Abstract
Objectives
To evaluate the trends of disease-modifying anti-rheumatic drugs (DMARDs) used in the treatment of rheumatoid arthritis (RA).
Methods
Patients who fulfilled the ACR criteria for RA from 1995 to 2006 and who attended the Rheumatology clinic at Ipoh Hospital were selected and their records were evaluated to determine the changing trends in the use of DMARDs.
Results
128 patients with RA were identified. The most commonly prescribed DMARD as monotherapy was sulphasalazine (47.7%), followed by methotrexate (35.9%) and hydroxychloroquine. Methotrexate and sulphasalazine were the most frequently prescribed DMARDs, of which the use of methotrexate has increased 6 folds from 1997 to 2007 and the use of sulphasalazine remains around 30% to 50%. The combination of methotrexate with leflunomide has significantly increased in usage by 4 folds during the study period whilst methotrexate with sulphasalazine combination usage had slightly declined.
Conclusion
DMARDs are still the cornerstone in the treatment of RA. Changes in the trend and aggressive use of DMARDs has been markedly influenced by the patient’s awareness of early treatment, the incapacitating damage, availability of recently introduced leflunomide and the advancement of current recommended treatment protocol.
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory disorder of unknown etiology which may be remitting, but if uncontrolled may lead to destruction of joints due to erosion of cartilage and bone, leading to deformity.
A Study by Wolfe et al. has shown that rheumatoid arthritis (RA) is associated with substantial long-term morbidity, mortality and healthcare costs.1 Disease-modifying anti-rheumatic drugs (DMARDs) control disease activity, reduce joint erosions and improve quality of life as well as reduce cardiovascular morbidity associated with RA such as ischemic heart disease.2 In recent years, there has been a change towards early and more dynamic treatment of RA. Early diagnosis of RA prompted the use of DMARDs in higher doses and often in combination therapy to control the disease activity.3 Failure to achieve control with DMARDs, therapy is then followed by biological agents such as tumor necrosis factor (TNF) inhibitors. For decades, methotrexate became the most commonly used DMARD in both mono-therapy and in combination therapy with other DMARDs. Its disease modifying quality and tolerability account for long duration of therapy.1,4,5 However, despite the proven efficacy of DMARDs, it appears that a large number of RA patents received DMARD therapy late; and not at all in some cases.6 Most of the existing data on DMARDs use comes from secondary care alone and are susceptible to referral bias.
This study focuses on the treatment of RA patients in a single rheumatology centre by evaluating the prescribing habits of DMARDs.
Methods
This is a retrospective cross-sectional study involving patients attending the rheumatology clinic, Hospital Raja, Parmaisuri Bainum (HRBP) whom fulfilled the ACR criteria for RA from 1995 to 2006 at any stage of the disease, received at least a single DMARD prescription and who are at least 18 years old.7 The patients were identified by the outpatient’s clinic hospital records, which included the patients’ initials and information about their illness and medication, their age, gender, race, date of diagnosis, duration of disease and co-morbidities.
EpiCalc 2000 v3.32 and Microsoft Office Excel 2003 were used for statistical analysis. Continuous variables were summarized as mean ± SD and categorical variables as frequencies and percentages. Calculation of odds ratio and related 95% confidence intervals were used. Results were considered significant at a P value of <0.05.
Results
A total of 128 patients who fulfilled the ACR criteria for RA between 1996 and 2006 were identified. The mean age of individuals with RA was 52.7 year (SD - 11.5) with the youngest being 24 years old and the oldest being 80 years old. 64.1% of the RA patients were within the range of 41 to 60 years. Females were the predominant gender, who constituted 85.2% (n - 109) of the total study population. Patients of Chinese ethnicity constituted 33.60% (n - 43) of the population, followed by Indians who constituted 32.80% (n - 42), Malays who constituted 27.30% (n - 35), and 6.30% of the study group was constituted by patients from other ethnicities, (Table 1).
Table 1. Demographic Characteristics.
| Demographic | N = 128 |
|---|---|
| Mean (SD) age (years) | 52.7 (11.5) |
| Sex, n (%) Female Male Ratio (F: M) |
109 (85.2) 19 (14.8) |
| Ethnicity, n (%) Malay Chinese Indian Others |
35 (27.3) 43 (33.6) 42 (32.8) 8 (6.3) |
SD: Standard Deviation
The most commonly prescribed DMARD as an agent of first choice in monotherapy approach was sulphasalazine, which was used by 47.7% (n - 61) of the study subjects, followed by methotrexate (35.9%, n - 46) and hydroxychloroquine (16.4%, n - 21). The Combination therapy approach was ranked among the third most commonly prescribed (8.6%). D-Penicillamine, cyclosporine A and prednisolone were not commonly prescribed. Leflunomide was only recently available in HRBP and the total use during the study period was only 1.5%.
Table 2. The Distribution Frequencies of Combination Drug Approach as First Treatment when Diagnosed with RA (n - 11).
| Combination for the 1st DMARDs used | Frequency | Percent |
|---|---|---|
| MTX+Sulphasalazine | 4 | 36.4 |
| MTX+Hydroxychloroquine | 3 | 27.2 |
| Sulphasalazine+Hydroxychloroquine | 2 | 18.2 |
| MTX+Leflunomide | 1 | 9.1 |
| MTX+Leflunomide+Hydroxychloroquine | 1 | 9.1 |
| Total | 11 | 100 |
MTX: Methotrexate
The most commonly prescribed DMARDs in combination drug approach were Methotrexate and Sulphasalazine (36.4%)followed by Methotrexate and Hydroxychloroquine (27.2%).
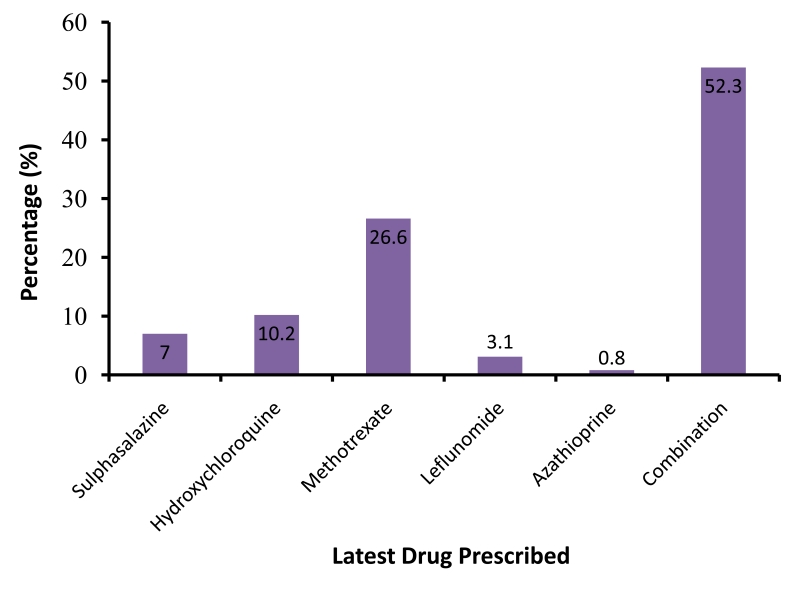
During the last clinic consultation in 2007, combination of DMARD therapy accounted for 52.3% (n - 67) followed by monotherapy with Methotrexate (26.6%), Hydroxychloroquine (10.2%) and Sulphasalazine (7.0%), (Figure 1).
Figure 1.
The Distribution Frequencies of the Latest Drug Prescribed in RA patients (n=128).
Table 3 shows the frequencies (%) of combinations of DMARDs from the latest treatment figures in 2007 for patients with RA. The use of Methotrexate with Leflunomide was the commonest combination therapy (32.8%, n - 22), followed by the combination of Methotrexate and Sulphasalazine, 25.4% (n - 17).
Table 3. The Distribution of frequencies of combination approach for the latest treatment in patients with RA.
| Combination for the Latest Drug | Frequency | Percent |
|---|---|---|
| MTX+Sulphasalazine | 17 | 25.4 |
| MTX+Hydroxychloroquine | 3 | 4.5 |
| Sulphasalazine+Hydroxychloroquine | 5 | 7.5 |
| MTX+Leflunomide | 22 | 32.8 |
| MTX+Leflunomide+Sulphasalazine | 6 | 9.0 |
| Leflunomide+Sulphasalazine | 6 | 9.0 |
| Leflunomide+Hydroxychloroquine | 3 | 4.5 |
| MTX+Leflunomide+Hydroxychloroquine | 1 | 1.5 |
| MTX+Hydroxychloroquine+Sulphasalazine | 2 | 3.0 |
| Azathioprine+Hydroxychloroquine | 2 | 3.0 |
| Total | 67 | 100.0 |
MTX: Methotrexate
The relative use of different DMARDs has changed over the 12-year period. Methotrexate prescriptions increased by a 6-fold from 10% of all DMARDs used in 1997 to 60% in 2006. The use of sulphasalazine remained fairly constant at 30% to 50% in all RA patients. However, combination therapy became more popular over this period, with almost 52.3% of patients prescribed more than one DMARD in 2007.
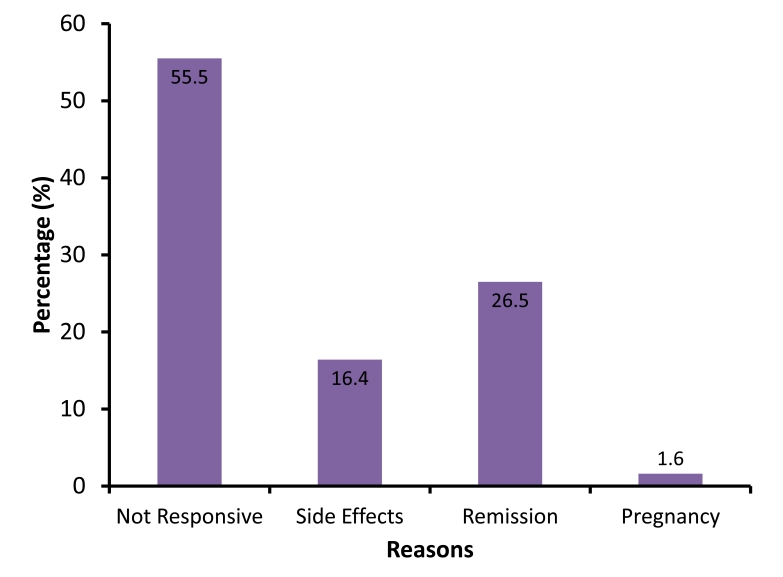
There was a significant association between the first DMARD prescribed and the reasons for changing to other DMARDs (p - 0.003). The first DMARDs prescribed often produced inadequate control of disease activity in most patients (55.5%), and in some cases, the patients developed adverse reactions to certain DMARDs (31.8%).
Figure 2.
The Distribution of Reasons for Changing Drugs in RA patients (n - 128).
71 patients (55.5%) did not achieve satisfactory remission period. However, 26.5% of patients achieved clinical remission with combination therapy after failed monotherapy and 16.4% of patients (n - 21) switched to another DMARD due to side effects. Meanwhile, pregnancy accounted for 1.6% of the reasons for changing DMARDs.
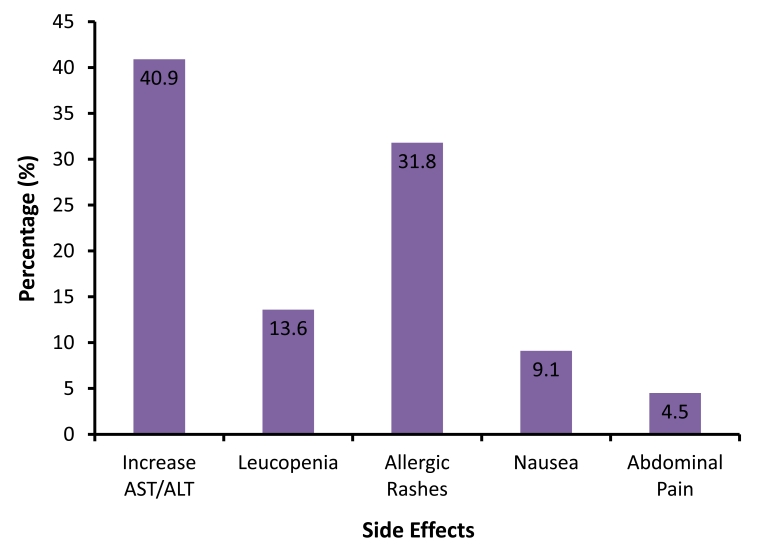
Figure 3.
The distribution of frequencies (%) of side effects of using DMARDS in RA patients (n - 21). AST - Aspartate Transaminase, ALT - Alanine Transaminase.
The results showed that 21 of 128 patients developed side effects, the most frequently encountered was an increase in liver transaminases (AST/ALT) (40.9%), followed by rashes (31.8%) and leucopenia (13.6%). The remaining adverse reactions were minor symptoms such as nausea and vomiting.
Discussion
This study focused on the use of DMARDs in Rheumatoid Arthritis patients who were treated at the rheumatology clinic. However, this was a single center study and therefore does not reflect the true prevalence and practice throughout the country. In Malaysia, there are still no recorded databases which have been cross-checked and validated for accuracy. Hence, the factors that govern the use of DMARDs are still individualized in respective rheumatology centres. Drug availability, cost, patient compliance and adverse events played an important role in determining the pattern of treatment.
DMARD monotherapy has long been used for treating RA patients. In early years, methotrexate and sulphasalazine were the most commonly used; furthermore, the use of Steroids was tremendously overused as well during the same era. Hence, due to the lack of awareness among the clinicians and patients, untreated symptoms led to several RA complications such as deformities, as a result of improper monitoring of DMARD and steroid usage, thus patients experienced adverse effects, which were inevitably unavoidable under the circumstances. However, in recent years, the numbers of rheumatologist in the country has encouragingly increased. Thus the delivery of healthcare for the management of RA patients has markedly improved. The paradigm shift in the treatment of RA patients has greatly influenced the treatment trend illustrated in this study.
Nevertheless, methotrexate monotherapy has been proven to be the most effective compared to other DMARDs and the everlasting use of methotrexate in 50% of RA patients dispute it is ineffective. The withdrawal of methotrexate however, was mainly due to adverse effects.1,4,5 It has been shown in previous studies that RA patients were less likely to receive DMARDs such as methotrexate if they were treated by a non-rheumatologist.8 Over the 12 yr follow-up, sulphasalazine was the most commonly prescribed DMARD as monotherapy, followed by methotrexate. However, there was an enormous change in the prescribing trend of DMARDs in recent years when all RA patients at the center were managed by rheumatologists. The use methotrexate has increased by 6-fold, which was partly due to more frequent usage as the first-line DMARD as a result of its long lasting effects in RA patients.
Most DMARDs have a wide range of side effects, from serious hepatotoxicity, bone marrow suppression, pulmonary complications, to less threatening gastrointestinal effects, hair loss and other constitutional symptoms. DMARDs act by modifying the immune system; therefore leaving the patients more susceptible to infections. Certain DMARDs are also known for their teratogenic effects if taken by pregnant women or women who may become pregnant. The use of DMARDs requires ongoing monitoring to detect the adverse effects on the liver, kidney and other organs. As demonstrated in this study, most of the side effects encountered included an increase in liver enzymes (40.9%) and rashes (31.8%).
The progression of RA can lead to poor quality of life and can become a burden on patients, particularly those from low socio-economic backgrounds. This has prompted early diagnosis and aggressive treatment with DMARDs and therefore, resulting in tight control of the disease activity. This study showed that there was a significant increase in the trend of shifting from mono to combination therapy over the period of 12 years. This increasingly dynamic and aggressive approach in management of RA has also been reported in previous studies.9,10
There were some limitations in this study however; such as the inability to properly evaluate the treatment response over the period mentioned as there was no proper measurement of clinical response such as DAS28 score, ACR responses, HAQ or SF-26 available or performed on regular basis.
Conclusion
Clinicians, Rheumatologist and Pharmacists play a major role in managing and educating RA patients to ensure the compliance and they also need to evaluate and determine the reasons for noncompliance, thus prolonging the survival of RA patients and improving their quality of life. The RA registry in Malaysia was just recently established and it is expected to provide better care and treatment to registered RA patients. With this advancement, further studies will enable better evaluation and assessment of the treatment outcomes in larger study groups of RA patients.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
- 1.Wolfe F, Hawley DJ, Cathey MA. Termination of slow acting antirheumatic therapy in rheumatoid arthritis: a 14-year prospective evaluation of 1017 consecutive starts. J Rheumatol 1990. Aug;17(8):994-1002 [PubMed] [Google Scholar]
- 2.Choi HK, Hernán MA, Seeger JD, Robins JM, Wolfe F. Methotrexate and mortality in patients with rheumatoid arthritis: a prospective study. Lancet 2002. Apr;359(9313):1173-1177 10.1016/S0140-6736(02)08213-2 [DOI] [PubMed] [Google Scholar]
- 3.American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines Guidelines for the management of rheumatoid arthritis: 2002 Update. Arthritis Rheum 2002. Feb;46(2):328-346 10.1002/art.10148 [DOI] [PubMed] [Google Scholar]
- 4.Weinblatt ME, Weissman BN, Holdsworth DE, Fraser PA, Maier AL, Falchuk KR, et al. Long-term prospective study of methotrexate in the treatment of rheumatoid arthritis. 84-month update. Arthritis Rheum 1992. Feb;35(2):129-137 10.1002/art.1780350202 [DOI] [PubMed] [Google Scholar]
- 5.Rau R, Schleusser B, Herborn G, Karger T. Long-term treatment of destructive rheumatoid arthritis with methotrexate. J Rheumatol 1997. Oct;24(10):1881-1889 [PubMed] [Google Scholar]
- 6.Johannes CB, Schneider G, Aygun AC, L’Italien GJ, Viveash D, Wallis WJ. Time to first disease modifying anti-rheumatic drug therapy (DMARD) among rheumatic disease patients in a population based study (abstract).Arthritis Rheum 2003;48(Suppl):S337 [Google Scholar]
- 7.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988. Mar;31(3):315-324 10.1002/art.1780310302 [DOI] [PubMed] [Google Scholar]
- 8.Criswell LA, Such CL, Yelin EH. Differences in the use of second-line agents and prednisone for treatment of rheumatoid arthritis by rheumatologists and non-rheumatologists. J Rheumatol 1997. Dec;24(12):2283-2290 [PubMed] [Google Scholar]
- 9.Carli C, Ehlin AG, Klareskog L, Lindblad S, Montgomery SM. Trends in disease modifying antirheumatic drug prescription in early rheumatoid arthritis are influenced more by hospital setting than patient or disease characteristic. Ann Rheum 2006;65:1102-1105 . 10.1136/ard.2004.027656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Möttönen T, Hannonen P, Korpela M, Nissilä M, Kautiainen H, Ilonen J, et al. FIN-RACo Trial Group. FINnish Rheumatoid Arthritis Combination therapy Delay to institution of therapy and induction of remission using single-drug or combination-disease-modifying antirheumatic drug therapy in early rheumatoid arthritis. Arthritis Rheum 2002. Apr;46(4):894-898 10.1002/art.10135 [DOI] [PubMed] [Google Scholar]