Abstract
Objective
The purpose of this study was to determine if early response predicted remission at the end of a controlled trial.
Method
80 adolescents with bulimia nervosa participated in an RCT comparing family-based treatment and individual supportive psychotherapy. Response to treatment was assessed via self-report of bingeing and purging. Remission was defined as abstinence from bingeing and purging for the last 28 days and measured by investigator-based interview, i.e., the Eating Disorder Examination.
Results
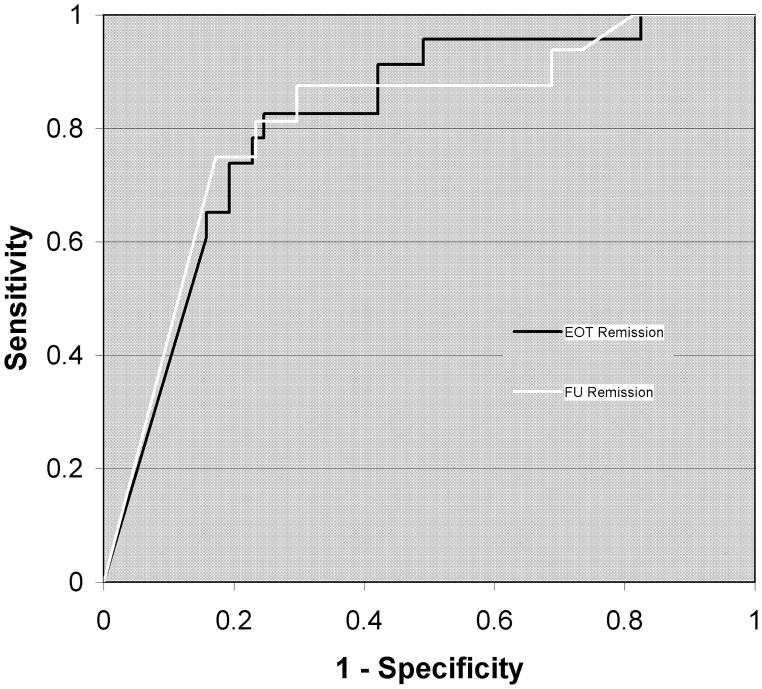
Receiver operating characteristic analyses showed that, regardless of treatment, symptom reduction at session 6 predicted remission at post-treatment (AUC = .814 (p<.001)) and 6-month follow-up (AUC = .811 (p<.001)).
Conclusion
Results suggest that adolescents with BN who do not show early reductions in bulimic symptoms are unlikely to remit at post-treatment or follow-up.
Keywords: adolescent bulimia nervosa, psychotherapy, early treatment response, receiver operating characteristics curves
Introduction
Early response to treatment in adult bulimia nervosa (BN) has been found to be a robust predictor of post-treatment outcome. In trials of cognitive behavior therapy (CBT) for BN, both with and without concurrent antidepressant medication administration, individuals who reduced bingeing and purging (reductions >50–75% from baseline levels) by the fourth week of a 16–20 week treatment protocol were more likely to be abstinent from bulimic symptoms at post-treatment.1,2 Findings are similar for BN treatment utilizing interpersonal psychotherapy (IPT)3 or desipramine.4 Across these studies, the majority of individuals could be correctly identified as responders or non-responders at post-treatment by evaluating early response to treatment, as early as week 2 but more typically by week 3 or 4 (sessions 6–8). Moreover, early response to treatment has been shown to predict longer-term outcome in adults with BN.3
Previous studies only report on treatment in adult BN samples. However, an estimated 1 to 2% of adolescent females suffer from this eating disorder and an additional 2 to 3% exhibit clinically significant bulimic symptoms that fall short of meeting full criteria for BN.5 To our knowledge, only one study, using a multivariate model, explored a range of putative predictors of outcome for adolescents with BN.6 In this study, we showed that lower eating concerns were the best predictor of outcome. Utilizing data from the same randomized controlled trial, which compared two outpatient psychotherapies7, the present study specifically examined whether early response to treatment in terms of binge and purge reductions is a predictor of outcome for adolescents with BN.
Method
Participants
The sample consisted of 80 adolescents (98% female; mean age = 16.1, SD = 1.6; mean body mass index = 22.1, SD = 3.0; mean duration of illness = 21.2, SD = 22.3 months). Participants met full DSM-IV criteria for BN (46%) or a strict definition of partial BN (54%) (i.e., all DSM-IV criteria except a binge/purge frequency of at least once per week for 6 months) and were enrolled in a randomized controlled psychotherapy trial comparing 20 sessions of outpatient family-based treatment (FBT-BN) or supportive psychotherapy (SPT) conducted over 6 months. All participants and their parents or legal guardians provided written informed consent for participation and study procedures were approved by the Institutional Review Board of The University of Chicago. For a detailed description of the study, see Le Grange, Crosby, Rathouz, & Leventhal (2007).7
Measures
All participants and their parents completed comprehensive assessments at baseline, mid-treatment, post-treatment and at 6-month follow-up. For the purposes of this report we were primarily interested in binge and purge frequency. To determine session-to-session change in the frequency of binge eating and vomiting episodes, participants were required to self-report these behaviors at the start of each treatment session. Remission, defined as abstinence from bingeing and purging for the last 28 days, was assessed by a standardized investigator-based interview, the Eating Disorder Examination (EDE).8 The EDE measures the severity of eating disorder psychopathology over the last 28 days and generates eating disorders diagnoses. The frequency of eating disorder behavior (e.g., objective binge eating and self-induced vomiting) and the severity of eating disorder attitudes are assessed, yielding four subscales: Restraint, Eating concern, Weight concern and Shape concern. The EDE has acceptable reliability, discriminant and concurrent validity and has demonstrated sensitivity to change due to treatment.8 The EDE has been widely used in adult eating disorders and found to be useful in the assessment of adolescents with eating disorders.9 The EDE was administered at baseline, post-treatment and 6-month follow-up and utilized to determine treatment outcome.
Statistical Analyses
Receiver operating characteristic (ROC) analyses were conducted to examine whether a reduction in binge-purge symptoms in early treatment sessions was predictive of remission status. ROC analyses evaluated the association between percent reductions in baseline binge-purge symptoms from sessions 1–10 and remission status at post-treatment and 6-month follow-up. Predictors were evaluated in terms of their area-under-the curve (AUC) values, which represent the probability that a randomly selected remitted case will have a greater reduction in binge-purge symptoms than a randomly selected non-remitted case.
Results
Eighty participants were included in these analyses. ROC curves revealed that reductions in binge-purge symptoms at each session were significantly associated with post-treatment remission status, with AUC values ranging from .666–.814. Symptom reduction at session 6 of treatment, which equates with week 6, was the strongest predictor of remission at post-treatment (AUC = .814 (p<.001)). A reduction in baseline binge-purge symptoms of 85% at session 6 achieved an optimal balance of sensitivity and specificity in distinguishing those that met criteria for remission at post-treatment compared to those that did not. Across treatments, 78% of patients that remitted by the end of treatment reduced their bingeing and purging by 85% or more by session 6 (i.e., sensitivity = .78). Similarly, 77% of patients that did not remit failed to reduce their bingeing and purging to this degree by session 6 (i.e., specificity = .77). ROC analyses of post-treatment remission were repeated separately by treatment group. As in the combined analysis, binge-purge reduction at week 6 was the strongest predictor of remission at post-treatment for both FBT (AUC = .736, p = .012) and SPT (AUC = .893, p = .001).
ROC curves revealed that reductions in binge-purge symptoms at each session, except session 1, were significantly associated with remission status at 6-month follow-up, with AUC values ranging from .653–.811. Reduction in binge-purge by session 6 also predicted outcome at 6-month follow-up, with 75% of remitters reducing their bingeing and purging by 93% or more and 78% of non-remitters failing to do so (AUC = .811 (p<.001)). Figure 1 shows the sensitivity and one minus specificity of the session 6 reductions in predicting remission status at post-treatment and 6-month follow-up. Separate ROC analysis of remission status at follow-up by treatment group revealed binge-purge reduction at week 6 was the best predictor for FBT participants (AUC = .816, p = .002), while binge purge reduction at week 4 was the best predictor for SPT participants (AUC = .707, p = .179).
Figure 1.
ROC Curves for Session 6 at End-of-Treatment and Six-Month Follow-up
Conclusion
Reduction in bingeing and purging by session 6 of FBT-BN or SPT predicts remission at post-treatment and at 6-month follow-up in adolescents with BN. These findings are similar to that reported for adults with BN. Agras et al.,1 found that adults receiving CBT for BN who reduced purging by 70% at week 4 (session 6) were more likely to be responders at post-treatment. Fairburn et al. (2004)3 also found that reduction in baseline purge frequency by 50% or greater at week 4 (session 6) predicted outcome at post-treatment and 8-month follow-up in adults with BN treated with either CBT or IPT.
Limitations of the current study include assessment of binge and purge frequency based on participant self-report. These findings also need to be replicated in a larger sample of adolescents with BN. A strength of this study is that it contributes to what has been a dearth of literature examining early response in adolescents with BN. While other studies have primarily examined early response in CBT for adults with BN, this study examines early response in two treatments not previously examined for adolescents with BN (i.e., FBT-BN and SPT). Additionally, this study examined the relationship of early response to remission status at both post-treatment and 6-month follow-up.
Future research is needed to determine if adolescents with BN who do not respond by session 6 of FBT-BN or SPT might benefit from a change or adjustment in treatment approach. Alternatively, for those who respond early, it is uncertain whether a full course of treatment is necessary. Dismantling studies may help clarify if there are specific treatment components presented in early sessions that may be particularly potent (e.g., focus on changing eating disorder symptoms). More research is needed to describe whether early non-responders may show certain characteristics or personality profiles different than responders, (e.g., negative affect subtyping, higher levels of psychiatric comorbidity, or increased harm avoidance).10,11 Speculatively, early non-responders may perceive treatment as less suitable or helpful or have lower treatment expectations. Finally, this study suggests a stepped care approach may be appropriate for addressing the treatment needs of both adolescent BN early responders and non-responders.
Acknowledgments
This research was supported by grant K23 MH001923 from the National Institute of Mental Health, MD, USA (Dr le Grange). Dr. le Grange receives royalties from Guilford Press and Dr. Crosby receives royalties from American Psychiatric Press.
References
- 1.Agras W, Crow SJ, Halmi KA, Mitchell JE, Wilson G, Kraemer HC. Outcome predictors for the cognitive behavior treatment of bulimia nervosa: Data from a multisite study. Am J Psychiatry. 2000;157:1302–1308. doi: 10.1176/appi.ajp.157.8.1302. [DOI] [PubMed] [Google Scholar]
- 2.Wilson GT, Loeb KL, Walsh BT, Labouvie E, Petkova E, Liu X, et al. Psychological versus pharmacological treatments of bulimia nervosa: Predictors and processes of change. J Cons Clin Psychol. 1999;67:451–459. doi: 10.1037//0022-006x.67.4.451. [DOI] [PubMed] [Google Scholar]
- 3.Fairburn CG, Agras W, Walsh B, Wilson G, Stice E. Prediction of outcome in bulimia nervosa by early change in treatment. Am J Psychiatry. 2004;161:2322–2324. doi: 10.1176/appi.ajp.161.12.2322. [DOI] [PubMed] [Google Scholar]
- 4.Walsh BT, Sysko R, Parides MK. Early response to desipramine among women with nulimia nervosa. Int J Eat Disord. 2006;39:72–75. doi: 10.1002/eat.20209. [DOI] [PubMed] [Google Scholar]
- 5.Flament M, Ledoux S, Choquet M, Simon Y. A population study of bulimia nervosa and subclinical eating disorders in adolescence. In: Steinhausen H, editor. Eating disorders in adolescence: Anorexia and bulimia nervosa. London: Brunner/Mazel; 1995. pp. 21–36. [Google Scholar]
- 6.Le Grange D, Crosby RD, Lock J. Predictors and moderators of outcome in family-based treatment for adolescent bulimia nervosa. J Am Acad Child Adol Psychiatry. 2008;47:464–470. doi: 10.1097/CHI.0b013e3181640816. [DOI] [PubMed] [Google Scholar]
- 7.Le Grange D, Crosby R, Rathouz P, Leventhal B. A randomized controlled comparison of family based treatment and supportive psychotherapy for adolescent bulimia nervosa. Arch Gen Psychiatry. 2007;64:1049–1056. doi: 10.1001/archpsyc.64.9.1049. [DOI] [PubMed] [Google Scholar]
- 8.Fairburn C, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment and treatment. New York: The Guilford Press; 1993. pp. 317–366. [Google Scholar]
- 9.Binford RB, Le Grange D. Adolescents with bulimia nervosa and Eating Disorder Not Otherwise Specified-Purging Only. Int J Eat Disord. 2005;38:157–161. doi: 10.1002/eat.20167. [DOI] [PubMed] [Google Scholar]
- 10.Bulik CM, Sullivan PF, Carter FA, McIntosh VV, Joyce PR. Predictors of rapid and sustained response to cognitive-behavioral therapy for bulimia nervosa. Int J Eat Disord. 1999;26:137–144. doi: 10.1002/(sici)1098-108x(199909)26:2<137::aid-eat2>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 11.Chen YE, Le Grange D. Subtyping adolescents with bulimia nervosa into “dietary-depressive’ and “depressive” subtypes. Beh Res Therapy. 2007;45:2813–2820. doi: 10.1016/j.brat.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]