Abstract
Nocardia brain abscess is rare. We report on a unique case of N. farcinica brain abscess in a liver transplant recipient, following Aspergillus fumigatus pneumonia. A 43-year-old liver transplant recipient presented with altered mentality at 2 months after A. fumigates pneumonia. He was successfully treated with surgical removal and antibiotic therapy with trimethoprim-sulfamethoxazole and ceftriaxone.
Keywords: Brain abscess, Liver transplant, Nocardia
INTRODUCTION
Brain abscesses after organ transplantation are rare, however, they are known to result in the high mortality and morbidity20). In a review, the incidence of brain abscess is 0.6% among the liver transplant recipients, and patients with brain abscess shows a mortality rate of 20% and high morbidity, including seizures (up to 80%), altered mentality, and focal neurological deficits2,25). Fungi are the predominant organisms in the immunocompromised host and usually arise by hematogenous dissemination from the lung16). Aspergillus species are the most common respiratory pathogens, 10% of which disseminates to the brain7,18-20).
Nocardia species, as a nonfungal organism, are the rare cause of brain abscess and N. farcinica brain abscess is much rare. Only a single case has been reported in Korea21). Here, we report on a case of N. farcinica brain abscess in a liver transplant recipient, following Aspergillus fumigatus pneumonia.
CASE REPORT
A 43-year-old man was admitted for the evaluation and treatment of sudden altered mentality in June 2008. He had been diagnosed as hepatitis B virus-related liver cirrhosis 12 years before and had undergone liver transplantation from a living donor in September 2007. After the surgery, he has been taking immunosuppressive (tacrolimus and prednisolone) and antiviral agents (adefovir and lamivudine). Post-transplantation clinical course has been uneventful until April 2008, with neither transplant rejection nor serious infectious diseases. Two months prior to the admission, he was diagnosed as Aspergillus fumigatus pneumonia, and was prescribed amphotericin B for 3 weeks, resulting in complete recovery.
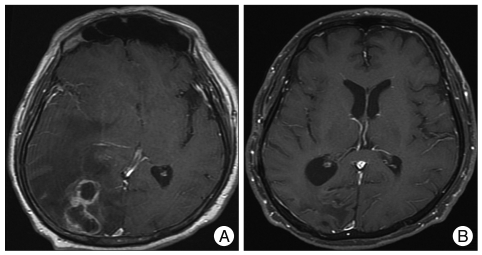
He suffered from headache and blurred vision a month ago and rigidity of the legs which made him unable to walk a week ago. His mentality became drowsy a day ago. At admission, he was semicomatose and hemiparetic on the left side. Brain computed tomographic scan and magnetic resonance (MR) imaging demonstrated a 4×4-cm multiloculated rim-enhancing lesion with massive perilesional edema which was presumed to be a brain abscess (Fig. 1).
Fig. 1.
A : Brain magnetic resonance (MR) imaging. A multiloculated rim-enhancing lesion with perilesional edema is observed in the right occipital lobe with a significant mass effect. B : Follow-up MR imaging. There is no residual enhancing lesion and no edema in the right occipital lobe at 2 months after operation.
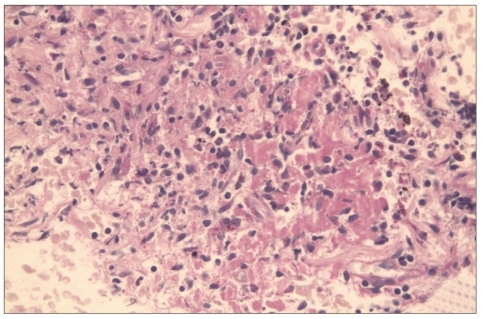
To achieve etiologic diagnosis and reduction of mass effect, craniotomy and removal of the lesion was performed. During the operation, non-odorous and creamy pus was drained from two cavities. The lesion could be easily dissected from the surrounding brain and was completely removed. After surgery, the patient became alert but right homonymous hemianopsia and left side weakness (Grade II/V) persisted. On the pathologic examination, the lesion was found to be organizing abscess with necrosis and fibrosis (Fig. 2). The microbiological studies revealed that the etiologic agent was Nocardia farcinica.
Fig. 2.
Pathologic examination of brain tissue. There is chronic active inflammation with reactive gliosis (H&E staining, ×400).
He was treated with intravenous trimethoprim-sulfamethoxazole (TMP/SMX) 1,920 mg every 8 hour (15 mg/kg/day) and ceftriaxone 2 gm every 12 hour for t2 weeks and then with intravenous TMP/SMX for additional 3 weeks. During the antibiotic treatment, he also received immunosuppressive and antiviral therapies although prednisolone was reduced from 30 mg to 5 mg. During the second week of the treatment, he developed progressive thrombocytopenia probably caused by TMP/SMX. Instead of withdrawing the drug, platelet concentrates were transfused, and his platelet count was maintained in the range of 50,000/uL to 100,000/uL. He also developed hyperkalemia (6.0 mmol/L) which thought to be due to TMP/SMX medication. It was controlled with oral kalimate administration.
After 6 weeks of rehabilitation, he was discharged home in a state of walker ambulation. The follow-up MR images 2 months after operation demonstrated no residual brain abscess. The antibiotic treatment with TMP/SMX was continued up to 12 months after operation. The patient achieved good recovery in 15 months after operation.
DISCUSSION
Nocardia species are soil-borne aerobic actinomycetes, and most of human infections have been caused by Nocardia asteroids and brasiliensis13). Nocardia brain abscesses account for about 1% to 2% of all brain abscesses, and most of them occur as a primary lesion with no evidence of extracranial lesions16). Overall, the mortality associated with brain abscesses is estimated to be 10%9,18), however, cerebral nocardiosis shows the fatality rate of 30%17). Half of the affected patients are immunocompromised.
To our knowledge, cases of brain abscess caused by N. farcinica have been reported less than 20 in number3-5,8,10,22-24). This is the second case report of N. farcinica brain abscess in Korea. It is unique in that the brain abscess was preceded by Aspergillus fumigatus pneumonia with a 2-month interval. Diagnosis of nocardial respiratory infection is difficult because of the slow growth of the bacteria and the presence of normal flora in the culture1). If the patient had not undergone operation for the brain lesion, he might have been treated with an antifungal agent, such as amphotericin B, which was used for treatment of the previous pneumonia. We confirmed that the etiologic organism was N. farcinica by the microbiological study. After successful surgical removal of the lesion and the etiologic diagnosis, we could start an appropriate antimicrobial therapy, including TMP/SMX, which led to a satisfactory outcome in the present case.
Due to the good tolerance and excellent penetration into the cerebrospinal fluid space, TMP/SMX is the preferred initial treatment option for N. farcinica brain abscesses. Amikacin, carbapenem, sulfonamide, minocycline, ciprofloxacin, or a third-generation cephalosporin are also reported to be effective14,16,17). In this case, the platelet count number was decreased to 50,000/uL during the antimicrobial therapy. The sulfamethoxazole component of TMP/SMX is known to be one of the most common causes of isolated leukopenia or thrombocytopenia11). However, majority of them have safely continued to receive TMP/SMX with resolution of the adverse reactions, either spontaneously or with a supportive care with drugs, such as anti-histamine, anti-pyretic, or corticosteroid therapy6). Our patient responded well to corticosteroid therapy and platelet transfusion. Antimicrobial therapy is often continued for many months after apparent cure because of high relapse rate. If the brain is involved or the patient is immunosuppressed, the treatment should be continued for 12 months12,15).
CONCLUSION
In immunocompromised patients who present with a brain abscess, it is important to know that various organisms, including N. farcinica, can cause the lesion, irrespective of the previous infections. In this case, we confirmed the etiologic agents, and achieved a good outcome through surgical removal of the mass lesion and adequate antibiotic treatment.
References
- 1.Barnaud G, Deschamps C, Manceron V, Mortier E, Laurent F, Bert F, et al. Brain abscess caused by Nocardia cyriacigeorgica in a patient with human immunodeficiency virus infection. J Clin Microbiol. 2005;43:4895–4897. doi: 10.1128/JCM.43.9.4895-4897.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carpenter J, Stapleton S, Holliman R. Retrospective analysis of 49 cases of brain abscess and review of the literature. Eur J Clin Microbiol Infect Dis. 2007;26:1–11. doi: 10.1007/s10096-006-0236-6. [DOI] [PubMed] [Google Scholar]
- 3.Chung TT, Lin JC, Hsieh CT, Chen GJ, Ju DT. Nocardia farcinica brain abscess in an immunocompetent patient treated with antibiotics and two surgical techniques. J Clin Neurosci. 2009;16:1675–1677. doi: 10.1016/j.jocn.2009.03.029. [DOI] [PubMed] [Google Scholar]
- 4.Fellows GA, Kalsi PS, Martin AJ. Nocardia farcinica brain abscess in a patient without immunocompromise. Br J Neurosurg. 2007;21:301–303. doi: 10.1080/02688690701365770. [DOI] [PubMed] [Google Scholar]
- 5.Fihman V, Berçot B, Mateo J, Losser MR, Raskine L, Riahi J, et al. First successful treatment of Nocardia farcinica brain abscess with moxifloxacin. J Infect. 2006;52:e99–e102. doi: 10.1016/j.jinf.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Gleckman R, Altschullter C. Trimethoprim-sulphamethoxazole. In: Gorbach SL, Barlett JG, Blacklow NR, editors. Infectious Disease. Philadelphia: Lippincott Williams and Wilkins; 2004. p. 247. [Google Scholar]
- 7.Hur JH, Kwon AH, Gwak HS, Rhee CH. Postoperative brain abscess caused by co-infection of aspergillus and staphylococcus : case report. J Korean Neurosurg Soc. 2003;33:81–84. [Google Scholar]
- 8.Iannotti CA, Hall GS, Procop GW, Tuohy MJ, Staugaitis SM, Weil RJ. Solitary Nocardia farcinica brain abscess in an immunocompetent adult mimicking metastatic brain tumor : rapid diagnosis by pyrosequencing and successful treatment. Surg Neurol. 2009;72:74–79. doi: 10.1016/j.surneu.2008.02.025. discussion 79. [DOI] [PubMed] [Google Scholar]
- 9.Jansson AK, Enblad P, Sjölin J. Efficacy and safety of cefotaxime in combination with metronidazole for empirical treatment of brain abscess in clinical practice : a retrospective study of 66 consecutive cases. Eur J Clin Microbiol Infect Dis. 2004;23:7–14. doi: 10.1007/s10096-003-1055-7. [DOI] [PubMed] [Google Scholar]
- 10.Kandasamy J, Iqbal HJ, Cooke RP, Eldridge PR. Primary Nocardia farcinica brain abscess with secondary meningitis and ventriculitis in an immunocompetent patient, successfully treated with moxifloxacin. Acta Neurochir (Wien) 2008;150:505–506. doi: 10.1007/s00701-008-1578-x. [DOI] [PubMed] [Google Scholar]
- 11.Katzung BG, Trevor AJ. Sulfonamids, trimethoprim, and fluoroquinolones. In: Katzung BG, Trevor AJ, editors. Examination and board review pharmacology. Norwalk: Appleton and Lange; 1998. pp. 338–341. [Google Scholar]
- 12.Kramer MR, Uttamchandani RB. The radiographic appearance of pulmonary nocardiosis associated with AIDS. Chest. 1990;98:382–385. doi: 10.1378/chest.98.2.382. [DOI] [PubMed] [Google Scholar]
- 13.Lai CC, Lee LN, Teng LJ, Wu MS, Tsai JC, Hsueh PR. Disseminated Nocardia farcinica infection in a uraemia patient with idiopathic thrombocytopenia purpura receiving steroid therapy. J Med Microbiol. 2005;54:1107–1110. doi: 10.1099/jmm.0.46084-0. [DOI] [PubMed] [Google Scholar]
- 14.Lee GY, Daniel RT, Brophy BP, Reilly PL. Surgical treatment of nocardial brain abscesses. Neurosurgery. 2002;51:668–671. discussion 671-672. [PubMed] [Google Scholar]
- 15.Lerner PI. Nocardiosis. Clin Infect Dis. 1996;22:891–903. doi: 10.1093/clinids/22.6.891. quiz 904-905. [DOI] [PubMed] [Google Scholar]
- 16.Malincarne L, Marroni M, Farina C, Camanni G, Valente M, Belfiori B, et al. Primary brain abscess with Nocardia farcinica in an immunocompetent patient. Clin Neurol Neurosurg. 2002;104:132–135. doi: 10.1016/s0303-8467(01)00201-3. [DOI] [PubMed] [Google Scholar]
- 17.Mamelak AN, Obana WG, Flaherty JF, Rosenblum ML. Nocardial brain abscess : treatment strategies and factors influencing outcome. Neurosurgery. 1994;35:622–631. doi: 10.1227/00006123-199410000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Mathisen GE, Johnson JP. Brain abscess. Clin Infect Dis. 1997;25:763–779. doi: 10.1086/515541. [DOI] [PubMed] [Google Scholar]
- 19.Patchell RA. Neurological complications of organ transplantation. Ann Neurol. 1994;36:688–703. doi: 10.1002/ana.410360503. [DOI] [PubMed] [Google Scholar]
- 20.Selby R, Ramirez CB, Singh R, Kleopoulos I, Kusne S, Starzl TE, et al. Brain abscess in solid organ transplantation recipients receiving cyclosporine-based immunosuppression. Arch Surg. 1997;132:304–310. doi: 10.1001/archsurg.1997.01430270090019. quiz 780-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sim SH, Park HC, Kim CJ, Jeon JH, Kim EC, Oh MD, et al. A case of Nocardia farcinica brain abscess in the patient receiving steroid treatment. Infect Chemother. 2008;40:301–304. [Google Scholar]
- 22.Sonesson A, Oqvist B, Hagstam P, Björkman-Burtscher IM, Miörner H, Petersson AC. An immunosuppressed patient with systemic vasculitis suffering from cerebral abscesses due to Nocardia farcinica identified by 16S rRNA gene universal PCR. Nephrol Dial Transplant. 2004;19:2896–2900. doi: 10.1093/ndt/gfh412. [DOI] [PubMed] [Google Scholar]
- 23.Tatti KM, Shieh WJ, Phillips S, Augenbraun M, Rao C, Zaki SR. Molecular diagnosis of Nocardia farcinica from a cerebral abscess. Hum Pathol. 2006;37:1117–1121. doi: 10.1016/j.humpath.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 24.Viganò SM, Edefonti A, Ferraresso M, Ranzi ML, Grossi P, Righini A, et al. Successful medical treatment of multiple brain abscesses due to Nocardia farcinica in a paediatric renal transplant recipient. Pediatr Nephrol. 2005;20:1186–1188. doi: 10.1007/s00467-005-1978-6. [DOI] [PubMed] [Google Scholar]
- 25.Yang SY. Brain abscess : a review of 400 cases. J Neurosurg. 1981;55:794–799. doi: 10.3171/jns.1981.55.5.0794. [DOI] [PubMed] [Google Scholar]