Abstract
Background/Aims
Around 70,000–80,000 Danes suffer from dementia. As average life expectancy increases, the number of people suffering from dementia is expected to increase in the future with informal care provided by family and friends becoming more important. The aim of this study was to estimate the time spent by family and friends on informal care of persons suffering from dementia in a Danish setting and calculate the economic implications.
Methods
Information on informal care time was collected in a postal survey of members of the Danish Alzheimer's Association. Data from 469 informal caregivers were obtained corresponding to an adjusted response rate of 62%.
Results
On a typical day, informal care time was 4.97–6.91 h for primary caregivers and 0.70–1.06 h for other caregivers. Using the proxy good method to value informal care, daily costs ranged between EUR 160 and 223 for primary caregivers and between EUR 23 and 34 for others.
Conclusion
Informal care delivered by family and friends is significant. The value of informal care constitutes an important part of the societal cost of dementia in Denmark.
Key Words: Alzheimer's disease, Dementia, Denmark, Economics, Family caregiver, Health care surveys, Informal care
Introduction
More than 34 million people are suffering from dementia worldwide, with more than 9 million people living in Europe [1]. In Denmark, around 70–80,000 people suffer from dementia, corresponding to 1.3% of the population [2]. The most frequent cause of dementia is Alzheimer's disease, representing 60–70% of the cases in Europe [3]. With increasing life expectancy in Europe, the number of people suffering from dementia is expected to grow in the future as the incidence rate rises with age.
Dementia is characterized by deterioration in intellectual capacity that impairs independent functioning in everyday life [4]. Cognitive and functional impairment increases as the disease progresses: starting with difficulty with instrumental activities of daily living (IADLs), e.g. cooking, shopping or taking care of economic matters, and ending with the loss of ability to perform basic activities of daily living (ADLs), e.g. dressing, hygiene or eating [5]. The cognitive and functional impairment results in an increasing dependence and need for care with progressing disease. This was shown by Stern et al. [6] in 1994, who developed the dependence scale aiming at linking the required amount of assistance from others to Alzheimer's patients with the progression of disease. The content validity of the dependence scale was recently tested and approved by Frank et al. [7] in 2010. In some cases, progression of the disease can be decelerated or symptoms can be relieved with proper medical treatment [8].
The costs of dementia are significant. Besides direct costs related to treatment and formal care in the healthcare sector and the social care sector, there are indirect costs associated with informal care provided by family and friends.
Informal care covers a wide range of different activities carried out by family or friends, including ADLs, IADLs and supervision. Informal care differs from formal care as the informal caregiver does not receive any payment or alternatively payment below market wages [9].
Studies have shown that informal caregivers – i.e. family and friends – play a substantial role in caring for people suffering from dementia and that informal care time accounts for a considerable part of the societal costs associated with dementia [3]. In a recent study, the total societal worldwide costs of dementia were estimated to be USD 608 billion, of which the costs of informal care amounted to USD 329 billion when ADLs and IADLs were considered [1]. This is a rough estimate based on the cost model in the Dementia Worldwide Cost Database with standard assumptions about informal care time (3.7 h/day). In reality, informal care time varies across countries due to differences in the institutional setting and level of services, which highlight the need for having country-specific data.
A previous Danish population-based study estimated the direct costs of dementia in Denmark, including hospital and physician services, community services and nursing home care, but did not include informal care [10]. Information on informal care time related to dementia in Denmark has been collected as a part of studies covering the Nordic and European countries. However, the samples of Danish informal caregivers included in these studies were rather small [11, 12]. There are no previous studies based on larger sample sizes that address the costs of informal care related to dementia in Denmark.
The demand for informal care is likely to increase due to the aging of the population and some rationing of formal care in countries such as Denmark. Therefore, it becomes even more important to estimate the amount of time spent on informal care of persons suffering from dementia and the associated costs with a view to attracting the attention of decision-makers and the public, as well as to include such costs in economic evaluations of dementia care in the future.
The aim of the present study was therefore twofold. First, the study investigated and estimated time spent by family and friends on informal care of persons suffering from dementia in a Danish setting. Secondly, the study valued this time and estimated the costs of informal care related to dementia in Denmark.
Materials and Methods
Data Collection
The study was designed as a postal self-administered questionnaire to members of the Danish Alzheimer's Association. The Danish Alzheimer's Association is a voluntary organization with the aim to improve the conditions for people suffering from dementia and their relatives. Members are patients, relatives and others.
At the end of September 2010, an information letter about the study together with a questionnaire about time spent on care of relatives suffering from dementia by primary and other informal caregivers was sent to 1,000 members randomly selected among all household members of the Danish Alzheimer's Association. The primary caregiver was asked to fill out and return the questionnaire using a pre-stamped addressed envelope – hereby giving his or her informed consent to participate in the study. Participation was voluntary and consent to participate could be withdrawn at any time. A reminder was sent out after 2 weeks with a deadline by the end of October 2010.
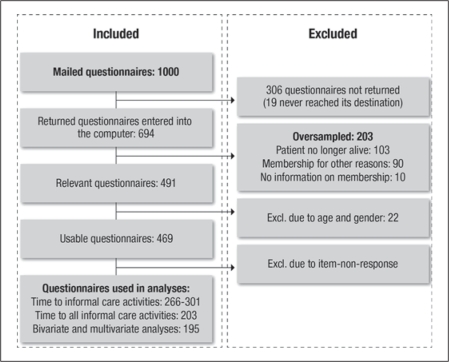
As illustrated in figure 1, 694 members returned the questionnaire corresponding to a response rate above 70% (19 questionnaires never reached their destination). Among the 694 questionnaires, 203 were found ineligible either because the person with dementia had died (103), the respondent did not have a relative with dementia (90) or further information was missing (10). Moreover, additional 22 questionnaires were excluded due to an unlikely low age stated for the person with dementia (<50 years) or low age of the primary caregiver (<20 years). The final study population therefore consisted of 469 primary caregivers (adjusted response rate was 62% when excluding those mentioned above without living relatives with dementia, for example).
Fig. 1.
Reasons for the inclusion or exclusion of respondents in the analysis.
Various instruments have been developed to assess informal care time. Most apply the recall method, e.g. the Caregiver Activities Time Survey (CATS), the Caregiver Activity Survey and the Resource Utilization in Dementia instrument [13, 14, 15, 16, 17], as it is less time consuming than the diary method or direct observations, which are regarded as the gold standard [16, 17].
The questionnaire used in this study was developed with inspiration from existing instruments, most notably the CATS instrument [13]. Respondents were asked to estimate, in hours and minutes, the amount of time spent on a typical day on different activities related to care of the person suffering from dementia, including ADLs, IADLs and supervision. The CATS instrument was modified by including activities such as cooking and shopping. This was done to make the instrument better suited to a Danish context and to take into account criticism of the CATS instrument for not systematically assessing all activities that can be part of informal care [18, 19]. Furthermore, the time spent on informal care by both primary and other caregivers was included [18, 19]. Finally, the questionnaire included questions about the characteristics of the respondent as well as assessment questions. A pilot test of the questionnaire among eight members of the Danish Alzheimer's Association found it to be relevant, easily understood and simple to fill out.
It was assumed that primary and other caregivers could spend no more than 24 h on informal care per day. If the sum of the reported time spent on different informal care activities exceeded 24 h, then the time spent on supervision was reduced and if this was not sufficient, the time spent on other informal care activities was scaled down as well. This method is in accordance with the method applied by others [15, 19]. All questions relating to time spent on different caregiver activities were based on the number of hours/minutes spent on these activities on a typical day.
In valuing the informal care time, the proxy good method was used in the baseline analysis. The reason for choosing this method is that it values informal care time at the (labour) market price of a close substitute, such as a professional caregiver, that could have delivered some of the informal care if decided at the political level. The average wage rate of a professional caregiver with vocational training employed in the Danish municipal sector was used (the wage rate was inflation adjusted to autumn 2010). In sensitivity analyses, two other methods of valuation of informal care time were applied. The first is the opportunity cost method, where time is valued with the market-based wage rate of the individual caregiver, i.e. the informal caregiver's benefits foregone due to spending time on providing informal care (in this study, age- and gender-adjusted mean wages were applied). The second is the loss-of-production method, where time is valued as lost production to society due to the caregiver's time spent on informal care (calculated as the opportunity cost method, but time spent on informal care during weekends and holidays and by caregivers outside the labour market was not included).
When relevant for comparison purposes, cost estimates have been inflation adjusted based on the Gross Domestic Product deflator of the country or group of countries in question, and conversion to euros has been conducted based on the average exchange rate in October 2010.
The study was approved by the Danish Data Protection Agency (2010-41-4613). Approval from an ethics committee was not required by Danish law since the study did not involve collection of or research on biological material.
Statistical Methods
The average time that the primary and other informal caregivers spent in total and on different activities related to care of their relative suffering from dementia was estimated for a typical day. Missing values on the specific time spent on an activity were handled using three different strategies to show its impact. Strategy 1: missing data count as missing and are excluded from the analyses; strategy 2: missing data are set to zero, and strategy 3: missing data are set to the conditional mean of the time spent on the activity by the rest of the respondents. Both bivariate analyses and multivariate regression analyses were applied to examine factors influencing informal care time, such as sex, age, the type of relationship between the person suffering from dementia and the caregiver and use of formal services. In these analyses, missing data counted as missing (strategy 1). For the bivariate analyses, non-parametric tests were used as the parametric assumptions were not fulfilled in all cases. A level of 5% significance was chosen. In the multivariate regression analysis, a Tobit model was used as this model was considered best suited to fit the skewed nature of the available time data. Time spent on supervision was not included in the multivariate regression analysis to ensure fulfillment of model assumptions. Two models were estimated – a small and a large model in terms of number of covariates. The statistical program SAS 9.2 (SAS Institute Inc., Cary, N.C., USA) was used to analyze data.
Results
A total of 469 primary caregivers were included in the study. Their average age was 66 years, and 67% were women. The majority of the caregivers (76%) were the spouse/partner of the person suffering from dementia while 21% were the daughter/son of the demented; 56% of the caregivers lived together with the demented. About one third of the caregivers were working – either full time (23%) or part time (10%). The average age of the persons suffering from dementia was 75 years. Nearly all of them (97%) had been diagnosed, the majority (77%) with Alzheimer's disease. The persons suffering from dementia lived in different regions of Denmark covering both urban and rural areas. The majority lived at home (61%), and about one third lived in a care facility (35%).
As table 1 shows, time spent on informal care, including supervision, was estimated to be on average 5.85 h on a typical day for the primary caregiver (95% confidence interval: 4.77–6.93) and 0.70 h for other caregivers (95% confidence interval: 0.35–1.05) when missing data counted as missing. When missing data were set to zero or the conditional mean, time spent on informal care was estimated to be either 4.97 or 6.91 h, respectively, for the primary caregiver and 0.73 or 1.06 h, respectively, for other caregivers. For all three strategies of handling missing data, this corresponds to average costs between EUR 160 and 223 per day for primary caregivers and between EUR 23 and 34 per day for other caregivers when the informal care time is valued by the proxy good method, i.e. where the cost per hour of informal care is set equal to the average wage rate of a professional caregiver. Using the opportunity cost method for valuation of informal care time resulted in average costs between EUR 187 and 260 per day for the primary caregiver and between EUR 26 and 39 per day for other caregivers, whereas the use of the loss-of-production method resulted in average costs only between EUR 35 and 45 per day for the primary caregiver and between EUR 9 and 14 per day for other caregivers. The reason for the low cost estimates using the loss-of-production method is that the time spent on informal care during weekends/holidays as well as by caregivers outside the labour market was not included.
Table 1.
Time and value of informal care
| n | Mean | Median | SD | Proportion |
||
|---|---|---|---|---|---|---|
| with 0 h | with 24 h | |||||
| Time spent on informal care, h | ||||||
| Primary caregiver | ||||||
| Missing counts as missing | 203 | 5.85 | 2 | 7.86 | 12% | 10% |
| Missing set to zero | 321 | 4.97 | 1.5 | 7.44 | 22% | 9% |
| Missing set to conditional mean | 321 | 6.91 | 3.6 | 7.68 | 7% | 9% |
| Other caregivers | ||||||
| Missing counts as missing | 297 | 0.70 | 0 | 3.12 | 82% | 1% |
| Missing set to zero | 321 | 0.73 | 0 | 3.06 | 80% | 1% |
| Missing set to conditional mean | 321 | 1.06 | 0 | 3.38 | 75% | 1% |
| Value of informal time, EUR1 | ||||||
| Primary caregiver | ||||||
| Missing counts as missing | 203 | 188.74 | 64.48 | 253.35 | 12% | |
| Missing set to zero | 321 | 160.38 | 48.36 | 239.97 | 22% | |
| Missing set to conditional mean | 321 | 222.83 | 116.04 | 247.52 | 7% | |
| Other caregivers | ||||||
| Missing counts as missing | 297 | 22.66 | 0.00 | 100.67 | 82% | |
| Missing set to zero | 321 | 23.66 | 0.00 | 98.52 | 80% | |
| Missing set to conditional mean | 321 | 34.28 | 0.00 | 109.10 | 75% | |
Currency rate: 7.4567 (October 2010, Danmarks Nationalbank).
Only 203 of the 469 respondents were included in the estimation of informal care time of the primary caregiver when missing data counted as missing. Analyses of dropouts revealed that non-respondents were older than respondents and more often not living together with the relative suffering from dementia (he or she was living in a care facility).
Most of the informal care time is spent on supervision (table 2). The primary caregivers answering that they spent time on supervision (30%) spent on average above 8 h on a typical day on this activity. Most caregivers answered that they spent time on finding lost things and administering medication, i.e. more than half of the primary caregivers answered that they spent time on such activities. The average time spent on finding lost things and on administering medication is 0.49 and 0.19 h, respectively, on a typical day for the caregivers in question.
Table 2.
Quantity of informal care (hours per day)
| Primary caregiver |
Other caregivers |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | proportion with time >0 | max | mean | conditional mean | n | proportion with time >0 | max | mean | conditional mean | |
| Toilet visits | 305 | 0.19 | 7.00 | 0.15 | 0.81 | 320 | 0.06 | 1.00 | 0.03 | 0.57 |
| Grooming and bathing | 301 | 0.32 | 24.00 | 0.27 | 0.82 | 317 | 0.07 | 2.00 | 0.05 | 0.66 |
| Dressing | 296 | 0.37 | 5.00 | 0.16 | 0.44 | 316 | 0.06 | 1.25 | 0.03 | 0.52 |
| Taking medication | 290 | 0.53 | 0.75 | 0.10 | 0.19 | 315 | 0.06 | 0.50 | 0.01 | 0.21 |
| Eating | 301 | 0.27 | 5.25 | 0.24 | 0.90 | 315 | 0.03 | 1.50 | 0.03 | 0.78 |
| Transportation | 274 | 0.35 | 4.50 | 0.28 | 0.81 | 319 | 0.06 | 3.00 | 0.04 | 0.69 |
| Shopping | 284 | 0.45 | 2.17 | 0.29 | 0.65 | 316 | 0.06 | 2.50 | 0.04 | 0.67 |
| Escorting | 266 | 0.39 | 4.00 | 0.35 | 0.89 | 311 | 0.08 | 6.00 | 0.09 | 1.22 |
| Cooking | 291 | 0.41 | 14.00 | 0.60 | 1.45 | 314 | 0.04 | 2.00 | 0.03 | 0.80 |
| Find things that are lost | 277 | 0.55 | 3.00 | 0.27 | 0.49 | 312 | 0.05 | 1.00 | 0.02 | 0.31 |
| Disturbances at night | 292 | 0.27 | 19.92 | 0.42 | 1.58 | 316 | 0.02 | 1.50 | 0.02 | 0.84 |
| Supervision | 283 | 0.30 | 24.00 | 2.46 | 8.18 | 314 | 0.08 | 22.23 | 0.35 | 4.29 |
| All | 203 | 0.88 | 24.00 | 5.85 | 6.64 | 297 | 0.18 | 24.00 | 0.70 | 4.01 |
Bivariate and multivariate analyses showed that caregivers who live together with and/or are married to the person suffering from dementia spent significantly more time on informal care, as illustrated in tables 3 and 4. Age, gender, type of dementia and the region of Denmark where the person suffering from dementia lives did not have a statistically significant impact on informal care time.
Table 3.
Bivariate analyses of time of informal care (without supervision) in hours (n = 195)
| n | Mean | SD | p value | ||
|---|---|---|---|---|---|
| Caregiver gender | Male | 74 | 3.814 | 4.591 | 0.1982 |
| Female | 121 | 2.978 | 3.909 | ||
| Caregiver age | 20–49 years | 16 | 1.351 | 2.021 | 0.0003 |
| 50–59 years | 47 | 2.622 | 4.326 | ||
| 60–69 years | 68 | 3.744 | 4.656 | ||
| 70–79 years | 45 | 3.000 | 2.654 | ||
| ≥80 years | 19 | 5.693 | 5.330 | ||
| Labour market | Working, full time | 46 | 2.141 | 3.964 | 0.0006 |
| Working, part time | 24 | 2.986 | 3.970 | ||
| Other status | 6 | 9.583 | 9.406 | ||
| Not working | 119 | 3.487 | 3.668 | ||
| Relation to patient | Spouse | 149 | 3.977 | 4.499 | <0.0001 |
| Other relation | 46 | 1.087 | 1.599 | ||
| Patient gender | Male | 100 | 3.364 | 4.177 | 0.6500 |
| Female | 95 | 3.223 | 4.223 | ||
| Patient age | 50–64 years | 42 | 3.383 | 4.494 | 0.1418 |
| 65–79 years | 104 | 3.561 | 4.094 | ||
| ≥80 years | 49 | 2.656 | 4.140 | ||
| Type of dementia | Alzheimer's disease | 152 | 3.257 | 4.305 | 0.3046 |
| Other dementia | 43 | 3.429 | 3.795 | ||
| Area | Big city | 51 | 2.724 | 3.221 | 0.8902 |
| Town | 117 | 3.366 | 4.049 | ||
| Country | 27 | 4.067 | 6.045 | ||
| Region | Western Denmark | 28 | 3.597 | 3.418 | 0.7683 |
| Northern Denmark | 14 | 4.752 | 6.687 | ||
| Eastern Denmark | 37 | 3.350 | 4.077 | ||
| Southern Denmark | 39 | 3.768 | 5.487 | ||
| Capital region | 77 | 2.655 | 3.018 | ||
| Formal care | Nursing home | 41 | 2.220 | 3.462 | 0.0005 |
| Home care | 65 | 4.004 | 3.869 | ||
| Other care | 37 | 4.176 | 5.327 | ||
| No help | 52 | 2.631 | 3.994 | ||
For two categories, the Mann-Whitney U test with normal approximation was employed, and for more than two categories, the Kruskal-Wallis χ2 test.
Table 4.
Tobit regression model of time to informal care (in hours)
| Variable | Model 1 (n = = 202) |
Model 2 (n = = 195) |
|||||
|---|---|---|---|---|---|---|---|
| coefficient | t test p value | partial effects | coefficient | t test p value | partial effects | ||
| Constant | Intercept | −4.048 | 0.2293 | −8.164 | 0.0309 | ||
| Labour market | Working, full time | 0.252 | 0.7799 | 0.183 | 0.905 | 0.3319 | 0.676 |
| Working, part time | 1.402 | 0.1910 | 1.079 | 1.752 | 0.1040 | 1.362 | |
| Other status | 5.133 | 0.0023 | 4.455 | 7.018 | 0.0002 | 6.295 | |
| Not working | reference | reference | |||||
| Relation to patient | Spouse | 4.775 | <0.0001 | 3.039 | 5.326 | <0.0001 | 3.374 |
| Other relation | reference | reference | |||||
| Patient age/gender | Female gender | 0.749 | 0.2527 | 0.561 | 0.784 | 0.2446 | 0.597 |
| Age | 0.036 | 0.3217 | 0.027 | 0.067 | 0.0920 | 0.051 | |
| Type of dementia | Alzheimer's disease | −0.239 | 0.7418 | −0.181 | −0.075 | 0.9211 | −0.057 |
| Other dementia | reference | reference | |||||
| Area | Big city | −0.389 | 0.7382 | −0.284 | |||
| Town | 0.531 | 0.5896 | 0.407 | ||||
| Country | reference | ||||||
| Region | Western Denmark | 0.008 | 0.9940 | 0.006 | |||
| Northern Denmark | 1.763 | 0.1853 | 1.406 | ||||
| Eastern Denmark | 0.401 | 0.6802 | 0.301 | ||||
| Southern Denmark | 0.773 | 0.3611 | 0.590 | ||||
| Capital region | reference | ||||||
| Formal care | Nursing home | −0.223 | 0.8278 | −0.158 | |||
| Home care | 1.302 | 0.1349 | 1.000 | ||||
| Other care | 0.899 | 0.3384 | 0.677 | ||||
| No help | reference | ||||||
σ: Model 1: 4.203; model 2: 4.062.
Discussion
This study provides an estimate of time spent on and costs associated with informal care for persons suffering from dementia in Denmark. Time spent on informal care, including supervision, was estimated to be on average 5.85 h on a typical day for the primary caregiver and 0.70 h for other caregivers when missing data counted as missing. This corresponds to average costs of EUR 189 per day for primary caregivers and EUR 23 per day for other caregivers when the informal care time is valued by the proxy good method or annual costs of EUR 77,380 per person suffering from dementia when a typical day is considered to be an approximation to an average day.
Compared with previous studies, the number of respondents in the present study is one of its major strengths. However, the study population is not necessarily representative of informal caregivers and their relatives suffering from dementia in general. Other studies have shown that progression of the disease increases the time spent by informal caregivers on care when relatives suffering from dementia are still living at home [4, 12]. Nearly all the persons suffering from dementia who were included in the present study as relatives to the primary caregivers had been diagnosed with dementia. Because the onset of dementia is insidious, many persons suffering from dementia are not diagnosed when symptoms are mild [8]. This indicates that the severity of the disease of the persons included in this study might have been above average. This is supported by the fact that about one third of the persons suffering from dementia included in the present study live in a care facility. It is unclear how this affects the estimated time spent on informal care. On the one hand, disease progression will tend to increase the time estimate as long as the person suffering from dementia is living at home. On the other hand, disease progression will ultimately result in the person suffering from dementia being moved to a care facility which will tend to decrease the time estimate.
Furthermore, the study may be subject to non-response bias. Our analysis of respondents versus non-respondents (dropouts) showed that more often non-respondents did not live together with their relative suffering from dementia as was the case with respondents. As living together with a person suffering from dementia was found to be a predictor of informal care time, it is possible that the present study overestimates informal care time compared to the time actually spent by the 469 respondents included in the study.
Moreover, informal care time may be overestimated since the study relies on caregivers volunteering to participate in the survey. These caregivers may be more involved in the care of persons suffering from dementia than the average caregiver.
The estimated informal care time is based on information from primary caregivers. This is normal for these types of studies but still introduces the risk of recall bias, especially in terms of information on time spent on informal care by other caregivers. Furthermore, the information collected may be inexact as it is sometimes difficult to distinguish between normal household activities and informal care. Moreover, supervision is difficult to express in quantitative terms. Joint production, defined as doing two or more activities at the same time by one person, is another complicating factor, especially when e.g. leisure activities are combined with providing informal care, e.g. watching television and supervision [9].
We did not use one of the existing questionnaire instruments for estimating informal care time but developed our own with inspiration from existing instruments, most notably the CATS instrument. The major reason for designing a specific questionnaire was to make the instrument better suited to a Danish context and the purpose of the present study. We wanted to include all activities representing informal care, such as cooking and shopping, which are left out of the CATS instrument. Furthermore, we wanted to include the time spent on informal care by both primary and other caregivers in our survey. A pilot test of the final questionnaire was carried out to secure the validity and reliability of the questionnaire. It is therefore not assumed to be a problem to use a modified instrument.
Cost estimates of informal care are most commonly calculated using individual or societal lost earnings (opportunity cost method) or using formal care and domestic service replacement costs (proxy good method) [20]. The latter method has been applied in the present study. Since there is controversy over methods for valuing informal care, different approaches were compared in the sensitivity analyses, as presented above. The results of these sensitivity analyses showed that the opportunity cost method and the loss-of-production method formed an upper and a lower limit for the cost estimates of informal care. In the present study, the proxy good method was chosen because the method provides the most pragmatic estimate, namely an estimate of the costs that would be imposed on the healthcare/social care sector and ultimately the taxpayers if informal care was not provided by family and friends but had to be delivered by professional caregivers.
Several other studies have assessed the time informal caregivers spend on providing care for persons suffering from dementia and the associated costs [4, 11, 12, 13, 14, 15, 18, 19, 21, 22, 23]. The results vary greatly, which is partly due to the different definitions of informal care, the setting of the study and the characteristics of the study population with regard to the severity of the disease, for example [24]. Recognition of dependence as a distinct, measurable component of the dementing disease in relation to the progression of the disease may also explain differences between studies [6]. Problems related to quantifying with accuracy the amount of time spent probably also explain some of the variability. Furthermore, the choice of principle for valuing informal care has great importance for the cost estimates.
The estimated time spent on informal care per day by primary caregivers and other caregivers found in the present study based on a Danish sample of informal caregivers to persons suffering from dementia is similar to findings of German studies [18, 19]. Furthermore, the results are in line with a study covering the Nordic countries where the informal care time was estimated to be between 2 and 9 h per day for patients living in the community depending on disease severity [12]. Our results are also in accordance with American studies of patients with moderate-to-severe dementia or a high dependence scale score [4, 23].
Two previous studies have collected information on informal care time related to dementia in Denmark. In a recent study by Gustavsson et al. [11] of 1,381 persons with Alzheimer's disease living at home and attending memory clinics in 12 European countries, the estimated average annual cost of informal care per patient valued at the opportunity cost of the caregiver's time (lost production) corresponded to EUR 4,600 in 2010. There was substantial variability in the reported amount of informal care between countries. The study only included 43 persons with dementia from Denmark, which limits the ability to generalize the results to a Danish setting. In another study by Jönsson et al. [12], the costs of medical care, community care and informal care of 272 persons with Alzheimer's disease attending memory clinics in Sweden, Norway, Denmark and Finland were estimated; 45% of the study sample was from Sweden. The authors found that the estimated average annual costs of informal care valued at the opportunity cost of the caregiver's time (lost production) corresponded to about EUR 4,850 in 2010. Although no significant difference in resource utilization between the four countries was found, the study was not designed or powered to detect such differences. The cost estimates of both the study by Gustavsson et al. [11] and Jönsson et al. [12] are significantly lower than the estimated costs in the present study due to the choice of a different valuation method.
From a societal perspective, informal care accounts for a large proportion of societal resources spent on care for the 70,000–80,000 persons suffering from dementia in Denmark today. Informal care can postpone the point in time when a person suffering from dementia has to be institutionalized and live in some sort of publicly run care facility with annual costs between EUR 47,000 and 67,000 per patient per year [25]. From a central and local governmental point of view, it may well be an economic advantage to enable people suffering from dementia to live at home longer by securing adequate early intervention and support programs, as well as supporting and acknowledging the importance of informal care provided by family and friends.
Disclosure Statement
COWI has received funding from Pfizer Denmark ApS to conduct the research project. Peter Bo Poulsen and Troels Reiche are employees of Pfizer Denmark ApS.
References
- 1.Wimo A, Winblad B, Jonsson L. The worldwide societal costs of dementia: estimates for 2009. Alzheimers Dement. 2010;62:98–103. doi: 10.1016/j.jalz.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 2.www.demensnet.dk (accessed 2-5-2011).
- 3.Jonsson L, Wimo A. The cost of dementia in Europe: a review of the evidence, and methodological considerations. Pharmacoeconomics. 2009;275:391–403. doi: 10.2165/00019053-200927050-00004. [DOI] [PubMed] [Google Scholar]
- 4.Langa KM, Chernew ME, Kabeto MU, Herzog AR, Ofstedal MB, Willis RJ, Wallace RB, Mucha LM, Straus WL, Fendrick AM. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. J Gen Intern Med. 2001;1611:770–778. doi: 10.1111/j.1525-1497.2001.10123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mauskopf J, Racketa J, Sherrill E. Alzheimer's disease: the strength of association of costs with different measures of disease severity. J Nutr Health Aging. 2010;148:655–663. doi: 10.1007/s12603-010-0312-6. [DOI] [PubMed] [Google Scholar]
- 6.Stern Y, Albert SM, Sano M, Richards M, Miller L, Folstein M, Albert M, Bylsma FW, Lafleche G. Assessing patient dependence in Alzheimer's disease. J Gerontol. 1994;49:M216–M222. doi: 10.1093/geronj/49.5.m216. [DOI] [PubMed] [Google Scholar]
- 7.Frank L, Howard K, Jones R, Lacey L, Leibman C, Lleo A, Mannix S, Mucha L, McLaughlin T, Zarit S. A qualitative assessment of the concept of dependence in Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2010;25:239–247. doi: 10.1177/1533317509356690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu CW, Sano M. Economic considerations in the management of Alzheimer's disease. Clin Interv Aging. 2006;12:143–154. doi: 10.2147/ciia.2006.1.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van den Berg B, Brouwer WB, Koopmanschap MA. Economic valuation of informal care. An overview of methods and applications. Eur J Health Econ. 2004;51:36–45. doi: 10.1007/s10198-003-0189-y. [DOI] [PubMed] [Google Scholar]
- 10.Kronborg Andersen C, Sogaard J, Hansen E, Kragh-Sorensen A, Hastrup L, Andersen J, Andersen K, Lolk A, Nielsen H, Kragh-Sorensen P. The cost of dementia in Denmark: the Odense Study. Dement Geriatr Cogn Disord. 1999;104:295–304. doi: 10.1159/000017135. [DOI] [PubMed] [Google Scholar]
- 11.Gustavsson A, Jonsson L, Rapp T, Reynish E, Ousset PJ, Andrieu S, Cantet C, Winblad B, Vellas B, Wimo A. Differences in resource use and costs of dementia care between European countries: baseline data from the ICTUS study. J Nutr Health Aging. 2010;148:648–654. doi: 10.1007/s12603-010-0311-7. [DOI] [PubMed] [Google Scholar]
- 12.Jönsson L, Eriksdotter Jönhagen M, Kilander L, Soininen H, Hallikainen M, Waldemar G, Nygaard H, Andreasen N, Winblad B, Wimo A. Determinants of costs of care for patients with Alzheimer's disease. Int J Geriatr Psychiatry. 2006;21:449–459. doi: 10.1002/gps.1489. [DOI] [PubMed] [Google Scholar]
- 13.Clipp EC, Moore MJ. Caregiver time use: an outcome measure in clinical trial research on Alzheimer's disease. Clin Pharmacol Ther. 1995;582:228–236. doi: 10.1016/0009-9236(95)90201-5. [DOI] [PubMed] [Google Scholar]
- 14.Davis KL, Marin DB, Kane R, Patrick D, Peskind ER, Raskind MA, Puder KL. The Caregiver Activity Survey (CAS): development and validation of a new measure for caregivers of persons with Alzheimer's disease. Int J Geriatr Psychiatry. 1997;1210:978–988. doi: 10.1002/(sici)1099-1166(199710)12:10<978::aid-gps659>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Wimo A, Nordberg G, Jansson W, Grafstrom M. Assessment of informal services to demented people with the RUD instrument. Int J Geriatr Psychiatry. 2000;1510:969–971. doi: 10.1002/1099-1166(200010)15:10<969::aid-gps272>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 16.Wimo A, Nordberg G. Validity and reliability of assessments of time. Comparisons of direct observations and estimates of time by the use of the resource utilization in dementia (RUD)-instrument. Arch Gerontol Geriatr. 2007;441:71–81. doi: 10.1016/j.archger.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Wimo A, Jonsson L, Zbrozek A. The Resource Utilization in Dementia (RUD) instrument is valid for assessing informal care time in community-living patients with dementia. J Nutr Health Aging. 2010;148:685–690. doi: 10.1007/s12603-010-0316-2. [DOI] [PubMed] [Google Scholar]
- 18.Neubauer S, Holle R, Menn P, Grossfeld-Schmitz M, Graesel E. Measurement of informal care time in a study of patients with dementia. Int Psychogeriatr. 2008;206:1160–1176. doi: 10.1017/S1041610208007564. [DOI] [PubMed] [Google Scholar]
- 19.Neubauer S, Holle R, Menn P, Grassel E. A valid instrument for measuring informal care time for people with dementia. Int J Geriatr Psychiatry. 2009;243:275–282. doi: 10.1002/gps.2103. [DOI] [PubMed] [Google Scholar]
- 20.McDaid D. Estimating the costs of informal care for people with Alzheimer's disease: methodological and practical challenges. Int J Geriatr Psychiatry. 2001;164:400–405. doi: 10.1002/gps.353. [DOI] [PubMed] [Google Scholar]
- 21.Nordberg G, Wimo A, Jonsson L, Kareholt I, Sjolund BM, Lagergren M, von Strauss E. Time use and costs of institutionalised elderly persons with or without dementia: results from the Nordanstig cohort in the Kungsholmen Project – a population based study in Sweden. Int J Geriatr Psychiatry. 2007;227:639–648. doi: 10.1002/gps.1724. [DOI] [PubMed] [Google Scholar]
- 22.Moore MJ, Zhu CW, Clipp EC. Informal costs of dementia care: estimates from the National Longitudinal Caregiver Study. J Gerontol B Psychol Sci Soc Sci. 2001;564:S219–S228. doi: 10.1093/geronb/56.4.s219. [DOI] [PubMed] [Google Scholar]
- 23.Zhu CW, Leibman C, McLaughlin T, Zbrozek AS, Scarmeas N, Albert M, Brandt J, Blacker D, Sano M, Stern Y. Patient dependence and longitudinal changes in costs of care in Alzheimer's disease. Dement Geriatr Cogn Disord. 2008;265:416–423. doi: 10.1159/000164797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wimo A, von Strauss E, Nordberg G, Sassi F, Johansson L. Time spent on informal and formal care giving for persons with dementia in Sweden. Health Policy. 2002;613:255–268. doi: 10.1016/s0168-8510(02)00010-6. [DOI] [PubMed] [Google Scholar]
- 25.Larsen K. Plejehjemskrævende opbevares på sygehuse. Ugeskr Laeger. 2005;167:719. [Google Scholar]