Abstract
The EGFR signaling pathway is involved in carcinogenesis at multiple sites, particularly colorectal cancer, and is a target of colorectal cancer chemotherapy. EGFR signaling is linked to pro-carcinogenic mechanisms, including cell proliferation, survival, angiogenesis, and more recently prostaglandin synthesis. Genetic variability in this pathway has not yet been studied in relation to colorectal carcinogenesis. In three case-control studies of colorectal adenoma (n=485 cases/578 controls), colon cancer (n=1424 cases/1780 controls) and rectal cancer (n=583 cases/775 controls), we investigated associations between candidate SNPs, tagSNPs and haplotypes in EGFR signaling (EGFR, Src, and HER2) and risk. We also examined associations with tumor subtypes: TP53 and KRAS2 mutations, CpG island methylator phenotype, and microsatellite instability. All three studies were genotyped using an identical Illumina GoldenGate assay, allowing thorough investigation of genetic variability across stages and locations of colorectal neoplasia. The EGFR tagSNP 142572T>C (rs3752651) CC genotype was associated with a suggested increased risk for both colon (OR: 1.40; 95% CI: 1.00-1.96; p-trend=0.04) and rectal cancer (OR: 1.39; 95% CI: 0.81-2.41; p-trend=0.65). In tumor subtype analyses, the association was limited to TP53-mutated colon tumors. Using the Chatterjee 1 df Tukey test to assess gene-gene interactions, we observed a statistically significant (p<0.01) interaction between SNPs in EGFR and Src for colorectal adenoma risk. The association with EGFR 142572 should be investigated in additional studies and the significant gene-gene interaction between EGFR and Src in relation to adenoma risk suggests that these two genes are jointly affecting early stages in colorectal carcinogenesis and requires further follow-up.
Keywords: EGFR, colorectal cancer, colorectal polyps, genetics
Introduction
The epidermal growth factor receptor (EGFR; also known as ERBB1 and HER1) is a membrane-bound tyrosine kinase that contributes to signaling cascades with multiple pro-carcinogenic effects including cell proliferation, motility, adhesion, invasion, cell survival, and angiogenesis [1]. EGFR overexpression has been detected in several human cancers, including breast, lung, ovarian, prostate, and pancreatic cancers [reviewed in [1]]; EGFR overexpression is observed in aberrant crypt foci [2], colorectal adenomas [3, 4], and colorectal cancer [3-5], and correlates with progression and metastasis [6, 7]. Several therapies targeting EGFR have been investigated and approved by the FDA for treatment of metastatic colorectal cancer, including cetuximab and panitumumab, (monoclonal antibodies against EGFR), and ge-fitinib and erlotinib, (tyrosine kinase inhibitors) [reviewed in [8]]. Treatment of mice with EGFR inhibitors, such as gefitinib, results in decreased polyp formation [9-11], indicating that overexpression of EGFR may be an early event in colon carcinogenesis. In addition, egfr knockdown mice have shown a 10-fold reduction in adenomas [9]. Taken together, these studies indicate that EGFR plays a key role in colorectal cancer development and progression, and that inhibition of EGFR may be a promising treatment for colorectal neoplasia.
HER2 (also known as ERBB2 or neu) is structurally and functionally similar to EGFR [12]. HER2 overexpression or gene amplification has been observed in multiple cancer types, including breast [13], ovarian [14], and gastric tumors [15]. As with EGFR, HER2 overexpression has been observed in aberrant crypt foci in human colon [2]. However, studies of HER2 expression in colorectal cancer have been mixed, with some, but not all studies reporting HER2 RNA or protein overexpression [reviewed in [16]].
Src is a non-receptor tyrosine kinase involved in the EGFR signaling cascade [17]; among many downstream effects, Src signaling affects cell growth and differentiation in the intestine [18]. Src kinase activity or protein levels are elevated in several cancers, including colon, breast, lung, skin, ovarian, endometrial, and head and neck malignancies [19] and were associated with tumor recurrence in one study [20]. Src kinase activity is also elevated in colorectal adenomas [21] and in ulcerative colitis [22], indicating that Src may play a role in the early stages of colorectal cancer development.
Although polymorphisms and point mutations in EGFR have been studied for survival in many cancer types [23-29] and HER2 has been investigated for its role in breast cancer risk [30-35], no study has yet assessed the role of genetic variability in EGFR signaling in relation to risk of colorectal neoplasia, nor specifically in tumor subtypes. Using a linkage disequilibrium (LD)-based tagSNP approach, we have comprehensively assessed genetic variation in EGFR, Src, and HER2 in three independent case-control studies of colorectal adenoma or cancer, including tumors with specific alterations (TP53 or KRAS2 mutations, CpG island methylator phenotype (CIMP), and miscrosattelite instability (MSI)) using identical genotyping methods. In addition, we explored potential gene-gene interactions using the Chatterjee 1df Tukey test. Thus, we were able to thoroughly evaluate the roles of genetic variability in EGFR signaling throughout the stages of colorectal carcinogenesis, as well as in different tumor locations.
Materials and methods
Study populations
Adenoma study
Colorectal adenoma cases (n=485) and polyp-free controls (n=578) were recruited through a large multiclinic gastroenterological practice in the Twin Cities area of Minnesota from April 1991-April 1994, as previously described [36]. All participants received a colonoscopy. Cases were diagnosed with a first colonoscopy; controls were polyp-free. Eligibility criteria have been described elsewhere [36]; participants were aged 30-74 years, English-speaking residents of the Twin Cities metropolitan area with no known genetic syndrome associated with increased risk of colon neoplasia and no individual history of cancer (except non-melanoma skin cancer), prior colorectal polyps, or inflammatory bowel disease. The participation rate for all colonoscoped patients was 68%.
Colon and rectal cancer studies
Colon and rectal cancer cases and controls were recruited from the northern California Kaiser Permanente Medical Care Program (KPMCP), Utah, and the Twin Cities metropolitan area of Minnesota (colon cancer only), as described previously [37]. Two study populations are included in these analyses. The first study includes cases (n=1424) and controls (n=1780) from a population-based case-control study of colon cancer recruited between October 1, 1991 and September 30, 1994 [37]. The second study, with identical data collection, includes cases with cancer of the rectosigmoid junction or rectum (n=583) and controls (n=775) who were identified between May 1997 and May 2001 in Utah and KPMCP [38]. Eligible cases were between 30 and 79 years old at time of diagnosis, English speaking, mentally competent to complete the interview, had no previous history of colorectal cancer, and no known (as indicated on the pathology report) familial adenomatous polyposis, ulcerative colitis, or Crohn's disease.
Controls were matched to cases by sex and by 5-year age group. At KPMCP, controls were randomly selected from membership lists; in Utah, controls 65 years and older were randomly selected from the Health Care Financing Administration lists and controls younger than 65 years were randomly selected from driver's license lists. In Minnesota (colon cancer only), controls were selected from driver's license and state-ID lists. For the colon study, 75.6% of contacted cases and 63.7% of contacted controls were interviewed; for the rectal study, 73.2% of contacted cases and 68.8% of contacted controls were interviewed. Response proportions (the number interviewed over all persons identified) were 61.4% for colon cancer cases and 52.5% for controls selected for the colon cancer study and 65.2% of cases and 65.3% of controls for the rectal cancer study.
Tumor markers
Tumor DNA was obtained from paraffin-embedded tissue as described [39]. As described in previous publications [40-43], tumors were characterized by their genetic profile that included: sequence data for exons 5 through 8, the mutation hotspots of the TP53 gene; sequence data for KRAS2 codons 12 and 13; microsatellite instability (MSI) status based on BAT26, TGFBR2, and a panel of 10 tetranucleotide repeats; methylation specific PCR of sodium-bisulfite-modified DNA for five CpG Island markers, CDKN2A, MLH1 and methylated in tumors (MINT) 1, 2 and 31. Tumors with two or more methylated CpG islands were scored as CIMP+. At the time we undertook the methylation-status analysis, there was no consensus CpG-island panel or method of detection to determine CIMP. However, we have used our panel to demonstrate relationships between CIMP and numerous clinicopathologic variables [40, 44], indeed, this work has supported the legitimacy of the CIMP concept in colorectal cancer [45, 46].
TagSNP selection
An identical tagSNP selection and genotyping procedure was used in all three studies. The coding regions and 2 kB beyond the 5’ and 3’ ends of EGFR and HER2 were resequenced in 23 individuals of European descent by the Innate Immunity Program for Genomic Applications (http://www.pharmgat.org/IIPGA2/index_html) and the UW-NIEHS Environmental Genome Project (http://egp.gs.washington.edu respectively). TagSNPs in EGFR and HER2 were selected from these resequenced individuals using the LD Select algorithm developed by Carlson and colleagues [47], with a cutoff minor allele frequency (MAF) of 4% (i.e., any variant that occurred twice) and an r2 value of 0.90. Src has not yet been resequenced by any groups, so tagSNPs were selected from polymorphisms genotyped in HapMap's CEPH population, using the same criteria as described for EGFR above. This resulted in the selection of 38 tagSNPs in EGFR, 5 tagSNPs in HER2, and 17 in Src, which were estimated by the Genome Variation Server http://gvs.gs.washington.edu/GVS/index.jsp) to cover ≥ 85% of the common (≥4% MAF) variation at these loci (see Supplemental Table S1 for a list of the polymorphisms selected). A total of 55 SNPs were successfully converted to the Illumina™ GoldenGate genotyping platform. All polymorphisms that failed to convert were “singleton” SNPs, not tagging for any other polymorphisms; we did not pursue these further.
Genotyping and QC
An identical set of SNPs were genotyped in all three studies. All SNPs were genotyped using the Illumina™ GoldenGate bead-based genotyping technology at the Translational Genomics Institute (TGen, Phoenix, Arizona). Intraplate and interplate replicates at a rate of ∼5% were included on all plates and in all batches. Blinded duplicates were also included on all plates as another QC measure. Genotype data from 30 CEPH trios (Coriell Cell Repository, Camden, NJ) that were genotyped by the HapMap project were used to confirm reliability and reproducibility of the genotyping. Genotypes were excluded from analyses by TGen if any of the following were true: GenTrain Score <0.4, 10%GC Score <0.25, AB T Dev >0.1239, Call Frequency <0.85, Replicate Errors >2, P-P-C Errors >2. Additionally, further exclusions were made for SNPs that had <85% concordance with blinded or non-blinded duplicates (see Supplemental Table S1) and for Hardy-Weinberg Equilibrium p-values <0.0001. Six SNPs failed in all three study populations, mainly due to low call rates or Hardy-Weinberg disequilibrium; four additional SNPs failed in at least one study, and two EGFR tagSNPs were in high LD (r2>0.90), leaving 44 SNPs in three genes included in the analyses presented here. Of these, one (EGFR -216G>T), was a candidate SNP.
Questionnaire data
Adenoma study
Information on lifestyle factors and diet, anthropometry, demographics, and medical information, including family history of cancer and polyps, were obtained by questionnaire as described previously [36].
Colon and rectal cancer studies
Data collection has been described previously [37, 38]. The referent period was the calendar year 2 years prior to date of diagnosis or interview. Questionnaire data included information on physical activity, diet, medication use, family history of cancer, smoking history, and recalled height and weight 2 years prior to interview.
Statistical analysis
Single SNP analyses
Unconditional logistic regression was used to estimate odds ratios (ORs) and corresponding 95% confidence intervals (CIs) for the associations between genotypes in EGFR, HER2, and Src and risk of colorectal adenoma or cancer. Most genotypes were modeled using indicator variables for the heterozygous and the homozygous variant genotypes (unrestricted or co-dominant model). If fewer than ten cases or controls had the homozygous variant genotype, we grouped the homozygous variant genotypes with the heterozygous genotypes for analysis (dominant model). Due to racial differences in genotype frequencies, our analyses were restricted to Caucasian individuals >82% in all three studies). Likelihood ratio tests were used to assess the association of each SNP with disease risk. To obtain tests for trend, the genotypes were treated as continuous variables.
Pooled analyses of the two cancer studies were conducted using a categorical variable that indicated both which study and the study site, because the Minnesota site contributed only colon cancer cases.
SNP-SNP interactions were explored only for genes that showed statistical significance in gene-gene interactions from Chatterjee testing (see below).
All models were adjusted for age and sex; the analyses of colon and rectal cancers were additionally adjusted for study site. All SNP analyses were carried out using SAS v.9. P-values < 0.05 are considered statistically significant. Multiple comparison adjusted p-values were also obtained, taking into account the correlation between tagSNPs using the method by Conneely and Boehnke [48]. To ease the presentation for the tables, we only present p-values that are not adjusted for multiple comparison. Adjusted p-values indicated by adj.p or adj.p trend are provided in the text.
Haplotype and principal components analyses
Haplotype analysis was conducted using a modified version of HaploStats (Version 1.3.8) which allows adjustment for potential confounders in R (Version 2.7.1). All haplotypes predicted to occur with more than 5% frequency among controls were analyzed separately. Haplotypes with frequency < 5% were grouped together for analyses. The most common haplotype among the controls was used as the referent group. We used the score test to evaluate whether a haplotype was associated with disease risk. For principal components analysis (PCA) [49], we chose the number of principal components that explained at least 80% of the variance in a gene and performed logistic regression using those components. Gene-level significance was determined using a likelihood-ratio test, comparing a model that contained the principal components and one that did not.
Tumor marker analyses
Tumors were defined by specific alterations detected; any TP53 mutation, any KRAS2 mutation, or CIMP+ defined as at least 2 of 5 markers methylated. As the proportion of MSI+ tumors in the rectal cases was <3% [50], there was insufficient power to examine rectal MSI. Population-based controls were used to assess associations for the population overall, while examining multiple outcomes defined by tumor status. To compare specific types of mutations to controls while adjusting for the other tumor mutations simultaneously in cases, a generalized estimating equation (GEE) with a multinomial outcome was used as case subjects could contribute to more than one outcome observation depending upon the number of mutations or alterations (TP53, KRAS2, CIMP+, and additionally MSI+ for colon cases) detected in an individual's tumor DNA expressed [51]. The GEE accounts for correlation introduced by including subjects multiple times and was implemented in SAS using the GENMOD procedure as described by Kuss and McLerran [52]. All GEE models were adjusted for sex, age at diagnosis or selection, and study center. A co-dominant model with three genotype categories was analyzed with molecular subtypes when minor allele frequencies provided sufficient power to examine the minor-allele homozygous genotype; otherwise, a dominant model was assumed. A recessive model was analyzed in addition to the co-dominant, when indicated by co-dominant ORs. P for linear trend was assessed using three ordered genotype categories and comparing the likelihood ratio of a model with the genotype variable (as continuous) to the likelihood ratio of a model without the variable using a chi-squared test with 1 degree of freedom.
Gene-gene interaction
We evaluated gene-gene interactions using the Tukey 1 degree of freedom (1df) interaction test proposed by Chatterjee et al [53]. The 1df Tukey test is a method that tests for gene-gene interactions with multiple SNPs within each gene in one model, using a 1df test, rather than a test with many more degrees of freedom or multiple 1df tests of interaction that require correction for multiple testing. All gene-gene interaction analyses were conducted in R (version 2.7.1).
Results
Characteristics of the study populations are shown for the genotyped subset in Table 1. Briefly, the full study populations were mostly Caucasian (97.2% for the adenoma study; 91.3% for the colon cancer study; and 82.3% for the rectal cancer study - data not shown); adenoma cases tended to be older and were more likely to be male than controls; the cancer case-control studies were frequency-matched on age and sex.
Table 1.
Characteristics of the three study populationsa
| Colorectal adenoma study | Colon cancer study | Rectal cancer study | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cases (N=485) | Controls (N=578) | p-value | Cases (N = 1424) | Controls (N=1780) | p-value | Cases (N=583) | Controls (N=775) | p-value | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Age | 58 (9.6) | 52.9 (11.0) | <0.01 | 65.2 (9.7) | 65.1(10.3) | NAc | 62.3 (10.8) | 62.6(10.5) | NAc |
| Caloric Intake (kcal) | 2101.6 (760.0) | 2019.8 (733.1) | 0.07 | 2427.9 (1116.6) | 2306.5 (1017.4) | <0.01 | 2702.5 (1294.7) | 2592.7 (1203.7) | 0.11 |
| Dietary Fiber Intake (gm) | 21.8 (9.4) | 21.8 (9.6) | 0.95 | 24.8 (11.8) | 24.9 (11.3) | 0.84 | 26.0 (13.0) | 26.7 (13.0) | 0.35 |
| Location | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Proximal | 104 (21.6) | NA | NA | 688 (49.6) | NA | NA | NA | NA | NA |
| Distal | 300 (62.4) | NA | 700 (50.4) | NA | NA | NA | |||
| Rectal | 77 (16.0) | NA | NA | NA | 583 | 775 | |||
| Sex | |||||||||
| Male | 304 (62.7) | 227 (39.3) | <0.01 | 797 (56.0) | 946 (53.2) | NAc | 346 (59.4) | 428 (55.2) | NAc |
| Female | 181(37.3) | 351(60.7) | 627 (44.0) | 834 (46.9) | 237 (40.7) | 347 (44.8) | |||
| Study Site | |||||||||
| Kaiser Northern California | NA | NA | NA | 617 (43.3) | 647 (36.4) | <0.01 | 349 (59.9) | 449 (57.9) | 0.48 |
| Minnesota | 485 (100) | 578 (100) | 565 (39.7) | 791 (44.4) | NA | NA | |||
| Utah | NA | NA | 242 (17.0) | 342 (19.2) | 234(40.1) | 326 (40.1) | |||
| Regular Use of NSAIDs (Ever vs. Never) | |||||||||
| Yes | 180 (37.1) | 257 (44.5) | 0.02 | 562 (39.5) | 865 (48.6) | <0.01 | 263(45.1) | 417 (53.8) | <0.01 |
| No | 305 (62.9) | 321(55.6) | 862 (60.5) | 915 (51.4) | 320 (54.9) | 358 (46.2) | |||
| Smoking in pack-years (amt per day)b | |||||||||
| 0 | 163 (34.4) | 276 (49.0) | <0.01 | 840 (47.3) | 581 (41.0) | <0.01 | 271(46.5) | 401(51.7) | 0.05 |
| 1-25 (<20) | 152 (32.1) | 171(30.4) | 336 (18.9) | 250(17.6) | 106 (18.2) | 133(17.2) | |||
| >25 (21+) | 159 (33.5) | 116 (20.6) | 599 (33.8) | 586 (41.4) | 206 (35.3) | 241 (31.1) | |||
| Post-menopausal Hormone Use (Women only) | |||||||||
| Yes | 71(40.6) | 181 (53.2) | 0.01 | 130 (23.9) | 221 (31.0) | 0.006 | 110(56.7) | 132 (45.2) | 0.01 |
| No | 104 (59.4) | 159 (46.8) | 414 (76.1) | 493 (69.1) | 84 (43.3) | 160 (54.8) | |||
Numbers may not total to 100% due to rounding and missing values
For adenoma and rectal cancers, pack-years are reported. For colon cancer, number of cigarettes per day is reported.
NA - this was a matching factor.
Genotype associations
Multiple single SNP associations were observed in one or more of the colorectal carcinogenesis studies. However, after adjusting for multiple comparisons, none of the associations remained statistically significant. Below, we focus on those results that show similar associations across multiple study populations in direction and magnitude, which may indicate a possible association of the SNPs with disease risk. Associations with all analyzed SNPs can be seen in Supplemental Tables S2-S4.
In both the colon and rectal cancer populations, the EGFR 142572T>C (rs3752651) CC genotype was associated with an approximate 40% increase in risk compared to the TT genotype (colon OR: 1.40; 95% CI: 1.00-1.96; p-trend=0.04; adj. p-trend=0.55; rectal OR: 1.39; 95% CI: 0.81-2.41; p-trend=0.65; adj. p-trend=1.00). When the cancer populations were pooled, the association was also statistically significant (OR: 1.39; 95% CI: 1.05-1.86; p-trend=0.13; adj. p-trend=0.90; Table 2). However, the significant association did not remain after adjustment for multiple testing.
Table 2.
Genetic variability in selected EGFR and Src SNPs and risk of colorectal neoplasiaa
| Colorectal Adenomab | Colon Cancerc | Rectal cancerc | Colorectal cancerd | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gene | SNPd | Cases/Controls | OR | 95%CI | p | p-trend | Cases/Controls | OR | 95%CI | p | p-trend | Cases/Controls | OR | 95%CI | p | p-trend | Cases/Controls | OR | 95%CI | p | p-trend |
| EGFR | rs759171 (-759C<A) | ||||||||||||||||||||
| CC | 353/411 | 1.00 | (ref.) | 1021/1315 | 1.00 | (ref.) | 407/579 | 1.00 | (ref.) | 1428/1894 | 1.00 | (ref.) | |||||||||
| CA | 117/149 | 0.95 | (0.70-1.27) | 375/427 | 1.12 | (0.96-1.32) | 163/184 | 1.26 | (0.99-1.61) | 538/611 | 1.16 | (1.02-1.33) | |||||||||
| AA | 10/18 | 0.62 | (0.27-1.41) | 0.50 | 0.36 | 28/36 | 0.98 | (0.59-1.62) | 0.37 | 0.26 | 12/11 | 1.54 | (0.67-3.53) | 0.12 | 0.04 | 40/47 | 1.10 | (0.72-1.70) | 0.09 | 0.04 | |
| CA/AA | 127/168 | 0.91 | (0.68-1.21) | 0.51 | NA | 403/463 | 1.11 | (0.95- | 0.19 | NA | 175/195 | 1.28 | (1.00-1.63) | 0.05 | NA | 578/658 | 1.16 | (1.02-1.32) | 0.03 | NA | |
| rs759162 (141202T>C) | |||||||||||||||||||||
| TT | 242/307 | 1.00 | (ref.) | 764/900 | 1.00 | (ref.) | 308/426 | 1.00 | (ref.) | 1072/1326 | 1.00 | (ref.) | |||||||||
| TC | 200/231 | 1.06 | (0.81-1.39) | 550/706 | 0.92 | (0.80-1.07) | 235/290 | 1.13 | (0.90-1.41) | 785/996 | 0.98 | (0.87-1.11) | |||||||||
| CC | 40/40 | 1.34 | (0.82-2.20) | 0.51 | 0.29 | 105/171 | 0.73 | (0.56-0.95) | 0.05 | 0.02 | 40/59 | 0.94 | (0.61-1.44) | 0.51 | 0.67 | 145/230 | 0.78 | (0.63-0.98) | 0.09 | 0.10 | |
| rs3752651 (142572T>C) | |||||||||||||||||||||
| TT | 313/358 | 1.00 | (ref.) | 900/1178 | 1.00 | (ref.) | 369/468 | 1.00 | (ref.) | 1269/1646 | 1.00 | (ref.) | |||||||||
| TC | 150/198 | 0.90 | (0.68-1.19) | 446/529 | 1.11 | (0.95-1.29) | 183/278 | 0.83 | (0.66-1.05) | 629/807 | 1.01 | (0.89-1.15) | |||||||||
| CC | 19/21 | 1.04 | (0.53-2.05) | 0.75 | 0.63 | 75/70 | 1.40 | (1.00-1.96) | 0.09 | 0.04 | 29/26 | 1.39 | (0.81-2.41) | 0.11 | 0.65 | 104/96 | 1.39 | (1.05-1.86) | 0.08 | 0.13 | |
| rs10277413(151493T>G) | |||||||||||||||||||||
| TT | 211/232 | 1.00 | (ref.) | 626/792 | 1.00 | (ref.) | 247/365 | 1.00 | (ref.) | 873/1157 | 1.00 | (ref.) | |||||||||
| TG | 221/271 | 0.86 | (0.66-1.14) | 611/775 | 0.98 | (0.85-1 14) | 272/313 | 1.28 | (1.02-1.62) | 883/1088 | 1.06 | (0.94-1.21) | |||||||||
| GG | 49/75 | 0.64 | (0.41-0.98) | 0.11 | 0.04 | 182/206 | 1.10 | (0.88-1.38) | 0.62 | 0.59 | 61/94 | 0.97 | (0.67-1.39) | 0.07 | 0.40 | 243/300 | 1.06 | (0.88-1.28) | 0.59 | 0.37 | |
| rsl7290559 (172479C>T) | |||||||||||||||||||||
| CC | 442/546 | 1.00 | (ref.) | 1344/1655 | 1.00 | (ref.) | 552/720 | 1.00 | (ref.) | 1896/2375 | 1.00 | (ref.) | |||||||||
| CT/TT | 35/27 | 1.55 | (0.90-2.66) | 0.11 | NA | 67/108 | 0.77 | (0.56-1.05) | 0.10 | NA | 27/43 | 0.82 | (0.50-1.35) | 0.74 | NA | 94/151 | 0.78 | (0.60-1.02) | 0.07 | NA | |
| rs17337331(172977C>G) | |||||||||||||||||||||
| CC | 277/338 | 1.00 | (ref.) | 833/1003 | 1.00 | (ref.) | 354/429 | 1.00 | (ref.) | 1187/1432 | 1.00 | (ref.) | |||||||||
| CG | 170/208 | 1.00 | (0.76-1.31) | 473/648 | 0.88 | (0.76-1.02) | 201/306 | 0.80 | (0.64-1.01) | 674/954 | 0.86 | (0.75-0.97) | |||||||||
| GG | 30/27 | 1.30 | (0.73-2.31) | 0.65 | 0.57 | 80/93 | 1.03 | (0.75-1.41) | 0.23 | 0.33 | 27/39 | 0.84 | (0.51-1.40) | 0.15 | 0.08 | 107/132 | 0.98 | (0.75-1.27) | 0.05 | 0.08 | |
| Src | rs6017944 (-34985A>G) | ||||||||||||||||||||
| AA | 284/350 | 1.00 | (ref.) | 831/992 | 1.00 | (ref.) | 346/425 | 1.00 | (ref.) | 1177/1417 | 1.00 | (ref.) | |||||||||
| AG | 171/191 | 1.16 | (0.88-1.52) | 494/660 | 0.88 | (0.76-1.02) | 204/302 | 0.82 | (0.65-1.03) | 698/962 | 0.86 | (0.76-0.98) | |||||||||
| GG | 26/37 | 0.90 | (0.52-1.58) | 0.49 | 0.65 | 90/116 | 0.94 | (0.70-1.25) | 0.24 | 0.18 | 31/45 | 0.85 | (0.53-1.38) | 0.22 | 0.12 | 121/161 | 0.91 | (0.71-1.17) | 0.06 | 0.05 | |
Only SNPs with p<0.10 in Table 2. The associations with all SNPs can be seen in Supplemental Tables S2-4
Adjusted for age and sex
Adjusted for age, sex, and study center
Pooled analysis of the colon and rectal cancer studies, adjusted for age, sex, study center, and study
The heterozygous and homozygous variant genotype groups are combined if the homozygous variant group had < 5 study participants.
For rectal cancer, EGFR -759C>A (rs759171) was associated with an increased risk (het OR: 1.26; 95%CI: 0.99-1.61; hzv OR: 1.54; 95% CI: 0.67-3.53; p-trend=0.04; adj. p-trend=0.55). A similarly increased risk of colon cancer was suggested among the heterozygous genotypes. When both cancer populations were pooled, results were statistically significant, but only prior to multiple test correction (OR: 1.16; 95% CI: 1.02-1.32, p=0.03 adj. p=0.53).
In Src, we observed a consistently decreased risk for -34985A>G (rs6017944) (Table 2). The pooled analysis of colon and rectal cancers yielded het OR: 0.86; 95% CI: 0.76-0.98; hzv OR: 0.91; 95% CI: 0.71-1.17; p=0.06, p-trend=0.05; adj. p=0.47, adj. p-trend=0.40). Associations with adenoma risk appeared to be often opposite to those for colon and rectal cancer, for example for EGFR 172479C>T (rs17290559) and 141202T>C (rs759162). There were no statistically significant associations with the candidate SNP Arg521Lys (rs2227983) in EGFR, nor with the candidate and tagSNPs in HER2 (Supplemental Table S3).
Haplotype and principal components analysis (PCA) associations
Haplotype associations are shown in Supplemental Tables S5-S7. Among colon cancers, Src block 2 was associated with colon cancer risk. This haplotype block was comprised of -33208C>G (rs12106024) and -29667A>G (rs747182), neither of which was independently associated with colon cancer risk. Compared to the most common haplotype (CA), the GA haplotype was associated with a statistically significant decrease in colon cancer risk (OR: 0.81; 95% CI: 0.69-0.96); whereas the GG haplotype was not associated with risk (OR: 1.03; 95% CI: 0.90-1.19). No statistically significant haplotype associations were observed for colorectal adenomas and rectal cancers, nor were there significant associations using PCA (data not shown).
Associations with tumor subtypes
We evaluated whether polymorphisms in EGFR, Src, and HER2 were associated with specific colon and rectal cancer subtypes (MSI+, CIMP+, TP53 mutation, or KRAS2 mutation). Because these were exploratory analyses, we did not adjust for multiple comparisons. In the colon cancers, we observed that four EGFR SNPs and one Src SNP was associated with risk of colon cancer with a TP53 mutation (Table 3A). Of note, the increased risk of colon cancer for EGFR 142572T>C (rs3752651), which was associated with risk of both colon and rectal cancers above, was only observed for TP53-mutated colon cancers (het OR: 1.27; 95% CI: 1.04-1.55; hzv OR: 1.35; 95% CI: 0.87-2.08; p=0.02).
Table 3A.
Associations between selected SNPs and risk of colon cancer molecular subtypesa
| Controls | TP53 mutation | KRAS mutation | CIMP+ | MSI + | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gene | SNP | N | N | OR | (95% CI) | P | N | OR | (95% CI) | P | N | OR | (95% CI) | P | N | OR | (95% CI) | P |
| EGFR | 141202 T>C(rs759162) | |||||||||||||||||
| TT | 898 | 253 | 1.00 | (ref.) | 156 | 1.00 | (ref.;) | 116 | 1.00 | (ref.) | 83 | 1.00 | (ref.) | |||||
| TC | 705 | 181 | 0.89 | (0.73-1.07) | 129 | 1.05 | (0.83-1.32) | 115 | 1.22 | (0.95-1.56) | 74 | 1.10 | (0.81-1.50) | |||||
| CC | 170 | 28 | 0.64 | (0.43-0.94) | 0.03 | 22 | 0.87 | (0.56-1.36) | 0.63 | 16 | 0.84 | (0.51-1.39) | 0.85 | 12 | 0.85 | (0.47-1.53) | 0.77 | |
| 142572 T>C(rs3752651) | ||||||||||||||||||
| TT | 1176 | 280 | 1.00 | (ref.) | 199 | 1.00 | (ref.;) | 167 | 1.00 | (ref.) | 112 | 1.00 | (ref.) | |||||
| TC | 528 | 158 | 1.27 | (1.04-1.55) | 85 | 0.91 | (0.71-1.18) | 68 | 0.87 | (0.67-1.15) | 52 | 1.02 | (0.74-1.41) | |||||
| CC | 69 | 25 | 1.35 | (0.87-2.08) | 0.02 | 22 | 1.70 | (1.09-2.65) | 0.22 | 11 | 0.98 | (0.53-1.80) | 0.86 | 6 | 0.80 | (0.35-1.83) | 0.82 | |
| 154784 G>A(rsl7337107) | ||||||||||||||||||
| GG | 1624 | 407 | 1.00 | (ref.) | 273 | 1.00 | (ref.;) | 225 | 1.00 | (ref.) | 154 | 1.00 | (ref.) | |||||
| GA or AA | 145 | 53 | 1.38 | (1.03-1.84) | 0.03 | 33 | 1.25 | (0.88-1.77) | 0.12 | 22 | 0.99 | (0.65-1.51) | 0.71 | 15 | 0.99 | (0.59-1.67) | 0.80 | |
| 161260 G>A(rsl2532468) | ||||||||||||||||||
| GG | 596 | 177 | 1.00 | (ref.) | 104 | 1.00 | (ref.) | 76 | 1.00 | (ref.) | 58 | 1.00 | (ref.) | |||||
| GA | 853 | 220 | 0.86 | (0.70-1.06) | 143 | 0.98 | (0.76-1.26) | 133 | 1.23 | (0.94-1.61) | 83 | 1.00 | (0.71-1.39) | |||||
| AA | 316 | 65 | 0.70 | (0.53-0.94) | 0.03 | 58 | 1.16 | (0.84-1.60) | 0.76 | 37 | 0.97 | (0.67-1.42) | 0.91 | 27 | 0.92 | (0.59-1.44) | 0.61 | |
| Src | -25903 G>A(rs6017996) | |||||||||||||||||
| GG | 1293 | 312 | 1.00 | (ref.) | 206 | 1.00 | (ref.) | 176 | 1.00 | (ref.) | 133 | 1.00 | (ref.) | |||||
| GA | 440 | 134 | 1.22 | (0.99-1.49) | 92 | 1.25 | (0.98-1.59) | 65 | 1.02 | (0.78-1.34) | 34 | 0.71 | (0.49-1.02) | |||||
| AA | 38 | 15 | 1.61 | (0.96-2.72) | 0.03 | 6 | 0.86 | (0.38-1.93) | 0.16 | 6 | 1.19 | (0.54-2.63) | 0.51 | 2 | 0.51 | (0.12-2.12) | 0.13 | |
| 9597 A>G (rs6018256) | ||||||||||||||||||
| AA | 1483 | 376 | 1.00 | (ref.) | 244 | 1.00 | (ref.) | 207 | 1.00 | (ref.) | 153 | 1.00 | (ref.) | |||||
| AG or GG | 291 | 88 | 1.19 | (0.94-1.51) | 0.19 | 64 | 1.33 | (1.01-1.76) | 0.06 | 40 | 0.93 | (0.67-1.29) | 0.96 | 17 | 0.52 | (0.32-0.86) | 0.02 | |
| 9982 A>G (rs6018257) | ||||||||||||||||||
| AA | 1379 | 353 | 1.00 | (ref.) | 221 | 1.00 | (ref.) | 192 | 1.00 | (ref.) | 145 | 1.00 | (ref.) | |||||
| AG | 357 | 100 | 1.10 | (0.88-1.37) | 76 | 1.35 | (1.04-1.75) | 49 | 0.95 | (0.70-1.28) | 21 | 0.53 | (0.34-0.83) | |||||
| GG | 21 | 6 | 1.26 | (0.55-2.87) | 0.45 | 4 | 1.33 | (0.50-3.55) | 0.06 | 1 | 0.33 | (0.05-2.12) | 0.58 | 1 | 0.43 | (0.06-2.89) | 0.01 | |
Adjusted for age, sex, and study center.
In rectal cancer, in which MSI+ tumors are too rare to analyze, we observed a striking association between EGFR -759C>A (rs759171) and risk of KRAS-mutated rectal cancer (Table 3B; p=0.0002). The CA genotype was associated with a 73% increased risk (95% CI: 1.20-2.50) and the AA genotype was associated with an almost 4-fold increase in risk (OR: 1.69-7.82). This SNP was observed with risk of rectal cancer overall (as described above), but the associations for TP53-mutated or CIMP+ rectal cancers were not significant. Although no associations were observed between HER2 SNPs and rectal tumor markers overall, HER2 -658C>A (rs4252596) was associated with a ∼50% decreased risk of TP53 or KRAS2 tumor mutation in women and an interaction term for sex was nominally significant at the 0.01 level (data not shown).
Table 3B.
Associations between selected SNPs and risk of rectal cancer molecular subtypesa
| Controls | TP53 mutation | KRAS mutation | CIMP+ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gene | SNP | N | N | OR | (95% CI) | p | N | OR | (95% CI) | p | N | OR | (95% CI) | p |
| EGFR | -759C>A (rs759171) | |||||||||||||
| CC | 579 | 148 | 1.00 | (ref.) | 81 | 1.00 | (ref.) | 34 | 1.00 | (ref.) | ||||
| CA | 184 | 54 | 1.05 | (0.76-1.44) | 46 | 1.73 | (1.20-2.50) | 12 | 1.00 | (0.52-1.93) | ||||
| AA | 11 | 6 | 1.48 | (0.71-3.07) | 0.19 | 7 | 3.64 | (1.69-7.82) | 0.0002 | 1 | 0.98 | (0.14-6.99) | 0.65 | |
| 154784 G>A (rs17337107) | ||||||||||||||
| GG | 686 | 191 | 1.00 | (ref.) | 117 | 1.00 | (ref.) | 46 | 1.00 | (ref.) | ||||
| GA/AA | 87 | 18 | 0.76 | (0.47-1.23) | 0.27 | 17 | 1.26 | (0.76-2.09) | 0.64 | 1 | 0.18 | (0.03-1.28) | 0.02 | |
| HER2 | Pro1140 Ala (rs1058808) | |||||||||||||
| GG | 361 | 83 | 1.00 | (ref.) | 59 | 1.00 | (ref.) | 19 | 1.00 | (ref.) | ||||
| GC | 337 | 94 | 1.19 | (0.88-1.61) | 60 | 1.04 | (0.72-1.49) | 22 | 1.18 | (0.64-2.17) | ||||
| CC | 73 | 30 | 1.70 | (1.09-2.64) | 0.03 | 14 | 1.01 | (0.56-1.81) | 0.57 | 6 | 1.37 | (0.55-3.37) | 0.33 | |
Adjusted for age, sex, and study center.
Gene-gene interactions
Results from the 1df Tukey test are shown in Table 4. For adenomas, SNPs in EGFR and Src showed a significant interaction (p<0.01). To follow-up on this finding, SNP-SNP interactions between tagSNPs in EGFR and Src were explored (see below). No statistically significant interactions were detected for colon or rectal cancer.
Table 4.
Chatterjee 1df Tukey tests for gene-gene interaction
| Colorectal Adenomaa | Colon Cancerb | Rectal cancerb | |||||
|---|---|---|---|---|---|---|---|
| Gene 1 | Gene 2 | Permutation p | Asymptotic p | Permutation p | Asymptotic p | Permutation p | Asymptotic p |
| EGFR | HER2 | 0.71 | 0.77 | 0.24 | 0.26 | 0.47 | 0.50 |
| EGFR | Src | <0.01 | <0.01 | 0.60 | 0.59 | 0.14 | 0.17 |
| HER2 | Src | 0.67 | 0.68 | 0.99 | 0.99 | 0.39 | 0.36 |
Adjusted for age and sex
Adjusted for age, sex, and study center.
SNP-SNP interactions
Prior to correcting for multiple testing, we detected 8 statistically significant interactions between tagSNPs in EGFR and Src and adenoma risk (Table 5). However, when these interactions were corrected for multiple testing, none remained statistically significant. It is worth noting that two EGFR SNPs, EGFR 179446C>T (rs1140475; Thr903Thr) and EGFR 122960T>G (rs6964705), each interacted with two Src SNPs.
Table 5.
Selected interactions between tagSNPs in EGFR and Src and risk of colorectal adenomaa
| Src-29667A>G | ||||||||||
| AA | AG or GG | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 179446OT (Thr903Thr) | CC | 275 | 345 | 1.00 | (ref.) | 98 | 96 | 1.30 | (0.92-1.82) | |
| CT or TT | 89 | 98 | 1.12 | (0.80-1.59) | 20 | 43 | 0.62 | (0.35-1.12) | 0.02 | |
| Src -41278A>C | ||||||||||
| AA | AC or CC | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 179446C>T (Thr903Thr) | CC | 196 | 252 | 1.00 | (ref.) | 176 | 187 | 1.24 | (0.93-1.67) | |
| CT or TT | 72 | 72 | 1.21 | (0.81-1.80) | 37 | 69 | 0.78 | (0.49-1.24) | 0.04 | |
| Src -34985A>G | ||||||||||
| AA | AG or GG | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 122960T>G | TT | 79 | 101 | 1.00 | (ref.) | 45 | 73 | 0.70 | (0.43-1.16) | |
| TG or GG | 206 | 249 | 0.96 | (0.66-1.39) | 152 | 158 | 1.24 | (0.84-1.83) | 0.04 | |
| Src-25903G>A | ||||||||||
| GG | GA or AA | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 122960T>G | TT | 99 | 127 | 1.00 | (ref.) | 26 | 47 | 0.70 | (0.39-1.25) | |
| TG or GG | 247 | 298 | 1.03 | (0.74-1.44) | 110 | 107 | 1.37 | (0.92-2.04) | 0.04 | |
| Src 9982A>G | ||||||||||
| AA | AG or GG | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 151493T>G | TT | 168 | 187 | 1.00 | (ref.) | 44 | 46 | 1.20 | (0.74-1.97) | |
| TG or GG | 232 | 270 | 0.92 | (0.69-1.23) | 38 | 79 | 0.53 | (0.33-0.85) | 0.03 | |
| Src-3411G>A | ||||||||||
| GG | GA or AA | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 124345G>A | GG | 396 | 469 | 1.00 | (ref.) | 36 | 51 | 0.87 | (0.54-1.40) | |
| GA or AA | 43 | 59 | 0.87 | (0.56-1.35) | 8 | 3 | 3.40 | (0.84-13.74) | 0.04 | |
| EGFR 140539G>A | GG | 302 | 370 | 1.00 | (ref.) | 25 | 44 | 0.71 | (0.42-1.23) | |
| GA or AA | 137 | 158 | 1.09 | (0.81-1.46) | 19 | 10 | 2.61 | (1.15-5.93) | 0.02 | |
| Src -4395A>G | ||||||||||
| AA | AG or GG | |||||||||
| snp | genotype | Cases | Controls | OR | 95% CI | Cases | Controls | OR | 95% CI | p-interactionb |
| EGFR 142044A>G | AA | 186 | 230 | 1.00 | (ref.) | 84 | 91 | 1.17 | (0.81-1.71) | |
| AG or GG | 161 | 175 | 1.05 | (0.77-1.43) | 52 | 85 | 0.68 | (0.45-1.03) | 0.04 | |
Adjusted for age and sex; only statistically significant interactions are shown
Uncorrected for multiple comparisons. After Bonferroni correction, none of the interactions are statistically significant.
EGFR 179446C>T showed statistically significant interactions with both Src -29667A>G (rs747182) and -41278A>C (rs6017916), which are in moderate LD (r2=0.46, Supplemental Figure). In both cases, the combination of variants in Src and EGFR resulted in the relatively lowest risk, combined to all other groups (p-interaction=0.02 and 0.04, respectively).
EGFR 122960T>G (rs6964705) showed interactions with both Src -34985A>G (rs6017944) and -25903G>A (rs6017996), which are not in LD (r2=0.08, Supplemental Figure). For both of these, those with at least one variant Src and EGFR allele were at increased polyp risk (p-interaction=0.04 for both).
Discussion
In this comprehensive study of genetic variability in EGFR signaling across the continuum of colorectal carcinogenesis, we observed several associations between SNPs in EGFR and Src and risk of colorectal cancer; specifically, the EGFR 142572T>C CC genotype was associated with an approximately 40% increase in both colon and rectal cancer risk, compared to the wildtype. This replication of findings across these two tumor locations is interesting and potentially important. However, because we did not have access to an independent study population for replication, we performed multiple comparison adjustment which attenuated the p-values. We also observed several SNP-SNP interactions, indicating that these tagSNPs may need to be considered within a wider context.
Several polymorphisms in EGFR have previously been associated with cancer outcomes. The Arg521Lys polymorphism has been associated with colorectal cancer survival in a small study (n=318) [23]. In that study, opposite associations were observed for men and women, indicating that EGFR polymorphisms may interact with hormone status in colorectal cancer, although this pattern of findings could also have been the result of small numbers. The Arg521Lys polymorphism has also been associated with response to the EGFR inhibitor cetuximab in a study of 32 colorectal cancer patients [24]. In the present study, we observed no association between Arg521Lys and colorectal neoplasia risk overall or when stratified by sex (data not shown), indicating that this EGFR variant may be more important for colorectal cancer progression or response to treatment than for cancer development.
Another EGFR SNP, -216G>T, has been associated with changes in promoter activity [54] and with overall survival among non-small cell lung cancer patients [25], especially among those treated with the EGFR inhibitor gefitinib [26]. This SNP did not pass QC measures in our study. A third polymorphism, a CA-repeat polymorphism in intron 1, in which higher numbers of repeats results in lower EGFR expression, has been associated with risk of breast cancer risk [27] and with survival in head and neck [28], lung [29], colorectal [23] and non-small cell lung cancer [26]. Taken together, these results suggest that genetic variability in EGFR may be associated with increased risk of several cancer types and may predict response to EGFR inhibitors. Given that several EGFR inhibitors have been approved for cancer treatment, it will be important in the future to determine whether the observed associations with cancer survival or response to treatment can be confirmed, and whether a pattern of polymorphisms can identify those most or least likely to benefit from treatment with EGFR inhibitors.
As KRAS mutation is a predictor of response to anti-EGFR antibody therapy in colorectal cancer [55], the association of EGFR -759C>A with increased risk of KRAS-mutated rectal tumors is intriguing and further studies are needed to elucidate the role of common variants in EGFR in relation to KRAS mutations.
To our knowledge, no study has investigated the role of HER2 polymorphisms in colorectal neoplasia risk. However, several studies have investigated the role of IIe655Val in breast cancer development, with mixed results. Several studies have shown increased risk with the variant genotypes [30-32] [reviewed in [34]], whereas others have shown decreased risk [33, 34], or no association [35], reviewed in [34], indicating that the role of this polymorphism, if any, requires further elucidation. A small study of gastric cancer patients and hospital-based controls in Japan found an increased risk associated with the variant genotypes [56], but this requires confirmation in a larger study. We observed no association with this polymorphism in our study populations; thus genetic variability HER2 may be less important for colorectal neoplasia. An exploratory analysis indicated HER2 may influence risk differentially in men and women. In Src, we observed a decreased risk of colorectal cancer with -34985A>G. No other epidemiologic studies of Src polymorphisms have been conducted to date. In one small study, a rare coding mutation in Src was observed in a subset of advanced colorectal tumors [57]; however, two subsequent studies did not observe this mutation [58, 59].
Due to the number of statistical tests that were performed in this study, the likelihood of false positives is high. However, because we conducted a parallel investigation of identical candidate and tagSNPs in three independent study populations, we decided to present uncorrected as well as corrected p-values and evaluate whether the associations with any of these SNPs were consistent across the three study populations. SNPs that are associated with colorectal neoplasia risk in multiple study populations are more likely to be true positives. Further, this is the first study that has comprehensively examined common EGFR, HER2, and Src genetic variability in relation to colorectal adenoma and cancer risk; thus, we report any observed associations to inform future studies.
This study has several strengths. By using both tagSNPs and candidate polymorphisms in this pathway, we achieved comprehensive coverage of genetic variability in the EGFR signaling. For EGFR and HER2, we had access to resequencing data, ensuring that we captured all common variants that are likely to exist among Caucasians. Further, we have comprehensively assessed genetic variation in EGFR, Src, and HER2 in three independent case-control studies of colorectal adenoma or cancer (including tumor markers), using identical genotyping methods, thus allowing us to replicate any promising findings. It is, however, important to consider that the outcomes in the three study populations were not identical: colon and rectal cancer share some, but not all epidemiologic risk factors, and adenoma are precursors that occur years prior to invasive cancer.
In summary, our study provides a thorough investigation, not only of genetic variability in EGFR signaling, but also of the spectrum of the colorectal carcinogenic process. We provide some evidence that EGFR 142575T>C may be important in both colon and rectal cancer, but this should be confirmed in future studies. Given that genetic variants in EGFR may be related to colorectal cancer survival or responsiveness to treatment with EGFR inhibitors, further study of the impact of genetic variability in the EGFR signaling pathway, specifically replication of the tumor subtype analyses, should be conducted.
Acknowledgments
The authors would like to thank Dr. Roberd Bostick and Lisa Fosdick for their contributions to the initial establishment of the adenoma study. We also gratefully acknowledge Sandie Edwards for her contributions to the colon and rectal cancer studies. Sources of financial support: Grants R01 CA114467, R03 CA123577, R25 CA094880, T32 DK007742, and T32 CA009001.
Supplementary material
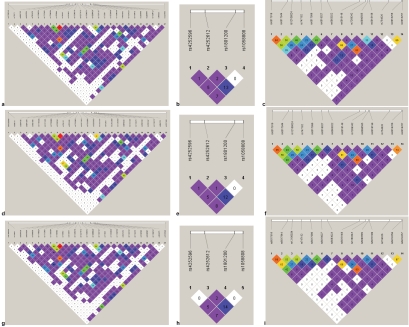
Figure S1.
Linkage disequilibrium among controls in the three study populations; a-c=colon cancer controls; d-f=rectal cancer controls; g-i=adenoma controls. a, d, g=EGFR;
References
- 1.Grandis JR, Sok JC. Signaling through the epidermal growth factor receptor during the development of malignancy. Pharmacol Ther. 2004;102:37–46. doi: 10.1016/j.pharmthera.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Cohen G, Mustafi R, Chumsangsri A, Little N, Nathanson J, Cerda S, Jagadeeswaran S, Dougherty U, Joseph L, Hart J, Yerian L, Tretiakova M, Yuan W, Obara P, Khare S, Sinicrope FA, Fichera A, Boss GR, Carroll R, Bissonnette M. Epidermal growth factor receptor signaling is up-regulated in human colonic aberrant crypt foci. Cancer Res. 2006;66:5656–64. doi: 10.1158/0008-5472.CAN-05-0308. [DOI] [PubMed] [Google Scholar]
- 3.Malecka Panas E, Kordek R, Biernat W, Tureaud J, Liberski PP, Majumdar AP. Differential activation of total and EGF receptor (EGF-R) tyrosine kinase (tyr-k) in the rectal mucosa in patients with adenomatous polyps, ulcerative colitis and colon cancer. Hepatogastroenterology. 1997;44:435–40. [PubMed] [Google Scholar]
- 4.Porebska I, Harlozinska A, Bojarowski T. Expression of the tyrosine kinase activity growth factor receptors (EGFR, ERB B2, ERB B3) in colorectal adenocarcinomas and adenomas. Tumour Biol. 2000;21:105–15. doi: 10.1159/000030116. [DOI] [PubMed] [Google Scholar]
- 5.Messa C, Russo F, Caruso MG, Di Leo A. EGF, TGF-alpha, and EGF-R in human colorectal adenocarcinoma. Acta Oncol. 1998;37:285–9. doi: 10.1080/028418698429595. [DOI] [PubMed] [Google Scholar]
- 6.Tong WM, Ellinger A, Sheinin Y, Cross HS. Epidermal growth factor receptor expression in primary cultured human colorectal carcinoma cells. Br J Cancer. 1998;77:1792–8. doi: 10.1038/bjc.1998.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radinsky R, Risin S, Fan D, Dong Z, Bielenberg D, Bucana CD, Fidler IJ. Level and function of epidermal growth factor receptor predict the metastatic potential of human colon carcinoma cells. Clin Cancer Res. 1995;1:19–31. [PubMed] [Google Scholar]
- 8.Ng K, Zhu AX. Targeting the epidermal growth factor receptor in metastatic colorectal cancer. Crit Rev Oncol Hematol. 2008;65:8–20. doi: 10.1016/j.critrevonc.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Roberts RB, Min L, Washington MK, Olsen SJ, Settle SH, Coffey RJ, Threadgill DW. Importance of epidermal growth factor receptor signaling in establishment of adenomas and maintenance of carcinomas during intestinal tumorigenesis. Proc Natl Acad Sci USA. 2002;99:1521–6. doi: 10.1073/pnas.032678499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torrance CJ, Jackson PE, Montgomery E, Kinzler KW, Vogelstein B, Wissner A, Nunes M, Frost P, Discafani CM. Combinatorial chemoprevention of intestinal neoplasia. Nat Med. 2000;6:1024–8. doi: 10.1038/79534. [DOI] [PubMed] [Google Scholar]
- 11.Fichera A, Little N, Jagadeeswaran S, Dougherty U, Sehdev A, Mustafi R, Cerda S, Yuan W, Khare S, Tretiakova M, Gong C, Tallerico M, Cohen G, Joseph L, Hart J, Turner JR, Bissonnette M. Epidermal growth factor receptor signaling is required for microadenoma formation in the mouse azoxymethane model of colonic carcinogenesis. Cancer Res. 2007;67:827–35. doi: 10.1158/0008-5472.CAN-05-3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baselga J, Swain SM. Novel anticancer targets: revisiting ERBB2 and discovering ERBB3. Nat Rev Cancer. 2009;9:463–75. doi: 10.1038/nrc2656. [DOI] [PubMed] [Google Scholar]
- 13.Owens MA, Horten BC, Da Silva MM. HER2 amplification ratios by fluorescence in situ hybridization and correlation with immunohistochemistry in a cohort of 6556 breast cancer tissues. Clin Breast Cancer. 2004;5:63–9. doi: 10.3816/cbc.2004.n.011. [DOI] [PubMed] [Google Scholar]
- 14.Vermeij J, Teugels E, Bourgain C, Xiangming J, in ‘t Veld P, Ghislain V, Neyns B, De Greve J. Genomic activation of the EGFR and HER2-neu genes in a significant proportion of invasive epithelial ovarian cancers. BMC Cancer. 2008;8:3. doi: 10.1186/1471-2407-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaehne J, Urmacher C, Thaler HT, Friedlander Klar H, Cordon Cardo C, Meyer HJ. Expression of Her2/neu oncogene product p185 in correlation to clinicopathological and prognostic factors of gastric carcinoma. J Cancer Res Clin Oncol. 1992;118:474–9. doi: 10.1007/BF01629433. [DOI] [PubMed] [Google Scholar]
- 16.Roskoski R., Jr The ErbB/HER receptor proteintyrosine kinases and cancer. Biochem Biophys Res Commun. 2004;319:1–11. doi: 10.1016/j.bbrc.2004.04.150. [DOI] [PubMed] [Google Scholar]
- 17.Dehm SM, Bonham K. SRC gene expression in human cancer: the role of transcriptional activation. Biochem Cell Biol. 2004;82:263–74. doi: 10.1139/o03-077. [DOI] [PubMed] [Google Scholar]
- 18.Mathew S, George SP, Wang Y, Siddiqui MR, Srinivasan K, Tan L, Khurana S. Potential molecular mechanism for c-Src kinase-mediated regulation of intestinal cell migration. J Biol Chem. 2008;283:22709–22. doi: 10.1074/jbc.M801319200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Irby RB, Yeatman TJ. Role of Src expression and activation in human cancer. Oncogene. 2000;19:5636–42. doi: 10.1038/sj.onc.1203912. [DOI] [PubMed] [Google Scholar]
- 20.de Heer P, Koudijs MM, van de Velde CJ, Aalbers Rl, Tollenaar RA, Putter H, Morreau J, van de Water B, Kuppen PJ. Combined expression of the non-receptor protein tyrosine kinases FAK and Src in primary colorectal cancer is associated with tumor recurrence and metastasis formation. Eur J Surg Oncol. 2008;34:1253–61. doi: 10.1016/j.ejso.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Cartwright CA, Meisler AI, Eckhart W. Activation of the pp60c-src protein kinase is an early event in colonic carcinogenesis. Proc Natl Acad Sci USA. 1990;87:558–62. doi: 10.1073/pnas.87.2.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cartwright CA, Coad CA, Egbert BM. Elevated c-Src tyrosine kinase activity in premalignant epithelia of ulcerative colitis. J Clin Invest. 1994;93:509–15. doi: 10.1172/JCI117000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Press OA, Zhang W, Gordon MA, Yang D, Lurje G, Iqbal S, El Khoueiry A, Lenz HJ. Gender-related survival differences associated with EGFR polymorphisms in metastatic colon cancer. Cancer Res. 2008;68:3037–42. doi: 10.1158/0008-5472.CAN-07-2718. [DOI] [PubMed] [Google Scholar]
- 24.Goncalves A, Esteyries S, Taylor Smedra B, Lagarde A, Ayadi M, Monges G, Bertucci F, Esterni B, Delpero JR, Turrini 0, Lelong B, Viens P, Borg JP, Birnbaum D, Olschwang S, Viret F. A polymorphism of EGFR extracellular domain is associated with progression free-survival in metastatic colorectal cancer patients receiving cetuximab-based treatment. BMC Cancer. 2008;8:169. doi: 10.1186/1471-2407-8-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gregorc V, Hidalgo M, Spreafico A, Cusatis G, Ludovini V, Ingersoll RG, Marsh S, Steinberg SM, Vigano MG, Ghio D, Villa E, Sparreboom A, Baker SD. Germline polymorphisms in EGFR and survival in patients with lung cancer receiving gefitinib. Clin Pharmacol Ther. 2008;83:477–84. doi: 10.1038/sj.clpt.6100320. [DOI] [PubMed] [Google Scholar]
- 26.Liu G, Gurubhagavatula S, Zhou W, Wang Z, Yeap BY, Asomaning K, Su L, Heist R, Lynch TJ, Christiani DC. Epidermal growth factor receptor polymorphisms and clinical outcomes in non-small-cell lung cancer patients treated with gefitinib. Pharmacogenomics J. 2008;8:129–38. doi: 10.1038/sj.tpj.6500444. [DOI] [PubMed] [Google Scholar]
- 27.Brandt B, Hermann S, Straif K, Tidow N, Buerger H, Chang Claude J. Modification of breast cancer risk in young women by a polymorphic sequence in the egfr gene. Cancer Res. 2004;64:7–12. doi: 10.1158/0008-5472.can-03-2623. [DOI] [PubMed] [Google Scholar]
- 28.Bandres E, Barricarte R, Cantero C, Honorato B, Malumbres R, Zarate R, Alcalde J, Garcia-Foncillas J. Epidermal growth factor receptor (EGFR) polymorphisms and survival in head and neck cancer patients. Oral Oncol. 2007;43:713–9. doi: 10.1016/j.oraloncology.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Nie Q, Wang Z, Zhang GC, An SJ, Lin JY, Guo AL, Li R, Gan B, Huang Y, Mok TS, Wu YL. The epidermal growth factor receptor intronl (CA) n microsatellite polymorphism is a potential predictor of treatment outcome in patients with advanced lung cancer treated with Gefitinib. Eur J Pharmacol. 2007;570:175–81. doi: 10.1016/j.ejphar.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 30.Siddig A, Mohamed AO, Kamal H, Awad S, Hassan AH, Zilahi E, Al Haj M, Bernsen R, Adem A. HER-2/neu IIe655Val polymorphism and the risk of breast cancer. Ann N Y Acad Sci. 2008;1138:84–94. doi: 10.1196/annals.1414.014. [DOI] [PubMed] [Google Scholar]
- 31.Lee SC, Hou MF, Hsieh PC, Wu SH, Hou LA, Ma H, Tsai SM, Tsai LY. A case-control study of the HER2 IIe655Val polymorphism and risk of breast cancer in Taiwan. Clin Biochem. 2008;41:121–5. doi: 10.1016/j.clinbiochem.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 32.Millikan RC, Hummer AJ, Wolff MS, Hishida A, Begg CB. HER2 codon 655 polymorphism and breast cancer: results from kin-cohort and case -control analyses. Breast Cancer Res Treat. 2005;89:309–12. doi: 10.1007/s10549-004-2171-5. [DOI] [PubMed] [Google Scholar]
- 33.Nelson SE, Gould MN, Hampton JM, Trentham Dietz A. A case-control study of the HER2 IIe655Val polymorphism in relation to risk of invasive breast cancer. Breast Cancer Res. 2005;7:R357–64. doi: 10.1186/bcr1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox DG, Hankinson SE, Hunter DJ. The erbB2/ HER2/neu receptor polymorphism IIe655Val and breast cancer risk. Pharmacogenet Genomics. 2005;15:447–50. doi: 10.1097/01.fpc.0000166822.66754.c6. [DOI] [PubMed] [Google Scholar]
- 35.Qu S, Cai Q, Gao YT, Lu W, Cai H, Su Y, Wang SE, Shu XO, Zheng W. ERBB2 genetic polymorphism and breast cancer risk in Chinese women: a population-based case-control study. Breast Cancer Res Treat. 2008;110:169–76. doi: 10.1007/s10549-007-9691-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Potter JD, Bostick RM, Grandits GA, Fosdick L, Elmer P, Wood J, Grambsch P, Louis TA. Hormone replacement therapy is associated with lower risk of adenomatous polyps of the large bowel: the Minnesota Cancer Prevention Research Unit Case-Control Study. Cancer Epidemiol Biomarkers Prev. 1996;5:779–84. [PubMed] [Google Scholar]
- 37.Slattery ML, Potter JD, Duncan DM, Berry TD. Dietary fats and colon cancer: assessment of risk associated with specific fatty acids. Int J Cancer. 1997;73:670–7. doi: 10.1002/(sici)1097-0215(19971127)73:5<670::aid-ijc10>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 38.Slattery ML, Caan BJ, Benson J, Murtaugh M. Energy balance and rectal cancer: an evaluation of energy intake, energy expenditure, and body mass index. Nutr Cancer. 2003;46:166–71. doi: 10.1207/S15327914NC4602_09. [DOI] [PubMed] [Google Scholar]
- 39.Spirio LN, Samowitz W, Robertson J, Robertson M, Burt RW, Leppert M, White R. Alleles of APC modulate the frequency and classes of mutations that lead to colon polyps. Nat Genet. 1998;20:385–8. doi: 10.1038/3865. [DOI] [PubMed] [Google Scholar]
- 40.Samowitz WS, Albertsen H, Herrick J, Levin TR, Sweeney C, Murtaugh MA, Wolff RK, Slattery ML. Evaluation of a large, population-based sample supports a CpG island methylator phenotype in colon cancer. Gastroenterology. 2005;129:837–45. doi: 10.1053/j.gastro.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 41.Samowitz WS, Curtin K, Ma KN, Edwards S, Schaffer D, Leppert MF, Slattery ML. Prognostic significance of p53 mutations in colon cancer at the population level. Int J Cancer. 2002;99:597–602. doi: 10.1002/ijc.10405. [DOI] [PubMed] [Google Scholar]
- 42.Samowitz WS, Curtin K, Schaffer D, Robertson M, Leppert M, Slattery ML. Relationship of Kiras mutations in colon cancers to tumor location, stage, and survival: a population-based study. Cancer Epidemiol Biomarkers Prev. 2000;9:1193–7. [PubMed] [Google Scholar]
- 43.Slattery ML, Curtin K, Anderson K, Ma KN, Ballard L, Edwards S, Schaffer D, Potter J, Leppert M, Samowitz WS. Associations between cigarette smoking, lifestyle factors, and microsatellite instability in colon tumors. J Natl Cancer Inst. 2000;92:1831–6. doi: 10.1093/jnci/92.22.1831. [DOI] [PubMed] [Google Scholar]
- 44.Samowitz WS, Albertsen H, Sweeney C, Herrick J, Caan BJ, Anderson KE, Wolff RK, Slattery ML. Association of smoking, CpG island methylator phenotype, and V600E BRAF mutations in colon cancer. J Natl Cancer Inst. 2006;98:1731–8. doi: 10.1093/jnci/djj468. [DOI] [PubMed] [Google Scholar]
- 45.Issa JP, Shen L, Toyota M. CIMP, at last. Gastroenterology. 2005;129:1121–4. doi: 10.1053/j.gastro.2005.07.040. [DOI] [PubMed] [Google Scholar]
- 46.Samowitz WS. The CpG island methylator phenotype in colorectal cancer. J Mol Diagn. 2007;9:281–3. doi: 10.2353/jmoldx.2007.070031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carlson CS, Eberle MA, Rieder MJ, Yi Q, Kruglyak L, Nickerson DA. Selecting a maximally informative set of single-nucleotide polymorphisms for association analyses using linkage disequilibrium. Am J Hum Genet. 2004;74:106–20. doi: 10.1086/381000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Conneely KN, Boehnke M. So Many Correlated Tests, So Little Time! Rapid Adjustment of P Values for Multiple Correlated Tests. Am J Hum Genet. 2007;81:1158–68. doi: 10.1086/522036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gauderman WJ, Murcray C, Gilliland F, Conti DV. Testing association between disease and multiple SNPs in a candidate gene. Genet Epidemiol. 2007;31:383–95. doi: 10.1002/gepi.20219. [DOI] [PubMed] [Google Scholar]
- 50.Slattery ML, Curtin K, Wolff RK, Boucher KM, Sweeney C, Edwards S, Caan BJ, Samowitz W. A comparison of colon and rectal somatic DNA alterations. Dis Colon Rectum. 2009;52:1304–11. doi: 10.1007/DCR.0b013e3181a0e5df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burton P, Gurrin L, Sly P. Extending the simple linear regression model to account for correlated responses: an introduction to generalized estimating equations and multi-level mixed modelling. Stat Med. 1998;17:1261–91. doi: 10.1002/(sici)1097-0258(19980615)17:11<1261::aid-sim846>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 52.Kuss O, McLerran D. A note on the estimation of the multinomial logistic model with correlated responses in SAS. Comput Methods Programs Biomed. 2007;87:262–9. doi: 10.1016/j.cmpb.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 53.Chatterjee N, Kalaylioglu Z, Moslehi R, Peters U, Wacholder S. Powerful multilocus tests of genetic association in the presence of gene-gene and gene-environment interactions. Am J Hum Genet. 2006;79:1002–16. doi: 10.1086/509704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu W, Innocenti F, Wu MH, Desai AA, Dolan ME, Cook EH, Jr, Ratain MJ. A functional common polymorphism in a Sp1 recognition site of the epidermal growth factor receptor gene promoter. Cancer Res. 2005;65:46–53. [PubMed] [Google Scholar]
- 55.Watanabe T, Kobunai T, Yamamoto Y, Matsuda K, Ishihara S, Nozawa K, linuma H, Ikeuchi H, Eshima K. Differential gene expression signatures between colorectal cancers with and without KRAS mutations: Crosstalk between the KRAS pathway and other signalling pathways. Eur J Cancer. 2011;47:1946–54. doi: 10.1016/j.ejca.2011.03.029. [DOI] [PubMed] [Google Scholar]
- 56.Kuraoka K, Matsumura S, Hamai Y, Nakachi K, Imai K, Matsusaki K, Oue N, Ito R, Nakayama H, Yasui W. A single nucleotide polymorphism in the transmembrane domain coding region of HER-2 is associated with development and malignant phenotype of gastric cancer. Int J Cancer. 2003;107:593–6. doi: 10.1002/ijc.11450. [DOI] [PubMed] [Google Scholar]
- 57.Irby RB, Mao W, Coppola D, Kang J, Loubeau JM, Trudeau W, Karl R, Fujita DJ, Jove R, Yeatman TJ. Activating SRC mutation in a subset of advanced human colon cancers. Nat Genet. 1999;21:187–90. doi: 10.1038/5971. [DOI] [PubMed] [Google Scholar]
- 58.Laghi L, Bianchi P, Orbetegli O, Gennari L, Roncalli M, Malesci A. Lack of mutation at codon 531 of SRC in advanced colorectal cancers from Italian patients. Br J Cancer. 2001;84:196–8. doi: 10.1054/bjoc.2000.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Daigo Y, Furukawa Y, Kawasoe T, Ishiguro H, Fujita M, Sugai S, Nakamori S, Liefers GJ, Tollenaar RA, van de Velde CJ, Nakamura Y. Absence of genetic alteration at codon 531 of the human c-src gene in 479 advanced colorectal cancers from Japanese and Caucasian patients. Cancer Res. 1999;59:4222–4. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.