Abstract
Introduction
Cross-informant disagreement is common and results in different interpretations of a youth's behavior. Theoretical explanations for discrepancies typically rely on scale level analyses. This article explores whether caregivers and adolescents differ in when they notice and report symptoms of youth mania depending on the severity of overall manic disturbance.
Method
Participants were 459 adolescent-caregiver pairs recruited at either a community mental health center or an academic medical center. Adolescents were most likely to have a primary diagnosis of unipolar depression (37%) or attention-deficit/hyperactivity disorder/disruptive behavior disorder (36%). Nineteen percent of adolescents received a bipolar spectrum disorder diagnosis (4% bipolar I and 15% bipolar II, cyclothymia, or bipolar not otherwise specificed). Caregivers were primarily biological mothers (74%) or grandparents (8%). Adolescents and caregivers independently completed the Mood Disorder Questionnaire (MDQ) about the adolescent.
Results
Item response theory analyses of the entire sample indicated that in general, both caregivers and adolescents reserved endorsement of mania symptoms for the most severely ill half of participants. Comparisons of caregiver and adolescent report of symptoms on the MDQ indicated two significant differences. Caregivers were more likely to report irritability at significantly lower severity of mania than adolescents. Adolescents endorsed only increased energy or hyperactivity at lower severities than caregivers.
Conclusions
Adolescents and caregivers will have different concerns and might report different symptoms consistent with whom the symptom impacts first. Caregivers are more likely to report behaviors such as irritability, whereas adolescents are more likely to report subjective feelings such as feeling more energetic or more hyperactive.
Inter-rater reliability is a long-standing issue in the measurement of psychopathology. Best practices guidelines request clinicians collect information from multiple informants to gain a fuller understanding of adaptive and maladaptive behaviors (Carlson et al. 2003; Hunsley Mash 2008; Offord et al. 1996). Multiple informants often give substantially discrepant reports about the same individual. In fact, the average correlation among different reporters is between 0.2 and 0.3 (Achenbach et al. 2005; Achenbach et al. 1987). Outcomes in research are often dependent upon the informant (Findling et al. 2007; Findling et al. 2005; Khanna Kendall 2010; MTA 1999). The discrepancy amongst informants could account for differences in impressions of needs, wellness, relationship, and possibly diagnosis (Cantwell et al. 1997; Mattison et al. 2007; Perrin et al. 2000; Youngstrom et al. 2003).
There are various theoretical explanations for the discrepancy among informants. In both adult and pediatric bipolar disorder, discrepant reporting between the individual with the disorder and others has traditionally been viewed as a marker of compromised insight (Dell'Osso et al. 2002; Youngstrom et al. 2003). In fact, this perspective is so ingrained that an item on the Young Mania Rating Scale (Young et al. 1978), a measure commonly used in clinical trials to monitor the severity of manic symptoms, measures a patient's ability to perceive his/her current symptoms. In the assessment of pediatric bipolar disorder, parent report has consistently demonstrated higher validity in terms of predicting diagnosis or sensitivity to treatment effects (Youngstrom et al. 2009). This approach suggests a view that informant discrepancies reflect bias or error (De Los Reyes Kazdin 2008).
“Bias” or “error” represents the traditional view of informant discrepancy; however, recent theories implicate other mechanisms for the discrepancy between informants. For example, discrepancies between teacher and caregiver report can also be interpreted as discrepancies in situational or environmentally driven behavior (De Los Reyes 2011; Shoda 1995). This view suggests that behavior is moderated by the specific environment. Functional behavior analysis is a treatment approach that capitalizes on the situational-specificity model by investigating what is different in each setting that elicits and reinforces different behaviors (Schill et al. 1996). In fact, two caregivers in the same setting show significantly more accordance in ratings of youth behavior than adults in different settings, suggesting that symptoms do change as a function of the setting (Achenbach McConaughy Howell 1987; Achenbach Rescorla 2001; Reynolds Kamphaus 1992).
Approaching informant agreement and disagreement from either the “bias” or “situation specific”perspectives assumes that behavior is best measured at a scale level rather than using categories or individual items. In fact, scale scores are almost always more reliable than single item scores. However, these approaches assume that item content is equally important across informants. Caregivers and adolescents often focus on different symptoms of a disorder (e.g., Cantwell et al. 1997). One way to consider this difference in informant report could be to separate symptoms into “Self-First” and “Other-First” symptoms. “Self-First” symptoms are symptoms that bother the individual first. “Other-First” symptoms are symptoms that are noticed by others first. For example, irritability is often considered a classic “Other- First” symptom. Caregivers notice the youth's irritability, are most bothered by irritability relative to other symptoms, and seek treatment for that irritability (Jensen et al. 2007). In contrast, cognitive symptoms such as racing thoughts might not be as noticeable to caregivers at low levels as they would be to the youth. Hypomanic or manic symptoms are required for the diagnosis of bipolar disorder (APA 2001), and bipolar disorder definitely has features that could be characterized as an externalizing disorder (Youngstrom et al. 2008). Manic symptoms are generally considered to be “Other-First” symptoms (Youngstrom Birmaher Findling 2008), likely to be noticeable by others before they cause distress in the person experiencing them. Therefore, discrepancy in scale level reporting might be due to differences in thresholds at which each party recognizes and endorses symptoms.
The concepts of “Self-First’ and “Other-First” symptoms have existed for decades. However, statistical methods that could quantify the difference between “Self-First” and “Other- First” symptoms are only recently being used in clinical data with affective disorders (e.g., Weinstock et al. 2009, Weinstock, et al. 2010). Item response theory is a statistical approach that allows for the quantification of the thresholds, or level of severity, at which individuals typically endorse a symptom. As “Self-First” symptoms create distress for the individual experiencing the symptom first, the threshold at which a symptom is endorsed should be lower for self-report than informant report. As “Other-First” symptoms create distress for others prior to the individual experiencing the symptoms, the threshold at which a symptom is endorsed should be higher for self-report than informant report.
The primary aim of this article is to explore differences in manic symptom endorsement across caregiver and self-report in adolescents presenting at a community mental health clinic.
Method
Study design
Data for this study were derived from a study to examine evidence based methods for the assessment of pediatric bipolar disorder in diverse settings (NIH R01 MH066647). The study was approved by the Institutional Review Board (IRB) at both Case Western Reserve University and the University of North Carolina at Chapel Hill. All participants and their primary caregivers gave written informed assent and consent in accordance with local IRB regulations.
Participants
Participants were recruited using a consecutive case series design from all clinical intakes at a large community mental health center (n=320) or from an academic medical center (n=139) that were enrolling participants in treatment trials for bipolar spectrum disorders, depression, post-traumatic stress disorder, disruptive behavior disorders, and schizophrenia (Findling et al. 2001). Caregivers and community providers referred families for treatment. The research assessments were part of screening assessments conducted for participation in treatment trials.
Study inclusion and exclusion criteria were identical at the two sites. Participation required the youth to be between 11–18 years of age. Inclusion criteria at both sites were: 1) Both caregiver and youth provided written consent and assent, 2) both caregiver and youth presented for assessment, and 3) both caregiver and youth were conversant in English. Participants underwent the same assessment procedure regardless of presenting symptoms.
Caregivers were typically biological mothers (74%). Table 1 displays the demographic information about youth and caregivers. Biological fathers (5%), maternal grandmothers (5%), and adoptive mothers (5%) accounted for the next largest set of caregivers. Adolescent participants were 13.5 years of age (SD: 1.9), typically male (54%), and were primarily African American (68%) or Caucasian (25%). Adolescent participants met diagnostic criteria for between 0 and 8 DSM-IV diagnoses (median=3). Approximately 19% of the sample met criteria for a bipolar spectrum diagnosis (bipolar I, bipolar II, cyclothymia, or bipolar not otherwise specified (NOS)—most commonly due to insufficient duration of index mood episode. Approximately 65% of the sample met criteria for a disruptive behavior disorder (oppositional defiant disorder, conduct disorder, or disruptive behavior disorder NOS). Approximately 51% of the sample met criteria for an attention-deficit/hyperactivity disorder.
Table 1.
Demographic Characteristics
| Adolescents | N=459 |
|---|---|
| Gender | |
| Male | 248 (54%) |
| Female | 211 (46%) |
| Ethnicity | |
| Caucasian | 115 (25%) |
| African American | 312 (68%) |
| Other | 32 (7%) |
| Age in years | 13.5 (1.9) |
| Number of diagnoses | 2.7 (1.0) |
| Primary diagnosis | |
| Bipolar I | 18 (4%) |
| Other bipolar spectrum | 69 (15%) |
| Unipolar depression | 170 (37%) |
| Disruptive behavior disorder without mood | 165 (36%) |
| All other diagnoses | 37 (8%) |
| Caregivers | |
|---|---|
| Gender | |
| Male | 32 (7%) |
| Female | 427 (93%) |
| Relationship to Adolescent | |
| Biological mother | 340 (74%) |
| Biological father | 23 (5%) |
| Grandmother | 32 (7%) |
| Grandfather | 5 (1%) |
| Adoptive parent | 32 (7%) |
| Other | 27 (6%) |
Assessments
Diagnostic assessments were made using the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS) – Present and Lifetime – PLUS. This version of the KSADS amalgamates the mood modules from the Washington University KSADS (Geller et al. 2001) and the KSADS Present & Lifetime version (Kaufman et al. 1997). Research assistants were highly trained: Symptom level ratings were compared with a reliable rater for new raters for at least 5 interviews rating along and then 5 interviews leading. A new rater passed as session if he/she achieved an overall κ=.85 at the item level of the entire interview and a κ=1.0 at the diagnostic level. Research assistants were primarily predoctoral psychology interns or research staff with a M.A. or Ph.D. in Psychology or M.S.W. A team led by a licensed clinical psychologist assigned final consensus diagnoses using the longitudinal evaluation of all available data (LEAD) procedure (Spitzer 1983). Consensus teams were blind to the caregiver and youth-report rating scales.
Mood Disorder Questionnaire (MDQ)
Caregivers and adolescents completed the MDQ (Hirschfeld et al. 2003; Wagner et al. 2006). The MDQ consists of 13 items querying about manic symptoms. Respondents endorse or deny the presence of manic symptoms. The caregiver version was a slightly modified version of the original MDQ, where they reported about potential manic symptoms in their offspring (Wagner et al. 2006; Youngstrom, et al. 2005).
Data analysis
All participants data were analyzed. Item response theory (IRT) is a collection of models that evaluate both an item and the test's functioning on an underlying trait (e.g., underlying mania severity). The discrimination parameter represents the relationship between the item response and the latent trait, similar to a nonlinear factor loading, by quantifying the ability to measure level on the latent trait accurately. In psychopathology, the slope of the discrimination parameter reflects the rates of endorsement of an item at different severities. In psychopathology, the threshold parameter represents the severity of symptoms required before an item is endorsed at least 50% of the time. Threshold parameters are scaled relative to each other within the sample on a scale interpretable similar to z-scores. One parameter models concentrate on examining the thresholds; two parameter models study both the thresholds and the discrimination parameters simultaneously.
For example, IRT has been used to scale the latent trait of intelligence on general cognitive ability tests (e.g., Woodcock et al. 2007). Imagine a 14 year old taking an intelligence test. An item such as “What is a bird?” displays strong discrimination—a 14 year old getting the item incorrect will most likely miss most items of higher thresholds—and a low threshold parameter—the item requires relatively lower amounts of intelligence to answer correctly. In contrast, an item such as “What is a mitochondrion?” might have a weaker discrimination parameter due to knowledge acquired in biology courses causing more individuals to answer the item correctly regardless of their intelligence; however, the item will also display a substantially higher threshold parameter relative to the first item because a higher level of intelligence is required to answer the item correctly.
Item Response Theory allows for detection of Differential Item Functioning (DIF) via likelihood ratio tests (Thissen et al. 1993). DIF occurs when two groups of people with the same level of the trait in question do not have the same probability of choosing identical responses on a particular item (Lord 1980). In the present study, DIF would mean that at a given level of mania, the youth and the caregiver did not have the same probability of endorsing a particular manic symptom. Differences in the threshold parameter can be interpreted similarly to Cohen's D for t-tests (i.e., >0.2 is "small," >0.5 is "medium," >0.8 is "large"; Steinberg Thissen 2006). Significance tests of equality constraints between caregiver and youth values examined potential DIF, using a post hoc procedure to control Type I error. Items showing DIF were graphed and visually inspected to evaluate the extent of DIF (Steinberg Thissen 2006).
Results
Evaluation of item response theory assumptions
A two parameter IRT model that allowed the discrimination and threshold parameters to vary fit the data for both groups better than a one parameter IRT model that allowed only the threshold parameters to vary, p<.05. Therefore, a model estimating both the discrimination and threshold parameters was used. IRT assumes unidimensionality, meaning that only one latent dimension may be present and items should not show correlated error with each other. For the MDQ, this would mean that a single mania factor explained all of the correlations between responses on the items. The MDQ items did not satisfy the strict unidimensionality assumption in the present sample. The items assessing increased energy (MDQ 8) and hyperactivity (MDQ 9) were more correlated with each other than expected based on a mania factor (technically referred to as “local dependence”). To better model them, they were combined into a single item representing no to both, yes to one, yes to both after ordering was suggested appropriate by a nominal model. The unidimensional model fit the data with the combined item, RMSEA=.03 (where values <.05 are usually considered good fit).
Item Analyses
Table 2 displays the discrimination and threshold parameter estimates for caregiver and self-reported mania symptoms on the MDQ. Caregiver reported symptoms of mania displayed good discrimination (i.e., discrimination parameters greater than 1.0). The exceptions to this were the items measuring hypersexuality (MDQ 11) and monetary risk (MDQ 13), which have substantially lower discrimination parameters than the other items. Lower discrimination means that caregivers were unlikely to endorse these items across the severity spectrum and that endorsement is potentially less due to mania and more influenced by extraneous factors. The poor discrimination of these items is most likely a reflection of content that is less applicable to this developmental age range: Both hypersexuality and impulsive spending are behaviors more frequent among adults (Hirschfeld et al. 2000).
Table 2.
Item Response Parameter Estimates Displaying Differences in Thresholds between Caregiver and Adolescent Reports of Manic Symptoms in Order of Typical Endorsement by “Other-First” to “Self-First”
| Item | Content (Adolescent Report Version) | Summary | Reporter (% endorsed) | Discrimination | Threshold |
|---|---|---|---|---|---|
| 13 | Spending money got you or your family in trouble? | Monetary risk | Caregiver (10%) | .97 (.21) | 2.35 (.41) |
| Adolescent (11%) | .70 (.27) | 3.64 (1.22) | |||
| 2 | You were so irritable that you shouted at people or started fights or arguments? | Irritability | Caregiver (58%) | 1.23 (.17) | −.69 (.12)** |
| Adolescent (58%) | 1.38 (.21) | .17 (.08)** | |||
| 7 | You were so easily distracted by things around you that you had trouble concentrating or staying on track? | Distractibility | Caregiver (68%) | 1.72 (.23) | −.67 (.10)* |
| Adolescent (68%) | 1.85 (.26) | −.34 (.08)* | |||
| 12 | You did things that were unusual for you or that other people might have thought were excessive, foolish, or risky? | Sensation seeking | Caregiver (36%) | 1.35 (.18) | .46 (.10)* |
| Adolescent (36%) | 1.54 (.24) | .73 (.10)* | |||
| 10 | You were much more social or outgoing than usual, for example, you telephoned friends in the middle of the night? | Sociability | Caregiver (33%) | 1.13 (.17) | .85 (.14) |
| Adolescent (33%) | 1.13 (.19) | .82 (.13) | |||
| 5 | You were much more talkative or spoke much faster than usual? | Rapid speech | Caregiver (43%) | 2.11 (.27) | .50 (.08) |
| Adolescent (43%) | 2.15 (.31) | .39 (.07) | |||
| 1 | You felt so good or so hyper that other people thought you were not your normal self, or you were so hyper that you got into trouble? | Increased energy+irritability | Caregiver (45%) | 1.95 (.25) | .35 (.08) |
| Adolescent (45%) | 2.42 (.35) | .20 (.06) | |||
| 6 | Thoughts raced through your head or you couldn't slow your mind down? | Racing thoughts | Caregiver (38%) | 1.69 (.23) | .61 (.09) |
| Adolescent (38%) | 1.64 (.24) | .44 (.08) | |||
| 3 | You felt much more self-confident than usual? | Grandiosity | Caregiver (46%) | 1.28 (.17) | .44 (.10)* |
| Adolescent (46%) | 1.04 (.18) | .13 (.10)* | |||
| 4 | You got much less sleep than usual and found you didn't really miss it? | Decreased need for sleep | Caregiver (38%) | 1.36 (.19) | .75 (.11)* |
| Adolescent (38%) | 1.09 (.18) | .42 (.11)* | |||
| 8 | You had much more energy than usual? | Increased energy | Caregiver (21%, 34%) | 2.44 (.30)** | .16 (.07)**, .61 (.08) |
| Adolescent (21%, 34%) | 1.59 (.21)** | −.28 (.09)**, .63 (.09) | |||
| 9 | You were much more active or did many more things than usual? | Hyperactivity | |||
| 11 | You were much more interested in sex than usual? | Hypersexuality | Caregiver (18%) | .80 (.17) | 2.32 (.44) |
| Adolescent (19%) | 1.01 (.22) | 1.69 (.30) |
Note: * p<.05, ** p<.05 after controlling for the false discovery rate. On average, adolescent self-report (mean=5.34; standard deviation=3.05) was not different than caregiver report (mean=5.08, standard deviation=3.38); t (457)=1.22; p=.22.
Caregivers typically endorsed symptoms of mania at similar, elevated thresholds. The elevated threshold parameters indicated that caregivers typically did not endorse all symptoms of mania for all youth. Caregivers reserved endorsement of manic symptoms for more severe presentations, as seen by threshold parameters consistently greater than +0.25. Two exceptions existed: caregivers endorsed the nonspecific symptoms of irritability (MDQ 2) and distractibility (MDQ 7) at substantially lower thresholds than other items. Symptoms endorsed at lower thresholds are endorsed more frequently in general and as a result are less specific to mania.
Similar to caregiver reports, youth-endorsed symptoms of mania displayed good discrimination parameters, indicating that the symptoms were strongly related to the underlying factor of mania. Similar to caregivers, monetary risk (MDQ 13) displayed poor discrimination across severity of mania. Youth typically endorsed items in a similar, elevated range. Adolescents were more likely to report one of either increased energy (MDQ 8) or hyperactivity (MDQ 9) at lower severity relative to other self-reported symptoms.
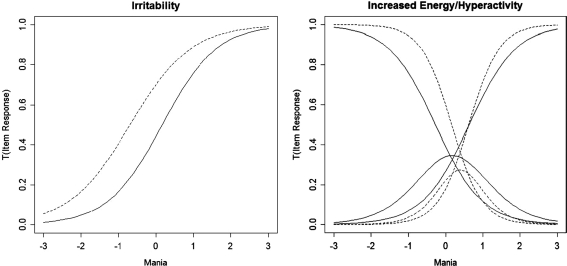
Differential item functioning analyses compared caregiver and adolescent self-report of mania symptoms. Six items displayed statistically significant differential item functioning; however, only two items retained significant differences after controlling for the false discovery rate (Benjamini Hochberg 1995). They are displayed in Figure 1. Adolescents trended toward reporting grandiosity and decreased need for sleep at lower thresholds than caregivers, whereas caregivers trended toward endorsing distractibility and sensation seeking at lower severity than adolescents. Caregivers endorsed irritability at significantly lower severity than adolescents, p<.01. The difference in thresholds suggests that irritability is an “Other-First” symptom, and to a lesser extent, distractibility and sensation seeking might be as well. Adolescents endorsed either increased energy or hyperactivity at significantly lower severity thresholds than caregivers; however, it should be noted that if both symptoms were present adolescents and caregivers endorsed the items similarly. The presence of only increased energy or only hyperactivity might be considered a “Self-First” symptom in that it reflects privileged awareness about one's own subjective feeling.
FIG. 1.
Differential item functioning of irritability and increased energy/hyperactivity. Note that item response theory analysis was conducted on the entire sample (N=459). Dashed line represents caregiver report; solid line represents adolescent self-report. If the curves are shifted to the left, then lower levels of the underlying mania factor are needed before endorsing an item.
Discussion
Recently, the clinical rate of diagnosis of pediatric bipolar disorder has increased substantially, leading to concerns of overdiagnosis (Blader Carlson 2007, Moreno, et al. 2007). Understanding the nature of informant discrepancies between youth and caregivers may help us to understand not only which symptoms are being reported but also by whom. This knowledge could help in understanding how to interpret discrepant reporting between youth and caregivers at a symptom level. As symptoms are the basis for diagnosis within the DSM framework, improvements knowledge about symptom reporting could help improve the accuracy of diagnoses. The aim of this study was to examine whether caregiver and adolescent reports of manic symptoms could be statistically differentiated into “Self-First” and “Other-First” symptoms. “Self-First” symptoms would be reported at lower levels of severity by the youth and “Other-First” symptoms would be endorsed earlier by caregivers. We compared 459 caregiver and adolescent pairs' reporting of manic symptoms on the MDQ. Symptom endorsement by both caregivers and adolescents occurred at consistently elevated thresholds, which means that not everyone attending the clinic endorsed symptoms of mania. Endorsing items more specific to mania at elevated thresholds suggest that both caregivers and adolescents reserve positive reporting for the most severe half of treatment seekers.
Symptoms were generally similar in their ability to discriminate positive responses from both caregivers and adolescents. The similarity and steepness of the discrimination parameters suggest that caregivers and adolescents appraise manic symptoms in broadly similar fashion. On average across symptoms, both informants were most likely to endorse a symptom when approximately the same severity of overall mania was present. The exceptions were items regarding hypersexuality and taking monetary risks, which caregivers were less likely to endorse regardless of the presence of mania. IRT analyses indicated that irritability and distractibility were “easier” items for caregivers to endorse—that is, the youth had to demonstrate a lower severity of mania in order for the caregiver to endorse these items. This suggests that irritability and distractibility are among the most noticeable and distressing symptoms of mania to caregivers. Additionally, irritability and distractibility are not specific to mania (Leibenluft et al. 2003; Youngstrom Birmaher Findling 2008) and could be endorsed for a variety of other reasons besides mania. For youth report, increased energy and hyperactivity were “easier” to endorse (i.e., a lower severity of mania needed to be present in order for the symptom to be endorsed).
Conclusions
The current analyses are some of the first to quantify this difference in symptom experience and examine how well a particular framing of symptoms reflects the underlying dimension of mania. Results suggested that at the same underlying level of mania, caregivers were significantly more likely than youths to report irritability. This suggests that irritability is an “Other-First” symptom—more concerning to the caregiver than to the youth. Conversely, at the same underlying level of mania, youth were significantly more likely than caregivers to report increased energy and hyperactivity. These may be experienced as “Self-First” symptoms of mania by adolescents—more likely that the adolescent notices first before they become bothersome to the caregiver. Additionally, the results indicate that both caregiver and youth interpret the items on the MDQ as reflecting a single, underlying trait. It is worth noting that for the MDQ, informant differences in item responses happened to occur in opposite directions, essentially canceling each other out at the total score level. However, if more items had been skewed towards the “Other First” direction, then caregiver MDQ total scores would be biased to be systematically higher than youth report for cases with the same level of mania. Conversely, a preponderance of “Self First” items would bias the youth total higher. Although the MDQ scores appear similar across informants, results underscore the potential value of checking item-level response patterns as a method of confirming validity across informants.
Clinical implications
In a clinical setting where youth are presenting with mania or bipolar disorder, clinicians should be aware that youths and caregivers will have different concerns and may report different symptoms. Clinicians will be more likely to hear about irritability from caregivers before it begins to bother the adolescent, while adolescents may report increased energy or hyperactivity before these become problematic for caregivers. Cantwell described a method to remember this difference by comparing symptoms to onions and garlic (Carlson, personal communication, September 3, 2003). “Self-First” symptoms could be considered onion symptoms—those that are noticed by the individual experiencing them first; while, “Other-First” symptoms could be considered garlic symptoms—those that interrupt others first.
Additionally, the symptoms with low thresholds—irritability, distractibility, increased energy, and hyperactivity—are likely to be least useful in differentiating mania or bipolar disorder from other conditions. These symptoms are endorsed at lower levels of mania, which means that they are more likely to be endorsed by caregivers and adolescents for whom mania is not a major concern. However, two potential alternate uses for these symptoms arise. First, nonspecific symptoms might be a useful predictor of severity, prognosis, and process concerns that could be used in conjunction with a specific diagnosis. Second, changes in reporting might indicate the beginning of therapeutic response. At the same time, because they are nonspecific, the symptoms could be associated with other nonbipolar factors, especially in a clinical sample with a mixture of diagnoses. Before diagnosing bipolar disorder in cases where these symptoms are the chief concern of the caregivers, clinicians should make a point of thoroughly assessing for other risk factors, such as episodic presentation, prior mood episodes, and family history.
Although irritability and distractibility are less useful for diagnosis, unfortunately no symptoms emerged as clearly most specific or decisive in making a diagnosis of mania. This finding contrasts with the emphasis sometimes placed on grandiosity or elated mood as a cardinal feature of pediatric bipolar disorder (Geller et al. 2007). It appears that when caregivers or youths complete scales about other symptoms of mania (e.g., elevated mood, racing thoughts), these symptoms tend to cluster together. That is, once caregivers/youths endorse one symptom, it is likely that they will endorse other symptoms as well. Our analyses suggest that no one symptom will be the key to making a diagnosis of mania or bipolar disorder, but that as clinicians begin to hear about manic symptoms they should query about other symptoms as they are likely to be present. A final implication is that parents and youths often will focus on different symptoms as being more problematic or impairing. This may influence how motivated each is for treatment, or which symptoms are perceived as important targets for intervention.
Limitations
There are limitations to this study based on design features. The current analyses are limited to the wording of items on the MDQ. Alternate wordings of a symptom might change severity thresholds as well as how well the item discriminates; however, the order of severity thresholds for the parent-reported symptoms is consistent with those of the Child Mania Rating Scale (Henry et al. 2008). Additionally, the findings consist of outpatients and their caregivers' interpretation of the items regardless of whether the youth met criteria for bipolar disorder. We did not check respondents' endorsements against their clinician-rated responses on the K-SADS, which might have provided some information as to their actual understanding of the items. Interpretation of items is always a limitation on rating scales. Nevertheless, the responses did seem to reflect emotions and behaviors that each respondent felt was most important to him or her. The discrimination and severity threshold parameter estimates reflect how caregivers and youths view themselves and not the results of a thorough clinical evaluation. Despite these limitations, the primary findings indicate that the respondent is important in determining which manic symptoms are likely to be endorsed such that regardless of diagnosis, caregivers are more likely to report irritability at lower severity than youth and youth are more likely to report increased energy or hyperactivity at lower severity.
Author Disclosures
Dr. E. Youngstrom has received travel support from Bristol-Myers Squibb. Dr. Findling receives or has received research support, acted as a consultant and/or served on a speaker's bureau for Abbott, Addrenex, AstraZeneca, Biovail, Bristol-Myers Squibb, Forest, GlaxoSmithKline, Johnson & Johnson, KemPharm Lilly, Lundbeck, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Rhodes Pharmaceuticals, Sanofi-Aventis, Schering- Plough, Seaside Therapeutics, Sepracore,Shire, Solvay, Sunovion, Supernus Pharmaceuticals, Validus, and Wyeth. Mr. Freeman, Ms. Freeman, and Dr. Youngstrom have no conflicts of interest to disclose.
References
- Achenbach TM. Krukowski R. Dumenci L. Ivanova M. Assessment of adult psychopathology: Meta-analyses and implications of cross-informant correlations. Psychol Bull. 2005;131:361–382. doi: 10.1037/0033-2909.131.3.361. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. McConaughy SH. Howell CT. Child/adolescent behavioral, emotional problems: Implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101:213–232. [PubMed] [Google Scholar]
- Achenbach TM. Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Benjamini Y. Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J Royal Statistical Soc Series B (Methodological) 1995;57:289–300. [Google Scholar]
- Blader JC. Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996–2004. Biol Psychiatry. 2007;62:107–114. doi: 10.1016/j.biopsych.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantwell DP. Lewinsohn PM. Rohde P. Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. J Am Acad Child Adolesc Psychiatry. 1997;36:610–619. doi: 10.1097/00004583-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Carlson GA. Jensen PS. Findling RL. Meyer RE. Calabrese J. DelBello MP. Emslie G. Flynn L. Goodwin F. Hellander M. Kowatch R. Kusumakar V. Laughren T. Leibenluft E. McCracken J. Nottelmann E. Pine D. Sachs G. Shaffer D. Simar R. Strober M. Weller EB. Wozniak J. Youngstrom EA. Methodological issues, controversies in clinical trials with child, adolescent patients with bipolar disorder: Report of a consensus conference. J Child Adolesc Psychopharm. 2003;13:13–27. doi: 10.1089/104454603321666162. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A. Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. J Clin Child Adolescent Psychol. 2011;40:1–9. doi: 10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A. Kazdin AE. When the evidence says, “Yes, No, Maybe So”: Attending to and interpreting inconsistent findings among evidence-based interventions. Current Directions in Psychological Science. 2008;17:47–51. doi: 10.1111/j.1467-8721.2008.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell'Osso L. Pini S. Cassano GB. Mastrocinque C. Seckinger RA. Saettoni M. Papasogli A. Yale SA. Amador XF. Insight into illness in patients with mania, mixed mania, bipolar depression and major depression with psychotic features. Bipolar Disorders. 2002;4:315–322. doi: 10.1034/j.1399-5618.2002.01192.x. [DOI] [PubMed] [Google Scholar]
- Findling RL. Frazier TW. Youngstrom EA. McNamara NK. Stansbrey RJ. Gracious BL. Reed MD. Demeter CA. Calabrese JR. Double-blind, placebo-controlled trial of divalproex monotherapy in the treatment of symptomatic youth at high risk for developing bipolar disorder. J Clin Psychiatry. 2007;68:781–788. doi: 10.4088/jcp.v68n0519. [DOI] [PubMed] [Google Scholar]
- Findling RL. Gracious BL. McNamara NK. Youngstrom EA. Demeter CA. Branicky LA. Calabrese JR. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disorders. 2001;3:202–210. [PubMed] [Google Scholar]
- Findling RL. McNamara NK. Youngstrom EA. Stansbrey R. Gracious BL. Reed MD. Calabrese JR. Double-blind 18-month trial of lithium versus divalproex maintenance treatment in pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:409–417. doi: 10.1097/01.chi.0000155981.83865.ea. [DOI] [PubMed] [Google Scholar]
- Geller B. Tillman R. Bolhofner K. Proposed Definitions of Bipolar I Disorder Episodes and Daily Rapid Cycling Phenomena in Preschoolers, School-Aged Children, Adolescents, and Adults. J Child Adolesc Psychopharmacol. 2007;17:217–222. doi: 10.1089/cap.2007.0017. [DOI] [PubMed] [Google Scholar]
- Geller B. Zimerman B. Williams M. Bolhofner K. Craney JL. DelBello MP. Soutullo C. Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. Journal Am Acad Child Adolesc Psychiatry. 2001;40:450–455. doi: 10.1097/00004583-200104000-00014. [DOI] [PubMed] [Google Scholar]
- Henry DB. Pavuluri MN. Youngstrom E. Birmaher B. Accuracy of brief and full forms of the Child Mania Rating Scale. J Clini Psychology. 2008;64:368–381. doi: 10.1002/jclp.20464. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM. Holzer C. Calabrese JR. Weissman M. Reed M. Davies M. Frye MA. Keck P. McElroy S. Lewis L. Tierce J. Wagner KD. Hazard E. Validity of the mood disorder questionnaire: A general population study. Am J Psychiatry. 2003;160:178–180. doi: 10.1176/appi.ajp.160.1.178. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM. Williams JB. Spitzer RL. Calabrese JR. Flynn L. Keck PE., Jr. Lewis L. McElroy SL. Post RM. Rapport DJ. Russell JM. Sachs GS. Zajecka J. Development, validation of a screening instrument for bipolar spectrum disorder: The Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- Hunsley J. Mash EJ. A Guide to Assessments That Work. New York, NY US: Oxford University Press; 2008. [Google Scholar]
- Jensen PS. Youngstrom EA. Steiner H. Findling RL. Meyer RE. Malone RP. Carlson GA. Coccaro EF. Aman MG. Blair J. Dougherty D. Ferris C. Flynn L. Green E. Hoagwood K. Hutchinson J. Laughren T. Leve LD. Novins DK. Vitiello B. Consensus report on impulsive aggression as a symptom across diagnostic categories in child psychiatry: Implications for medication studies. J Am Acad Child Adolesc Psychiatry. 2007;46:309–322. doi: 10.1097/chi.0b013e31802f1454. [DOI] [PubMed] [Google Scholar]
- Kaufman J. Birmaher B. Brent D. Rao U. Flynn C. Moreci P. Williamson D. Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adoles Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Khanna MS. Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. J Consult Clin Psychology. 2010;78:737–745. doi: 10.1037/a0019739. [DOI] [PubMed] [Google Scholar]
- Leibenluft E. Blair RJR. Charney DS. Pine DS. King JA. Ferris CF. Lederhendler II. Irritability in pediatric mania and other childhood psychopathology. In: King JA, editor; Ferris CF, editor; Lederhendler II, editor. Roots of Mental Illness in Children. New York, NY, US: New York Academy of Sciences; 2003. pp. 201–218. [DOI] [PubMed] [Google Scholar]
- Lord FM. Applications of Item Response Theory to Practical Testing Problems. Hillsdale, N.J.: L. Erlbaum Associates; 1980. [Google Scholar]
- Mattison RE. Carlson GA. Cantwell DP. Asarnow JR. Teacher and parent ratings of children with depressive disorders. J Emotional Behav Dis. 2007;15:184–192. [Google Scholar]
- Mischel W. Shoda Y. A cognitive-affective system theory of personality: Reconceptualizing situations, dispositions, dynamics, and invariance in personality structure. Psychol Rev. 1995;102:246–268. doi: 10.1037/0033-295x.102.2.246. [DOI] [PubMed] [Google Scholar]
- Moreno C. Laje G. Blanco C. Jiang H. Schmidt AB. Olfson M. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- MTA CG. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Offord DR. Boyle MH. Racine Y. Szatmari P. Fleming JE. Sanford M. Lipman EL. Integrating assessment data from multiple informants. J Am Acad Child Adolesc Psychiatry. 1996;35:1078–1085. doi: 10.1097/00004583-199608000-00019. [DOI] [PubMed] [Google Scholar]
- Perrin EC. Lewkowicz C. Young MH. Shared vision: Concordance among fathers, mothers, and pediatricians about unmet needs of children with chronic health conditions. Pediatrics. 2000;105:277–285. [PubMed] [Google Scholar]
- Reynolds CR. Kamphaus RR. Behavior Assessment System for Children: Manual. Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- Schill MT. Kratochwill TR. Gardner WI. Conducting a functional analysis of behavior. In: Breen MJ, editor; Fiedler CR, editor. Behavioral Approach to Assessment of Youth with Emotional/Behavioral Disorders: A Handbook for School-Based Practitioners. Austin, TX US: PRO-ED; 1996. pp. 83–179. [Google Scholar]
- Spitzer RL. Psychiatric diagnosis: Are clinicians still necessary? Comprehensive Psychiatry. 1983;24:399–411. doi: 10.1016/0010-440x(83)90032-9. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Thissen D. Using effect sizes for research reporting: Examples using item response theory to analyze differential item functioning. Psychological Methods. 2006;11:402–415. doi: 10.1037/1082-989X.11.4.402. [DOI] [PubMed] [Google Scholar]
- Thissen D. Steinberg L. Wainer H. Detection of differential item functioning using the parameters of item response models. In: Holland PW, editor; Wainer H, editor. Differential Item Functioning. Hillsdale, NJ: Erlbaum; 1993. pp. 67–113. [Google Scholar]
- Wagner KD. Hirschfeld RMA. Emslie GJ. Findling RL. Gracious BL. Reed ML. Validation of the Mood Disorder Questionnaire for bipolar disorders in adolescents. J Clin Psychiatry. 2006;67:827–830. doi: 10.4088/jcp.v67n0518. [DOI] [PubMed] [Google Scholar]
- Weinstock LM. Strong D. Uebelacker LA. Miller IW. Differential item functioning of DSM- IV depressive symptoms in individuals with a history of mania versus those without: An item response theory analysis. Bipolar Disorders. 2009;11:289–297. doi: 10.1111/j.1399-5618.2009.00681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock LM. Strong D. Uebelacker LA. Miller IW. DSM-IV depressive symptom expression among individuals with a history of hypomania: A comparison to those with or without a history of mania. J Psychiatric Res. 2010;44 doi: 10.1016/j.jpsychires.2010.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodcock RW. McGrew KS. Mather N. Woodcock-Johnson III Tests of Cognitive Abilities Normative Update. Itasca, IL: Riverside; 2007. [Google Scholar]
- Young RC. Biggs JT. Ziegler VE. Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Brit J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA. Birmaher B. Findling RL. Pediatric bipolar disorder: Validity, phenomenology, and recommendations for diagnosis. Bipolar Disorders. 2008;10:194–214. doi: 10.1111/j.1399-5618.2007.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom EA. Findling RL. Calabrese JR. Who are the comorbid adolescents? Agreement between psychiatric diagnosis, youth, parent, and teacher report. J Abnormal Child Psychol. 2003;31:231–245. doi: 10.1023/a:1023244512119. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA. Freeman AJ. Jenkins MM. The assessment of children and adolescents with bipolar disorder. Child Adolesc Psychiatric Clinics North America. 2009;18:353–390. doi: 10.1016/j.chc.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom EA. Gracious BL. Danielson CK. Findling RL. Calabrese JR. Toward an integration of parent and clinician report on the Young Mania Rating Scale. J Affective Dis. 2003;77:179–190. doi: 10.1016/s0165-0327(02)00108-8. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA. Meyers O. Demeter CA. Youngstrom J. Morello L. Piiparinen R. Feeny N. Calabrese JR. Findling RL. Comparing diagnostic checklists for pediatric bipolar disorder in academic and community mental health settings. Bipolar Disorders. 2005;7:507–517. doi: 10.1111/j.1399-5618.2005.00269.x. [DOI] [PubMed] [Google Scholar]