Abstract
Objective
External ventricular drain (EVD) is commonly performed with a freehand technique using surface anatomical landmarks at two different cranial sites, Kocher's point and the forehead. The aim of this study was to evaluate and compare the accuracy and safety of these percutaneous ventriculostomies.
Methods
A retrospectively review of medical records and head computed tomography scans were examined in 227 patients who underwent 250 freehand pass ventriculostomy catheter placements using two different methods at two institutions, between 2003 and 2009. Eighty-one patients underwent 101 ventriculostomies using Kocher's point (group 1), whereas 146 patients underwent 149 forehead ventriculostomies (group 2).
Results
In group 1, the catheter tip was optimally placed in either the ipsilateral frontal horn or the third ventricle, through the foramen of Monro (grade 1) in 82 (81.1%) procedures, in the contralateral lateral ventricle (grade 2) in 4 (3.9%), and into eloquent structures or non-target cerebrospinal space (grade 3) in 15 (14.8%). Intracerebral hemorrhage (ICH) >1 mL developed in 5 (5.0%) procedures. Significantly higher incidences of optimal catheter placements were observed in group 2. ICH>1 mL developed in 11 (7.4%) procedures in group 2, showing no significant difference between groups. In addition, the mean interval from the EVD to ventriculoperitoneal shunt was shorter in group 2 than in group 1, and the incidence of EVD-related infection was decreased in group 2.
Conclusion
Accurate and safe ventriculostomies were achieved using both cranial sites, Kocher's point and the forehead. However, the forehead ventriculostomies provided more accurate ventricular punctures.
Keywords: Computed tomography, Freehand, Hydrocephalus, Ventriculostomy
INTRODUCTION
Percutaneous bedside ventriculostomy with the placement of a ventricular catheter is a very common neurosurgical procedure and useful adjunct for the management of acute hydrocephalus, intraventricular hemorrhage, and intracranial hypertension. This procedure is performed with a freehand technique using surface anatomical landmarks, often in an emergency room and intensive care unit.
Two different cranial sites, Kocher's point and the forehead, are commonly used for percutaneous ventriculostomy. Both technical accuracy and safety of ventricular catheter placements are of primary concern, as they are often performed by junior neurological residents. Therefore, the authors investigated and compared the accuracy and safety of two different bedside ventriculostomy techniques : at Kocher's point and at the forehead. To the best of our knowledge, this is the first study comparing the accuracy and safety of these two techniques.
MATERIALS AND METHODS
Patients
For this retrospective study, we enrolled 227 patients who underwent 250 freehand bedside ventriculostomies in two hospitals, between 2003 and 2009. Among these 250 procedures, 101 (40%) bedside ventriculostomies were performed using Kocher's point on 81 patients with acute hydrocephalus, at Dongsan Medical Center, Keimyung University (group 1). The remaining 149 (60%) freehand ventriculostomies were performed via the forehead on 146 patients at Kyungpook National University Hospital (group 2).
Techniques of freehand ventriculostomy
Ventriculostomy at Kocher's point
The following technique described by Friedman and Vries4) was used. The location for the twist drill hole and point of insertion of the ventricular catheter was the junction of the coronal suture and a parasagittal plane passing through the pupil of the ipsilateral eye. From this site, the ventricular catheter insertion was directed towards the medial canthus of the ipsilateral eye, and maintained in the coronal plane that passes through the external auditory meatus. This trajectory leads to the foramen of Monro. The catheter was passed 6 cm from the outer table of the cranium to cannulate the frontal horn and then tunneled beneath the scalp.
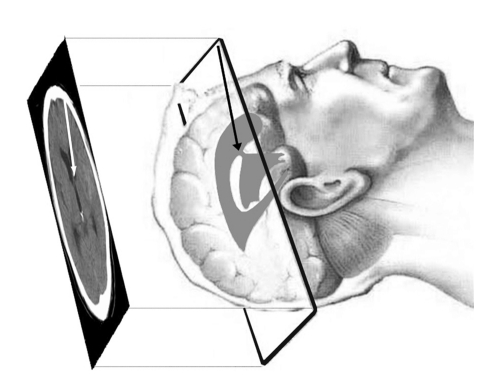
Forehead ventriculostomy using axial CT images
For computed tomography (CT) examination of the cranium, axial images are commonly obtained parallel to the orbitomeatal line, at a thickness of 5 mm. Thus, before the percutaneous ventriculostomy, the CT images were reviewed and the axial image showing the middle level of the frontal horn was selected as guidance image (Fig. 1). The location for the twist drill hole was marked on the skin based on the CT image, approximately 4 cm superior to the nasion and 3 cm lateral to the midline. After lidocaine injection, the forehead was prepared aseptically and draped, and 1 cm incision was made either in, or parallel to the skin crease. The trajectory of the drill bit was determined by tilting it from the midline based on an angle measured using the guidance CT image, in a plane parallel to the orbitomeatal plane. In other words, the twist drill hole was made with the bit directed towards a point in the frontal horn anterior to the foramen of Monro (Fig. 2). The catheter, with a stylet in place, followed the same trajectory for a measured length of 6 to 7 cm. Finally, the catheter was tunneled posteriorly under the galea aponeurotica and exited behind the hairline. The small skin incision was closed after suturing the frontalis muscle with absorbable suture material.
Fig. 1.
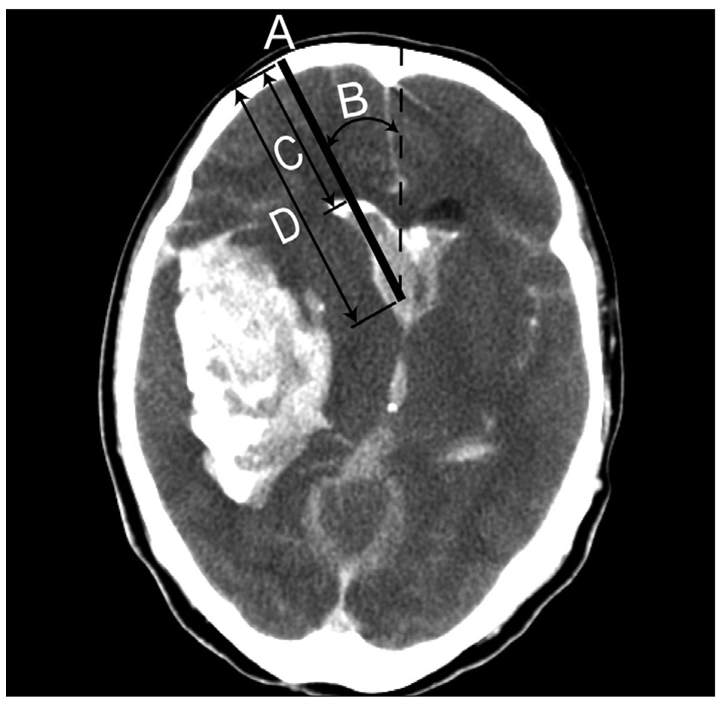
Axial computed tomography scan used as a guidance image showing ideal catheter location. The image provides information about the entrance point (A) located by the distance measured from the midline to the orbital roof, the angle between the catheter trajectory and the mid-sagittal plane (B), the depth of catheter insertion from the skull to the ventricular wall (C), and the depth of the catheter insertion from the skull to the foramen of Monro (D).
Fig. 2.
Concept of freehand forehead ventriculostomy using axial computed tomography scan as a guidance. Note that the CT image is turned over left to right. CT : computed tomography.
Accuracy assessment of ventriculostomy
The grading system proposed by Kakarla et al.8) was used to evaluate on the post-procedural CT scans the accuracy of the catheter tip location. Grade 1 represented optimal placement with the tip either in the ipsilateral frontal horn or in the third ventricle through the foramen of Monro. Grade 2 represented functional placement into the contralateral lateral ventricle. Grade 3 represented suboptimal placement into eloquent structures or non-target cerebrospinal fluid space, with or without functional drainage.
Safety assessment of ventriculostomy
Post-procedural CT scans were used to evaluate the development of procedure-related intracranial hematomas (ICH). Follow-up CT scans within a week after the procedure, were also evaluated to assess the growth of the hematomas and any delayed development of ICH related to the procedure. The ICH was defined as a hemorrhage of more than 1 mL, and trivial tract ICHs (less than 1 mL) were excluded.
CT volumetry was performed to measure the hematoma volume. PiViewStar™ software (INFINITT Co., Ltd, Seoul, Korea) was used to calculate the area of the intracranial hematoma for each axial slice, based on the manually outlined region of interest. The hematoma areas in each slice were then multiplied by the thickness of the slice and summed to determine the hematoma volume.
Statistical analysis
Data was analyzed using the SAS software version 9.12 for Windows (SAS Institute Inc., Cary, NC, USA). The Chi-square test was used for statistical comparison of the ventriculostomy methods, in terms of accuracy of the catheter placement and hemorrhage after the ventriculostomy. A p-value of less than 0.05 was considered statistically significant.
RESULTS
Patient characteristics
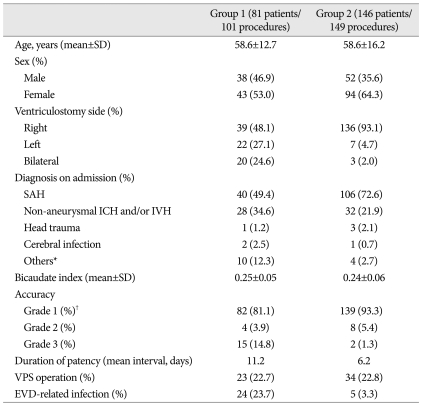
Group 1 (101 procedures on 81 patients) included the patients who underwent ventriculostomy at Kocher's point, and consisted of 38 males and 43 females. The patients' age ranged from 13 to 81 years (mean±standard deviation of the mean : 58.6±12.7 years). The right, non-dominant side was preferred for the procedure in 39 patients, whereas left ventriculostomy was performed in 22 patients; bilateral ventriculostomies were conducted in the remaining 20 patients, due to massive bilateral intraventricular hemorrhage. The acute hydrocephalus requiring ventriculostomy was caused by subarachnoid hemorrhage (n=40; 49.4%), non-aneurysmal ICH and/or intraventricular hemorrhage (n=28; 34.6%), trauma (n=1; 1.2%), infection (n=2; 2.5%), and other causes (n=10; 12.3%). The mean bicaudate index23) was 0.25±0.05 (range from 0.08 to 0.39). The mean interval from the external ventricular drain (EVD) to ventriculoperitoneal shunt (VPS) was 11.2 days. 23 (22.7%) patients who experienced weaning failure underwent direct conversion of the EVD to VPS. EVD-related infection occurred in 24 (23.7%) patients.
Group 2 (149 procedures on 146 patients) included the patients who underwent the ventriculostomy in the forehead, and consisted of 52 males and 94 females. The patients' age from 8 to 86 years (mean¡¾standard deviation : 58.6±16.2 years). The right side was preferred for the procedure in 136 patients, whereas left ventruculostomy was performed in only 7 patients; bilateral ventriculostomies were conducted in 3 patients, due to massive bilateral intraventricular hemorrhage. The acute hydrocephalus requiring ventriculostomy was caused by subarachnoid hemorrhage (n=106; 72.6%), non-aneurysmal ICH and/or intraventricular hemorrhage (n=32; 21.9%), trauma (n=3; 2.1%), infection (n=1; 0.7%), and other causes (n=4; 2.7%). The mean bicaudate index was 0.24±0.06 (range from 0.11 to 0.38). The two study groups were well matched for variables such as the patients' age and bicaudate index. The mean interval from EVD to VPS was 6.2 days. 34 (22.8%) patients who experienced weaning failure underwent direct conversion of the EVD to VPS. EVD-related infection occurred in only 5 (3.3%) patients (Table 1).
Table 1.
Summary of patients' characteristics and accuracy of ventriculostomy for group 1 (ventriculostomy at Kocher's point) and group 2 (forehead ventriculostomy)
*Others included meningitis, ischemic encephalopathy, and metabolic disorder, †p=0.0034. EVD : external ventricular drain, ICH : intracerebral hemorrhage, IVH : intraventricular hemorrhage, SAH : subarachnoid hemorrhage, SD : standard deviation, VPS : ventriculoperitoneal shunt
Accuracy of ventriculostomy
In group 1, 82 (81.1%) procedures out of a total of 101 ventriculostomies showed an optimal (grade 1) placement of the ventricular catheter, whereas 4 (3.9%) procedures showed grade 2 placement of the catheter into the contralateral lateral ventricle, and 15 (14.8%) ventriculostomies showed suboptimal grade 3 catheter placement through the ipsilateral caudate nucleus into the third ventricle.
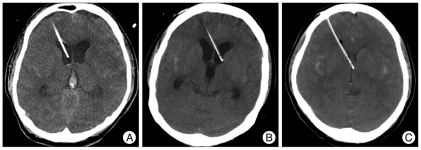
In group 2, optimal (grade 1) placement of the catheter with the tip in the ipsilateral frontal horn or in the third ventricle through the foramen of Monro was achieved in 139 (93.3%) procedures (Fig. 3A). Thus, the incidence of optimal catheter placement was significantly higher than that for group 1 (p=0.0034) (Table 1). Eight (5.4%) procedures showed functional grade 2 placement into the contralateral lateral ventricle (Fig. 3B), and only 2 (1.3%) procedures elicited suboptimal placement into the eloquent cortex or into non-target cerebrospinal fluid space (Fig. 3C).
Fig. 3.
Computed tomography images with grading system used to evaluate catheter tip location in a case of forehead ventriculostomy. A : Optimal placement with the tip in the ipsilateral frontal horn of the lateral ventricle (grade 1). B : Functional placement into the contralateral lateral ventricle (grade 2). C : Suboptimal placement into the third ventricle through the caudate nucleus (grade 3).
In group 1, the number of catheter passages ranged from 1 to 4, and successful ventricular puncture with one catheter passage was achieved in 62% of the cases, whereas in group 2, the number of catheter passage ranged from 1 to 3, and successful procedure with one catheter passage was obtained in 80% of the cases.
Safety of ventriculostomy
In group 1, placement of the ventriculostomy catheter resulted in the development of tract ICH over 1 mL in 5 (5.0%) out of 101 procedures. The amount of hemorrhage ranged from 1.2 mL to 17 mL (mean±standard deviation : 5.1±6.8 mL). A tract ICH >15 mL occurred in one (1.0%) procedure.
In group 2, placement of the catheter resulted in the development of ICH in 11 (7.4%) of the 149 procedures. A tract ICH >15 mL occurred in 3 (2.0%) procedures. The amount of hemorrhage ranged from 1 mL to 30 mL (mean±standard deviation : 9.3±9.8 mL). The difference in the incidence of a tract ICH >1 mL between the two groups was not statistically significant (p=0.264).
DISCUSSION
Since the first report by Tillmanns21), introducing the technique of ventriculostomy with catheter placement at a point along the midpupillary line, 10 cm posterior to the nasion, few practical changes have been made to improve the accuracy of this technique, despite recent advances in neuro-imaging techniques. Several studies have investigated the accuracy of the freehand placement of a ventriculostomy catheter using Kocher's point. Kakarla et al.8) reported 77% optimal catheter placement in the ipsilateral frontal horn and the third ventricle, through the foramen of Monro, whereas Huyette et al.7) reported only 56% catheter placement in the ipsilateral lateral ventricle.
Thus, efforts to increase the accuracy of ventriculostomy at Kocher's point have included the Ghajar guide and image guidance. The Ghajar guide consists of a molded plastic tripod that is applied to the patient's scalp; the catheter is introduced through the central guide tube directed perpendicular to the tripod base, and providing a high rate of accuracy for catheter placement5,15). In a prospective study using the Ghajar guide at Kocher's point, 24 (96%) out of 25 patients received optimal catheter placement in the ipsilateral frontal horn15). Similarly, image guidance can also provide accurate catheter placement (95%), as in the prospective study by Krotz et al.11) However, in that study, the procedure was performed with the patient on the CT tray and required several adjustments, including a CT monitor that could be observed from the head side of the CT gantry, enough space on the head side for the operator, an operation lamp, and tables for instruments. Notwithstanding, according to a survey of ventriculostomy placement practices by O'Neill et al.16), most practitioners still use only the freehand pass method; only 3% of neurosurgical centers use the Ghajar guide on a regular basis and only 1% use image guidance. Furthermore, the effectiveness of the Ghajar guide is limited in patients with a midline brain shift or with distorted ventricular system.
The technique of forehead ventriculostomy was originally advocated by Kaufmann et al.10). In that case, the twist drill hole was located 5 cm superior to the nasion and 3 cm lateral to the midline, and the catheter was directed toward the midline point, 3 cm above the external occipital protuberance. However, cosmetic concerns have hindered the prevalence of this technique, resulting in relatively few published reports10,19). Yet, a small incision parallel to, or in the skin crease, a small twist drill hole in the skull, and careful approximation of the frontalis muscle, can minimize the cosmetic problems. Furthermore, as elucidated in the present study, forehead ventriculostomy has as a higher accuracy than the ventriculostomy using Kocher's point. This can be explained by procedural characteristics, such as its dependence on closer surface landmarks and the usage of pre-procedural axial CT scan as guidance image, providing the location for the twist drill hole, catheter trajectory, and depth of the catheter implantation.
Many patients with external ventricular drainage are required to undergo a permanent shunt placement, while approximately 10 to 30% of patients with aneurysmal subarachnoid hemorrhage undergo a ventriculoperitoneal shunt placement3,6,20,24). Thus, it is important to preserve potential shunt placement sites, such as the frontal (Kocher's point) and parieto-occipital regions12,13,17,21,22), and this is another advantage of forehead ventriculostomy.
To ensure maximum safety during ventriculostomy placement, the catheter should be implanted into the frontal horn through non-eloquent brain tissue. using a minimal number of passages14). In the study by Tominaga et al.23), magnetic resonance imaging was used to investigate the brain damage resulting from a ventricular puncture, and large ICHs (more than 3 cm in diameter) were seen in 4% of patients. However, the present study found a lower incidence of large ICHs >15 mL, with only 1% in group 1 and 2% in group 2, reflecting a high degree of procedural safety in both hospitals. Forehead ventriculostomy can enhance the accuracy of ventriculostomy and reduce the number of passages of the catheter through the frontal lobe. Thus, it can reduce the risk of frontal lobe damage, responsible for emotional and social behavior changes and decision-making impairment2,18).
While the success rate of VPS was not different between the two investigated groups, there was significant difference in the mean interval from EVD to VPS placement and in EVD-related infection rates. It is because the time of weaning from EVD was shorter in group 2, compared to group 1. In group 2, in all patients with weaning failure, it has been our practice to perform early weaning from EVD (at 4 or 5 days after EVD insertion) for early placement of a VPS, so infection and immobilization are minimized9). In our previous study regarding early shunt conversions, the mean interval from EVD to VPS placement was 6.4 days, with no ventriculitis or shunt-related infection, and a low revision rate (6.1%) during the follow-up period. Thus, that study showed that earlier weaning from EVD and conversion to VPS could effectively treat SAH-induced hydrocephalus and decrease EVD-related infection rates. Bota et al.1) reported EVD-related infection rates of 0 to 22% and identified many of the risk factors, including SAH, IVH, craniotomy, cranial fracture, systemic infection, and longer duration of EVD. Results showed that the EVD-related infection occurred after at least 3 days and the rate of infection increased linearly, between days 3 and 9, associated with longer stay in the intensive care unit.
This study has limitations, as it was a retrospective review from only two institutions. In addition, differences in the skill of individual neurosurgeons could have affected the results.
CONCLUSION
External ventricular drain placement is commonly performed with a freehand technique, using surface anatomical landmarks. Two different cranial sites, i.e., Kocher's point and the forehead, can provide accurate and safe ventriculostomy. In our study, the forehead ventriculostomy provided higher accuracy for the ventricular puncture.
References
- 1.Bota DP, Lefranc F, Vilallobos HR, Brimioulle S, Vincent JL. Ventriculostomy-related infections in critically ill patients : a 6 year experience. J Neurosurg. 2005;103:468–472. doi: 10.3171/jns.2005.103.3.0468. [DOI] [PubMed] [Google Scholar]
- 2.Clark L, Manes F, Antoun N, Sahakian BJ, Robbins TW. The contributions of lesion laterality and lesion volume to decision-making impairment following frontal lobe damage. Neuropsychologia. 2003;41:1474–1483. doi: 10.1016/s0028-3932(03)00081-2. [DOI] [PubMed] [Google Scholar]
- 3.Dorai Z, Hynan LS, Kopitnik TA, Samson D. Factors related to hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2003;52:763–769. doi: 10.1227/01.neu.0000053222.74852.2d. discussion 769-771. [DOI] [PubMed] [Google Scholar]
- 4.Friedman WA, Vries JK. Percutaneous tunnel ventriculostomy. Summary of 100 procedure. J Neurosurg. 1980;53:662–665. doi: 10.3171/jns.1980.53.5.0662. [DOI] [PubMed] [Google Scholar]
- 5.Ghajar JB. A guide for ventricular catheter placement. Technical note. J Neurosurg. 1985;63:985–986. doi: 10.3171/jns.1985.63.6.0985. [DOI] [PubMed] [Google Scholar]
- 6.Hirashima Y, Hamada H, Hayashi N, Kuwayama N, Origasa H, Endo S. Independent predictors of late hydrocephalus in patients with aneurysmal subarachnoid hemorrhage--analysis by multivariate logistic regression model. Cerebrovasc Dis. 2003;16:205–210. doi: 10.1159/000071117. [DOI] [PubMed] [Google Scholar]
- 7.Huyette DR, Turnbow BJ, Kaufman C, Vaslow DF, Whiting BB, Oh MY. Accuracy of the freehand pass technique for ventriculostomy catheter placement : retrospective assessment using computed tomography scans. J Neurosurg. 2008;108:88–91. doi: 10.3171/JNS/2008/108/01/0088. [DOI] [PubMed] [Google Scholar]
- 8.Kakarla UK, Kim LJ, Chang SW, Theodore N, Spetzler RF. Safety and accuracy of bedside external ventricular drain placement. Neurosurgery. 2008;63:ONS162–ONS166. doi: 10.1227/01.neu.0000335031.23521.d0. discussion ONS166-ONS167. [DOI] [PubMed] [Google Scholar]
- 9.Kang DH, Park J, Park SH, Kim YS, Hwang SK, Hamm IS. Early ventriculoperitoneal shunt placement after severe aneurysmal subarachnoid hemorrhage : role of intraventricular hemorrhage and shunt function. Neurosurgery. 2010;66:904–908. doi: 10.1227/01.NEU.0000368385.74625.96. discussion 908-909. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann GE, Clark K. Emergency frontal twist drill ventriculostomy. Technical note. J Neurosurg. 1970;33:226–227. doi: 10.3171/jns.1970.33.2.0226. [DOI] [PubMed] [Google Scholar]
- 11.Krötz M, Linsenmaier U, Kanz KG, Pfeifer KJ, Mutschler W, Reiser M. Evaluation of minimally invasive percutaneous CT-controlled ventriculostomy in patients with severe head trauma. Eur Radiol. 2004;14:227–233. doi: 10.1007/s00330-003-2134-y. [DOI] [PubMed] [Google Scholar]
- 12.Mapstone TB, Ratcheson RA. Techniques of ventricular puncture. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. New York: McGraw-Hill Co. Inc.; 1996. pp. 179–183. [Google Scholar]
- 13.McComb JG. Techniques for CSF diversion. In: Scott RM, editor. Hydrocephalus : Concepts in Neurosurgery. vol 3. Baltimore: Williams & Wilkins; 1990. pp. 47–65. [Google Scholar]
- 14.Moon HH, Kim JH, Kang HI, Moon BG, Lee SJ, Kim JS. Brain injuries during intraoperative ventriculostomy in the aneurysmal subarachnoid hemorrhage patients. J Korean Neurosurg Soc. 2009;46:215–220. doi: 10.3340/jkns.2009.46.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Leary ST, Kole MK, Hoover DA, Hysell SE, Thomas A, Shaffrey CI. Efficacy of the Ghajar Guide revisited : a prospective study. J Neurosurg. 2000;92:801–803. doi: 10.3171/jns.2000.92.5.0801. [DOI] [PubMed] [Google Scholar]
- 16.O'Neill BR, Velez DA, Braxton EE, Whiting D, Oh MY. A survey of ventriculostomy and intracranial pressure monitor placement practices. Surg Neurol. 2008;70:268–273. doi: 10.1016/j.surneu.2007.05.007. discussion 273. [DOI] [PubMed] [Google Scholar]
- 17.Roitberg BZ, Khan N, Alp MS, Hersonskey T, Charbel FT, Ausman JI. Bedside external ventricular drain placement for the treatment of acute hydrocephalus. Br J Neurosurg. 2001;15:324–327. doi: 10.1080/02688690120072478. [DOI] [PubMed] [Google Scholar]
- 18.Rolls ET, Hornak J, Wade D, McGrath J. Emotion-related learning in patients with social and emotional changes associated with frontal lobe damage. J Neurol Neurosurg Psychiatry. 1994;57:1518–1524. doi: 10.1136/jnnp.57.12.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saunders RL, Lyons TA. External ventricular drainage. A technical note. Crit Care Med. 1979;7:556–558. doi: 10.1097/00003246-197912000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Sethi H, Moore A, Dervin J, Clifton A, MacSweeney JE. Hydrocephalus : comparison of clipping and embolization in aneurysm treatment. J Neurosurg. 2000;92:991–994. doi: 10.3171/jns.2000.92.6.0991. [DOI] [PubMed] [Google Scholar]
- 21.Tillmanns H. Something about puncture of the brain. Br Med J. 1908;2:983–984. [Google Scholar]
- 22.Timothy J, Hall G, Chumas P. Minimalist placement of external ventricular drains. A quick, safe, cheap and cosmetic procedure. Br J Neurosurg. 2000;14:339–340. doi: 10.1080/026886900417333. [DOI] [PubMed] [Google Scholar]
- 23.Tominaga J, Shimoda M, Oda S, Kumasaka A, Yamazaki K, Tsugane R. MRimaging findings after ventricular puncture in patients with SAH. Acta Neurochir (Wien) 2001;143:1133–1140. doi: 10.1007/s007010100004. [DOI] [PubMed] [Google Scholar]
- 24.Vale FL, Bradley EL, Fisher WS., 3rd The relationship of subarachnoid hemorrhage and the need for postoperative shunting. J Neurosurg. 1997;86:462–466. doi: 10.3171/jns.1997.86.3.0462. [DOI] [PubMed] [Google Scholar]
- 25.van Gijn J, Hijdra A, Wijdicks EF, Vermeulen M, van Crevel H. Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. J Neurosurg. 1985;63:355–362. doi: 10.3171/jns.1985.63.3.0355. [DOI] [PubMed] [Google Scholar]