Abstract
Odontogenic carcinomas are rare lesions arising from dental embryogenic residues and have been designated by a variety of terms like malignant ameloblastoma, ameloblastic carcinoma, metastatic ameloblastoma or primary intra-alveolar epidermoid carcinoma. Ameloblastic carcinoma combines the histological features of ameloblastoma with cytological atypia, even in the absence of metastasis. The lesion has been reported to arise either from the odontogenic cyst or the ameloblastoma. Majority originate de novo and the remaining are malignant transformation of an ameloblastoma.
Keywords: Odontogenic malignancies, Ameloblastic carcinoma
Introduction
Odontogenic malignancies are rare lesions arising from dental embryogenic residues. Odontogenic carcinomas have been designated by a variety of terms, including malignant ameloblastoma, ameloblastic carcinoma (AC), metastatic ameloblastoma, or primary intra-alveolar epidermoid carcinoma. The clinical course and histopathology of these tumours are similar to each other, so the differential diagnosis is not easy to make.
Malignant ameloblastoma represent tumours that metastasize while both primary and metastatic lesions retain their benign histological appearance. The term ameloblastic carcinoma was introduced by Elzay [1]. In the last update of the WHO classification, published in 2005 [2] (Table 1) it is defined as a rare odontogenic malignancy that combines the histological features of ameloblastoma with cytological atypia, even in the absence of metastases. Being uncommon, little information is available in the literature regarding its clinical characteristics, treatment modalities and outcome.
Table 1.
World Health Organization classification of odontogenic carcinomas—2005 [2]
| Metastasizing (malignant) ameloblastoma |
| Ameloblastic carcinoma Primary type Secondary type (dedifferentiated) intraosseus Secondary type (dedifferentiated) peripheral |
| Primary intraosseus squamous cell carcinoma Solid type Derived from keratocystic odontogenic tumor Derived from odontogenic cysts |
| Clear cell odontogenic carcinoma |
| Ghost cell odontogenic carcinoma |
Case Report
A 67-year-old female patient reported with complaint of rapidly growing painless swelling of the right side of the lower jaw since past 6 months. Clinically, a painless ovoid shaped swelling was seen on the right body of the mandible approximately 4 × 3 cm in size which extended anteriorly from the commissure of the lip on right side and posteriorly to the angle of the mandible. Inferiorly the extent was 0.5 cm below the lower border of the mandible. No parasthesia was associated with the swelling nor were regional lymph nodes palpable.
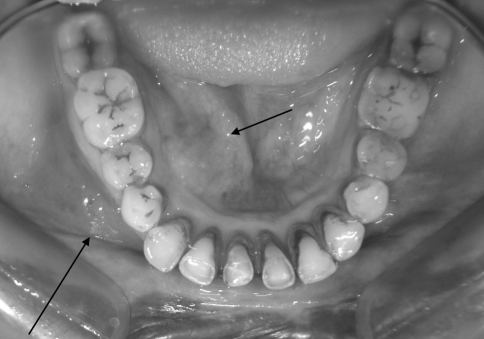
Intra-oral examination revealed a painless smooth swelling extending from 43 to 47 region obliterating the right buccal sulcus and extended lingually with expansion of the lingual cortex (Fig. 1). On intra oral palpation the swelling was soft in consistency with absence of any secondary changes like ulceration/fistula formation/infection/discharge. It was non tender, fluctuant with crepitus positive lingually. Thinning and perforation of the lingual cortex was felt with mobility of 44, 45 and 46.
Fig. 1.
Intra-oral view
Aspirate obtained was a sero sanguinous fluid which was sent for biochemical investigations subsequently revealing protein content 8 mg/dl and sugar content 108 mg/dl. A provisional diagnosis of an ameloblastoma of the right body of the mandible with high virulence was established. Differential diagnosis included variants of ameloblastoma, central giant cell lesion and haemorrhagic bone cyst.
Radiologic Findings
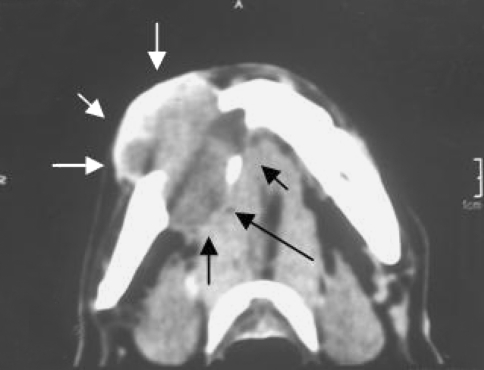
A right lateral oblique radiograph of the mandible showed a single well defined unilocular radiolucent lesion of approximately 2.5 × 2.5 cm in size in the right body with scalloped and irregular margins extending from the 43 to 47 region with thinning and erosion of the inferior border. The roots of 44, 45, and mesial root 46 were resorbed. Occlusal radiograph revealed gross lingual expansion and cortical perforation. A non enhanced axial and coronal computed tomography showed a homogenous expansile lesion affecting the right body of the mandible with thinning and expansion of the buccal cortex with lingual cortex totally destroyed and tumour extending into the soft tissue (Fig. 2). A PA and lateral chest radiograph ruled out presence of any metastatic deposits.
Fig. 2.
Computed tomography
Treatment
Biopsy: An intra-oral vestibular incision was placed and the lesion was carefully dissected out from multiple sites from the surrounding margins and lingual soft tissues to which the lesion had ingress. There was a clear demarcation between the lesion and lingual tissues.
Histopathological Findings
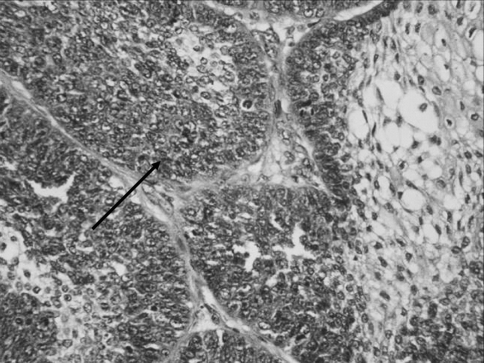
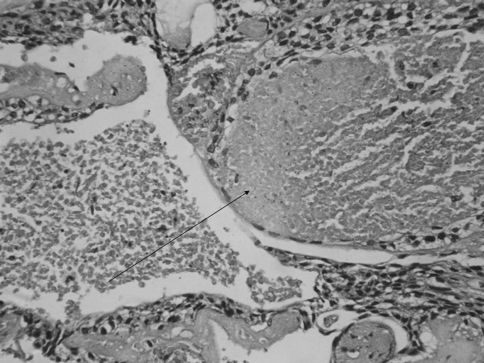
The surgical specimen consisted of multiple bits of soft tissue with the largest sample measuring 4 × 2 × 1 cm. The tissue was soft to firm with the external surface showing areas of congestion and papillary excrescences. The cut surface showed a nodular growth which was pearly white in colour with areas of congestion. Microscopic findings showed nests and islands of epithelium within a collagenous stroma. The cell nests were composed of a peripheral layer of polarised cells enclosing stellate to basaloid cells (Fig. 3). The cells showed large nuclei some of which showed prominent nucleoli and nuclear pleomorphism. Mitotic activity was seen with 3–4 mitotic figures/10 HPF. Central foci of necrosis were present (Fig. 4). No perineural or vascular invasion was seen. Impression was of a very aggressive type of ameloblastoma suggestive of ameloblastic carcinoma.
Fig. 3.
Tumour exhibiting the morphology of an ameloblastoma with high mitotic activity (arrow) and nuclear pleomorphism and basaloid hyperplasia (H&E ×400)
Fig. 4.
Photomicrograph showing focal area of necrosis (H&E ×400)
Surgery: The patient was taken up for surgical resection of the lesion and excision of the surrounding soft tissues. Segmental resection was carried extending from 32 region to the right angle of the mandible with 2 cm of bony margins on each side of the lesion along with excision of surrounding soft tissues in the lingual region. Supraomohyoid neck dissection was carried out on the right side along with excision of submandibular gland. Reconstruction of the defect was done using a rigid titanium reconstruction plate and surgical wound closed primarily in layers. Prosthetic guide flange appliance was provisioned and intermaxillary fixation done with elastics to help in guiding the mandible and stabilize the occlusion. Recovery was uneventful and surgical wounds healed well. Six months follow-up showed no signs of recurrence. Presently the patient is under regular follow-up.
Histopathological report of the resected specimen confirmed the initial report of ameloblastic carcinoma. The resected margins were free of any residual tumour. The lymph nodes showed features of reactive lymphadenitis but free of tumour infiltration.
Discussion
Ameloblastic carcinoma is a rare neoplasm that represents a challenge in its diagnosis, treatment, and prognosis. Information regarding its clinical features is scanty. According to Benlyazid et al. in 2007 [2], a total of 67 cases of ameloblastic carcinoma have been reported in the literature including one case reported by them. Ameloblastic carcinoma has been reported to arise either de novo, ex odontogenic cyst, or ex ameloblastoma [2]. Majority originates de novo, and the remaining are malignant transformation of an ameloblastoma (Fig. 5).
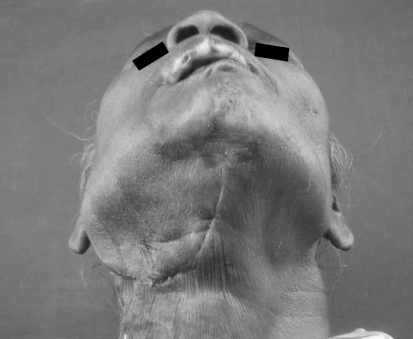
Fig. 5.
Postoperative photograph of the patient
Ameloblastic carcinoma shows cytologic features of malignancy but is otherwise recognizable as an ameloblastoma [3]. The clinical presentation of ameloblastic carcinoma is variable, such as a cystic lesion with benign clinical features or a large tissue mass with ulceration, bone resorption, and tooth mobility. Clinically, they cause expansion of the jaw, grow rapidly, frequently cause pain and results in perforation of the cortex [4]. ‘Expansion’ or ‘hard mass’ is the most common chief complaint followed by pain or discomfort, toothache or tooth mobility, a non-healing extraction site, ulcer or fistula, facial asymmetry and trismus. Perforation of the cortex and rapid growth of the lesion with parasthesia of the lower lip may also be presenting features, though not an essential feature. Although rare, these lesions have been known to metastasize mostly to the lung or regional lymph nodes. It is located most frequently in the posterior mandibular region [5].
Ameloblastic carcinoma does not seem to show any age group predilection, it appears more frequently in men (2/3 of cases) and involves more often the mandible (2/3 of cases). According to Sciubba et al. age range of the patients varies widely with a range of 51/2–84 years, with a mean age of 53.5 years and a male to female ratio of 1.5:1. The location of the tumour is 80% in the mandible as per the available literature [6].
The differential diagnosis between ameloblastoma and ameloblastic carcinoma is dependent on the integration of histologic changes with demographic features and biologic behavior. The diagnostic criteria of an ameloblastic carcinoma that de-differentiated from ameloblastoma are based on cytologic atypia and an increased mitotic index [7]. In cases where ameloblastic carcinoma arise de novo, the microscopic distinction from ameloblastoma is not always obvious and may be subjective. Because numerous mitotic figures are unusual in ameloblastoma, cases where they are sufficiently numerous probably justify the diagnosis of ameloblastic carcinoma. Available literature suggests that the diagnosis of ameloblastic carcinoma is based on several admittedly arbitrary features. Analysis has shown that there are four features namely:
Higher proliferative mitotic index emphasized by higher mitotic activity [8], higher proliferating cell nuclear antigen expression and higher Ki67 [5];
Nuclear atypia such as nuclear pleomorphism and basilar hyperplasia;
Hyperchromatic nuclei of basaloid cells; and
Other features of malignancy such as perineural or perivascular invasion.
The clinical course is reported as typically aggressive, with extensive local destruction and distant metastatic spread if left untreated. This criterion seems to be the major factor of prognosis, with preferentially a haematogenous spreading way. However, metastatic lymph nodes have been described. In addition, this relatively high risk of distant metastasis contrasts with the behaviour of squamous cell carcinomas that spread rather by the lymphatic way. The most involved site of metastasis is the lung, but brain or bony locations have been reported. Wide local excision is the treatment of choice. Some authors advocate 2- or 3-cm bony margins by the means of an en bloc removal [9, 10]. Cervical lymph node dissection should be considered when there is obvious lymphadenopathy. Radiotherapy and chemotherapy seem to be of limited value; however, these methods need to be considered when there is a locally advanced or metastatic disease not amenable to surgical resection. Close periodic reassessment with a long period of follow-up (at least 10 years) is mandatory.
Conclusion
Ameloblastic carcinoma is a rare entity of odontogenic tumors that exhibits malignant histologic features in the primary or metastasis. Ameloblastic carcinomas exhibit rapid growth, perforates the cortical plate, and may exhibit pain and parasthesia. Its histological characterization is difficult and needs the exclusion of many differential diagnoses. Prognosis is good if an early diagnosis of the lesion is made with prompt surgical intervention.
References
- 1.Elzay RP. Primary intraosseous carcinoma of the jaws. Review and update of odontogenic carcinomas. Oral Surg Oral Med Oral Pathol. 1982;54(3):299–303. doi: 10.1016/0030-4220(82)90099-8. [DOI] [PubMed] [Google Scholar]
- 2.Benlyazid A, Lacroix-Triki M, Aziza R, Gomez-Brouchet A, Guichard M, Sarini J. Ameloblastic carcinoma of the maxilla: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(6):e17–e24. doi: 10.1016/j.tripleo.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 3.Slootweg PJ, Müller H. Malignant ameloblastoma or ameloblastic carcinoma. Oral Surg Oral Med Oral Pathol. 1984;57(2):168–176. doi: 10.1016/0030-4220(84)90207-X. [DOI] [PubMed] [Google Scholar]
- 4.Eversole LR. Malignant epithelial odontogenic tumours. Semin Diagn Pathol. 1999;16(4):317–324. [PubMed] [Google Scholar]
- 5.Akrish S, Buchner A, Shoshani Y, Vered M, Dayan D. Ameloblastic carcinoma: report of a new case, literature review, and comparison to ameloblastoma. J Oral Maxillofac Surg. 2007;65(4):777–783. doi: 10.1016/j.joms.2005.11.116. [DOI] [PubMed] [Google Scholar]
- 6.Dhir K, Sciubba J, Tufano RP. Ameloblastic carcinoma of the maxilla. Oral Oncol. 2003;39(7):736–741. doi: 10.1016/S1368-8375(03)00036-8. [DOI] [PubMed] [Google Scholar]
- 7.Slater LJ. Odontogenic malignancies. Oral Maxillofac Surg Clin North Am. 2004;16(3):409–424. doi: 10.1016/j.coms.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(6):660–669. doi: 10.1016/S1079-2104(96)80441-0. [DOI] [PubMed] [Google Scholar]
- 9.Datta R, Winston JS, Diaz-Reyes G, Loree TR, Myers L, Kuriakose MA, Rigual NR, Hicks WL., Jr Ameloblastic carcinoma: report of an aggressive case with multiple bony metastases. Am J Otolaryngol. 2003;24(1):64–69. doi: 10.1053/ajot.2003.15. [DOI] [PubMed] [Google Scholar]
- 10.Avon SL, McComb J, Clokie C. Ameloblastic carcinoma: case report and literature review. J Can Dent Assoc. 2003;69(9):573–576. [PubMed] [Google Scholar]