectors (V) onto the nanoparticles (P) such as for a molecular imaging probe.
The linkage must be stable (it should be resistant to hydrolysis, oxidizing and reducing conditions) and performed in mild conditions to avoid vector degradation. Typical vector are peptides, proteins, antibodies, mimetic molecules, carbohydrates, lipids, etc. The usual reacting group is an amine or a carboxylic function in the presence of carbodiimine as activator of the carboxylic group but reactions with hydroxyl, thiol or phenol residues are also possible. An oxidative conjugation strategy has been used in previous studies. This method is based on the periodate oxidation of a carbohydrate polymer like dextran or carboxydextran to aldehydes, which may then be linked to biomolecules through the formation of a Schiff base. This strategy has been used for the covalent conjugation of dextran coated magnetic nanoparticles with peptides [127], proteins [128, 129], monoclonal antibodies [130-132] or agglutinin [133]. A substantial loss of the biological activity of the protein has been observed. To minimize this effect, Hogemann et al. [134] have linked proteins and iron oxide particles via a linker. Their results suggest that the oxidative conjugation chemistry significantly interferes with the binding of the conjugates of the receptor. Current efforts are devoted in the direction of non oxidative strategies. The target molecules can be covalently linked through a 3 step-reaction sequence described by Josephson et al. [135]. This approach is based on amine-terminated CLIO nanoparticles, which can be obtained from dextran-coated nanoparticles by cross-linking using epichlorohydrin and then ammonia. A peptide was attached to the amino group of a cross linked dextran iron oxide (CLIO-NH2) using SPDP through a disulfide exchange reaction. A range of target biomolecules can be conjugated by using standard organic chemistry methods: formation of disulfide, carbon-thiol, and amide bonds [105, 136-139].
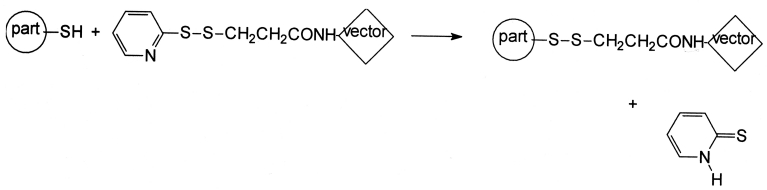
In the so-called “DMSA techniques” 2,3-dimercaptosuccinic acid (DMSA) -coated magnetic nanoparticles can be covalently linked to a variety of biomolecules via S-S bonds using N-succinimidyl 3-(2-pyridyldithio) propionate (SPDP) as a coupling agent (see Figure 3) [118]. This approach has been used to couple antibodies, lectins and annexin V to DMSA-coated magnetic nanoparticles [119, 140, 141].
Figure 3.
Formation of grafted particles via S-S bridge: the pyridyl sulfide moiety of SPDP grafted on the vector is substituted by the SH group on the nanoparticles. Reprinted with permission from (reference 52). Copyright 2010 American Chemical Society.
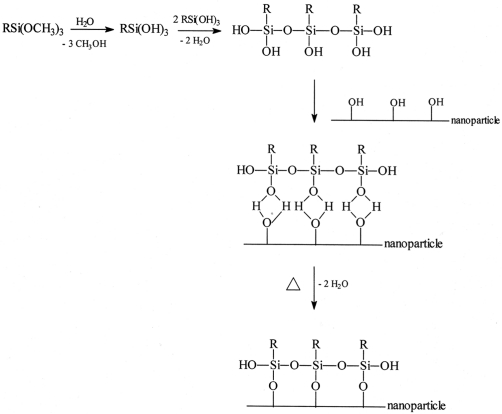
Magnetite nanoparticles coated with silica were prepared, after surface modification with an amino-silane coupling agent, SG-Si900, amine was covalently linked using glutaraldehyde as a cross-linker [142]. Alternatively, vectors with carboxylic functions can be directly grafted on the silica coated particles using EDC to activate the carboxyl groups [143]. The silane coupling materials (like 3-aminopropyltrimethoxysilane or p-aminophenyl trimethoxysilane) [144] are able to adsorptively or covalently bind to the metal oxide and are able to form covalent bonds with bioaffinity adsorbents through organo-functionalities. The mechanism of the silane coupling agents reaction according to Arkles was depicted in Figure 4 [145].
Figure 4.
Adsorption mechanism of organosilane and chemical reactions of silane coupling agents on magnetic particles (R= CH2CH2CH2NH2, CH2CH2CH2CN, …; R'=CH3, C2H5). Reprinted with permission from (reference 52). Copyright 2010 American Chemical Society.
The silane is deposited on the metal oxide core from acidic solution (see Figure 5). The silinization reaction occurs in two steps: (i) the trimeth-oxysilane is placed in acidic water, phosphorous acid and glacial acetic acid and it condenses to form silane polymers; (ii) these polymers associate with the metal oxide by forming covalent bond with surface OH groups through dehy-dratation or by adsorption of silane polymers to the metal oxide. Diazotation of aminophenyl-terminated silane or the use of glutaraldehyde on 3-aminopropyl-terminated silane can be used to couple antibodies or immunoglobulins. This second procedure also consists of two basic steps: (i) activation of the particle by reaction with glutaraldehyde followed by (ii) removal of unreacted glutaraldehyde and reaction of the proteins with the activated particles followed by removal of the unreacted proteins. If the magnetic particles are coated by carboxy-terminated silanes, proteins can be coupled to them by treating the particles with 3-(3-dimethylaminopropyl) carbodiimide. The surface chemsitry involving reactions with alkyltrialkoxysilane or trichloroalkylsilane compounds is a good way for grafting biomolecules [146, 147].
Figure 5.
Possibilities of surface modification with organosilane following the chemical reactions described in Figure 4. Reprinted with permission from (reference 52). Copyright 2010 American Chemical Society.
Finally, the recently developed “click” chemistry, based on the azide-alkyne reaction, has been applied to the functionalization of iron oxide nanoparticles [114, 148, 149], and allows the relatively simple synthesis of azido- or alkyne-functionalized nanoparticles, which then can be linked to appropriate target molecules. For example, Turro et al. [114] described the stabilization of Fe2O3 nanoparticles using alkyne-terminated organophosphate or carboxylic acid groups to exchange with oleic acid on the Fe2O3 surface. The IONPs were subsequently cova-lently attached to poly(tert-butyl acrylate) via click reactions using CuSO4.
A pan-bombesin analog was conjugated through a linker to dye-functionalized superparamag netic iron oxide nanoparticles for the targeting of prostate cancer cells. The peptide was conjugated via click chemistry. The peptide-functionalized nanoparticles were then demonstrated to be selectively taken up by PC-3 prostate cancer cells relative to unfunctionalized nanoparticles and this uptake was inhibited by the presence of free peptide, confirming the specificity of the interaction [150].
SPIONs against cancer diseases
Drug delivery
Widder et al. [151] employed the first magnetic drug (i.e. doxorubicin (Dox)) delivery systems, where Dox was encapsulated in albumin magnetic nanoparticles. After this report, intense research has focused on targeted delivery and imaging using magnetic nanoparticles [152-169]. Some of the developed magnetic nanoparticles have rapid hepatic uptake after intravenous administration; these uptakes would be of crucial importance for hepatic tumors diagnosis and treatment [170, 171]. However, the crucial matter for high-yield drug delivery using magnetic nanoparticles is their targeting capabilities. In order to increase the targeting capability of magnetic particles, it is essential to attach targeting moieties (e.g. antibodies and hormones) to the surface of magnetic nanoparticles. In this case, there are varieties of methods for conjugation of antibodies to the surface of magnetic nanoparticles with no detectable effects on the colloidal stability of the particles [172, 173]. Attachment of epidermal growth factor (EGF) to the magnetic nanoparticles can be useful in treatment of colorectal and breast cancers [174]. HER2 antibody was also conjugated with glycerol mono-oleate coated SPIONs and the resulting materials showed enhanced uptake in human breast carcinoma cell line (i.e. MCF-7) [175]. Hormones (e.g. LHRH) conjugated SPIONs also showed good capability for targeting of cancer cells in both the primary breast tumors and the lung metastases cells [176].
In relation to targeting properties, there are also two main additional problems for high yield targeted delivery. First, as the drug coats the surface of nanoparticles, a significant portion of it is quickly released upon injection (i.e. burst effect). Therefore, only small amounts of the drug reach the specific site after, for instance, magnetic drug targeting. Second, once the surface-derivatized nanoparticles are inside the cells, the coating is likely digested, leaving the bare particles exposed to other cellular components and organelles, thereby potentially influencing the overall integrity of the cells. To overcome these two shortcomings, Mahmoudi et al. [177] used cross-linked poly (ethylene glycol)-co-fumarate (PEGF) coating on the surface of SPIONs. To investigate if the coating could reduce the burst effect, nanoparticles were prepared by incorporating the anticancer drug Tamoxifen (TMX). The cross-linked PEGF coating reduced the burst effect rate by 21% in comparison with the noncross-linked tamoxifen nanoparticles [177]. Thus, the authors claimed that the SPIONs with coating based on crosslinked unsatu-rated aliphatic polyesters are potentially useful to develop novel carriers for drug and gene delivery applications [177].
Another crucial matter is the multifunctional capabilities of the engineered SPIONs, which are a key focus in bionanotechnology and will have profound impact on molecular diagnostics, imaging and therapeutic of cancer diseases. Gao et al. [178] prepared FePt coated SPIONs and claimed that their core-shell particles have good capability to be functionalized by various targeting molecules (e.g. antibodies). These multifunctional nanoparticles can enhance the capability of magnetic particles for simultaneous detection and monitoring of the transformation of tumors by noninvasive MRI during chemotherapeutic treatment by nanoparticles. In order to combine multiple components on a nanometer scale for creation of new imaging modalities, which are unavailable from individual components, Jin et al. [179] prepared multifunctional nanoprobes. These not only offered contrast for electron microscopy, MRI and scattering-based imaging but also, more importantly, enabled a new imaging mode, magnetomotive photoacoustic imaging. This form of imaging with remarkable contrast enhancement compared with photoacoustic images using conventional nanoparticle contrast agents; these particles were composed of thin gold coated SPIONs by creating a gap between the core and the shell. Very recently, Mahmoudi et al. [50] synthesized a multi-component system made of gold-coupled core-shell SPIONs, as a new nano-probe with signal enhancement in surface Raman spectroscopy, due to its jagged-shaped gold shell coating. These new classes of multifunctional magnetic nanoparticles [50, 179] may have great impact in the future in relation to cancer diagnosis and therapy.
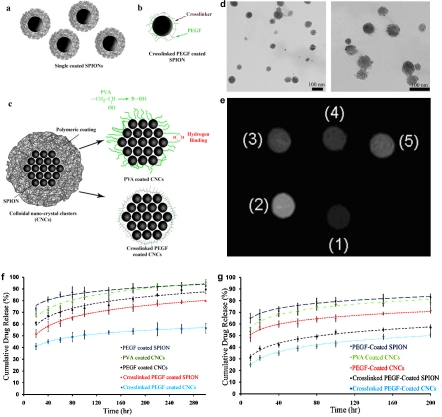
Amiri et al. [180] reported cell endocytosis, drug release, NMR relaxometry and in vitro MRI studies on a novel class of superparamagnetic colloidal nano-crystal clusters (CNCs) with various biocompatible coatings. They claimed that the transverse relaxivity r2, the parameter representing the MRI efficiency in negative contrast agents, for the polyvinyl alcohol (PVA)-coated, polyethylene glycol-co-fumarate (PEGF)-coated, and crosslinked PEGF-coated CNCs was efficient enough to contrast suitably the MRI (see Figure 6). In addition, their prepared samples have been shown to facilitate controlled drug release (particularly the crosslinked PEGF-coated compound), thereby finally allowing them to propose this class of compounds for future applications in cancer, as theranostics agents.
Figure 6.
(a-c) Schemes of the various synthesized magnetic nanoparticles including (a) single coated SPIONs, (b) crosslinked coated SPION, and (c) PVA- and crosslinked PEGF- coated CNCs. (d) TEM images of crosslinked PEGF-coated CNCs with various magnifications. (e) MRI image of vials containing different samples with the same iron concentrations (0.02 mg/ml) obtained by Artoscan S.p.A. imager at H=0.2T: (1) Endorem (commercially available dextran coated SPIONs), (2) bare SPIONs, (3) PVA-Coated CNCs, (4) PEGF-coated CNCs, (5) Crosslinked PEGF-Coated CNCs. Release profiles of (f) TMX and (g) DOX from PEGF- and crosslinked PEGF- coated single nanoparticles; and PVA-, PEGF- and crosslinked PEGF- coated CNCs over 300 and 200 hours, respectively. With permission from reference [180].
Besides in vitro evaluations of drug loaded surface engineered magnetic nanoparticles, there are numerous in vivo targeting assessments. For instance SPIONs have been injected very close to tumor sites in animal models and human clinical studies for targeting delivery of anticancer drugs [181-188]. SPIONs have the capability to enhance MRI in combination with diffusion weighted MRI, which can be a novel, accurate, and fast method for detecting pelvic lymph node metastases even in normal-sized nodes of patients with bladder or prostate cancer [189]. The surface engineered SPIONs can be also employed in diagnosis and treatment of colorectal cancer [190].
In order to increase the yield of magnetic targeting, Widder et al. [191, 192] employed intra-arterial injection proximal to the tumor site (Dox filled magnetic particles). Their results demonstrated a 200-fold increased targeting yield in comparison with intravenous injection [193]. Since this study, success in cytotoxic drug delivery and tumor remission has been reported by several groups using animals models including swine [194, 195], rabbits [196] and rats [197-199]. In order to increase the targeting yield of magnetic nanoparticles, permanent magnets can be implanted in a targeted site; for example, permanent magnets were implanted at solid osteosarcoma sites in hamsters and anti-cancer drugs subsequently delivered to the targeted site using magnetic liposomes [200]. Using magnetic implantation methods, the yield of targeting were enhanced four-fold in comparison with normal intravenous (non-magnetic) delivery. Results also showed significant increase in anti-tumor activity and the elimination of weight-loss as a side effect [201]. This technique has also been employed to target cytotoxic drugs to brain tumors, where passing the drugs through the blood-brain barrier is difficult [199]. Preliminary successful animal trials have lead to the development of magnetic nanoparticles for use in human trials. For example, magnetic nanoparticles (metallic Fe coated with activated carbon) which carried the Dox as drug is employed by FeRx [195]. It is noteworthy to mention that FeRx Inc. was granted fast-track status to proceed with multi-centre Phases I and II clinical trials of their magnetic targeting system for hepatocellular carcinomas. However, in April 2004 FeRx halted its clinical trial, putting into doubt company's ability to continue as a going concern [2].
Hyperthermia
One of the crucial capabilities of Magnetic nanoparticles is that they can be made to generate heat, which leads to their use as hyper thermia agents, delivering toxic amounts of thermal energy to cancerous tumors where a moderate degree of tissue warming results in more effective cell destruction [202, 203]. The production of local heat in magnetic nanoparticles is due to the fact that the magnetic anisotropy of magnetic nanoparticles can be much greater than those of a bulk materials, while differences in the Curie or Néel temperatures, i.e., the temperatures of spontaneous parallel or antiparallel orientation of spins between magnetic nanoparticles and the corresponding microscopic phases, reach hundreds of degrees [203, 204]. Magnetic nanoparticles were first employed in hyperthermia application in the work of Chan et al. [205] and Jordan et al. [206] in 1993, where they proved that superparamagnetic crystal suspension had great capability to absorb the energy of an alternating magnetic field; this absorbed energy can in turn be converted into heat. Given that tumor cells are more sensitive to a temperature increase than healthy ones [207, 208], this property can be used in vivo to increase the temperature of cancerous tissue and to destroy the pathological cells by hyperthermia.
During the last 2 decades, intense efforts were focused on improvement of hyperthermia techniques for clinical applications. Advances in the area of nanotechnology have contributed to the development of superparamagnetic fluid hyperthermia, which is well recognized as promising method for cancer treatment because of the ease of targeting the cancerous tissue and hence having fewer side effects than chemotherapy and radiotherapy, as proven by the results of current/ongoing clinical trials [209].
Hergt et al. [210] injected 100 mg dextran coated magnetic nanoparticles into the tail vein of Sprague Dawley rats, treated with AC magnetic field (12 min, 450 kHz, unknown field and SAR). According to authors’ considerable the tumor shrinkage and tissue necrosis was observed. Jordan and co-workers [211-225] did the first clinical patient trials [226] with magnetic nanoparticles. In this case, a special hyperthermia-generating prototype instrument was developed which is able to generate variable magnetic fields in the range of 0 -15 kA/m at a frequency of 100 kHz. At the same time, the machine allows for real-time patient temperature measurements to ensure that neither the upper limit of the therapeutic temperature threshold is exceeded, thus preventing thermal ablation, nor the lower, ineffective limit is crossed. This prototype is capable of treating tumors placed in any region of the body (e.g., prostate cancer, brain tumors).
Maier-Hauff et al. [227] injected neuro-navigationally controlled intra-tumoral instillation of an aqueous dispersion of iron-oxide nanoparticles in 66 patients (59 with recurrent glioblastoma) and subsequently the particles were heated up using an alternating magnetic field. Treatment was combined with fractionated stereotactic radiotherapy. A median dose of 30 grays (Gy) using a fractionation of 5 x 2 Gy/ week was applied. The primary study endpoint was overall survival following diagnosis of first tumor recurrence (OS-2), while the secondary endpoint was overall survival after primary tumor diagnosis (OS-1). The median overall survival from diagnosis of the first tumor recurrence among the 59 patients with recurrent glioblastoma was 13.4 months (95% CI: 10.6-16.2 months). Median OS-1 was 23.2 months while the median time interval between primary diagnosis and first tumor recurrence was 8.0 months. The authors claimed that the side effects of their new therapeutic approach were moderate, and no serious complications were observed [227]. According to these results, one can conclude that thermotherapy using magnetic nanoparticles in conjunction with a reduced radiation dose is reasonably safe and effective and leads to longer OS-2 compared to conventional therapies in the treatment of recurrent glioblastoma [227]. Till now, only local hyperthermia is applicable for magnetic fluid hyperthermia; in this case, surface-engineered magnetic nanoparticles, which are dispersed in a carrier fluid, are placed inside the cancerous tumor through direct injection or tumor specific antibody targeting. This specific antibody targeting cause the attachments of nanoparticles to the cancerous cells and the labeled-cells are exposed to an alternating magnetic field. This field makes the magnetic nanoparticles generate heat by magnetic relaxation mechanisms; these local heats can induce apoptosis to the labeled cells.
Simultaneous drug delivery and hyperthermia
One of the crucial problems with magnetic targeted hyperthermia is that a limited dose of nanoparticles reached the tumor tissue. This resulted in insufficient temperature enhancement in the cancerous sites; thus there is a risk of proliferation of cancer cells that survived during thermotherapy [229]. In order to overcome the problem, several specific tumor receptor targeting moieties together with anticancer drugs can be attached to the surface of particles. These employed targeting moieties together with anti-cancerous drugs may induce cell apoptosis. In this case, the hyperthermia treatment was used as a driving force for simultaneous drug delivery purposes (e.g. using ther-mosensitive polymers [203], as nanoparticle's coating) [230] For example, β-cyclodextrin (CD) was used as a drug container for hydrophilic (paclitaxel) or lipophilic (doxorubicin) structures. Drugs incorporated in the CD can thus be released through the use of induction heating, or hyperthermic effects, by applying a high-frequency magnetic field. In this case, folic acid (FA) and CD-functionalized magnetic nanoparticles were synthesized and it was found that by induction of heating, drug release was triggered from the CD cavity on the particle - a behavior that was controlled by switching the high-frequency magnetic field on and off. Another drug delivery system, based on cova-lently attaching genistein onto SPIONs coated by cross-linked carboxymethylated chitosan (CMCH), has been developed [231] and the results confirmed that the nanosystem could significantly enhanced cancer cell apoptosis.
Importance of protein-nanoparticle interactions
It has been long recognized that proteins were associated with nanoparticles, upon entrance of nano-objects into a biological fluid [232-235]. The amount and types of the associated proteins, which is called a protein “corona", on the surface of the nanoparticles leads to an in vivo response [232]. More specifically, composition of the obtained protein corona can be used for prediction of the way cells interact with, recognize and process the nanoparticles [236].
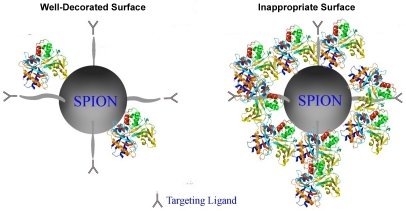
It also has been shown that the composition of the hard corona protein profiles can be significantly different due to the changes in surface chemistries of the same materials [237]. Thus, decoration of the surface of magnetic nanoparticles would be very useful for the efficient design of targeted delivery systems where the targeting moieties are covered on the surface of SPIONs. More specifically, inappropriate surface chemistry of nanoparticles have great capability to be severely covered by the proteins which may causing the elimination of targeting moieties; in contrast, the targeting species of the well surface decorated particles are active due to their lower protein affinity (lowest thickness of protein corona in comparison with inappropriate surface) to proteins causing the highest targeting yields (see Figure 7). Clearly there is a significant amount of work to be done to confirm these issues.
Figure 7.
Cartoon showing the importance of surface chemistries in targeted delivery/imagingapplications.
Conclusions and future perspectives
Multifunctional SPIONs play an important role in the development of simultaneous targeted delivery, imaging, and hyperthermia for diagnosis and treatment of cancerous tumors in vivo. Deeper understanding on the protein corona compositions at the surface of nanoparticles are essential for development of nanoparticle specific uptake by desired cells in vivo. In addition, control of the protein corona which is formed at the surface of magnetic particles, which are decorated by cancer-specific binding agents, would make targeted delivery and magnetic fluid hyperthermia treatment much more selective than traditional chemotherapy and even conventional hyperthermia. Furthermore, multifunctional magnetic particles can be magnetically targeted and concentrated in the target tissue, and drug release together with heating are then only induced to significant burst effects and temperatures where the magnetic nanoparticles have been deposited. In addition, tissue-deposited magnetic particles will generally stay where they were initially deposited, thus allowing for repeated and concentrated drug release and hyperthermia treatments in the same area.
At the moment the amount of particles delivered to the cancerous tissues/cells by means of antibody targeting is too low for a sufficient drug release and temperature increase. Thus, the main challenges in this field will be the design of stealth nanoparticles able to circulate in the blood compartment for a long time and the surface grafting of ligands able to facilitate their specific internalization in cancerous cells. Although the results obtained from the first clinical trials of magnetic nanoparticles are very promising, it would be premature to claim that these molecules contribute therapeutic advantages because survival and disease progression benefits were not defined endpoints of the feasibility studies.
There are several matters that should be considered to enhance the targeted drug delivery, targeted imaging and hyperthermia yield of SPIONs. These include the exact definition of cell membrane composition; in vivo control of drug release; in vivo control of heat distribution; management surface of the nanoparticles’ for formation of desired protein corona composition followed by fast internalization by the target cells; and optimization of the biophysicochemical properties of the particles. A non homogeneous particle distribution in the tissue may lead to the occurrence of uncontrollable targeting, drug release, and hot spots where the high drug amounts/temperature could cause non-specific necrosis of the tissue. In contrast, in regions with a low particle concentration the drug and/ or temperature would not be sufficiently high enough to trigger the onset of apoptosis and a proliferation of surviving cancerous cells can still occur. Both effects should be prevented and thus more even distribution of particles in the tissue as well as the monitoring of the spatial heat distribution should form the focus of future research.
Acknowledgments
In memory of Baba Ardeshir.
References
- 1.Anand P, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB. Cancer is a Preventable Disease that Requires Major Lifestyle Changes. Pharm Res. 2008;25:2097–116. doi: 10.1007/s11095-008-9661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmoudi M, Sant S, Wang B, Laurent S, Sen T. Superparamagnetic iron oxide nanoparticles (SPIONs): Development, surface modification and applications in chemotherapy. Advanced Drug Delivery Reviews. 2011;63:24–46. doi: 10.1016/j.addr.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Means GE, Feeney RE. Chemical Modifications of Proteins: History and Applications. Bioconjugate Chemistry. 1990;1:2–12. doi: 10.1021/bc00001a001. [DOI] [PubMed] [Google Scholar]
- 4.Chau Y, Dang NM, Tan FE, Langer R. Investigation of targeting mechanism of new dextran-peptide-methotrexate conjugates using biodistribution study in matrix-metalloproteinase-overexpressing tumor xenograft model. Journal of Pharmaceutical Sciences. 2006;95:542–51. doi: 10.1002/jps.20548. [DOI] [PubMed] [Google Scholar]
- 5.Gregoriadis G. Engineering liposomes for drug delivery: Progress and problems. Trends in Biotechnology. 1995;13:527–37. doi: 10.1016/S0167-7799(00)89017-4. [DOI] [PubMed] [Google Scholar]
- 6.Adams ML, Lavasanifar A, Kwon GS. Amphiphilic block copolymers for drug delivery. Journal of Pharmaceutical Sciences. 2003;92:1343–55. doi: 10.1002/jps.10397. [DOI] [PubMed] [Google Scholar]
- 7.Rosler A, Vandermeulen GWM, Klok HA. Advanced drug delivery devices via self-assembly of amphiphilic block copolymers. Advanced Drug Delivery Reviews. 2001;53:95–108. doi: 10.1016/s0169-409x(01)00222-8. [DOI] [PubMed] [Google Scholar]
- 8.Wu GH, Milkhailovsky A, Khant HA, Fu C, Chiu W, Zasadzinski JA. Remotely triggered liposome release by near-infrared light absorption via hollow gold nanoshells. Journal of the American Chemical Society. 2008;130:8175–7. doi: 10.1021/ja802656d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Son SJ, Bai X, Lee SB. Inorganic hollow nanoparticles and nanotubes in nanomedicine. Part 1. Drug/gene delivery applications. Drug Discovery Today. 2007;12:650–6. doi: 10.1016/j.drudis.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Akerman ME, Chan WCW, Laakkonen P, Bhatia SN, Ruoslahti E. Nanocrystal targeting in vivo. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:12617–21. doi: 10.1073/pnas.152463399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uhrich KE, Cannizzaro SM, Langer RS, Shakesheff KM. Polymeric systems for controlled drug release. Chemical Reviews. 1999;99:3181–98. doi: 10.1021/cr940351u. [DOI] [PubMed] [Google Scholar]
- 12.Veronese FM, Pasut G. PEGylation, successful approach to drug delivery. Drug Discovery Today. 2005;10:1451–8. doi: 10.1016/S1359-6446(05)03575-0. [DOI] [PubMed] [Google Scholar]
- 13.Richardson TP, Peters MC, Ennett AB, Mooney DJ. Polymeric system for dual growth factor delivery. Nature Biotechnology. 2001;19:1029–34. doi: 10.1038/nbt1101-1029. [DOI] [PubMed] [Google Scholar]
- 14.Vinogradov SV, Bronich TK, Kabanov AV. Nanosized cationic hydrogels for drug delivery: preparation, properties and interactions with cells. Advanced Drug Delivery Reviews. 2002;54:135–47. doi: 10.1016/s0169-409x(01)00245-9. [DOI] [PubMed] [Google Scholar]
- 15.Gupta P, Vermani K, Garg S. Hydrogels: from controlled release to pH-responsive drug delivery. Drug Discovery Today. 2002;7:569–79. doi: 10.1016/s1359-6446(02)02255-9. [DOI] [PubMed] [Google Scholar]
- 16.Qiu Y, Park K. Environment-sensitive hydrogels for drug delivery. Advanced Drug Delivery Reviews. 2001;53:321–39. doi: 10.1016/s0169-409x(01)00203-4. [DOI] [PubMed] [Google Scholar]
- 17.Santini JT, Cima MJ, Langer R. A controlled-release microchip. Nature. 1999;397:335–8. doi: 10.1038/16898. [DOI] [PubMed] [Google Scholar]
- 18.LaVan DA, McGuire T, Langer R. Small-scale systems for in vivo drug delivery. Nature Biotechnology. 2003;21:1184–91. doi: 10.1038/nbt876. [DOI] [PubMed] [Google Scholar]
- 19.Grayson ACR, Choi IS, Tyler BM, Wang PP, Brem H, Cima MJ, Langer R. Multi-pulse drug delivery from a resorbable polymeric microchip device. Nature Materials. 2003;2:767–72. doi: 10.1038/nmat998. [DOI] [PubMed] [Google Scholar]
- 20.Razzacki SZ, Thwar PK, Yang M, Ugaz VM, Burns MA. Integrated microsystems for controlled drug delivery. Advanced Drug Delivery Reviews. 2004;56:185–98. doi: 10.1016/j.addr.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 21.Collins JM. PHARMACOLOGIC RATIONALE FOR REGIONAL DRUG DELIVERY. Journal of Clinical Oncology. 1984;2:498–504. doi: 10.1200/JCO.1984.2.5.498. [DOI] [PubMed] [Google Scholar]
- 22.Egan TD. Intravenous drug delivery systems: Toward an intravenous ‘'vaporizer''. Journal of Clinical Anesthesia. 1996;8:S8–S14. doi: 10.1016/s0952-8180(96)90005-7. [DOI] [PubMed] [Google Scholar]
- 23.Markman M. Intraperitoneal antineoplastic drug delivery: rationale and results. Lancet Oncology. 2003;4:277–83. doi: 10.1016/s1470-2045(03)01074-x. [DOI] [PubMed] [Google Scholar]
- 24.Edwards DA, Hanes J, Caponetti G, Hrkach J, BenJebria A, Eskew ML, Mintzes J, Deaver D, Lotan N, Langer R. Large porous particles for pulmonary drug delivery. Science. 1997;276:1868–71. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- 25.Prausnitz MR, Bose VG, Langer R, Weaver JC. ELECTROPORATION OF MAMMALIAN SKIN - A MECHANISM TO ENHANCE TRANSDERMAL DRUG-DELIVERY. Proceedings of the National Academy of Sciences of the United States of America. 1993;90:10504–8. doi: 10.1073/pnas.90.22.10504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henry S, McAllister DV, Allen MG, Prausnitz MR. Microfabricated microneedles: A novel approach to transdermal drug delivery. Journal of Pharmaceutical Sciences. 1998;87:922–5. doi: 10.1021/js980042+. [DOI] [PubMed] [Google Scholar]
- 27.Prausnitz MR, Mitragotri S, Langer R. Current status and future potential of transdermal drug delivery. Nature Reviews Drug Discovery. 2004;3:115–24. doi: 10.1038/nrd1304. [DOI] [PubMed] [Google Scholar]
- 28.Illum L. Nasal drug delivery: new developments and strategies. Drug Discovery Today. 2002;7:1184–9. doi: 10.1016/s1359-6446(02)02529-1. [DOI] [PubMed] [Google Scholar]
- 29.Illum L. Nasal drug delivery - possibilities, problems and solutions. J Control Release. 2003;87:187–98. doi: 10.1016/s0168-3659(02)00363-2. [DOI] [PubMed] [Google Scholar]
- 30.rannonpeppas L. NOVEL VAGINAL DRUG-RELEASE APPLICATIONS. Advanced Drug Delivery Reviews. 1993;11:169–77. [Google Scholar]
- 31.Loftssona T, Jarvinen T. Cyclodextrins in ophthalmic drug delivery. Advanced Drug Delivery Reviews. 1999;36:59–79. doi: 10.1016/s0169-409x(98)00055-6. [DOI] [PubMed] [Google Scholar]
- 32.Le Bourlais C, Acar L, Zia H, Sado PA, Needham T, Leverge R. Ophthalmic drug delivery systems - Recent advances. Progress in Retinal and Eye Research. 1998;17:33–58. doi: 10.1016/s1350-9462(97)00002-5. [DOI] [PubMed] [Google Scholar]
- 33.Jeong B, Bae YH, Lee DS, Kim SW. Biodegradable block copolymers as injectable drug-delivery systems. Nature. 1997;388:860–2. doi: 10.1038/42218. [DOI] [PubMed] [Google Scholar]
- 34.Li F, Liu WG, De Yao K. Preparation of oxidized glucose-crosslinked N-alkylated chitosan membrane and in vitro studies of pH-sensitive drug delivery behaviour. Biomaterials. 2002;23:343–7. doi: 10.1016/s0142-9612(01)00111-9. [DOI] [PubMed] [Google Scholar]
- 35.Mitragotri S. Innovation - Healing sound: the use of ultrasound in drug delivery and other therapeutic applications. Nature Reviews Drug Discovery. 2005;4:255–60. doi: 10.1038/nrd1662. [DOI] [PubMed] [Google Scholar]
- 36.Liu YY, Miyoshi H, Nakamura M. Encapsulated ultrasound microbubbles: Therapeutic application in drug/gene delivery. Journal of Controlled Release. 2006;114:89–99. doi: 10.1016/j.jconrel.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 37.Ng KY, Liu Y. Therapeutic ultrasound: Its application in drug delivery. Medicinal Research Reviews. 2002;22:204–23. doi: 10.1002/med.10004. [DOI] [PubMed] [Google Scholar]
- 38.Lubbe AS, Alexiou C, Bergemann C. Clinical applications of magnetic drug targeting. Journal of Surgical Research. 2001;95:200–6. doi: 10.1006/jsre.2000.6030. [DOI] [PubMed] [Google Scholar]
- 39.Polyak B, Friedman G. Magnetic targeting for site-specific drug delivery: applications and clinical potential. Expert Opinion on Drug Delivery. 2009;6:53–70. doi: 10.1517/17425240802662795. [DOI] [PubMed] [Google Scholar]
- 40.Sahoo SK, Labhasetwar V. Nanotech approaches to delivery and imaging drug. Drug Discovery Today. 2003;8:1112–20. doi: 10.1016/s1359-6446(03)02903-9. [DOI] [PubMed] [Google Scholar]
- 41.Torchilin VP, Lukyanov AN. Peptide and protein drug delivery to and into tumors: challenges and solutions. Drug Discovery Today. 2003;8:259–66. doi: 10.1016/s1359-6446(03)02623-0. [DOI] [PubMed] [Google Scholar]
- 42.Naldini L, Blomer U, Gallay P, Ory D, Mulligan R, Gage FH, Verma IM, Trono D. In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science. 1996;272:263–7. doi: 10.1126/science.272.5259.263. [DOI] [PubMed] [Google Scholar]
- 43.Zufferey R, Nagy D, Mandel RJ, Naldini L, Trono D. Multiply attenuated lentiviral vector achieves efficient gene delivery in vivo. Nature Biotechnology. 1997;15:871–5. doi: 10.1038/nbt0997-871. [DOI] [PubMed] [Google Scholar]
- 44.Mahmoudi M, Serpooshan V, Laurent S. Engineered nanoparticles for biomolecular imaging. Nanoscale. 2011;3:3007–29. doi: 10.1039/c1nr10326a. [DOI] [PubMed] [Google Scholar]
- 45.Mahmoudi M, Hosseinkhani H, Hosseinkhani M, Boutry S, Simchi A, Shane Journeay Ws, Subramani K, Laurent S. Magnetic resonance imaging tracking of stem cells in vivo using iron oxide nanoparticles as a tool for the advancement of clinical regenerative medicine. Chemical Reviews. 2011;111:253–80. doi: 10.1021/cr1001832. [DOI] [PubMed] [Google Scholar]
- 46.Gupta AK, Gupta M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 2005;26:3995–4021. doi: 10.1016/j.biomaterials.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 47.Mahmoudi M, Milani AS, Stroeve P, Arbab SA. New York: Nova Science Publisher; 2011. Superparamagnetic Iron Oxide Nanoparticles: Synthesis, Surface Engineering, Cytotoxicity and Biomedical Applications. ISBN: 978-1-61668-964-3. [Google Scholar]
- 48.Mahmoudi M, Simchi A, Imani M, Milani AS, Stroeve P. Optimal design and characterization of superparamagnetic iron oxide nanoparticles coated with polyvinyl alcohol for targeted delivery and imaging. Journal of Physical Chemistry B. 2008;112:14470–81. doi: 10.1021/jp803016n. [DOI] [PubMed] [Google Scholar]
- 49.Mahmoudi M, Sahraian MA, Shokrgozar MA, Laurent S. Superparamagnetic iron oxide nanoparticles: Promises for diagnosis and treatment of multiple sclerosis. ACS Chemical Neuroscience. 2011;2:118–40. doi: 10.1021/cn100100e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mahmoudi M, Amiri H, Shokrgozar MA, Sasanpour P, Rashidian B, Laurent S, Casula MF, Lascialfari A. Raman active jagged-shaped gold-coated magnetic particles as a novel multimodal nanoprobe. Chemical Communications. 2011;47:10404–6. doi: 10.1039/c1cc13413b. [DOI] [PubMed] [Google Scholar]
- 51.Mahmoudi M, Simchi A, Imani M. Recent advances in surface engineering of superparamagnetic iron oxide nanoparticles for biomedical applications. Journal of the Iranian Chemical Society. 2010;7:S1–S27. [Google Scholar]
- 52.Laurent S, Forge D, Port M, Roch A, Robic C, Vander Elst L, Muller RN. Magnetic Iron Oxide Nanoparticles: Synthesis, Stabilization, Vectorization, Physicochemical Characterizations, and Biological Applications. Chemical Reviews. 2008;108:2064–110. doi: 10.1021/cr068445e. [DOI] [PubMed] [Google Scholar]
- 53.Laurent S, Boutry S, Mahieu I, Vander Elst L, Muller RN. Iron Oxide Based MR Contrast Agents: from Chemistry to Cell Labeling. Current Medicinal Chemistry. 2009;16:4712–27. doi: 10.2174/092986709789878256. [DOI] [PubMed] [Google Scholar]
- 54.Fukukura Y, Kamiyama T, Takumi K, Shindo T, Higashi R, Nakajo M. Comparison of ferucar-botran-enhanced fluid-attenuated inversion-recovery echo-planar, T2-weighted turbo spinecho, T2*-weighted gradient-echo, and diffusion-weighted echo-planar imaging for detection of malignant liver lesions. Journal of Magnetic Resonance Imaging. 2010;31:607–16. doi: 10.1002/jmri.22098. [DOI] [PubMed] [Google Scholar]
- 55.Saito K, Sugimoto K, Nishio R, Araki Y, Moriyasu F, Kakizaki D, Tokuuye K. Perfusion study of liver lesions with superparamagnetic iron oxide: distinguishing hepatocellular carcinoma from focal nodular hyperplasia. Clinical imaging. 2009;33:447–53. doi: 10.1016/j.clinimag.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 56.Santoro L, Grazioli L, Filippone A, Grassedonio E, Belli G, Colagrande S. Resovist enhanced MR imaging of the liver: Does quantitative assessment help in focal lesion classification and characterization? Journal of Magnetic Resonance Imaging. 2009;30:1012–20. doi: 10.1002/jmri.21937. [DOI] [PubMed] [Google Scholar]
- 57.Meier R, Henning TD, Boddington S, Tavri S, Arora S, Piontek G, Rudelius M, Corot C, Daldrup-Link HE. Breast Cancers: MR Imaging of Folate-Receptor Expression with the Folate-Specific Nanoparticle P1133. Radiology. 2010;255:527–35. doi: 10.1148/radiol.10090050. [DOI] [PubMed] [Google Scholar]
- 58.Radermacher KA, Boutry S, Laurent S, Elst LV, Mahieu I, Bouzin C, Magat J, Gregoire V, Feron O, Muller RN, Jordan BF, Gallez B. Iron oxide particles covered with hexapeptides targeted at phosphatidylserine as MR biomarkers of tumor cell death. Contrast Media & Molecular Imaging. 2010;5:258–67. doi: 10.1002/cmmi.382. [DOI] [PubMed] [Google Scholar]
- 59.Nasongkla N, Bey E, Ren J, Ai H, Khemtong C, Guthi JS, Chin SF, Sherry AD, Boothman DA, Gao J. Multifunctional Polymeric Micelles as Cancer-Targeted, MRI-Ultrasensitive Drug Delivery Systems. Nano Letters. 2006;6:2427–30. doi: 10.1021/nl061412u. [DOI] [PubMed] [Google Scholar]
- 60.Winter PM, Caruthers SD, Allen JS, Cai K, Williams TA, Lanza GM, Wickline SA. Molecular imaging of angiogenic therapy in peripheral vascular disease with ανβ3-integrin-targeted nanoparticles. Magnetic Resonance in Medicine. 2010;64:369–76. doi: 10.1002/mrm.22447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Park J, An K, Hwang Y, Park JG, Noh HJ, Kim JY, Park JH, Hwang NM, Hyeon T. Ultra-large-scale syntheses of monodisperse nanocrystals. Nat Mater. 2004;3:891–5. doi: 10.1038/nmat1251. [DOI] [PubMed] [Google Scholar]
- 62.Mahmoudi M, Milani AS, Stroeve P. Synthesis, surface architecture and biological response of superparamagnetic iron oxide nanoparticles for application in drug delivery: a review. International Journal of Biomedical Nanoscience and Nanotechnology. 2010;1:164–201. [Google Scholar]
- 63.Wang X, Zhuang J, Peng Q, Li Y. A general strategy for nanocrystal synthesis. Nature. 2005;437:121–4. doi: 10.1038/nature03968. [DOI] [PubMed] [Google Scholar]
- 64.Khan Y, Durrani SK, Siddique M, Mehmood M. Hydrothermal synthesis of alpha Fe2O3 nanoparticles capped by Tween-80. Materials Letters. 2011;65:2224–7. [Google Scholar]
- 65.Sun S, Zeng H, Robinson DB, Raoux S, Rice PM, Wang SX, Li G. Monodisperse MFe2O4 (M = Fe, Co, Mn) Nanoparticles. Journal of the American Chemical Society. 2004;14:273–9. doi: 10.1021/ja0380852. [DOI] [PubMed] [Google Scholar]
- 66.Chikate RC, Jun KW, Rode CV. Nonaqueous synthesis and characterization of capped -±£ Fe2O3 nanoparticles from iron(III) hydroxyoleate precursor. Polyhedron. 2008;27:933–8. [Google Scholar]
- 67.Dresco PA, Zaitsev VS, Gambino RJ, Chu B. Preparation and Properties of Magnetite and Polymer Magnetite Nanoparticles. Langmuir. 1999;15:1945–51. [Google Scholar]
- 68.Narita A, Naka K, Chujo Y. Facile control of silica shell layer thickness on hydrophilic iron oxide nanoparticles via reverse micelle method. Colloids and Surfaces A: Physicochemical and Engineering Aspects. 2009;336:46–56. [Google Scholar]
- 69.Lu A-H, Salabas EL, Schüth F. Magnetic Nanoparticles: Synthesis, Protection, Function-alization, and Application. Angewandte Chemie International Edition. 2007;46:1222–44. doi: 10.1002/anie.200602866. [DOI] [PubMed] [Google Scholar]
- 70.Shen L, Stachowiak A, Fateen S-EK, Laibinis PE, Hatton TA. Structure of Alkanoic Acid Stabilized Magnetic Fluids. A Small-Angle Neutron and Light Scattering Analysis. Langmuir. 2000;17:288–99. [Google Scholar]
- 71.Boyer C, Whittaker MR, Bulmus V, Liu J, Davis TP. The design and utility of polymer-stabilized iron-oxide nanoparticles for nanomedicine applications. NPG Asia Materials. 2010;2:23–30. [Google Scholar]
- 72.Hong RY, Feng B, Chen LL, Liu GH, Li HZ, Zheng Y, Wei DG. Synthesis, characterization and MRI application of dextran-coated Fe3O4 magnetic nanoparticles. Biochemical Engineering Journal. 2008;42:290–300. [Google Scholar]
- 73.Saboktakin MR, Tabatabaie RM, Maharramov A, Ramazanov MA. A synthetic macromolecule as MRI detectable drug carriers: Aminodextran -coated iron oxide nanoparticles. Carbohydrate Polymers. 2010;80:695–8. [Google Scholar]
- 74.Corot C, Robert P, Idee JM, Port M. Recent advances in iron oxide nanocrystal technology for medical imaging. Advanced Drug Delivery Reviews. 2006;58:1471–504. doi: 10.1016/j.addr.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 75.Gomez-Lopera SA, Arias JL, Gallardo V, Delgado AV. Colloidal Stability of Magnetite/ Poly(lactic acid) Core/Shell Nanoparticles. Langmuir. 2006;22:2816–21. doi: 10.1021/la0530079. [DOI] [PubMed] [Google Scholar]
- 76.Arias JL, Gallardo V, oacute, mez-Lopera SA, Delgado AV. Loading of 5-Fluorouracil to Poly (ethyl-2-cyanoacrylate) Nanoparticles with a Magnetic Core. Journal of Biomedical Nanotechnology. 2005;1:214–23. [Google Scholar]
- 77.Molday RS, Mackenzie D. Immunospecific ferromagnetic iron-dextran reagents for the labeling and magnetic separation of cells. Journal of Immunological Methods. 1982;52:353–67. doi: 10.1016/0022-1759(82)90007-2. [DOI] [PubMed] [Google Scholar]
- 78.Lunov O, Syrovets T, Büchele B, Jiang X, Röcker C, Tron K, Nienhaus GU, Walther P, Mailänder V, Landfester K, Simmet T. The effect of carboxydextran-coated superparamagnetic iron oxide nanoparticles on c-Jun N-terminal kinase-mediated apoptosis in human macrophages. Biomaterials. 2010;31:5063–71. doi: 10.1016/j.biomaterials.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 79.Mouaziz H, Veyret R, Theretz A, Ginot F, ric, Elaissari A. Aminodextran Containing Magnetite Nanoparticles for Molecular Biology Applications: Preparation and Evaluation. Journal of Biomedical Nanotechnology. 2009;5:172–81. doi: 10.1166/jbn.2009.1023. [DOI] [PubMed] [Google Scholar]
- 80.Paul KG, Frigo TB, Groman JY, Groman EV. Synthesis of Ultrasmall Superparamagnetic Iron Oxides Using Reduced Polysaccharides. Bioconjugate Chemistry. 2004;15:394–401. doi: 10.1021/bc034194u. [DOI] [PubMed] [Google Scholar]
- 81.Kampert E, Janssen FFBJ, Boukhvalov DW, Russcher JC, Smits JMM, de Gelder R, de Bruin B, Christianen PC, Zeitler U, Katsnelson MI, Maan JC, Rowan AE. Ligand-Controlled Magnetic Interactions in Mn4 Clusters. Inorganic Chemistry. 2009;48:11903–8. doi: 10.1021/ic901930w. [DOI] [PubMed] [Google Scholar]
- 82.Chu WJ. Surface properties of superparamagnetic iron oxide MR contrast agents: Ferumoxides, ferumoxtran, ferumoxsil. Magnetic Resonance Imaging. 1995;13:675–91. doi: 10.1016/0730-725x(95)00023-a. [DOI] [PubMed] [Google Scholar]
- 83.Carmen Bautista M, Bomati-Miguel O, del Puerto Morales Ma, Serna CJ, Veintemillas-Verdaguer S. Surface characterisation of dextran-coated iron oxide nanoparticles prepared by laser pyrolysis and coprecipitation. Journal of Magnetism and Magnetic Materials. 2005;293:20–7. [Google Scholar]
- 84.Anzai Y, McLachlan S, Morris M, Saxton R, Lufkin RB. Dextran-coated superparamagnetic iron oxide, an MR contrast agent for assessing lymph nodes in the head and neck. American Journal of Neuroradiology. 1994;15:87–94. [PMC free article] [PubMed] [Google Scholar]
- 85.Bourrinet P, Bengele HH, Bonnemain B, Dencausse A, Idee JM, Jacobs PM, Lewis JM. Pre-clinical Safety and Pharmacokinetic Profile of Ferumoxtran-10, an Ultrasmall Superparamagnetic Iron Oxide Magnetic Resonance Contrast Agent. Investigative Radiology. 2006;41:313–24. doi: 10.1097/01.rli.0000197669.80475.dd. [DOI] [PubMed] [Google Scholar]
- 86.Bellin MF, Beigelman C, Precetti-Morel S. Iron oxide-enhanced MR lymphography: initial experience. European Journal of Radiology. 2000;34:257–64. doi: 10.1016/s0720-048x(00)00204-7. [DOI] [PubMed] [Google Scholar]
- 87.Clement O, Siauve N, Cuénod CA, Frija G. Liver Imaging With Ferumoxides (Feridex(R)): Fundamentals, Controversies, and Practical Aspects. Topics in Magnetic Resonance Imaging. 1998;9:167–82. [PubMed] [Google Scholar]
- 88.Mornet Sp, Portier J, Duguet E. A method for synthesis and functionalization of ultrasmall superparamagnetic covalent carriers based on maghemite and dextran. Journal of Magnetism and Magnetic Materials. 2005;293:127–34. [Google Scholar]
- 89.Catherine CB, Adam SGC. Functionalisation of magnetic nanoparticles for applications in biomedicine. Journal of Physics D: Applied Physics. 2003;36:R198. [Google Scholar]
- 90.Wapner K, Grundmeier G. Spectroscopic analysis of the interface chemistry of ultra-thin plasma polymer films on iron. Surface and Coatings Technology. 2005;200:100–3. [Google Scholar]
- 91.Love JC, Estroff LA, Kriebel JK, Nuzzo RG, Whitesides GM. Self-Assembled Monolayers of Thiolates on Metals as a Form of Nanotechnology. Chemical Reviews. 2005;105:1103–70. doi: 10.1021/cr0300789. [DOI] [PubMed] [Google Scholar]
- 92.Chen Y, Liu W, Ye C, Yu L, Qi S. Preparation and characterization of self-assembled alkanephosphate monolayers on glass substrate coated with nano-TiO2 thin film. Materials Research Bulletin. 2001;36:2605–12. [Google Scholar]
- 93.Arbab AS, Wilson LB, Ashari P, Jordan EK, Lewis BK, Frank JA. A model of lysosomal metabolism of dextran coated superparamagnetic iron oxide (SPIO) nanoparticles: implications for cellular magnetic resonance imaging. NMR in Biomedicine. 2005;18:383–9. doi: 10.1002/nbm.970. [DOI] [PubMed] [Google Scholar]
- 94.Kim DK, Mikhaylova M, Wang FH, Kehr J, Bjelke Br, Zhang Y, Tsakalakos T, Muhammed Mamoun. Starch-Coated Superparamagnetic Nanoparticles as MR Contrast Agents. Chemistry of Materials. 2003;15:4343–51. [Google Scholar]
- 95.Lee HS, Hee Kim E, Shao H, Kook Kwak B. Synthesis of SPIO-chitosan microspheres for MRI-detectable embolotherapy. Journal of Magnetism and Magnetic Materials. 2005;293:102–5. [Google Scholar]
- 96.Huang HY, Shieh YT, Shih CM, Twu YK. Magnetic chitosan/iron (II, III) oxide nanoparticles prepared by spray-drying. Carbohydrate Polymers. 2010;81:906–10. [Google Scholar]
- 97.Reimer P, Marx C, Rummeny EJ, Müller M, Lentschig M, Balzer T, Dietl KH, Sulkowski U, Berns T, Shamsi K, Peters PE. SPIO-enhanced 2D-TOF MR angiography of the portal venous system: Results of an intraindividual comparison. Journal of Magnetic Resonance Imaging. 1997;7:945–9. doi: 10.1002/jmri.1880070602. [DOI] [PubMed] [Google Scholar]
- 98.Holgado MA, Alvarez-Fuentes J, Fernández-Arévalo M, Arias JL. Possibilities of Poly(D,L-lactide-co-glycolide) in the Formulation of Nanomedicines Against Cancer. Current Drug Targets. 2011;12:1096–111. doi: 10.2174/138945011795906606. [DOI] [PubMed] [Google Scholar]
- 99.Hu FX, Neoh KG, Kang ET. Synthesis and in vitro anti-cancer evaluation of tamoxifen-loaded magnetite/PLLA composite nanoparticles. Biomaterials. 2006;27:5725–33. doi: 10.1016/j.biomaterials.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 100.Bulte JWM, Cuyper Md, Despres D, Frank JA. Preparation, relaxometry, and biokinetics of PEGylated magnetoliposomes as MR contrast agent. Journal of Magnetism and Magnetic Materials. 1999;194:204–9. [Google Scholar]
- 101.Shultz MD, Calvin S, Fatouros PP, Morrison SA, Carpenter EE. Enhanced ferrite nanoparticles as MRI contrast agents. Journal of Magnetism and Magnetic Materials. 2007;311:464–8. [Google Scholar]
- 102.Ai H, Flask C, Weinberg B, Shuai XT, Pagel MD, Farrell D, Duerk J, Gao J. Magnetite-Loaded Polymeric Micelles as Ultrasensitive Magnetic-Resonance Probes. Advanced Materials. 2005;17:1949–52. [Google Scholar]
- 103.Li Z, Wei L, Gao MY, Lei H. One-Pot Reaction to Synthesize Biocompatible Magnetite Nanoparticles. Advanced Materials. 2005;17:1001–5. [Google Scholar]
- 104.Sun C, Veiseh O, Gunn J, Fang C, Hansen S, Lee D, Sze R, Ellenbogen RG, Olson J, Zhang M. In Vivo MRI Detection of Gliomas by Chlorotoxin-Conjugated Superparamagnetic. Nano-probes Small. 2008;4:372–9. doi: 10.1002/smll.200700784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dodd CH, Hsu HC, Chu WJ, Yang P, Zhang HG, Mountz JD, Jr, Zinn K, Forder J, Josephson L, Weissleder R, Mountz JM, Mountz JD. Normal T-cell response and in vivo magnetic resonance imaging of T cells loaded with HIV trans-activator-peptide-derived superparamagnetic nanoparticles. Journal of Immunological Methods. 2001;256:89–105. doi: 10.1016/s0022-1759(01)00433-1. [DOI] [PubMed] [Google Scholar]
- 106.Sun C, Sze R, Zhang M. Folic acid-PEG conjugated superparamagnetic nanoparticles for targeted cellular uptake and detection by MRI. Journal of Biomedical Materials Research Part A. 2006;78:550–7. doi: 10.1002/jbm.a.30781. [DOI] [PubMed] [Google Scholar]
- 107.Zhang Y, Zhang J. Surface modification of monodisperse magnetite nanoparticles for improved intracellular uptake to breast cancer cells. Journal of Colloid and Interface Science. 2005;283:352–7. doi: 10.1016/j.jcis.2004.09.042. [DOI] [PubMed] [Google Scholar]
- 108.Xu C, Xu K, Gu H, Zheng R, Liu H, Zhang X, Guo Z, Xu B. Dopamine as A Robust Anchor to Immobilize Functional Molecules on the Iron Oxide Shell of Magnetic Nanoparticles. Journal of the American Chemical Society. 2004;126:9938–9. doi: 10.1021/ja0464802. [DOI] [PubMed] [Google Scholar]
- 109.Raty JK, Liimatainen T, Wirth T, Airenne KJ, Ihalainen TO, Huhtala T, Hamerlynck E, Vihinen-Ranta M, Närvänen A, Ylä-Herttuala S, Hakumäki JM. Magnetic resonance imaging of viral particle biodistribution in vivo. Gene Ther. 2006;13:1440–6. doi: 10.1038/sj.gt.3302828. [DOI] [PubMed] [Google Scholar]
- 110.Schellenberger E, Schnorr J, Reutelingsperger C, Ungethüm L, Meyer W, Taupitz M, Hamm B. Linking Proteins with Anionic Nanoparticles via Protamine: Ultrasmall Protein-Coupled Probes for Magnetic Resonance Imaging of Apoptosis. Small. 2008;4:225–30. doi: 10.1002/smll.200700847. [DOI] [PubMed] [Google Scholar]
- 111.Hodenius MAJ, Niendorf T, Krombach GA, Richtering W, Eckert T, Lueken H, Speldrich M, Günther RW, Baumann M, Soenen SJ, De Cuyper M, Schmitz-Rode T. Synthesis, Physicochemical Characterization and MR Relaxometry of Aqueous Ferrofluids. Journal of Nanoscience and Nanotechnology. 2008;8:2399–409. doi: 10.1166/jnn.2008.312. [DOI] [PubMed] [Google Scholar]
- 112.Racuciu M, Creanga D, Airinei A. Citric-acid-coated magnetite nanoparticles for biological applications. The European Physical Journal E: Soft Matter and Biological Physics. 2006;21:117–21. doi: 10.1140/epje/i2006-10051-y. [DOI] [PubMed] [Google Scholar]
- 113.Sahoo Y, Pizem H, Fried T, Golodnitsky D, Burstein L, Sukenik CN, Markovich G. Alkyl Phosphonate/Phosphate Coating on Magnetite Nanoparticles: A Comparison with Fatty Acids. Langmuir. 2001;17:7907–11. [Google Scholar]
- 114.White MA, Johnson JA, Koberstein JT, Turro NJ. Toward the Syntheses of Universal Ligands for Metal Oxide Surfaces: Controlling Surface Functionality through Click Chemistry. Journal of the American Chemical Society. 2006;128:11356–7. doi: 10.1021/ja064041s. [DOI] [PubMed] [Google Scholar]
- 115.Auernheimer J, Zukowski D, Dahmen C, Kantlehner M, Enderle A, Goodman SL, Kessler H. Titanium Implant Materials with Improved Biocompatibility through Coating with Phosphonate-Anchored Cyclic RGD Peptides. ChemBioChem. 2005;6:2034–40. doi: 10.1002/cbic.200500031. [DOI] [PubMed] [Google Scholar]
- 116.Mohapatra S, Pramanik P. Synthesis and stability of functionalized iron oxide nanoparticles using organophosphorus coupling agents. Colloids and Surfaces A: Physicochemical and Engineering Aspects. 2009;339:35–42. [Google Scholar]
- 117.Barja BC, Herszage J, dos Santos Afonso M. Iron(III)-phosphonate complexes. Polyhedron. 2001;20:1821–30. [Google Scholar]
- 118.Fauconnier N, Pons JN, Roger J, Bee A. Thiolation of Maghemite Nanoparticles by Dimercap-tosuccinic Acid. Journal of Colloid and Interface Science. 1997;194:427–33. doi: 10.1006/jcis.1997.5125. [DOI] [PubMed] [Google Scholar]
- 119.Halbreich A, Roger J, Pons JN, Geldwerth D, Da Silva MF, Roudier M, Bacri JC. Biomedical applications of maghemite ferrofluid. Biochimie. 1998;80:379–90. doi: 10.1016/s0300-9084(00)80006-1. [DOI] [PubMed] [Google Scholar]
- 120.Barnakov YA, Yu MH, Rosenzweig Z. Manipulation of the Magnetic Properties of Magnetite-Silica Nanocomposite Materials by Controlled Stober Synthesis. Langmuir. 2005;21:7524–7. doi: 10.1021/la0508893. [DOI] [PubMed] [Google Scholar]
- 121.Im SH, Herricks T, Lee YT, Xia Y. Synthesis and characterization of monodisperse silica colloids loaded with superparamagnetic iron oxide nanoparticles. Chemical Physics Letters. 2005;401:19–23. [Google Scholar]
- 122.Galvin P, Thompson D, Ryan K, McCarthy A, Moore AC, Burke CS, Dyson M, Maccraith BD, Gun'ko YK, Byrne MT, Volkov Y, Keely C, Keehan E, Howe M, Duffy C, Macloughlin R. Nanoparticle-based drug delivery: case studies for cancer and cardiovascular applications. Cellular and Molecular Life Sciences. 2011 doi: 10.1007/s00018-011-0856-6. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sun EY, Josephson L, Kelly KA, Weissleder R. Development of Nanoparticle Libraries for Biosensing. Bioconjugate Chemistry. 2005;17:109–13. doi: 10.1021/bc050290e. [DOI] [PubMed] [Google Scholar]
- 124.Jung HI, Kettunen MI, Davletov B, Brindle KM. Detection of Apoptosis Using the C2A Domain of Synaptotagmin I. Bioconjugate Chemistry. 2004;15:983–7. doi: 10.1021/bc049899q. [DOI] [PubMed] [Google Scholar]
- 125.Artemov D, Mori N, Okollie B, Bhujwalla ZM. MR molecular imaging of the Her-2/neu receptor in breast cancer cells using targeted iron oxide nanoparticles. Magnetic Resonance in Medicine. 2003;49:403–8. doi: 10.1002/mrm.10406. [DOI] [PubMed] [Google Scholar]
- 126.Go KG, Bulte JWM, de Ley L, The TH, Kamman RL, Hulstaert CE, Blaauw EH, Ma LD. Our approach towards developing a specific tumour-targeted MRI contrast agent for the brain. European Journal of Radiology. 1993;16:171–5. doi: 10.1016/0720-048x(93)90064-t. [DOI] [PubMed] [Google Scholar]
- 127.Johansson LO, Bjørnerud A, Ahlström HK, Ladd DL, Fujii DK. A targeted contrast agent for magnetic resonance imaging of thrombus: Implications of spatial resolution. Journal of Magnetic Resonance Imaging. 2001;13:615–8. doi: 10.1002/jmri.1086. [DOI] [PubMed] [Google Scholar]
- 128.Kresse M, Wagner S, Pfefferer D, Lawaczeck R, Elste V, Semmler W. Targeting of ultrasmall superparamagnetic iron oxide (USPIO) particles to tumor cells in Vivo by using transferrin receptor pathways. Magnetic Resonance in Medicine. 1998;40:236–42. doi: 10.1002/mrm.1910400209. [DOI] [PubMed] [Google Scholar]
- 129.Zhao M, Beauregard DA, Loizou L, Davletov B, Brindle KM. Non-invasive detection of apoptosis using magnetic resonance imaging and a targeted contrast agent. Nat Med. 2001;7:1241–4. doi: 10.1038/nm1101-1241. [DOI] [PubMed] [Google Scholar]
- 130.Weissleder R, Lee AS, Fischman AJ, Reimer P, Shen T, Wilkinson R, Callahan RJ, Brady TJ. Polyclonal human immunoglobulin G labeled with polymeric iron oxide: antibody MR imaging. Radiology. 1991;181:245–9. doi: 10.1148/radiology.181.1.1887040. [DOI] [PubMed] [Google Scholar]
- 131.Toma A, Otsuji E, Kuriu Y, Okamoto K, Ichikawa D, Hagiwara A, Ito H, Nishimura T, Yamagishi H. Monoclonal antibody A7-superparamagnetic iron oxide as contrast agent of MR imaging of rectal carcinoma. Br J Cancer. 2005;93:131–6. doi: 10.1038/sj.bjc.6602668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bulte JWM, Zhang SC, van Gelderen P, Herynek V, Jordan EK, Duncan ID, Frank JA. Neuro-transplantation of magnetically labeled oli-godendrocyte progenitors: Magnetic resonance tracking of cell migration and myelina-tion. Proceedings of the National Academy of Sciences. 1999;96:15256–61. doi: 10.1073/pnas.96.26.15256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.van Everdingen KJ, Enochs WS, Bhide PG, Nossiff N, Papisov M, Bogdanov A, Jr, Brady TJ, Weissleder R. Determinants of in vivo MR imaging of slow axonal transport. Radiology. 1994;193:485–91. doi: 10.1148/radiology.193.2.7526413. [DOI] [PubMed] [Google Scholar]
- 134.Hogemann D, Josephson L, Weissleder R, Basilion JP. Improvement of MRI Probes To Allow Efficient Detection of Gene Expression. Bioconjugate Chemistry. 2000;11:941–6. doi: 10.1021/bc000079x. [DOI] [PubMed] [Google Scholar]
- 135.Josephson L, Tung CH, Moore A, Weissleder R. High-Efficiency Intracellular Magnetic Labeling with Novel Superparamagnetic-Tat Peptide Conjugates. Bioconjugate Chemistry. 1999;10:186–91. doi: 10.1021/bc980125h. [DOI] [PubMed] [Google Scholar]
- 136.Montet X, Weissleder R, Josephson L. Imaging Pancreatic Cancer with a Peptide Nanoparticle Conjugate Targeted to Normal Pancreas. Bioconjugate Chemistry. 2006;17:905–11. doi: 10.1021/bc060035+. [DOI] [PubMed] [Google Scholar]
- 137.Tsourkas A, Shinde-Patil VR, Kelly KA, Patel P, Wolley A, Allport JR, Weissleder R. In Vivo Imaging of Activated Endothelium Using an Anti-VCAM-1 Magnetooptical Probe. Bioconjugate Chemistry. 2005;16:576–81. doi: 10.1021/bc050002e. [DOI] [PubMed] [Google Scholar]
- 138.Montet X, Funovics M, Montet-Abou K, Weissleder R, Josephson L. Multivalent Effects of RGD Peptides Obtained by Nanoparticle Display. Journal of Medicinal Chemistry. 2006;49:6087–93. doi: 10.1021/jm060515m. [DOI] [PubMed] [Google Scholar]
- 139.Kelly KA, Allport JR, Tsourkas A, Shinde-Patil VR, Josephson L, Weissleder R. Detection of Vascular Adhesion Molecule-1 Expression Using a Novel Multimodal Nanoparticle. Circulation Research. 2005;96:327–36. doi: 10.1161/01.RES.0000155722.17881.dd. [DOI] [PubMed] [Google Scholar]
- 140.Huh YM, Jun Yw, Song HT, Kim S, Choi Js, Lee JH, Yoon S, Kim KS, Shin JS, Suh JS, Cheon J. In Vivo Magnetic Resonance Detection of Cancer by Using Multifunctional Magnetic Nanocrystals. Journal of the American Chemical Society. 2005;127:12387–91. doi: 10.1021/ja052337c. [DOI] [PubMed] [Google Scholar]
- 141.Chen ZP, Zhang Y, Zhang S, Xia JG, Liu JW, Xu K, Gu N. Preparation and characterization of water-soluble monodisperse magnetic iron oxide nanoparticles via surface double-exchange with DMSA. Colloids and Surfaces A: Physicochemical and Engineering Aspects. 2008;316:210–6. [Google Scholar]
- 142.Cao JQ, Wang YX, Yu JF, Xia JY, Zhang CF, Yin DZ, Häfeli, Urs O. Preparation and radiolabeling of surface-modified magnetic nanoparticles with rhenium-188 for magnetic targeted radiotherapy. Journal of Magnetism and Magnetic Materials. 2004;277:165–74. [Google Scholar]
- 143.Daou TJ, Pourroy G, Greneche JM, Bertin A, Felder-Flesch D, Begin-Colin S. Water soluble dendronized iron oxide nanoparticles. Dalton Trans. 2009:4442–9. doi: 10.1039/b823187g. [DOI] [PubMed] [Google Scholar]
- 144.Whitehead RA, Chagnon MS, Groman EV, Josephson L. Magnetic particles for use in separations, US Patent 4,695,392, 1987.
- 145.Arkles B. Tailoring surfaces with silanes. Chem Tech. 1977;7:766. [Google Scholar]
- 146.Brandriss S, Margel S. Synthesis and characterization of self-assembled hydrophobic monolayer coatings on silica colloids. Langmuir. 1993;9:1232–40. [Google Scholar]
- 147.Zablotskaya A, Segal I, Maiorov M, Zablotsky D, Mishnev A, Lukevics E, Shestakova I, Domracheva I. Synthesis and characterization of nanoparticles with an iron oxide magnetic core and a biologically active trialkylsilylated aliphatic alkanolamine shell. Journal of Magnetism and Magnetic Materials. 2007;311:135–9. [Google Scholar]
- 148.Sun EY, Josephson L, Weissleder R. “Clickable” Nanoparticles for Targeted Imaging. Molecular Imaging. 2006;5:1535–3508. [PubMed] [Google Scholar]
- 149.Shukoor MI, Natalio F, Therese HA, Tahir MN, Ksenofontov V, Panthofer M, et al. Fabrication of a Silica Coating on Magnetic γ-Fe2O3 Nanoparticles by an Immobilized Enzyme. Chemistry of Materials. 2008;20:3567–73. [Google Scholar]
- 150.Martin A, Hickey J, Ablack A, Lewis J, Luyt L, Gillies E. Synthesis of bombesin-functionalized iron oxide nanoparticles and their specific uptake in prostate cancer cells. Journal of Nanoparticle Research. 2010;12:1599–608. doi: 10.1007/s11051-009-9681-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Widder KJ, Senyei AE, Ranney DF. Magnetically responsive microspheres and other carriers for the biophysical targeting of antitumor agents. Advances in Pharmacology and Chemotherapy. 1979;16:213–71. doi: 10.1016/s1054-3589(08)60246-x. [DOI] [PubMed] [Google Scholar]
- 152.Devineni D, Blanton CD, Gallo JM. Preparation and in vitro Evaluation of Magnetic Micro-sphere-Methotrexate Conjugate Drug Delivery Systems. Bioconjugate Chemistry. 1995;6:203–10. doi: 10.1021/bc00032a008. [DOI] [PubMed] [Google Scholar]
- 153.Febvay S, Marini DM, Belcher AM, Clapham DE. Targeted Cytosolic Delivery of Cell-Impermeable Compounds by Nanoparticle-Mediated, Light-Triggered Endosome Disruption. Nano Letters. 2010;10:2211–9. doi: 10.1021/nl101157z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Gao W, Chan JM, Farokhzad OC. pH-Responsive Nanoparticles for Drug Delivery. Molecular Pharmaceutics. 2010;7:1913–20. doi: 10.1021/mp100253e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hammond PT. Virtual Issue on Nanomaterials for Drug Delivery. ACS Nano. 2011;5:681–4. doi: 10.1021/nn2003508. [DOI] [PubMed] [Google Scholar]
- 156.Hu SH, Liu TY, Huang HY, Liu DM, Chen SY. Magnetic-Sensitive Silica Nanospheres for Controlled Drug Release. Langmuir. 2007;24:239–44. doi: 10.1021/la701570z. [DOI] [PubMed] [Google Scholar]
- 157.Jin Q, Mitschang F, Agarwal S. Biocompatible Drug Delivery System for Photo-Triggered Controlled Release of 5-Fluorouracil. Biomacro-molecules. 2011;12:3684–91. doi: 10.1021/bm2009125. [DOI] [PubMed] [Google Scholar]
- 158.Kamaly N, Kalber T, Thanou M, Bell JD, Miller AD. Folate Receptor Targeted Bimodal Lipo-somes for Tumor Magnetic Resonance Imaging. Bioconjugate Chemistry. 2009;20:648–55. doi: 10.1021/bc8002259. [DOI] [PubMed] [Google Scholar]
- 159.Kang H, Trondoli AC, Zhu G, Chen Y, Chang YJ, Liu H, Huang YF, Zhang X, Tan W. Near-Infrared Light-Responsive Core-Shell Nanogels for Targeted Drug Delivery. ACS Nano. 2011;5:5094–9. doi: 10.1021/nn201171r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Park J, Gao W, Whiston R, Strom TB, Metcalfe S, Fahmy TM. Modulation of CD4+ T Lymphocyte Lineage Outcomes with Targeted, Nanoparticle-Mediated Cytokine Delivery. Molecular Pharmaceutics. 2010;8:143–52. doi: 10.1021/mp100203a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Shi J, Votruba AR, Farokhzad OC, Langer R. Nanotechnology in Drug Delivery and Tissue Engineering: From Discovery to Applications. Nano Letters. 2010;10:3223–30. doi: 10.1021/nl102184c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Shi J, Xiao Z, Kamaly N, Farokhzad OC. Self-Assembled Targeted Nanoparticles: Evolution of Technologies and Bench to Bedside Translation. Accounts of Chemical Research. 2011;44:1123–34. doi: 10.1021/ar200054n. [DOI] [PubMed] [Google Scholar]
- 163.Sigot V, Arndt-Jovin DJ, Jovin TM. Targeted Cellular Delivery of Quantum Dots Loaded on and in Biotinylated Liposomes. Bioconjugate Chemistry. 2010;21:1465–72. doi: 10.1021/bc100054c. [DOI] [PubMed] [Google Scholar]
- 164.Singh A, Dilnawaz F, Mewar S, Sharma U, Jagannathan NR, Sahoo SK. Composite Polymeric Magnetic Nanoparticles for Co-Delivery of Hydrophobic and Hydrophilic Anticancer Drugs and MRI Imaging for Cancer Therapy. ACS Applied Materials & Interfaces. 2011;3:842–56. doi: 10.1021/am101196v. [DOI] [PubMed] [Google Scholar]
- 165.Singh P, Gupta U, Asthana A, Jain NK. Folate and Folate-PEG-PAMAM Dendrimers: Synthesis, Characterization, and Targeted Anticancer Drug Delivery Potential in Tumor Bearing Mice. Bioconjugate Chemistry. 2008;19:2239–52. doi: 10.1021/bc800125u. [DOI] [PubMed] [Google Scholar]
- 166.Yu X, Pishko MV. Nanoparticle-Based Biocompatible and Targeted Drug Delivery: Characterization and in Vitro Studies. Biomacromolecules. 2011;12:3205–12. doi: 10.1021/bm200681m. [DOI] [PubMed] [Google Scholar]
- 167.Zeng F, Lee H, Allen C. Epidermal Growth Factor-Conjugated Poly(ethylene glycol)-block-Poly(delta-valerolactone) Copolymer Micelles for Targeted Delivery of Chemotherapeutics. Bioconjugate Chemistry. 2006;17:399–409. doi: 10.1021/bc050350g. [DOI] [PubMed] [Google Scholar]
- 168.Zhu Y, Fang Y, Kaskel S. Folate-Conjugated Fe3O4@SiO2 Hollow Mesoporous Spheres for Targeted Anticancer Drug Delivery. The Journal of Physical Chemistry C. 2010;114:16382–8. [Google Scholar]
- 169.Zou P, Yu Y, Wang YA, Zhong Y, Welton A, Galban C, Wang S, Sun D. Superparamagnetic Iron Oxide Nanotheranostics for Targeted Cancer Cell Imaging and pH-Dependent Intracellular Drug Release. Molecular Pharmaceutics. 2010;7:1974–84. doi: 10.1021/mp100273t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Cuenca AG, Jiang H, Hochwald SN, Delano M, Cance WG, Grobmyer SR. Emerging implications of nanotechnology on cancer diagnostics and therapeutics. Cancer. 2006;107:459–66. doi: 10.1002/cncr.22035. [DOI] [PubMed] [Google Scholar]
- 171.Brigger In, Dubernet C, Couvreur P. Nanoparticles in cancer therapy and diagnosis. Advanced Drug Delivery Reviews. 2002;54:631–51. doi: 10.1016/s0169-409x(02)00044-3. [DOI] [PubMed] [Google Scholar]
- 172.Gruttner C, Muller K, Teller J, Westphal F, Foreman A, Ivkov R. Synthesis and antibody conjugation of magnetic nanoparticles with improved specific power absorption rates for alternating magnetic field cancer therapy. Journal of Magnetism and Magnetic Materials. 2007;311:181–6. [Google Scholar]
- 173.Pantic I. Magnetic nanoparticles in cancer diagnosis and treatment: novel approaches. Reviews on Advanced Materials Science. 2010;26:67–73. [Google Scholar]
- 174.Creixell M, Herrera AP, Ayala V, Latorre-Esteves M, Perez-Torres M, Torres-Lugo M, Rinaldi C. Preparation of epidermal growth factor (EGF) conjugated iron oxide nanoparticles and their internalization into colon cancer cells. Journal of Magnetism and Magnetic Materials. 2010;322:2244–50. [Google Scholar]
- 175.Dilnawaz F, Singh A, Mohanty C, Sahoo SK. Dual drug loaded superparamagnetic iron oxide nanoparticles for targeted cancer therapy. Biomaterials. 2010;31:3694–706. doi: 10.1016/j.biomaterials.2010.01.057. [DOI] [PubMed] [Google Scholar]
- 176.Zhou J, Leuschner C, Kumar C, Hormes JF, Soboyejo WO. Sub-cellular accumulation of magnetic nanoparticles in breast tumors and metastases. Biomaterials. 2006;27:2001–8. doi: 10.1016/j.biomaterials.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 177.Mahmoudi M, Shokrgozar MA, Simchi A, Imani M, Milani AS, Stroeve P, Vali H, Hafeli UO, Bonakdar S. Multiphysics flow modeling and in vitro toxicity of iron oxide nanoparticles coated with poly(vinyl alcohol) Journal of Physical Chemistry C. 2009;113:2322–31. [Google Scholar]
- 178.Gao J, Liang G, Cheung JS, Pan Y, Kuang Y, Zhao F, Zhang B, Zhang X, Wu EX, Xu B. Multifunctional Yolk-Shell Nanoparticles: A Potential MRI Contrast and Anticancer Agent. Journal of the American Chemical Society. 2008;130:11828–33. doi: 10.1021/ja803920b. [DOI] [PubMed] [Google Scholar]
- 179.Jin Y, Jia C, Huang SW, O'Donnell M, Gao X. Multifunctional nanoparticles as coupled contrast agents. Nat Commun. 2010;1:41. doi: 10.1038/ncomms1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Amiri H, Mahmoudi M, Lascialfari A. Superparamagnetic colloidal nanocrystal clusters coated with polyethylene glycol fumarate: A possible novel theranostic agent. Nanoscale. 2011;3:1022–30. doi: 10.1039/c0nr00603c. [DOI] [PubMed] [Google Scholar]
- 181.Lubbe AS, Bergemann C, Huhnt W, Fricke T, Riess H, Brock JW, Huhn D. Preclinical experiences with magnetic drug targeting: Tolerance and efficacy. Cancer Research. 1996;56:4694–701. [PubMed] [Google Scholar]
- 182.Lubbe AS, Bergemann C, Riess H, Schriever F, Reichardt P, Possinger K, Matthias M, Dörken B, Herrmann F, Gürtler R, Hohenberger P, Haas N, Sohr R, Sander B, Lemke AJ, Ohlendorf D, Huhnt W, Huhn D. Clinical experiences with magnetic drug targeting: A phase I study with 4'-epidoxorubicin in 14 patients with advanced solid tumors. Cancer Research. 1996;56:4686–93. [PubMed] [Google Scholar]
- 183.Koo H, Huh MS, Sun IC, Yuk SH, Choi K, Kim K, Kwon IC. In Vivo Targeted Delivery of Nanoparticles for Theranosis. Accounts of Chemical Research. 2011;44:1018–28. doi: 10.1021/ar2000138. [DOI] [PubMed] [Google Scholar]
- 184.Lee JE, Lee N, Kim T, Kim J, Hyeon T. Multifunctional Mesoporous Silica Nanocomposite Nanoparticles for Theranostic Applications. Accounts of Chemical Research. 2011;44:893–902. doi: 10.1021/ar2000259. [DOI] [PubMed] [Google Scholar]
- 185.Foy SP, Manthe RL, Foy ST, Dimitrijevic S, Krishnamurthy N, Labhasetwar V. Optical Imaging and Magnetic Field Targeting of Magnetic Nanoparticles in Tumors. ACS Nano. 2010;4:5217–24. doi: 10.1021/nn101427t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.He X, Na MH, Kim JS, Lee GY, Park JY, Hoffman AS, Nam JO, Han SE, Sim GY, Oh YK, Kim IS, Lee BH. A Novel Peptide Probe for Imaging and Targeted Delivery of Liposomal Doxorubicin to Lung Tumor. Molecular Pharmaceutics. 2011;8:430–8. doi: 10.1021/mp100266g. [DOI] [PubMed] [Google Scholar]
- 187.Hultman KL, Raffo AJ, Grzenda AL, Harris PE, Brown TR, O'Brien S. Magnetic Resonance Imaging of Major Histocompatibility Class II Expression in the Renal Medulla Using Immunotargeted Superparamagnetic Iron Oxide Nanoparticles. ACS Nano. 2008;2:477–84. doi: 10.1021/nn700400h. [DOI] [PubMed] [Google Scholar]
- 188.Li C, Penet MF, Wildes F, Takagi T, Chen Z, Winnard PT, Artemov D, Bhujwalla ZM. Nanoplex Delivery of siRNA and Prodrug Enzyme for Multimodality Image-Guided Molecular Pathway Targeted Cancer Therapy. ACS Nano. 2010;4:6707–16. doi: 10.1021/nn102187v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Thoeny HC, Triantafyllou M, Birkhaeuser FD, Froehlich JM, Tshering DW, Binser T, Fleischmann A, Vermathen P, Studer UE. Combined Ultrasmall Superparamagnetic Particles of Iron Oxide-Enhanced and Diffusion-Weighted Magnetic Resonance Imaging Reliably Detect Pelvic Lymph Node Metastases in Normal-Sized Nodes of Bladder and Prostate Cancer Patients. European Urology. 2009;55:761–9. doi: 10.1016/j.eururo.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 190.Qiang Y, Antony J, Sharma A, Nutting J, Sikes D, Meyer D. Iron/iron oxide core-shell nanoclusters for biomedical applications. Journal of Nanoparticle Research. 2006;8:489–96. [Google Scholar]
- 191.Widder KJ, Morris RM, Howard DP, Senyei AE. Tumor remission in Yoshida sarcoma-bearing rats by selective targeting of magnetic albumin microspheres containing doxorubicin. Proceedings of the National Academy of Sciences of the United States of America. 1981;78:579–81. doi: 10.1073/pnas.78.1.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Widder KJ, Morris RM, Poore GA, Howard DP, Senyei AE. Selective targeting of magnetic albumin microspheres containing lowdose doxorubicin: total remission in Yoshida sarcoma-bearing rats. European Journal of Cancer and Clinical Oncology. 1983;19:135–9. doi: 10.1016/0277-5379(83)90408-x. [DOI] [PubMed] [Google Scholar]
- 193.Senyei AE, Reich SD, Gonczy C, Widder KJ. In vivo kinetics of magnetically targeted low-dose doxorubicin. Journal of Pharmaceutical Sciences. 1981;70:39–41. doi: 10.1002/jps.2600700412. [DOI] [PubMed] [Google Scholar]
- 194.Goodwin S, Peterson C, Hoh C, Bittner C. Targeting and retention of magnetic targeted carriers (MTCs) enhancing intra-arterial chemotherapy. Journal of Magnetism and Magnetic Meterials. 1999;194:132–9. [Google Scholar]
- 195.Goodwin SC, Bittner CA, Peterson CL, Wong G. Single-dose toxicity study of hepatic intraarterial infusion of doxorubicin coupled to a novel magnetically targeted drug carrier. Toxicological Sciences. 2001;60:177–83. doi: 10.1093/toxsci/60.1.177. [DOI] [PubMed] [Google Scholar]
- 196.Alexiou C, Arnold W, Klein RJ, Parak FG, Hulin P, Bergemann C, Erhardt W, Wagenpfeil S, Andreas S Lübbe. Locoregional cancer treatment with magnetic drug targeting. Cancer Research. 2000;60:6641–8. [PubMed] [Google Scholar]
- 197.Lubbe AS, Bergemann C, Brock J, McClure DG. Physiological aspects in magnetic drug-targeting. Journal of Magnetism and Magnetic Meterials. 1999;194:149–55. [Google Scholar]
- 198.Pulfer SK, Gallo JM. Enhanced brain tumor selectivity of cationic magnetic polysaccharide microspheres. Journal of Drug Targeting. 1998;6:215–27. doi: 10.3109/10611869808997896. [DOI] [PubMed] [Google Scholar]
- 199.Pulfer SK, Ciccotto SL, Gallo JM. Distribution of small magnetic particles in brain tumor-bearing rats. Journal of Neuro-Oncology. 1999;41:99–105. doi: 10.1023/a:1006137523591. [DOI] [PubMed] [Google Scholar]
- 200.Kubo T, Sugita T, Shimose S, Nitta Y, Ikuta Y, Murakami T. Targeted delivery of anticancer drugs with intravenously administered magnetic liposomes in osteosarcoma-bearing hamsters. International Journal of Oncology. 2000;17:309–15. doi: 10.3892/ijo.17.2.309. [DOI] [PubMed] [Google Scholar]
- 201.Kubo T, Sugita T, Shimose S, Nitta Y, Ikuta Y, Murakami T. Targeted systemic chemotherapy using magnetic liposomes with incorporated adriamycin for osteosarcoma in hamsters. International Journal of Oncology. 2001;18:121–5. doi: 10.3892/ijo.18.1.121. [DOI] [PubMed] [Google Scholar]
- 202.Pankhurst QA, Connolly J, Jones SK, Dobson J. Applications of magnetic nanoparticles in biomedicine. Journal of Physics D: Applied Physics. 2003;36:R167–R81. [Google Scholar]
- 203.Laurent S, Dutz S, Häfeli UO, Mahmoudi M. Magnetic fluid hyperthermia: Focus on superparamagnetic iron oxide nanoparticles. Advances in Colloid and Interface Science. 2011;166:8–23. doi: 10.1016/j.cis.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 204.Gubin SP, Koksharov YA, Khomutov GB, Yurkov GY. Magnetic nanoparticles: preparation, structure and properties. Russian Chem Reviews. 2005;74:489–520. [Google Scholar]
- 205.Chan DCF, Kirpotin DB, Bunn PA. Synthesis and evaluation of colloidal magnetic iron-oxides for the sitespecific radiofrequency-induced hyperthermia of cancer. Journal of Magnetism and Magnetic Materials. 1993;122:374–8. [Google Scholar]
- 206.Jordan A, Wust P, Fahling H, John W, Hinz A, Felix R. Inductive heating of ferrimagnetic particles and magnetic fluids: Physical evaluation of their potential for hyperthermia. International Journal of Hyperthermia. 1993;9:51–68. doi: 10.3109/02656739309061478. [DOI] [PubMed] [Google Scholar]
- 207.Jordan A, Scholz R, Wust P, Schirra H, Thomas Schiestel, Schmidt H, Felix R. Endocytosis of dextran and silan-coated magnetite nanoparticles and the effect of intracellular hyperthermia on human mammary carcinoma cells in vitro. Journal of Magnetism and Magnetic Materials. 1999;194:185–96. [Google Scholar]
- 208.Moroz P, Jones SK, Gray BN. Magnetically mediated hyperthermia: current status and future directions. Int J Hyperthermia. 2002;18:267–84. doi: 10.1080/02656730110108785. [DOI] [PubMed] [Google Scholar]
- 209.Maier-Hauff K, Ulrich F, Nestler D, Niehoff H, Wust P, Thiesen B, Orawa H, Budach V, Jordan A. Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. Journal of Neuro-Oncology. 2011;103:317–24. doi: 10.1007/s11060-010-0389-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Hergt R, Andra W, D'Ambly CG, Hilger I, Kaiser WA, Richter U, Schmidt HG. Physical limits of hyperthermia using magnetite fine particles. IEEE Transactions on Magnetics. 1998;34:3745–3754. [Google Scholar]
- 211.Dudeck O, Bogusiewicz K, Pinkernelle J, Gaffke G, Pech M, Wieners G, Bruhn H, Jordan A, Ricke J. Local arterial infusion of superparamagnetic iron oxide particles in hepatocellular carcinoma: A feasibility and 3.0 T MRI study. Investigative Radiology. 2006;41:527–35. doi: 10.1097/01.rli.0000209601.15533.5a. [DOI] [PubMed] [Google Scholar]
- 212.Johannsen M, Gneveckow U, Eckelt L, Feussner A, Waldfner N, Scholz R, Deger S, Wust P, Loening SA, Jordan A. Clinical hyperthermia of prostate cancer using magnetic nanoparticles: Presentation of a new interstitial technique. International Journal of Hyperthermia. 2005;21:637–47. doi: 10.1080/02656730500158360. [DOI] [PubMed] [Google Scholar]
- 213.Johannsen M, Gneveckow U, Taymoorian K, Cho CH, Thiesen B, Scholz R, Waldöfner N, Loening SA, Wust P, Jordan A. Thermal therapy of prostate cancer using magnetic nanoparticles. Actas Urol Esp. 2007;31:660–7. doi: 10.1016/s0210-4806(07)73703-8. [DOI] [PubMed] [Google Scholar]
- 214.Johannsen M, Gneveckow U, Taymoorian K, Thiesen B, Waldofner N, Scholz R, Jung K, Jordan A, Wust P, Loening SA. Morbidity and quality of life during thermotherapy using magnetic nanoparticles in locally recurrent prostate cancer: Results of a prospective phase I trial. International Journal of Hyperthermia. 2007;23:315–23. doi: 10.1080/02656730601175479. [DOI] [PubMed] [Google Scholar]
- 215.Johannsen M, Gneveckow U, Thiesen B, Taymoorian K, Cho CH, Waldöfner N, Scholz R, Jordan A, Loening SA, Wust P. Thermotherapy of Prostate Cancer Using Magnetic Nanoparticles: Feasibility, Imaging, and Three-Dimensional Temperature Distribution. European Urology. 2007;52:1653–62. doi: 10.1016/j.eururo.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 216.Johannsen M, Thiesen B, Gneveckow U, Taymoorian K, Waldufner N, Scholz R, Deger S, Jung K, Loening SA, Jordan A. Thermotherapy using magnetic nanoparticles combined with external radiation in an orthotopic rat model of prostate cancer. Prostate. 2006;66:97–104. doi: 10.1002/pros.20324. [DOI] [PubMed] [Google Scholar]
- 217.Johannsen M, Thiesen B, Jordan A, Taymoorian K, Gneveckow U, Waldöfner N, Scholz R, Koch M, Lein M, Jung K, Loening SA. Magnetic fluid hyperthermia (MFH) reduces prostate cancer growth in the orthotopic Dunning R3327 rat model. Prostate. 2005;64:283–92. doi: 10.1002/pros.20213. [DOI] [PubMed] [Google Scholar]
- 218.Jordan A. MagForce® Nanotherapy: With tumor-specific nanoparticles against cancer. VDI. Berichte;2005:111–6. [Google Scholar]
- 219.Jordan A, Maier-Hauff K. Magnetic nanoparticles for intracranial thermotherapy. Journal of Nanoscience and Nanotechnology. 2007;7:4604–6. [PubMed] [Google Scholar]
- 220.Jordan A, Maier-Hauff K, Wust P, Rau B, Johannsen M. Thermotherapy using magnetic nanoparticles. Thermotherapie mit magnetischen nanopartikeln. 2007;13:894–902. [Google Scholar]
- 221.Jordan A, Scholz R, Maier-Hauff K, van Landeghem FKH, Waldoefner N, Teichgraeber U, Pinkernelle J, Bruhn H, Neumann F, Thiesen B, von Deimling A, Felix R. The effect of thermotherapy using magnetic nanoparticles on rat malignant glioma. Journal of Neuro-Oncology. 2006;78:7–14. doi: 10.1007/s11060-005-9059-z. [DOI] [PubMed] [Google Scholar]
- 222.Maier-Hauff K, Rothe R, Scholz R, Gneveckow U, Wust P, Thiesen B, Feussner A, von Deimling A, Waldoefner N, Felix R, Jordan A. Intracranial thermotherapy using magnetic nanoparticles combined with external beam radiotherapy: Results of a feasibility study on patients with glioblastoma multiforme. Journal of Neuro-Oncology. 2007;81:53–60. doi: 10.1007/s11060-006-9195-0. [DOI] [PubMed] [Google Scholar]
- 223.Morgul MH, Raschzok N, Schwartlander R, Vondran FW, Michel R, Stelter L, Pinkernelle J, Jordan A, Teichgraber U, Sauer IM. Tracking of primary human hepatocytes with clinical MRI: Initial results with Tat-peptide modified super-paramagnetic iron oxide particles. International Journal of Artificial Organs. 2008;31:252–7. doi: 10.1177/039139880803100309. [DOI] [PubMed] [Google Scholar]
- 224.Thiesen B, Jordan A. Clinical applications of magnetic nanoparticles for hyperthermia. International Journal of Hyperthermia. 2008;24:467–74. doi: 10.1080/02656730802104757. [DOI] [PubMed] [Google Scholar]
- 225.Wust P, Gneveckow U, Johannsen M, Buhmer D, Henkel T, Kahmann F, Sehouli J, Felix R, Ricke J, Jordan A. Magnetic nanoparticles for interstitial thermotherapy - Feasibility, tolerance and achieved temperatures. International Journal of Hyperthermia. 2006;22:673–85. doi: 10.1080/02656730601106037. [DOI] [PubMed] [Google Scholar]
- 226.Maier-Hauff K, Ulrich F, Nestler D, Niehoff H, Wust P, Thiesen B, Orawa H, Budach V, Jordan A. Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. Journal of Neuro-Oncology. 2011;103:317–24. doi: 10.1007/s11060-010-0389-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Maier-Hauff K, Ulrich F, Nestler D, Niehoff H, Wust P, Thiesen B, Orawa H, Budach V, Jordan A. Efficacy and safety of intratumoral thermotherapy using magnetic iron-oxide nanoparticles combined with external beam radiotherapy on patients with recurrent glioblastoma multiforme. Journal of Neuro-Oncology. 2011;103:317–24. doi: 10.1007/s11060-010-0389-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Johannsen M, Thiesen B, Wust P, Jordan A. Magnetic nanoparticle hyperthermia for prostate cancer. International Journal of Hyperthermia. 2010;26:790–5. doi: 10.3109/02656731003745740. [DOI] [PubMed] [Google Scholar]
- 229.Hergt R, Dutz S. Magnetic particle hyperthermia-biophysical limitations of a visionary tumour therapy. Journal of Magnetism and Magnetic Materials. 2007;311:187–92. [Google Scholar]
- 230.Hayashi K, Ono K, Suzuki H, Sawada M, Moriya M, Sakamoto W, Yogo T. High-frequency, magnetic-field-responsive drug release from magnetic nanoparticle/organic hybrid based on hyperthermic effect. ACS Appl Mater Interfaces. 2010;2:1903–11. doi: 10.1021/am100237p. [DOI] [PubMed] [Google Scholar]
- 231.Si HY, Li DP, Wang TM, Zhang HL, Ren FY, Xu ZG, Zhao YY. Improving the anti-tumor effect of genistein with a biocompatible superparamagnetic drug delivery system. J Nanosci Nanotechnol. 2010;10:2325–31. doi: 10.1166/jnn.2010.1913. [DOI] [PubMed] [Google Scholar]
- 232.Cedervall T, Lynch I, Lindman S, Berggård T, Thulin E, Nilsson H, Dawson KA, Linse S. Understanding the nanoparticle-protein corona using methods to quantify exchange rates and affinities of proteins for nanoparticles. Proceedings of the National Academy of Sciences. 2007;104:2050–5. doi: 10.1073/pnas.0608582104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Lundqvist M, Stigler J, Elia G, Lynch I, Cedervall T, Dawson KA. Nanoparticle size and surface properties determine the protein corona with possible implications for biological impacts. Proceedings of the National Academy of Sciences. 2008;105:14265–70. doi: 10.1073/pnas.0805135105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Cedervall T, Lynch I, Foy M, Berggård T, Donnelly SC, Cagney G, Linse S, Dawson KA. Detailed Identification of Plasma Proteins Adsorbed on Copolymer Nanoparticles. Angewandte Chemie. 2007;119:5856–8. doi: 10.1002/anie.200700465. [DOI] [PubMed] [Google Scholar]
- 235.Mahmoudi M, Shokrgozar MA, Sardari S, Moghadam MK, Vali H, Laurent S, Stroeve P. Irreversible changes in protein conformation due to interaction with superparamagnetic iron oxide nanoparticles. Nanoscale. 2011;3:1127–38. doi: 10.1039/c0nr00733a. [DOI] [PubMed] [Google Scholar]
- 236.Mahmoudi M, Azadmanesh K, Shokrgozar MA, Journeay WS, Laurent S. Effect of nanoparticles on the cell life cycle. Chemical Reviews. 2011;111:3407–32. doi: 10.1021/cr1003166. [DOI] [PubMed] [Google Scholar]
- 237.Mahmoudi M, Lynch I, Ejtehadi MR, Monopoli MP, Bombelli FB, Laurent S. Proteinnanoparticle interactions: Opportunities and challenges. Chemical Reviews. 2011;111:5610–37. doi: 10.1021/cr100440g. [DOI] [PubMed] [Google Scholar]