Abstract
Proboscis lateralis describes a rudimentary nasal structure or appendage that is located off- center from the vertical midline of the face. This anomaly is embryologically related to the median facial cleft and results in incomplete formation of one side of the nose. The abnormal side of the nose is represented by a tube-like rudimentary nasal structure attached at any point along the embryonic fusion line between the anterior maxillary process and the frontonasal process. Reconstruction should start at an early age as proboscis itself is the best option for heminose reconstruction. Cartilaginous or bony support can be planned in the late teens to give good aesthetic result. Here we report a rare case of proboscis lateralis in a 4-year-old female patient.
Keywords: Frontonasal reconstruction, Proboscis lateralis (PL), Medial canthus
Introduction
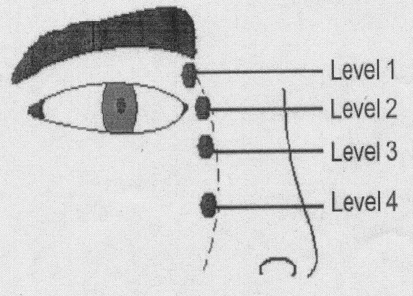
Proboscis lateralis (PL) is a rare craniofacial anomaly with a reported incidence of less than 1 in 100,000. This condition is caused by the developmental failure or absence of medial and lateral nasal processes, resulting in fusion of the maxillary process with the contralateral frontal process [1]. The various localization points of PL may be at the embryonic fusion line between the anterior maxillary process and the frontonasal process, level 1, supramedial canthal area; level 2, medial canthal area; level 3, inframedial canthal area; level 4, supranostril area (Fig. 1) [2].
Fig. 1.
Schematic view of the various localization points of proboscis lateralis
Khoo-Boo Chai classified them into four groups discussed various management options, and advised dilatation of the proboscis before starting the reconstruction [3]. For the complete evaluation of this anomaly CT scan is important which allows assessment of growth of facial and skull bones as well as CNS implications.
Management should start early in childhood to avoid psychological consequences related to this deformity. For the heminose reconstruction, use of proboscis itself is the best option. Later secondary procedures are required to correct skeleton deformity and groove of the inset of proboscis with normal heminose.
Case Report
A 4-year-old female patient reported to Department of Oral and Maxillofacial surgery for evaluation of a soft, approximately 3-cm long and 1-cm-diameter trunk like process originating from the region of the right medial canthus (Figs. 2, 3). A diagnosis of PL was made on the basis of the characteristic appearance of the anomaly. There was no history of consanguinous or family history of congenital defects. The prenatal history was negative for exposure to alcohol, drugs, or ionizing radiation.
Fig. 2.
A 4-year-old child with right sided proboscis lateralis
Fig. 3.
Tubular structure arising from medial canthus area and absent heminose
Physical examination revealed a hypoplastic right nostril with a normal left nasal structure. The nasal airway was unilaterally patent. There was no accompanying abnormality of the eye, eyelid, lip, or palate. Diagnostic imaging consisting of CT was obtained to evaluate the full extent of the congenital anomaly and to rule out communication between the intracranial compartment and the proboscis prior to surgical repair. The right maxillary and ethmoid sinuses were absent and the nasal septum was totally deviated to the right (Fig. 4.). The left side was normal and the left nasal airway was patent. First stage nasal reconstruction was done under general anesthesia using one stage degloving method for right heminose (Fig. 5)
Fig. 4.
The coronal multislice computed tomographic image shows the agenesia of the right maxillary and ethmoidal sinus
Fig. 5.
Schematic representation of surgical reconstruction of the right heminose using the proboscis
A foil template of the normal left heminose was made and reversed to design a right heminose from the proboscis. The midportion of the columella base was defined, and the distance from this point to the alar base was measured. From this measurement, the width of the nasal base was determined, and the position of the right alar base was marked. The medial portion of the proboscis was marked and de-epithelialized to recreate a right nasoseptal lining. With the template used as a guide, the right alar subunit was created and sutured into position with 5-0 polyglactin suture. The deepithelialized portion of the proboscis was then sutured to the septum as a right nasoseptal lining using 5-0 polyglactin suture. The proboscis was left pedicled at its base in the right medial canthal region. The procedure was carried out and the aplastic right nostril was incised horizontally at the location of the future nostril. The skin covering the proboscis was deepithelized and sutured under the skin over the opposite nostril to prevent the formation of a furrow (Fig. 6). The patient was discharged from the hospital on the second postoperative day and the sutures were removed after 1 week (Fig. 7) and the patient was followed regularly up to 6 months (Fig. 8).
Fig. 6.
A tunnel is prepared on the right nasal dorsum and the proboscis is deepithelialized
Fig. 7.
Postoperative view of the patient after 1 week
Fig. 8.
Worms eye view of the patient after 6 months
Discussion
Proboscis lateralis typically manifests as a soft, 2- to 3-cm-long and 1-cm diameter trunk like process originating from the region of the medial canthus. It is characterized by a central tract lined with squamous and ciliated respiratory epithelium that typically expresses clear mucus from the blind dimple at its distal end. Although PL has been described in the absence of other congenital anomalies, it is characteristically accompanied by ipsilateral heminasal hypoplasia or aplasia and rarely by choanal atresia [4]. Ocular and/or ocular adnexal findings as well as cleft lip and/or palate are the most common anomalies seen in conjunction with PL and have been used as the basis for a classification system [5]. Group 1 consists of isolated PL without other associated anomalies (9%). Group 2 consists of PL with associated ipsilateral nasal defect (23%). Group 3 consists of PL with associated ipsilateral nasal and ocular and/or ocular adnexal defect (47%). Group 4 includes the features of group 3 with the addition of cleft lip and/or palate (21%). Embryologic development of the face and nose is a complex process. The nasal placodes appear to function as the primary organizers for the developing nose. The nasal placodes invaginate into the frontonasal process, separating this structure into the medial and lateral nasal processes. The precise embryologic mechanism responsible for the development of PL has not been defined. Popular theories include imperfect fusion of the lateral nasal and maxillary processes and aberrant fusion of the maxillary process of the affected side to the medial nasal process (globular process) [6]. Rontal and Duritz correctly point out that these theories do not adequately explain the associated anomalies and suggest a primary insult to the nasal placode as the likely mechanism for PL development [7].
Initial reports regarding the treatment of PL recommended simple surgical excision of the proboscis. More recently, surgical management of PL has been approached with reconstruction in mind. Many authors advocate use of the proboscis to reconstruct the nose because it provides excellent color and texture match and is readily available. Dilation of the central canal may be performed prior to surgical repair. For cases with a patent nasal airway, the proboscis may be split along its length with the cut edges sutured to the pyriform margin and the nasal dorsum. Alternatively, if no nasal cavity exists on the affected side, the proboscis may be de-epithelialized and passed under a transverse bipedicled flap. With this method, the base of the proboscis is then excised at a later stage [8]. Alternatively, a wealth of experience exists with regard to the use of local pedicled flaps such as the melolabial flap or the paramedian forehead flap for reconstruction of nasal defects of various etiologies [9]. With this approach, the proboscis can be excised early with definitive reconstruction performed at a later date. Given the high degree of variability of associated anomalies, an individualized approach is suggested when undertaking surgical management of PL. In general, surgical repair can be accomplished as early as possible without adversely affecting the cosmetic outcome.
Conclusion
In conclusion, Proboscis lateralis is a rare congenital anomaly with a characteristic appearance. Radiographs and Computed tomography are complementary in determining the extent of the bony and soft tissue components of the anomaly. Proboscis lateralis is most commonly associated with developmental anomalies of the ipsilateral nasal and ocular structures. Complete surgical excision at the base of the proboscis is desirable as a primary procedure if there is adequate ipsilateral nasal development or as a delayed excision if the proboscis is used in nasal reconstruction. Definitive cosmetic reconstruction with bone or cartilage should be planned at a later age keeping in mind the possibility of further growth and development of the nasal complex.
References
- 1.Acarturk S, Kivanc K, Atilla E, Sekucoglu T. Proboscis lateralis: evaluation of the anomaly and a review of two cases. Plast Reconstr Surg. 2006;117(7):2119–2127. doi: 10.1097/01.prs.0000218801.38826.31. [DOI] [PubMed] [Google Scholar]
- 2.Thorne MC, Ruiz RE, Carvalho J, Lesperance MM. Proboscis lateralis: case report and review. Arch Otolaryngol Head Neck Surg. 2007;133(10):1051–1053. doi: 10.1001/archotol.133.10.1051. [DOI] [PubMed] [Google Scholar]
- 3.Abou-Elhamd KE. Proboscis lateralis: a report of two cases. Int J Pediatr Otorhinolaryngol. 2004;68(4):503–505. doi: 10.1016/j.ijporl.2003.11.021. [DOI] [PubMed] [Google Scholar]
- 4.David LR, Sanger C, Fisher D, Argenta LC. Proboscis lateralis: a rare craniofacial anomaly, reconstruction, and long-term evaluation. J Craniofac Surg. 2008;19(4):1107–1113. doi: 10.1097/SCS.0b013e318176ac9f. [DOI] [PubMed] [Google Scholar]
- 5.Guerrero JM, Cogen MS, Kelly DR, Wiatrak BJ. Proboscis lateralis. Arch Ophthalmol. 2001;119(7):1071–1074. [PubMed] [Google Scholar]
- 6.Khoo BC. The proboscis lateralis—a 14-year follow-up. Plast Reconstr Surg. 1985;75(4):569–577. doi: 10.1097/00006534-198504000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Rontal M, Duritz G. Probocis lateralis: case report and embryologic analysis. Laryngoscope. 1977;87(6):996–1006. [PubMed] [Google Scholar]
- 8.Eroglu L, Uysal OA. Proboscis lateralis: report of two cases. Br J Plast Surg. 2003;56(7):704–708. doi: 10.1016/S0007-1226(03)00356-4. [DOI] [PubMed] [Google Scholar]
- 9.Boyd CM, Baker SR, Fader DJ, Wang TS, Johnson TM. The forehead flap for nasal reconstruction. Arch Dermatol. 2000;136(11):1365–1370. doi: 10.1001/archderm.136.11.1365. [DOI] [PubMed] [Google Scholar]