Abstract
Idiopathic hypertrophic spinal pachymeningitis (IHSP) is a rare inflammatory disease characterized by hypertrophic inflammation of the dura mater and various clinical courses that are from myelopathy. Although many associated diseases have been suggested, the etiology of IHSP is not well understood. The ideal treatment is controversial. In the first case, a 55-year-old woman presented back pain, progressive paraparesis, both leg numbness, and voiding difficulty. Initial magnetic resonance imaging (MRI) demonstrated an anterior epidural mass lesion involving from C6 to mid-thoracic spine area with low signal intensity on T1 and T2 weighted images. We performed decompressive laminectomy and lesional biopsy. After operation, she was subsequently treated with steroid and could walk unaided. In the second case, a 45-year-old woman presented with fever and quadriplegia after a spine fusion operation due to lumbar spinal stenosis and degenerative herniated lumbar disc. Initial MRI showed anterior and posterior epidural mass lesion from foramen magnum to C4 level. She underwent decompressive laminectomy and durotomy followed by steroid therapy. However, her conditions deteriorated gradually and medical complications occurred. In our cases, etiology was not found despite through investigations. Initial MRI showed dural thickening with mixed signal intensity on T1- and T2-weighted images. Pathologic examination revealed chronic nonspecific inflammation in both patients. Although one patient developed several complications, the other showed slow improvement of neurological symptoms with decompressive surgery and steroid therapy. In case of chronic compressive myelopathy due to the dural hypertrophic change, decompressive surgery such as laminectomy or laminoplasty may be helpful as well as postoperative steroid therapy.
Keywords: Idiopathic hypertrophic spinal pachymeningitis, Spinal cord compression, Chronic nonspecific inflammation, Dural thickening
INTRODUCTION
Idiopathic hypertrophic spinal pachymeningitis (IHSP) is a comparatively rare disorder characterized by marked inflammatory hypertrophy of the dura mater, with subsequent neurological deficits resulting from the compression of adjacent structures3). We present two cases of IHSP with description of etiologies, diagnoses, managements and clinical outcomes.
CASE REPORT
Case 1
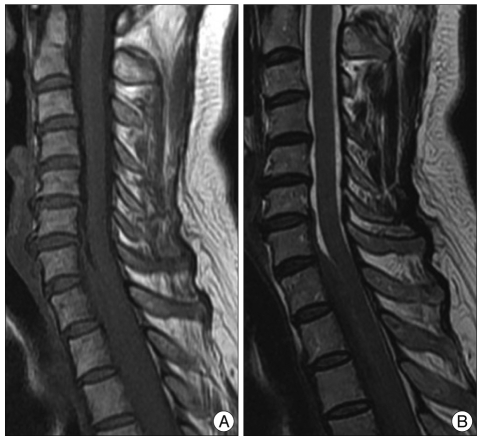
A 55-year-old woman visited to our hospital complaining of back pain, progressive paraparesis, both leg numbness, and voiding difficulty in July, 2009. These symptoms had been started 7 months ago and worsened gradually. Her family and past histories were noncontributory. There was no trauma history. On physical examination, motor and sensory function were intact. Her deep tendon reflexes and ankle clonus were checked as normal. There was no documented fever or leukocytosis [White blood cell (WBC) count 6,280/uL]. However, erythrocyte sedimentation rate (ESR) was elevated to 47 mm/hr (normal : 0-20 mm/hr), and C-reactive protein (CRP) level also was elevated to 37.9 mg/L (normal : 0.1-6.0 mg/L). Other laboratory data were within normal ranges and various culture studies revealed no growth. Initial magnetic resonance imaging (MRI) showed an epidural lesion involving from C6 vertebral body level to mid-thoracic spine area with low signal intensity on T1 (Fig. 1A) and T2 (Fig. 1B) weighted images.
Fig. 1.
Sagittal T1 (A)- and T2 (B)- weighted MRI taken in mid-July 2009, showing an epidural lesion with low signal intensity from C6 to mid-thoracic spine area.
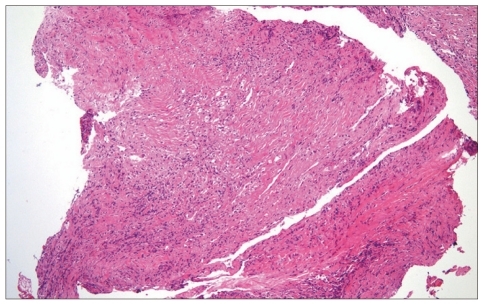
The patient was treated initially with dexamethasone 5 mg every 6 hours for 7 days, but she had no improvement. Seven days later, follow-up MRI with gadolinium enhancement revealed diffuse homogeneous enhancement (Fig. 2) which was suspected as acute or early subacute stage of epidural hematoma, surgical exploration was done. Total laminectomies of T6 and T7, lesional biopsies were performed immediately. No extradural abnormality was visible during the operation. After opening dura mater, we found yellowish tumor-like lesion and resected partially for biopsy. Pathologic examination revealed a chronic nonspecific inflammation and fibrosis (Fig. 3). Staining for cytokeratin was negative. These findings were compatible with diagnosis of idiopathic hypertrophic spinal pachymeningitis. The patient was treated with dexamethasone postoperatively for 6 days, and symptoms were gradually improved and laboratory data including ESR, CRP turned to be normal. Two months later after the surgery, follow-up MRI showed decreased dural thickening from C7 to T8 (Fig. 4B). The patient had undergone oral prednisolone and kept improved state for 4 months.
Fig. 2.
Sagittal (A) and axial (B) gadolinium-enhanced T1-weighted MRI taken around the end of July 2009, demonstrating diffusely homogeneous enhancement.
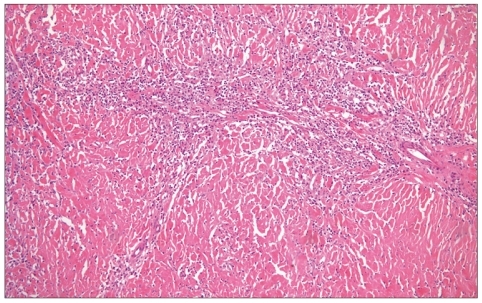
Fig. 3.
Photomicrograph of a section of the excised dura mater, consisting of thick fibrous collagenous tissue mixed with many chronic inflammatory cells (hematoxylin and eosin, original magnification 100×).
Fig. 4.
Sagittal gadolinium enhanced T1-weighted MRI taken in August 2009 (B) after the surgery and the steroid therapy have demonstrated decrease of epidural mass compared with initial MRI (A).
However, 4 months later, the patient was admitted to our hospital again presenting with back pain, both leg numbness, and gait disturbance as much as caine-assisted gait. MRI revealed increase of diffusely thickened dura comparing to the previous MRI. ESR (30 mm/hr) and CRP (7.7 mg/L) levels were mildly elevated. She was treated with steroid (solumedrol) pulse therapy and followed by maintenance treatment with oral prednisolone as well as rehabilitation. One month later, MRI revealed decrease of dural thickening. The patient recovered almost completely from the neurologic symptoms slowly and could walk unaided eventually.
Case 2
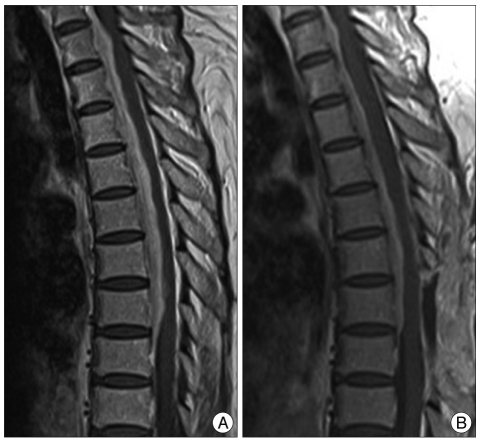
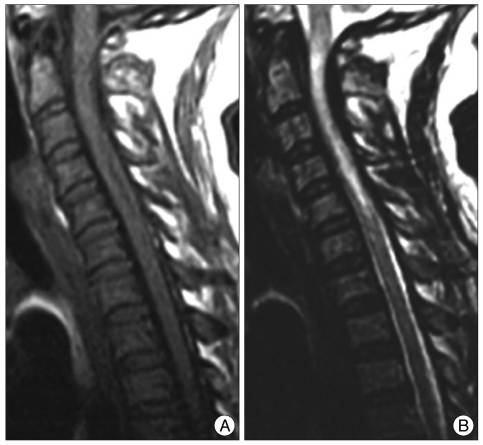
A 45-year-old woman presented with fever and quadriplegia in November 2000. One day before, she had a spinal fusion operation due to lumbar spinal stenosis and degenerative disc herniation in another hospital. Because she awoke slowly from the general anesthesia and, showed quadriplegia and respiratory difficulty immediate postoperatively, she was transferred to our hospital. At the time of admission, she had mild fever (37.9℃) and mild leukocytosis (WBC count 9,890/uL). Her ESR and CRP were also slightly elevated. However, ordinary blood culture was negative. Initial MRI showed an extramedullary mass compressing the upper cervical spinal cord posteriorly from foramen magnum to C4 level (Fig. 5). On suspicion of epidural hematoma, emergent decompressive laminectomy from C1 to C4 was performed. There was no definite epidural and subdural hematoma, but 8 mm-thickened dura were noted. Through dural excision, we achieved the decompression of spinal cord. Subsequently, we took multiple biopsy specimens from the dura. Postoperatively the patient was treated with dexamethasone for 2 weeks. In spite of the surgery, neurological symptoms including weakness showed no improvement. Pathologic examination (Fig. 6) showed acute and chronic nonspecific inflammation with dense, collagenous fibrosis. The patient then suffered from hydrocephalus, pneumonia, and central nervous system infection. Ultimately her weakness did not improve.
Fig. 5.
MRI taken in November 2000, showing epidural mass compressing the cervical spinal cord from the foramen magnum to C4 vertebral level. Sagittal T1 (A)-, T2 (B)-weighted MRI showed low signal intensity.
Fig. 6.
Photomicrograph of the surgical specimen showing acute and chronic nonspecific inflammation with dense collagenous fibrosis (hematoxylin and eosin, original magnification 100×).
DISCUSSION
Idiopathic hypertrophic pachymeningitis (IHP) is a comparatively rare inflammatory disease characterized by hypertrophic inflammation of the dura mater4). This rare disease is mostly found intracranially4). The spinal form of IHP is rarer and first described by Charcot and Joffroy with its first name as "Pachymeningitis hypertrophica cervicalis" in 18691,7,8,10-12). Charcot and Joffroy described three stages; in the first stage, patients experience local and radicular pain. The second stage can present signs of nerve root compression. In addition, in the third stage, patients eventually suffer from spinal cord compression5-7,14). Our patients have experienced all stages.
The etiology of hypertrophic spinal pachymeningitis (HSP) is still unknown in most cases, although various associated diseases have been recognized, including trauma, metabolic disease, sarcoidosis, infections such as syphilis, tuberculosis, HTLV-1, meningococcal meningitis, granulomatous sinusitis, mastoid sinusitis and fungal infection2,3,5,10,11,13,14). Also, HSP has been associated with various autoimmune disease including Wegener's granulomatosis, rheumatoid arthritis, orbital pseudotumor, multifocal fibrosclerosis and mixed connective tissue disease2,3,8). Intrathecal steroids, spinal anesthesia, and contrast medium for myelography also have been implicated as a cause of HSP10,11,14). A lot of cases have unknown etiology and are classified as IHSP3). In our cases, we could not find any predisposing illnesses such as infectious diseases or autoimmune diseases in spite of the through investigations.
On MRI, IHSP has been showed as dura-based mass of low signal intensity on T1- and T2-weighted images extending over multiple vertebral levels3,12). In addition, predominantly peripheral enhancement pattern is a highly suggestive of IHSP3,12). This pattern represents more intense enhancement in a peripheral zone of active inflammation than in a central zone of fibrosis3,4,12). Linear dural enhancement pattern was known to have better response to steroid therapy than those with nodular pattern because of its less fibrosis and more vascularity1,3,8,10,12,13). The typical pathologic features are a thickening of the dura, with nonnecrotizing chronic inflammatory infiltrate of lymphocytes, plasma cell, and, occasionally with histiocytes, giant cells, polymorphonuclear cells or eosinophils2,3,5,9,14). In our cases, typical radiologic and pathologic features observed in the literature can be shown.
The management of IHSP is controversial. For IHSP, surgical decompression by laminectomy and excision or incision of the involved dura has been recommended2,3,5,11,13,14). Recently, some case reports witnessed that biopsy with steroid therapy can decrease the thickness of the dura by serial MRI and can improve neurologic deficit3,9). If decompressive surgery is necessary, laminoplasty have been recommended instead of extensive laminectomy because the former could reduce chronic back discomfort and would enhance spinal stability3,11). Others have emphasized postoperative radiotherapy, immunosuppressive therapy such as azathioprine, and cyclophosphamide2,3,12,14). Among our two patients, one recovered from the weakness, the other did not recover from the quadriplegia status. The authors thought that the cause of the latter was acute spinal cord injury maybe from neck extension during induction of anesthesia, meanwhile, the former from chronic myelopathy.
CONCLUSION
Although IHSP is a rare disorder, the clinical and radiological findings are characteristic. Unaccountable motor weakness and gadolinium-enhancing thickened dura which can be shown by spinal MRI probably lead to a diagnosis. For the management of IHSP, we advocate surgical decompression with subsequent prolonged steroid therapy as our cases had.
References
- 1.Botella C, Orozco M, Navarro J, Riesgo P. Idiopathic chronic hypertrophic craniocervical pachymeningitis : case report. Neurosurgery. 1994;35:1144–1149. doi: 10.1227/00006123-199412000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Bucy PC, Freeman LW. Hypertrophic spinal pachymeningitis with special reference to appropriate surgical treatment. J Neurosurg. 1952;9:564–578. doi: 10.3171/jns.1952.9.6.0564. [DOI] [PubMed] [Google Scholar]
- 3.Dumont AS, Clark AW, Sevick RJ, Myles ST. Idiopathic hypertrophic pachymeningitis : a report of two patients and review of the literature. Can J Neurol Sci. 2000;27:333–340. doi: 10.1017/s0317167100001116. [DOI] [PubMed] [Google Scholar]
- 4.Friedman D, Flanders A, Tartaglino L. Contrast-enhanced MR imaging of idiopathic hypertrophic craniospinal pachymeningitis. AJR Am J Roentgenol. 1993;160:900–901. doi: 10.2214/ajr.160.4.8456697. [DOI] [PubMed] [Google Scholar]
- 5.Guidetti B, La Torre E. Hypertrophic spinal pachymeningitis. J Neurosurg. 1967;26:496–503. doi: 10.3171/jns.1967.26.5.0496. [DOI] [PubMed] [Google Scholar]
- 6.Ito Z, Osawa Y, Matsuyama Y, Aoki T, Harada A, Ishiguro N. Recurrence of hypertrophic spinal pachymeningitis. Report of two cases and review of the literature. J Neurosurg Spine. 2006;4:509–513. doi: 10.3171/spi.2006.4.6.509. [DOI] [PubMed] [Google Scholar]
- 7.Joffroy A. Deux cas d'atrophie musculaire progressive avec lesions de la substance grise et des faisceaux anterolateraux de la moelle epiniere. Arch Physiol Norm Path. 1869;2:354–367. [Google Scholar]
- 8.Kanamori M, Matsui H, Terahata N, Tsuji H. Hypertrophic spinal pachymeningitis. A case report. Spine. 1997;22:1787–1790. doi: 10.1097/00007632-199708010-00021. [DOI] [PubMed] [Google Scholar]
- 9.Kitai R, Sato K, Kubota T, Kabuto M, Uno H, Kobayashi H. Hypertrophic cranial pachymeningitis involving the pituitary gland : a case report. Surg Neurol. 1997;48:58–62. doi: 10.1016/s0090-3019(96)00433-8. discussion 62-63. [DOI] [PubMed] [Google Scholar]
- 10.Mikawa Y, Watanabe R, Hino Y, Hirano K. Hypertrophic spinal pachymeningitis. Spine. 1994;19:620–625. doi: 10.1097/00007632-199403000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Naffziger HC, Stern WE. Chronic pachymeningitis; report of a case and review of the literature. Arch Neurol Psychiatry. 1949;62:383–411. [PubMed] [Google Scholar]
- 12.Pai S, Welsh CT, Patel S, Rumboldt Z. Idiopathic hypertrophic spinal pachymeningitis : report of two cases with typical mr imaging findings. AJNR Am J Neuroradiol. 2007;28:590–592. [PMC free article] [PubMed] [Google Scholar]
- 13.Park SH, Whang CJ, Sohn M, Oh YC, Lee CH, Whang YJ. Idiopathic hypertrophic spinal pachymeningitis : a case report. J Korean Med Sci. 2001;16:683–688. doi: 10.3346/jkms.2001.16.5.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenfeld JV, Kaye AH, Davis S, Gonzales M. Pachymeningitis cervicalis hypertrophica. Case report. J Neurosurg. 1987;66:137–139. doi: 10.3171/jns.1987.66.1.0137. [DOI] [PubMed] [Google Scholar]