Abstract
Objective
The present study aimed to evaluate the prevalence, sex predilection and treatment modalities of OKC in Central India.
Materials and Methods
Total 2900 patients were screened from various hospitals and centers. Age of patients and site of lesion was recorded. OKC was classified into initial, moderate and advanced depending on the radiological involvement and treatment modalities given with respect to the extent of the OKC.
Result
Total 49 patients were diagnosed with the presence of OKC. It was found that mostly it is common in 3rd and 4th decades, with the mean age 28 years in males and 31 years in females. The most common site of occurrence was angle of mandible and the ramus region. The treatment of OKC, on the basis of the radiographic classification, gives excellent results with minimum recurrences.
Conclusion
The most common age and site occurrence was relevant with that of previous studies (Browne, Br Dent J 128(5):225–231, 1970, Chen and Lin, Gaoxiong Yi Xue Ke Xue Za Zhi 2(9):601–607, 1986). This study concluded by considering multicentric incidence, prevalence of OKC in Central India, that the population should be screened for OKC. The screening should be done by clinical, radiological and histopathological. While screening all the parameters should be considered to diagnose and treat the patients for the prevention of morbidity.
Keywords: Odontogenic keratocyst (OKC) prevalence, Treatment, Recurrence and Central India
Introduction
The odontogenic keratocyst (OKC) was first described and named by Phillipsen in 1956. It is one of the most aggressive odontogenic cysts of the oral cavity. OKC is known for its rapid growth and its tendency to invade the adjacent tissues including bone. It has a high recurrence rate of 16 to 30%. Odontogenic keratocysts are generally thought to be derived from either the epithelial remnants of the tooth germ or the basal cell layer of the surface epithelium. Odontogenic keratocysts are commonly seen in the mandible with the majority occurring in the angle of the mandible and ramus. OKC can be classified on the basis of locularity namely Unilocular and multilocular. Unilocular is isolated but not necessarily while multilocular is mostly associated with Naevus Basal Cell Carcinoma syndrome (Gorlin Syndrome). In this study we determined the mode of treatment depending upon the radiographic extent of the OKC. This type of study was carried out first time in central India for prevalence, treatment and recurrence of Odontogenic Keratocyst (Tables 1, 2).
Table 1.
Showing analysis of patients with OKC
| SN | Gender | Site | Treatment | Follow-up | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | Female | Maxilla | Mandible | Both | Enucleation | Segmental resection | 6 | 1 | 2 | 3 | |||||||
| M | Y | Y | Y | |||||||||||||||
| 2 | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | N | N | N |
| 3 | 33 | 67.34 | 16 | 32.66 | 03 | 06.13 | 45 | 91.83 | 1 | 2.4 | 37 | 75.51 | 12 | 24.49 | – | 1 | – | 1 |
N number of patients, M month, Y year
Table 2.
Distribution of cases according to their occurrence at various sites
| Mandible | Maxilla | ||||
|---|---|---|---|---|---|
| Angle | Ramus | Body | Symphysis | Anterior | Posterior |
| 18 | 20a | 05 | 03 | 02 | 02a |
a01 case had OKC both in maxilla and mandible
Materials and Methods
The study was carried out in Department of Oral and Maxillofacial Surgery, Sw.Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur and various private Hospitals in Nagpur from the period of August 2004 to July 2009 in Central India. The patients ranging from age group 15–60 years. Total 49 patients were diagnosed with OKC on the histological basis, out of that 33 patients were males and 16 patients were female. The patients were thoroughly examined with emphasis on the site and the size of lesion the extent of bony involvement on OPG and CT scan.
Procedure
As per treatment of OKC: All the patients after confirming diagnosis by incisional biopsy and on the basis of radiological involvement on OPG and CT scan and considering unilocularity and multilocularity treatment was planned same for both the variation were classified as:
Initial involvement: OKC which were involving mostly dento-alveolar region of size 1 cm × 2 cm (approx) on OPG (Figs. 1 and 3).
Moderate involvement: OKC involving dento-alveolar bone and basal bone with 1 cm of normal basal bone in mandible/ normal maxillary sinus in maxilla.
Advanced involvement: OKC involving dento-alveolar as well as entire mandibular basal bone/maxillary sinus.
Fig. 1.

Showing Intra-operative OKC
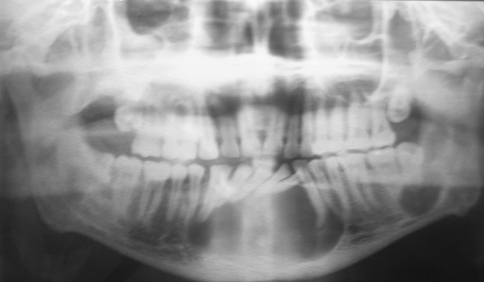
Fig. 3.
Photograph showing OPG of OKC
Initial and moderate involvement of OKC was treated with enucleation and advanced cases were treated with segmental resection (Fig. 2).
Fig. 2.
Showing postoperative specimen after enucleation
Follow up
In 3 years follow-up (after 6 month, after 1 year, after 2 years, after 3 years) recurrence was seen in 2 cases. The recurrence rate in this study is relatively less as compared to other studies as proper screening of OKC was done before treatment. Advanced OKC in 12 cases (24.49%) were treated with segmental resection and initial and moderate OKC cases 37 (75.51%) were treated with enucleation and curettage (Figs. 3 and 4).
Fig. 4.
Photograph showing postoperative healing of OKC
As per gender: Out of 49 cases there were 33(67.34%) males and 16(32.66%) females, there was predominance in males than females.
As per age group: Total 49 patients were diagnosed with presence of OKC. It was seen in 3rd and 4th with mean age of 28 years in male and 31 years in female.
Discussion
The data reported here constitutes one of the largest published studies of odontogenic keratocysts.
The rationale behind this study is to relate the clinical presentation of OKC in the multicentric patients with prevalence, treatment and recurrence with follow-up of 3 years. This incidence is slightly higher (49 out of 2900 biopsies) than in some reports, but very similar to that of Daley [38] who reported 335 cases in 40,000 biopsies. Incidence of OKC also seems to be increasing with time. El-Hajj [41] made the same observation which he attributed to “competence and knowledge of the morphologic characteristics of odontogenic keratocysts have increased among oral pathologists.” It is also noteworthy that the rate of accumulation of cases varies widely in different reports [10–12, 22, 24, 25, 35]. This may reflect regional factors such as race distribution, diet, or environmental exposures. The series of 430 cases from 393 patients seen over a period of 15 years is the most rapid collection rate in the USA and the second most rapid in the world literature other than Woolgar [24–26]. In this study we have small number and period but we have close relationship between the prevalence, treatment and recurrence in various centers of Central India population as per clinical and radiological we have classified and treated as advanced OKC (24.49%) with segmental resection and initial and moderate OKC (75.51%) with enucleation and curettage with no recurrences seen in 3 year follow-up.
Conclusion
The most common age and site of occurrence was relevant with that of previous studies [6, 23]. Although the literature contains many reports regarding management of OKC, debate still exists as to most effective treatment for this lesion. According to Ghali [43] as with any odontogenic lesion initial evaluation include a thorough history and physical examination, radiographic studies and the development of probable differential diagnosis. Depending on size, location and behaviour the clinician should decide on an incisional versus excisional biopsy in patients with multiple OKC. Evaluation for the presence of basal cell naevus syndrome should be undertaken. Larger OKC with possible perforation deserves CT scan in addition to OPG. Treatment of OKC varies from enucleation and curettage to segmental resection. Various factors that should be considered in the selection of the appropriate treatment include size, location, unilocularity or multilocularity on OPG, presence of perforation or soft tissue involvement, age of individual, long term follow-up is suggested because OKC have been known to have late recurrence. Recent factors support emerging molecular evidence that the OKC is more likely to be a benign cystic neoplasm than a simple odontogenic cyst. Our article suggests to bring out the importance of clinical awareness of OKC. It also emphasizes the importance of careful histological examination and the necessity of obtaining biopsy from various areas to prevent misdiagnosis of the large lesions. It may be concluded that the treatment of OKC, the basis of the radiographic classification, gives excellent results with minimum recurrences. Although the number of cases in the study was small, this study suggests by considering multicentric incidence, prevalence of OKC in central India, the population should be screened for OKC. While screening all the parameters should be considered to diagnose and treat the patients for the prevention of morbidity.
References
- 1.Pindborg JJ, Hansen J. Studies on odontogenic cyst epithelium. II. Clinical and roentgenologic aspects of odontogenic keratocysts. Acta Pathol Microbiol Scand. 1963;58:283–294. doi: 10.1111/j.1699-0463.1963.tb01572.x. [DOI] [PubMed] [Google Scholar]
- 2.Hjorting-Hansen E, Andreasen JO, Robinson LH. A study of odontogenic cysts with special reference to location of keratocysts. Br J Oral Surg. 1969;7(1):15–23. doi: 10.1016/S0007-117X(69)80056-9. [DOI] [PubMed] [Google Scholar]
- 3.Rud J, Pindborg JJ. Odontogenic keratocysts: a follow-up study of 21 cases. J Oral Surg. 1969;27(5):323–330. [PubMed] [Google Scholar]
- 4.Panders AK, Hadders HN. Solitary keratocysts of the jaws. J Oral Surg. 1969;27(12):931–938. [PubMed] [Google Scholar]
- 5.Main DM. Epithelial jaw cysts: a clinicopathological reappraisal. Br J Oral Surg. 1970;8(2):114–119. doi: 10.1016/S0007-117X(70)80002-6. [DOI] [PubMed] [Google Scholar]
- 6.Browne RM. The odontogenic keratocyst—clinical aspects. Br Dent J. 1970;128(5):225–231. doi: 10.1038/sj.bdj.4802449. [DOI] [PubMed] [Google Scholar]
- 7.Broume RM. The odontogenic keratocyst—histological features and their correlation with clinical behavior. Br Dent J. 1971;131(6):249–259. doi: 10.1038/sj.bdj.4802732. [DOI] [PubMed] [Google Scholar]
- 8.Keith DA. Macroscopic satellite cyst formation in the odontogenic keratocyst. Report of two cases. Oral Surg Oral Med Oral Pathol. 1973;35(1):21–27. doi: 10.1016/0030-4220(73)90089-3. [DOI] [PubMed] [Google Scholar]
- 9.Robinson HB. Primordial cyst versus keratocyst. Oral Surg Oral Med Oral Pathol. 1975;40(3):362–364. doi: 10.1016/0030-4220(75)90420-X. [DOI] [PubMed] [Google Scholar]
- 10.Sher MR, Stoopack JC. Odontogenic keratocyst. Report of a case. Oral Surg Oral Med Oral Pathol. 1974;37(4):518–525. doi: 10.1016/0030-4220(74)90282-5. [DOI] [PubMed] [Google Scholar]
- 11.Lucas RB (1976) Pathology of tumors of the oral tissues, 3rd edn. Edinburgh, Churchill Livingstone, p 358
- 12.Brannon RB. The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part I. Clinical features. Oral Surg Oral Med Oral Pathol. 1976;42(1):54–72. doi: 10.1016/0030-4220(76)90031-1. [DOI] [PubMed] [Google Scholar]
- 13.Rachanis CC, Shear M. Age-standardized incidence rates of primordial cyst (keratocyst) on the Witwatersrand. Community Dent Oral Epidemiol. 1978;6(6):296–299. doi: 10.1111/j.1600-0528.1978.tb01170.x. [DOI] [PubMed] [Google Scholar]
- 14.Vedtofte P, Praetorius F. Recurrence of the odontogenic keratocyst in relation to clinical and histological features. A 20-year follow-up study of 72 patients. Int J Oral Surg. 1979;8(6):412–420. doi: 10.1016/S0300-9785(79)80079-4. [DOI] [PubMed] [Google Scholar]
- 15.Forssell K. The primordial cyst. A clinical and radiographic study. Proc Finn Dent Soc. 1980;76(3):129–174. [PubMed] [Google Scholar]
- 16.Voorsmit RA, Stoelinga PJ, Haelst UJ. The management of keratocysts. J Maxillofac Surg. 1981;9(4):228–236. doi: 10.1016/S0301-0503(81)80049-5. [DOI] [PubMed] [Google Scholar]
- 17.Wright JM. The odontogenic keratocyst: orthokeratinized variant. Oral Surg Oral Med Oral Pathol. 1981;51(6):609–618. doi: 10.1016/S0030-4220(81)80011-4. [DOI] [PubMed] [Google Scholar]
- 18.Altini M, Cohen M. The follicular primordial cyst—odontogenic keratocyst. Int J Oral Surg. 1982;11(3):175–182. doi: 10.1016/S0300-9785(82)80005-7. [DOI] [PubMed] [Google Scholar]
- 19.Voorsmit RACA (1984) The incredible keratocyst. M.D. Dissertation, the Catholic University of Nijmegen, the Netherlands
- 20.Irvine GH, Bowerman JE. Mandibular keratocysts: surgical management. Br J Oral Maxillofac Surg. 1985;23(3):204–209. doi: 10.1016/0266-4356(85)90091-9. [DOI] [PubMed] [Google Scholar]
- 21.Zachariades N, Papanicolaou S, Triantafyllou D. Odontogenic keratocysts: review of the literature and report of sixteen cases. J Oral Maxillofac Surg. 1985;43(3):177–182. doi: 10.1016/0278-2391(85)90156-9. [DOI] [PubMed] [Google Scholar]
- 22.Lund VJ. Odontogenic keratocyst of the maxilla: a case report. Br J Oral Maxillofac Surg. 1985;23(3):210–215. doi: 10.1016/0266-4356(85)90092-0. [DOI] [PubMed] [Google Scholar]
- 23.Chen CH, Lin CC. Clinical and histopathological study of the odontogenic keratocyst—a follow-up study of 16 cases. Gaoxiong Yi Xue Ke Xue Za Zhi. 1986;2(9):601–607. [PubMed] [Google Scholar]
- 24.Woolgar JA, Rippin JW, Browne RM. A comparative study of the clinical and histological features of recurrent and non-recurrent odontogenic keratocysts. J Oral Pathol. 1987;16(3):124–128. doi: 10.1111/j.1600-0714.1987.tb01478.x. [DOI] [PubMed] [Google Scholar]
- 25.Woolgar JA, Rippin JW, Browne RM. A comparative histological study of odontogenic keratocysts in basal cell nevus syndrome and control patients. J Oral Pathol. 1987;16(2):75–80. doi: 10.1111/j.1600-0714.1987.tb00691.x. [DOI] [PubMed] [Google Scholar]
- 26.Woolgar JA, Rippin JW, Browne RM. The odontogenic keratocyst and its occurrence in the nevoid basal cell carcinoma syndrome. Oral Surg Oral Med Oral Pathol. 1987;64(6):727–730. doi: 10.1016/0030-4220(87)90176-9. [DOI] [PubMed] [Google Scholar]
- 27.Partridge M, Towers JF. The primordial cyst (odontogenic keratocyst): its tumour-like characteristics and behavior. Br J Oral Maxillofac Surg. 1987;25(4):271–279. doi: 10.1016/0266-4356(87)90065-9. [DOI] [PubMed] [Google Scholar]
- 28.Gorlin RJ. Nevoid basal-cell carcinoma syndrome. Medicine (Baltimore) 1987;66(2):98–113. doi: 10.1097/00005792-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Stoelinga PJ, Bronkhorst FB. The incidence, multiple presentation and recurrence of aggressive cysts of the jaws. J Craniomaxillofac Surg. 1988;16(4):184–195. doi: 10.1016/s1010-5182(88)80044-1. [DOI] [PubMed] [Google Scholar]
- 30.Haring JI, Dis ML. Odontogenic keratocysts: a clinical, radiographic, and histopathologic study. Oral Surg Oral Med Oral Pathol. 1988;66(1):145–153. doi: 10.1016/0030-4220(88)90082-5. [DOI] [PubMed] [Google Scholar]
- 31.Forssell K, Forssell H, Kahnberg KE. Recurrence of keratocysts. A long-term follow-up study. Int J Oral Maxillofac Surg. 1988;17(1):25–28. doi: 10.1016/S0901-5027(88)80224-8. [DOI] [PubMed] [Google Scholar]
- 32.Scharffetter K, Balz-Herrmann C, Lagrange W, Koberg W, Mittermayer C. Proliferation kinetics-study of the growth of keratocysts. Morpho-functional explanation for recurrences. J Craniomaxillofac Surg. 1989;17(5):226–233. doi: 10.1016/s1010-5182(89)80074-5. [DOI] [PubMed] [Google Scholar]
- 33.Kakarantza-Angelopoulou E, Nicolatou O. Odontogenic keratocysts: clinicopathologic study of 87 cases. J Oral Maxillofac Surg. 1990;48(6):593–599. doi: 10.1016/S0278-2391(10)80472-0. [DOI] [PubMed] [Google Scholar]
- 34.Brondum N, Jensen VJ. Recurrence of keratocysts and decompression treatment. A long-term follow-up of forty-four cases. Oral Surg Oral Med Oral Pathol. 1991;72(3):265–269. doi: 10.1016/0030-4220(91)90211-T. [DOI] [PubMed] [Google Scholar]
- 35.Gailani MR, Bale SJ, Leffell DJ, DiGiovanna JJ, Peck GL, Poliak S, Drum MA, Pastakia B, McBride OW, Kase R, et al. Developmental defects in Gorlin syndrome related to a putative tumor suppressor gene on chromosome 9. Cell. 1992;69(1):111–117. doi: 10.1016/0092-8674(92)90122-S. [DOI] [PubMed] [Google Scholar]
- 36.Crowley TE, Kaugars GE, Gunsolley JC. Odontogenic keratocysts: a clinical and histologic comparison of the parakeratin and orthokeratin variants. J Oral Maxillofac Surg. 1992;50(1):22–26. doi: 10.1016/0278-2391(92)90187-5. [DOI] [PubMed] [Google Scholar]
- 37.Farndon PA, Morris DJ, Hardy C, McConville CM, Weissenbach J, Kilpatrick MW, Reis A. Analysis of 133 meioses places the genes for nevoid basal cell carcinoma (Gorlin) syndrome and Fanconi anemia group C in a 2.6-cM interval and contributes to the fine map of 9q22.3. Genomics. 1994;23(2):486–489. doi: 10.1006/geno.1994.1528. [DOI] [PubMed] [Google Scholar]
- 38.Daley TD, Wysocki GP, Pringle GA. Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol. 1994;77(3):276–280. doi: 10.1016/0030-4220(94)90299-2. [DOI] [PubMed] [Google Scholar]
- 39.Anand VK, Arrowood JP, Jr, Krolls SO. Odontogenic keratocysts: a study of 50 patients. Laryngoscope. 1995;105(1):14–16. doi: 10.1288/00005537-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Nakamura T, Ishida J, Nakano Y, Ishii T, Fukumoto M, Izumi H, Kaneko K. A study of cysts in the oral region. Cysts of the jaw. J Nihon Univ Sch Dent. 1995;37(1):33–40. doi: 10.2334/josnusd1959.37.33. [DOI] [PubMed] [Google Scholar]
- 41.El-Hajj G, Anneroth G. Odontogenic keratocysts—a retrospective clinical and histologic study. Int J Oral Maxillofac Surg. 1996;25(2):124–129. doi: 10.1016/S0901-5027(96)80057-9. [DOI] [PubMed] [Google Scholar]
- 42.Ong Siewjin, Chong (2000) J Contemp Dent Pract 1(2), winter issue
- 43.Ghali GE, Connor MS. Surgical management of the odontogenic keratocyst. Oral Maxillofac Surg Clin North Am. 2003;15(3):383–392. doi: 10.1016/S1042-3699(03)00042-6. [DOI] [PubMed] [Google Scholar]
- 44.Barnes L, Eveson JW, Reeichart P, Sidransky D (2005) Pathology and genetic of head and neck tumours. IARC Press, Lyon; WHO classification of Tumours series
- 45.Maurette PE, Jorge J, Moraes M. Conservative treatment protocol of odontogenic keratocyst: a preliminary study. J Oral Maxillofac Surg. 2006;64(3):379–383. doi: 10.1016/j.joms.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 46.Madras J, Lapointe H (2008) Keratocystic odontogenic tumour: reclassification of the odontogenic keratocyst from cyst to tumour. J Can Dent Assoc 74(2):165–165h [PubMed]