Abstract
A robust, linear association between socioeconomic status (SES) and health has been identified across many populations and endpoints. This relationship is typically monotonic, so that each step down the SES hierarchy brings increased vulnerability to disease and premature mortality. Despite growing attention to health disparities, scientists and policy makers have made little progress toward confronting their causes and implementing effective solutions. Using the Reserve Capacity Model (Gallo & Matthews, 2003) as an organizing framework, the current article examines the contribution of resilient psychosocial resources to socioeconomic disparities in physical health. Findings suggest that deficient psychosocial resources, such as low perceptions of control and social support, may be one of many factors that connect low SES with poor health. Additional research is needed to test these relationships and their underlying mechanisms, to consider interventions to enhance reserve capacity, and to evaluate the efficacy of such efforts in fostering resilience to socioeconomic hardship.
Keywords: Health Disparities, Socioeconomic Status, Resources, Reserve Capacity
The powerful association between socioeconomic status (SES) and physical health has been recognized for many decades. Whether defined according to educational attainment, income, or occupational status, lower SES is associated with diverse disease endpoints and with premature mortality. The relationship is typically monotonic, such that each step down the socioeconomic hierarchy brings increased health vulnerability to health problems, including functional impairment, poor self-rated health, disease-specific morbidity, and premature mortality. Thus, the robust health impact of SES is not solely a reflection of the poor health suffered by those in poverty.
Despite growing attention to health disparities, efforts to confront their causes have lagged behind. In part, this is due to our limited understanding of the factors that underlie health disparities. The picture is complicated since SES shapes virtually every aspect of health risk, including healthcare access and quality, environmental exposures, community characteristics, health behaviors, and psychosocial functioning. The elimination of health disparities will require multi-level interventions that operate across systems and sectors. Psychological scientists can facilitate these efforts by uncovering key psychosocial and behavioral pathways and translating their findings into targeted prevention and intervention strategies.
The Reserve Capacity Model
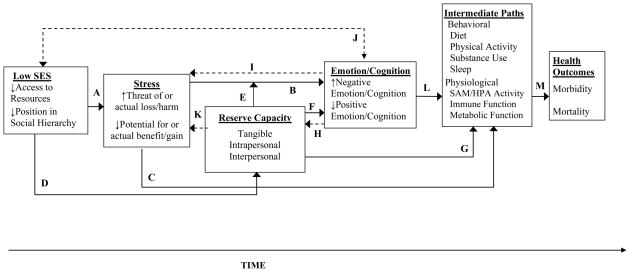
We developed the Reserve Capacity Model (Gallo, Bogart, Vranceanu, & Matthews, 2005; Gallo & Matthews, 2003) as a broad organizing framework for research examining psychosocial variables in SES-related health disparities. As shown in Figure 1, this model incorporates three fundamental psychosocial pathways.
Figure 1.
The Reserve Capacity Model (adapted and modified from Gallo & Matthews, 2003) of the dynamic associations among socioeconomic status (SES), stress, psychosocial resources, emotions, and health. Dashed lines indicate possible reverse or reciprocal effects. Arrow A shows the direct influence of SES on positive and negative psychosocial experiences, or stress experiences and appraisals. Arrow B indicates the direct impact of stressful experiences on emotions/cognitions. Arrow C shows the association between stress and intermediate, behavioral and physiological pathways to health outcomes. Arrow D shows that socioeconomic contexts can shape and deplete resilient resources, leading to reduced reserve capacity. Arrow E shows that Reserve Capacity may moderate the association between stress and emotional responses (i.e., interaction effects). Arrow F shows the direct association between reserve capacity resources and emotions. Arrow G shows that resilient resources can also impact behavioral and physiological risk pathways. Arrows H and I (dashed lines) indicate the possible influence of emotions/cognitions on reserve capacity and stress experiences or appraisals, respectively. Arrow J (dashed, bi-directional line) shows that SES may affect emotions/cognitions independent of the association with stress, and that emotional factors (particularly, emotional disorders) can also influence SES. Arrow K (dashed, bi-directional line) shows that one’s level of resilient resources can shape experiences or appraisals of stress, and vice versa. Arrows L and M depict the associations from emotions/cognitions, to intermediate pathways, to health outcomes. SAM = sympathetic adrenal medullary axis. HPA = hypothalamic, pituitary, adrenal axis.
First, as compared to their higher-SES counterparts, individuals with low SES endure more stress, which in turn predicts physical health outcomes such as cardiovascular disease and premature mortality (Arrows A, C and M). Second, increased negative and reduced positive emotions (well-known correlates of stressful environments) may contribute to the relationships among SES, stress and health (Arrows B and J). Compared to their higher SES counterparts, individuals with lower SES tend to report greater depression, anxiety, and hostility – emotional factors that subsequently relate to health risk factors and outcomes (Arrows L and M). Finally, individuals with low SES may be more physiologically and emotionally reactive to stress. Based on resource-models of stress (Hobfoll, 2001) and healthy aging, we proposed that this heightened vulnerability occurs because individuals with low SES have few resilient resources (i.e., Reserve Capacity) with which to manage frequent environmental demands (Arrow D). In addition, stress combined with low resources can generate further stress and resource deficiencies, fostering spiraling stress and losses (Arrow K; Hobfoll, 2001). Importantly, research suggests that resilient psychosocial factors also relate directly with health, so that Reserve Capacity could moderate (Arrow E) or mediate (Arrows F and G) the relationships among SES, stress, and emotional and physical health.
The Reserve Capacity Model emphasizes resilient personal and social factors that have been related to SES and physical health, and have been shown to alter emotional and physical stress responses. These include interpersonal resources, such as social support and social integration, and intrapersonal resources, such as perceived control (i.e., mastery), optimism, and self-esteem. Ultimately, resources are believed to affect health via converging biological and behavioral risk pathways. For example, they can dampen physiological stress responses that foster disease vulnerability, or they can help attenuate stress perceptions, facilitate positive outcome expectancies, and promote adaptive coping. Low resources and stress also relate to unhealthy behaviors, such as smoking, poor nutrition, and reduced sleep. In turn, these interrelated biobehavioral pathways can promote a host of health problems, including chronic and infectious diseases and premature mortality (Miller, Chen, & Cole, 2009).
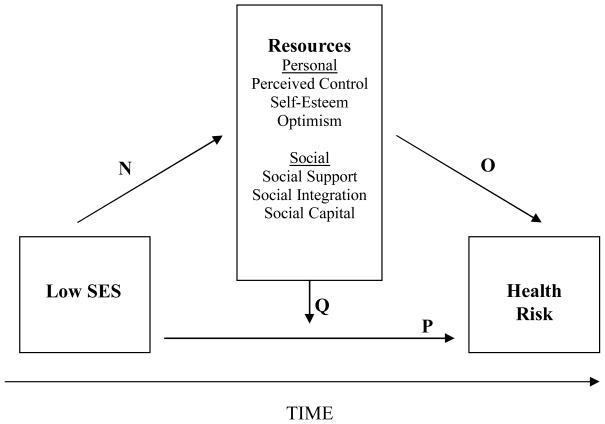
Much of the research that informed the Reserve Capacity Model provided indirect support, since few studies had concurrently examined associations among SES, psychosocial factors, and physical health prior to 2002. Although a more recent review suggests that the literature base remains somewhat limited (Matthews, Gallo, & Taylor, 2009), studies examining contributions of resilient resources are particularly promising. When combined with other research, these findings suggest that Reserve Capacity may represent a modifiable intermediate pathway connecting SES with health. The current manuscript examines what we have learned to date about the roles of resilient resources in associations among SES, stress, and physical health. As shown in Figure 2, we examine studies that have tested whether resilient resources mediate the association between SES and health outcomes – i.e., if, in part, the impact of SES on health occurs through an indirect pathway via a relationship with resource variables and their subsequent effects on health risk (Arrows N, O, P). Where possible, we describe the proportion of the SES effect attributable to resource variables in order to provide information about the importance, or magnitude, of the meditational pathway. We also examine studies that have addressed moderation, or the possibility that resources alter the relationship between SES and health risk (Arrow Q)--for example, by attenuating the unhealthy effects of stressful low SES environments. Our discussion includes examination of subjective as well as objective health outcomes. However, since a common underlying construct (e.g., negative affectivity) could influence perceptions of both resources and self-rated health, studies with subjective endpoints should be viewed more tentatively. We conclude with a discussion of future research directions and a brief examination of how the Reserve Capacity framework might guide intervention efforts aimed at eliminating socioeconomic-health disparities.
Figure 2.
Reserve Capacity Model pathways examined in the current article. Arrows N, O, and P depict the indirect association of SES and physical health through personal and social resources (mediated pathway). Arrow Q indicates that psychosocial resources can modify the impact of SES on physical health (moderated pathway).
Do resilient resources represent a meditational link between SES and health?
Several studies support the idea that differential access to social resources contributes to the relationship between SES and physical health. For example, a longitudinal study of elderly Taiwanese found that most of the effect of low SES on increased mortality occurred indirectly, through health (baseline health status and health behaviors) and social pathways. Moreover, of this indirect association, a quarter was accounted for by reduced social resources (i.e., social participation, integration, and support) in individuals with low SES, which in turn predicted mortality (Liu, Hermalin, & Chuang, 1998). Similarly, a 12-year prospective study showed that deficiencies in social integration explained approximately one third of the excess stroke risk attributed to low education and income (Avendano et al., 2006). Other research suggests that in addition to individual-level social resources, community social features may contribute to the SES-health associations. For example, Franzini, Caughy, Spears, and Esquer (2005) found that neighborhood social capital (perceptions of trust and norms of reciprocity) partially explained the relationship between community impoverishment and self-rated health, with individuals residing in poor neighborhoods reporting lower social capital and, in turn, worse health.
Perceived control (i.e., mastery) is another reserve capacity resource that has received attention as an intermediate factor in the SES-health relationship. Strong support for this pathway was identified in a study of Dutch residents, in which half of the increased mortality risk associated with low education was explained by generalized control beliefs (Bosma, Schrijvers, & Mackenbach, 1999). Another study in a representative sample of 11,110 Canadian adults (Bailis, Segall, Mahon, Chipperfield, & Dunn, 2001) identified a significant indirect effect of low SES on poor self-rated physical and mental health through low perceived control. Moreover, perceived control showed greater explanatory power than behavioral pathways, such as physical activity and smoking. Other studies have found similar evidence with outcomes such as incident heart disease, even after accounting for classical risk factors (e.g., smoking, BMI).
A conceptual limitation of much of the literature is the focus on a single factor–typically perceived control or social support –instead of a bank of resilient resources that might contribute to the SES and health relationship. This is problematic since some research suggests that aggregate resource availability is most relevant to health and well-being (Hobfoll, 2001). To address this issue, Gallo and Matthews have conducted several studies examining a composite indicator of Reserve Capacity in relation to SES- health disparities. In a small study of Hispanic women, psychological resources (aggregated optimism, mastery, self-esteem, and social support) accounted for one third of the relationship between SES and waist circumference (Gallo, Espinosa de los Monteros, Ferent, Urbina, & Talavera, 2007). Waist circumference is a primary pathophysiological mechanism underlying the metabolic syndrome, a constellation of closely related risk factors (i.e., abdominal adiposity, insulin resistance, dyslipidemia, hypertension) that conveys elevated risk of CVD and Type II diabetes. In addition, a 12-year prospective study of middle aged women showed that low SES predicted incident metabolic syndrome risk both directly and indirectly through reduced psychosocial resources (aggregated optimism, social support, and self-esteem) and subsequently higher negative emotions (Matthews, Räikkönen, Gallo, & Kuller, 2008). Thus resources may have direct effects on health risk, and may also affect health indirectly via associations with emotional factors.
Although the literature is not without gaps and inconsistencies (Matthews et al., 2009), these and other studies provide promising evidence that psychosocial resources represent a meditational pathway in the SES-health gradient. Prospective studies that have included large multiethnic samples and objective endpoints lend particularly robust support. However, additional studies are needed to address limitations of available research. For example, studies have mainly focused on limited components of reserve capacity (e.g., control, social support) while largely neglecting other potential resources (e.g., optimism, self-esteem, problem solving skills). Moreover, as stated previously, evaluating the contribution of resources in a piecemeal fashion can overlook their synergistic effects. Future studies should also strive to incorporate well validated measures of resilient factors, since assessments have sometimes consisted of only one or a few items, limiting the ability to fully evaluate meditational roles. Because the importance of resources to SES-health disparities may vary across demographic groups (e.g., sex or ethnicity), studies incorporating large, diverse samples are warranted. Finally, additional prospective studies that include multiple assessments of SES, psychosocial factors, and health will be important to address issues of temporal precedence and causality.
Do resilient resources moderate associations among SES, stress, and health?
The Reserve Capacity Model posits that in addition to their mediating contribution, resources could moderate associations among SES, stress, and health (Pathway Q). From a resilience perspective, low SES individuals who maintain a bank of adaptive personal and social resources could exhibit resistance to disadvantage. For example, Lachman and Weaver (1998) found that individuals with low income but strong control beliefs displayed overall self-rated health, functional limitations, and acute symptoms comparable to those with higher SES. Similarly, greater embeddedness in social life and frequency of social contact were shown to minimize the negative impact of unemployment on self-rated health (Gorman & Sivaganesan, 2007).
In a unique approach to addressing the moderating role of resources, Chen (2007) measured cardiovascular responses to a laboratory stressor in adolescents of varying SES, while manipulating access to resources (specifically, perceptions of control and social informational support). Interaction effects showed that access to informational support attenuated stressor responses in low but not high SES adolescents. Having a sense of control reduced reactivity in the low SES group to a lesser degree, but for high SES participants, neither resource made a difference. This suggests that access to resilient resources may be especially protective for individuals with low SES, possibly because their resource bank is otherwise deficient. In addition, the study demonstrates how hypotheses concerning psychosocial contributions to health disparities can also be examined in an experimental context.
Conclusions and Future Directions
The preceding discussion suggests that additional attention to the roles of psychosocial resources is warranted in efforts to understand and intervene with socioeconomic health disparities. Specifically, some research indicates that individuals with low SES experience a disproportionate burden of disease, in part, because they maintain an insufficient reserve of resilient resources with which to manage stressful environments. In addition, although the evidence base is more limited, some studies suggest that high levels of resources can buffer the deleterious consequences of stressful low SES environments. Nonetheless, additional integrative studies are needed to address the psychosocial pathways proposed in the Reserve Capacity Model, particularly for objective physical health outcomes and using prospective designs. Moreover, the relative strength of each resilient factor could be examined in greater detail, as well as the possible synergistic effects of factors in combination, as this could inform areas of focus for intervention. Longitudinal studies would be especially helpful in efforts to untangle the mechanisms that drive the relationship between SES and psychosocial functioning. For example, research suggests that low SES can increase exposure to “risky family” environments, characterized by parental conflict, neglect, and a lack of nurturance. Such environments may stifle the development of social-emotional coping skills necessary for effective psychological and social functioning. Studies that follow individuals through the lifecourse are also important since SES often “tracks” from childhood into adulthood and across generations. Other promising areas for future research include examining the possible influence of SES on biological and neurological processes underlying divergent psychosocial profiles, and the integrative effects of SES and genetic predispositions. These and other future research directions are discussed in greater detail in Matthews and colleagues (2009).
Despite the fact that much remains to be learned, the available research suggests that interventions that promote resilient psychosocial resources could have utility in efforts to close SES-related health gaps. For example, community building interventions that increase advocacy and enhance social capital could foster a sense of control and social connectedness among the socioeconomically disadvantaged, resulting in health benefits for the individual and community. Likewise, workplace interventions (e.g., encouraging flexible work hours or control over shift patterns) may be an effective means of resource-building in low-SES employed adults. Given the early origins of psychosocial risk trajectories, adapting school-based intervention programs to build protective resources and targeting prevention efforts toward at-risk families may be particularly effective strategies.
Notably, psychosocial resources form only one piece of the health disparities puzzle, and many researchers argue that attention should be directed toward upstream fundamental causes such as inequitable distribution of wealth, access to quality education, and concentrated poverty. Although the root social and economic forces must be addressed to effectively eliminate health disparities, interventions at the social-structural level (e.g., education and healthcare reform; income redistribution) require vast resources, rely extensively on political will, and can be met with substantial resistance. Such barriers highlight the need for multifaceted approaches that target both the fundamental causes of health disparities and the pathways that maintain and reinforce them. Interventions focused on reducing stress and increasing psychosocial resilience among vulnerable populations may provide an effective and timely complement to social and political efforts aimed at eliminating socioeconomic disparities in health.
Acknowledgments
This project/study was supported in part by grant numbers 1R01HL081604-01, 1T32HL079891-01A2, and F31HL087732-02 from the National Heart Lung and Blood Institute, National Institutes of Health and by grant number 1P20MD002293-01, San Diego Partnership to reduce CVD Disparities, National Center of Minority Health and Health Disparities, National Institutes of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the National Institutes of Health. We thank Dr. Karen Matthews for her comments on an earlier version of this manuscript.
References
- Avendano M, Kawachi I, Van LF, Boshuizen HC, Mackenbach JP, Van den Bos GA, et al. Socioeconomic status and stroke incidence in the US elderly: the role of risk factors in the EPESE study. Stroke. 2006;37:1368–1373. doi: 10.1161/01.STR.0000221702.75002.66. [DOI] [PubMed] [Google Scholar]
- Bailis DS, Segall A, Mahon MJ, Chipperfield JG, Dunn EM. Perceived control in relation to socioeconomic and behavioral resources for health. Social Science & Medicine. 2001;52:1661–1676. doi: 10.1016/s0277-9536(00)00280-x. [DOI] [PubMed] [Google Scholar]
- Bosma H, Schrijvers C, Mackenbach JP. Socioeconomic inequalities in mortality and importance of perceived control: cohort study. British Medical Journal. 1999;319:1469–1470. doi: 10.1136/bmj.319.7223.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E. Impact of socioeconomic status on physiological health in adolescents: an experimental manipulation of psychosocial factors. Psychosomatic Medicine. 2007;69:348–355. doi: 10.1097/PSY.0b013e3180592b20. [DOI] [PubMed] [Google Scholar]
- Franzini L, Caughy M, Spears W, Esquer MEF. Neighborhood economic conditions, social processes, and self-rated health in low-income neighborhoods in Texas: A multilevel latent variables model. Social Science & Medicine. 2005;61:1135–1150. doi: 10.1016/j.socscimed.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Bogart LM, Vranceanu AM, Matthews KA. Socioeconomic status, resources, psychological experiences and emotional responses: a test of the reserve capacity model. Journal of Personality and Social Psychology. 2005;88:386–399. doi: 10.1037/0022-3514.88.2.386. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Espinosa de los Monteros KE, Ferent V, Urbina J, Talavera G. Education, psychosocial resources, and metabolic syndrome variables in Latinas. Annals of Behavioral Medicine. 2007;34:14–25. doi: 10.1007/BF02879917. [DOI] [PubMed] [Google Scholar]
- Gorman BK, Sivaganesan A. The role of social support and integration for understanding socioeconomic disparities in self-rated health and hypertension. Social Science & Medicine. 2007;65:958–975. doi: 10.1016/j.socscimed.2007.04.017. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: Advancing Conservation of Resources theory. Applied Psychology. 2001;50:337–370. [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality & Social Psychology. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Liu X, Hermalin AI, Chuang YL. The effect of education on mortality among older Taiwanese and its pathways. Journals of Gerontology Series B: Psychological and Social Sciences. 1998;53:S71–S82. doi: 10.1093/geronb/53b.2.s71. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of ses and health connections?: A progress report and blueprint for the future. Annals of the New York Academy of Sciences. 2009 doi: 10.1111/j.1749-6632.2009.05332.x. In Press. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Räikkönen K, Gallo LC, Kuller LH. Association between socioeconomic status and metabolic syndrome in women: Testing the Reserve Capacity Model. Health Psychology. 2008;27:576–583. doi: 10.1037/0278-6133.27.5.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G, Chen E, Cole SW. Health Psychology: Developing Biologically Plausible Models Linking the Social World and Physical Health. Annual Review of Psychology. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
Recommended Readings
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. A comprehensive and clearly-written review of current knowledge and issues in ethnic and socioeconomic health disparities research. [DOI] [PubMed] [Google Scholar]
- Kroenke C. Socioeconomic status and health: youth development and neomaterialist and psychosocial mechanisms. Social Science & Medicine. 2008;66:31–42. doi: 10.1016/j.socscimed.2007.07.018. An interesting discussion of material versus psychosocial explanations in health disparities, from a lifecourse perspective. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of ses and health connections?: A progress report and blueprint for the future. Annals of the New York Academy of Sciences. 2009 doi: 10.1111/j.1749-6632.2009.05332.x. In Press. A review of the literature that has examined psychosocial mediators in SES-health disparities to date, incorporating a discussion of the environmental origins of psychosocial risk processes. [DOI] [PubMed] [Google Scholar]
- Myers HF. Ethnicity- and socio-economic status-related stresses in context: An integrative conceptual model. Journal of Behavioral Medicine. 2009;32:9–19. doi: 10.1007/s10865-008-9181-4. A thorough and accessible theoretical analysis of the multiple pathways through which SES and ethnicity interact to influence health. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Stanton AL. Coping Resources, Coping Processes, and Mental Health. Annual Review of Clinical Psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. An interesting review and discussion of resources that contribute to successful coping, their genetic and environmental origins, health implications and possible intervention strategies. [DOI] [PubMed] [Google Scholar]