Abstract
Most hamartomatous polyps in the stomach occur in patients with adenomatous polyposis coli and dysplasia. The authors report a case of a 57-year-old man without prior history of polyposis coli who presented with adenocarcinomas derived from hamartomatous polyps in the stomach. The patient underwent a radical subtotal gastrectomy with Billroth I anastomosis. Pathology revealed adenocarcinomas with moderate differentiation without evidence of lymph node metastasis in 60 nodes. We report a case of gastric cancers arising from de novo gastric hamartomatous polyps.
Keywords: Hamartoma, Stomach neoplasms, Gastrectomy
INTRODUCTION
Hamartomatous polyps are uncommon and usually found as a part of Peutz-Jegher syndrome, a rare autosomal dominant disorder associated with mucocutaneous pigmentation and family history [1]. Hamartomatous polyps are composed not only of epithelial elements, but also of bundles of smooth muscle cells. The essential feature of these polyps is the proliferation of muscularis mucosa. Such hamartomatous gastric polyps are almost always found in patients with Peutz-Jeghers syndrome, in association with intestinal polyps. In hamartomatous polyps, there is an increased risk of malignancy in both the gastrointestinal and extra-intestinal sites [2-4]. The risk increases with age (range, 1 to 33%) between 30 and 60 years [5].
CASE REPORT
Fifty seven years-old man with a history of epigastric pain was transferred from an outside hospital with the diagnosis of early gastric cancer. Physical examination and laboratory investigations were unremarkable. No pigmentation was found on the lips and perioral region, hands, buccal mucosa, and feet. Colonoscopy showed 6 tubular adenomas in the colon and rectum. Preoperative evaluation did not demonstrate evidence of an alternative primary malignant lesion. Endoscopy revealed two masses on the greater curvature side of the prepyloricantrum: a round, 1 cm polypoid lesion and an irregular 3 cm elevated mass with superficial ulcerations (Fig. 1A) and another 6 cm pedunculated polypoid mass on the greater curvature side of prepyloricantrum (Fig. 1B). Histology of the biopsy specimens revealed typical tubular adenocarcinoma. Upper gastrointestinal series showed three polypoid lesions in the gastric antrum which was considered as an advanced, Borrmann type I carcinoma preoperatively (Fig. 2A, B). Subsequently, the patient underwent a radical subtotal gastrectomy, which revealed a 6 × 5 cm mass confined to the mucosa of the greater curvature of the lower body and another 5.5 × 2 cm mass invading into the submucosa of the greater curvature of the antrum (Fig. 3). Under endoscopy, the 5.5 × 2 cm sized mass looked like two masses, but was a fused mass intraoperatively. There was no lymph node metastasis in 60 nodes. Microscopic analysis of the specimen revealed adenocarcinoma within the hamartomatous polyps demonstrated by proliferation of smooth muscle bundles within the lamina propria and between carcinomatous glands (Fig. 4A) with evidence of Epstein-Barr virus (EBV) in both lesions (Fig. 4B). The patient had an uneventful postoperative course and was discharged home on the 9th postoperative day.
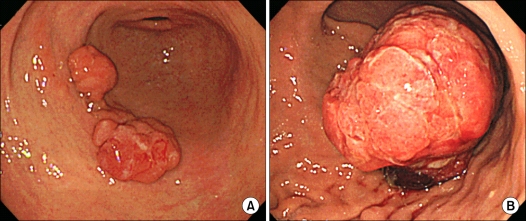
Fig. 1.
(A) Esophagogastroduodenoscopy showed three lesions. On greater curvature side of antrum, 1 cm and 3 cm sized lesions. (B) 6 cm sized pedunculated polypoid masson greater curvature side of antrum.
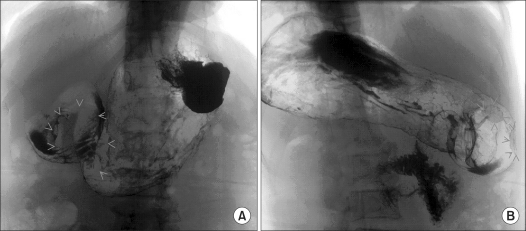
Fig. 2.
(A) Upper gastrointestinal series showed 6 cm sized, large polypoid mass and (B) Another two 2.5 cm sized polypoid masses in antrum.
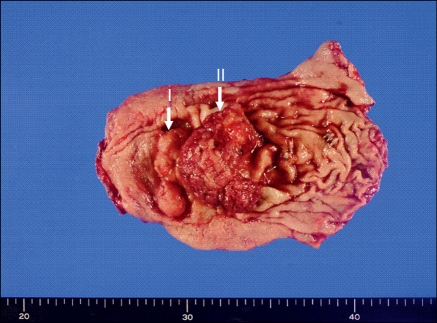
Fig. 3.
The specimen showed two lesions. On the lower body and lesser curvature, 6 × 5 cm sized pedunculated polypoid lesion (I) and on the antrum and greater curvature, a 5.5 × 2 cm sized irregular shaped elevated mass (II).
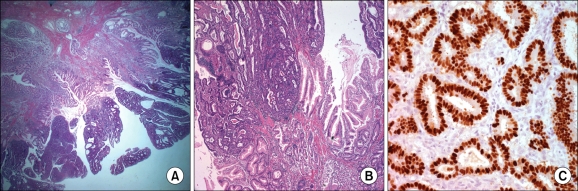
Fig. 4.
(A) There was ramifying proliferation of smooth muscle bundles within lamina propria, suggesting hamartomatous polyp (H&E, ×10). (B) Higher magnification showing adenocarcinoma, proliferation of smooth muscle bundles and foveolar epithelium. (H&E, ×50). (C) Epstein-Barr virus (EBV)-encoded RNA in situ hybridization of gastric carcinoma (EBV in situ hybridization, ×400).
DISCUSSION
Hamartomatous polyps are considered benign lesions with no malignant potential [6]. Tatsuta et al. [7] reported four cases of patients with multiple benign gastric hamartomatous polyps that were not associated with polyposis coli. However, syndrome-associated hamartomatous polyps may have malignant potential as cases of malignant hamartoma have been described [8-10]. From our review of the English-language literature, this case report appears to be the first documented case of adenocarcinoma derived from gastric hamartomatous polyps which was not accompanied by a known syndrome. We present a case report of a patient with malignant gastric hamartomatous polyps in the absence of familial polyposis nor pigmentation.
Furthermore, this case exhibited positive expression via in EBV-encoded RNA (EBER) in situ hybridization. To date, there is no report about incidence of adenocarcinoma in hamartomatous polyps in EBER-positive in situ hybridization. Additional studies are needed to validate the findings.
ACKNOWLEDGEMENTS
The authors thank Jenny J. Hong, M.D., M.P.H. for her contribution and drafting of the manuscript.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Jeghers H, McKusick VA, Katz KH. Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits; a syndrome of diagnostic significance. N Engl J Med. 1949;241:993. doi: 10.1056/NEJM194912222412501. illust; passim. [DOI] [PubMed] [Google Scholar]
- 2.Giardiello FM, Welsh SB, Hamilton SR, Offerhaus GJ, Gittelsohn AM, Booker SV, et al. Increased risk of cancer in the Peutz-Jeghers syndrome. N Engl J Med. 1987;316:1511–1514. doi: 10.1056/NEJM198706113162404. [DOI] [PubMed] [Google Scholar]
- 3.Giardiello FM, Brensinger JD, Tersmette AC, Goodman SN, Petersen GM, Booker SV, et al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000;119:1447–1453. doi: 10.1053/gast.2000.20228. [DOI] [PubMed] [Google Scholar]
- 4.Hizawa K, Iida M, Matsumoto T, Kohrogi N, Kinoshita H, Yao T, et al. Cancer in Peutz-Jeghers syndrome. Cancer. 1993;72:2777–2781. doi: 10.1002/1097-0142(19931101)72:9<2777::aid-cncr2820720940>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 5.Hearle N, Schumacher V, Menko FH, Olschwang S, Boardman LA, Gille JJ, et al. Frequency and spectrum of cancers in the Peutz-Jeghers syndrome. Clin Cancer Res. 2006;12:3209–3215. doi: 10.1158/1078-0432.CCR-06-0083. [DOI] [PubMed] [Google Scholar]
- 6.Park do Y, Lauwers GY. Gastric polyps: classification and management. Arch Pathol Lab Med. 2008;132:633–640. doi: 10.5858/2008-132-633-GPCAM. [DOI] [PubMed] [Google Scholar]
- 7.Tatsuta M, Okuda S, Tamura H, Taniguchi H. Gastric hamartomatous polyps in the absence of familial polyposis coli. Cancer. 1980;45:818–823. doi: 10.1002/1097-0142(19800215)45:4<818::aid-cncr2820450435>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 8.Flageole H, Raptis S, Trudel JL, Lough JO. Progression toward malignancy of hamartomas in a patient with Peutz-Jeghers syndrome: case report and literature review. Can J Surg. 1994;37:231–236. [PubMed] [Google Scholar]
- 9.Bertoni G, Sassatelli R, Nigrisoli E, Pennazio M, Tansini P, Arrigoni A, et al. Dysplastic changes in gastric fundic gland polyps of patients with familial adenomatous polyposis. Ital J Gastroenterol Hepatol. 1999;31:192–197. [PubMed] [Google Scholar]
- 10.Attard TM, Giardiello FM, Argani P, Cuffari C. Fundic gland polyposis with high-grade dysplasia in a child with attenuated familial adenomatous polyposis and familial gastric cancer. J Pediatr Gastroenterol Nutr. 2001;32:215–218. doi: 10.1097/00005176-200102000-00026. [DOI] [PubMed] [Google Scholar]