Abstract
Early diagnosis and multi-modality treatment has resulted in prolonged survival of many patients with carcinoma of breast. It is important that the surgeons who handle breast malignancies look at the psychological and cosmetic aspects without compromising the oncologic principles of surgery in carcinoma of the breast. Post mastectomy immediate breast reconstruction (IBR) addresses the psychological and cosmetic problems that follow mastectomy. There are various techniques available for post mastectomy primary breast reconstruction. The technique should be affordable to the large number of economically poor patients and should be less time consuming. During the period of 13 years from January 1996 to December 2008, we have operated 2932 cases of carcinoma breast, of which 546 patients had IBR using various procedures. In our centre, TRAM flap was found to be the best procedure for post mastectomy immediate breast reconstruction. Immediate reconstruction whenever possible is the best option. Presence of the tissue used for reconstruction was not found to affect any form of local adjuvant treatment like radiotherapy, or delay the detection of local recurrent disease.
Keywords: Carcinoma breast, Mastectomy, Immediate breast reconstruction, Transverse Rectus Abdominis Myocutaneous flap (TRAM flap)
Introduction
During the Halstedian era, which lasted for many years, radical mastectomy was the treatment offered for carcinoma breast. In fact Halsted warned against closure of breast wound after the surgery [1]. Hence attempts to reconstruct breast after mastectomy had to wait for many years. Today the concepts have changed and it is more of Breast Conservative Surgery. This is made possible because of early detection, better investigative facilities, increased understanding of the pattern of disease spread and better forms of adjuvant treatment options.
Despite the condemnation for reconstruction of breast, Vincent Czerny tried it for the first time in 1895 by transplanting a large lipoma of the flank to the mastectomy site, and it was reported that the patient was doing well after 1 year [2]. Tansini described the use of latissimus dorsii myocutaneous flap for the first time in 1906 for a breast reconstruction [3]. In 1942, Sir Harold Gillies described pedicled flap from abdomen requiring multiple stages for reconstructing breast [4]. It was Manchots landmark work on vascular territories of the body that ignited the interest of many, to develop different types of flaps including axial flaps [5].
A good number of patients do come in the early stages of the disease due to improved awareness and availability of better diagnostic tools. Better survival and improved quality of life have increased the expectations of these patients as well the surgeons. Fortunately today’s woman need not live her life with an anatomical deficiency and a cosmetic problem, which adversely affects her psychology and her social movements. Breast reconstructions, and mainly immediate breast reconstructions [6], have come to help these women who have undergone mastectomies. Compared to delayed reconstruction, IBR reduces the total hospital expense and total period of hospital stay [7].
In India, the percentage of patients who can be offered a conservative breast surgery for a malignant breast disease has not attained a sizable proportion. We still, do get patients presenting in the late stages of the disease, requiring only toilet mastectomies.
Forty percent patients, diagnosed to have breast cancer, still undergo mastectomy because of multifocal pathology, non-conservable disease status by inappropriate breast/tumour size ratio, or by choice of the patient [8]. Many of these women can be offered primary reconstruction and a good majority accepts this mode of therapy. The most common method of breast reconstruction is a Transverse Rectus Abdominis Myocutaneous (TRAM) flap because of its texture and large volume [10]. Other flaps used to reconstruct breast are LD flap, inferior gluteal flap, superior gluteal flap etc. [12].
Materials and Methods
Lourdes Hospital, Cochin, Kerala, India is a 750-bedded general hospital working at a tertiary referral level. The General Surgical department performs about 4500 major operations and about 5500 minor operations every year and has a predominant interest in oncology. All patients treated for carcinoma breast from January 1996 to December 2008 (13 year period) have been included in this study.
- Whenever a patient is presenting to the department directly with symptoms pertaining to breast, a thorough clinical examination is done and if suspected to have a malignancy the clinical stage is noted.
- Majority of the patients presented with a lump in the breast. These patients are sent for Fine Needle Aspiration Cytology (FNAC) study.
- If FNAC confirms malignancy, after a metastatic work up, patients are taken up for definitive surgery.
- If FNAC is suspicious/inconclusive of malignancy, a repeat FNAC or a True-cut biopsy or an excision biopsy is done depending upon the size of the lump and proceeded as above.
- If the patients with breast symptoms do not have a palpable disease a mammogram and/or a ductogram are done, depending on the symptoms along with a breast ultrasound examination to detect any mass lesion and targeted cytology/biopsy is done.
The referred patients with a proven breast malignancy were clinically reviewed and their slides were reviewed by our pathologists/cytopathologists and the diagnosis is reconfirmed.
Once the diagnosis is established and the staging work up is completed on an outpatient basis, the patients are offered treatment depending on their stage of the disease as per the protocol pertaining to UICC 1999 staging for carcinoma breast [14].
The criteria to offer breast reconstruction are
- Stage of the disease
- Stage III patients
- Stage I and II patients, not opting for Breast Conservative Treatment.
Likely anatomical deficiency after mastectomy: This pertains to a large group of patients who had a good-sized breast, which if removed will certainly leave behind unacceptable anatomical deficiency. A small group of ladies with very small sized breast having malignancy were not offered breast reconstruction as this would not have caused any significant benefit to the appearance of the lady.
Age of the patient: Breast reconstruction was suggested only to people below the age of 60 years and also after considering their active social/sexual life.
Mental make up of the patient: The age, social status, educational and economic background along with the stage of the disease alter the mental attitude of patients with breast malignancy. Breast reconstruction is offered only to those who have a very positive frame of mind and only to those who could be brought to that state after adequate counselling.
Economic status of the patient: As the expenses of treatment in India for all the patients will have to be borne by them, except in a small minority who are supported by the insurance companies, a major deciding factor in offering the reconstruction to these patients, was their economic status. In our department, an added expense of Rs. 7000/- to Rs. 8000/- will have to be borne by the patients opting for a breast reconstruction.
Educational back ground of the patient: Breast reconstruction was offered only to those who have clearly understood the philosophy behind this and only to whom the treating surgeon has thought, the message of adherence to the protocol of treatment and the need for constant follow up were clearly understood [15].
Demand of the patient: Irrespective of all the factors mentioned, the patient’s demand also will be taken into consideration at the time of total planning of treatment.
The surgery for carcinoma breast, in the group of patients, who had primary post mastectomy breast reconstruction, was a Modified Radical Mastectomy (MRM) (Auschinclos) where clearance of axilla is done up to level III lymph nodes. All throughout the surgery, no sutures are used and haemostasis is achieved by bipolar cautery. The incision put over the breast will include the nipple areolar complex and the skin over the tumour and it is through this incision that the breast tissue and the axilla are cleared to give the best cosmesis to the patient. If the nipple areolar complex can be spared without oncologic compromise it is done to achieve a better cosmetic result.
Post mastectomy primary breast reconstruction is done with a pedicled Transverse Rectus Abdominis Myocutaneous (TRAM) flap or Latissimus Dorsii (LD) flap.
Technique of Raising TRAM Flap
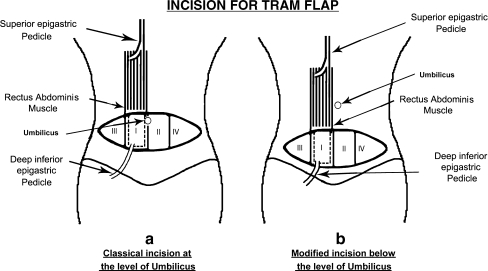
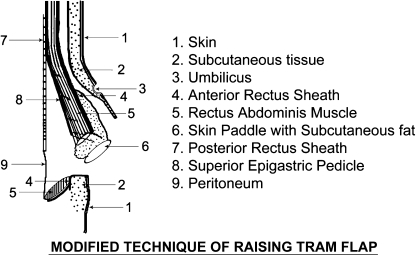
Depending on the volume of tissue needed to match other breast, the TRAM flap can be transferred on a single pedicle or a single pedicle with supercharging of the flap using the cut end of the pedicle or as a free flap. We have used single pedicled flap usually based on the contra-lateral superior epigastric artery in most of the cases [11]. We use a modified technique to harvest the TRAM flap. The skin incision is put as shown in Fig. 1, much below the level of umbilicus where the classical incision is put, so that the final scar is much more acceptable than that in the classical incision. The area of skin taken depends on the area needed to be covered over the mastectomy site. Skin is cut along with subcutaneous fat obliquely so as to include large amount of fat of the anterior abdominal wall to provide the bulk for reconstruction. The take of fat on to the flap is up to the level of umbilicus to have the peri-umbilical perforators also to be retained in the flap for a better vascularity. At the upper part of the flap the incision is extended down to the anterior rectus sheath at the level above the umbilicus. As shown in Fig. 2, a plane is then created anterior to the anterior rectus sheath all the way up to the mastectomy site crossing the midline and it is through this space that the flap is taken from the donor site to the recipient area. At the lower part of the flap, the incision is extended in depth through the anterior rectus sheath to include the rectus muscle and the preperitoneal fat, where the inferior epigastric artery lies, which is divided and the upper part, the vascular pedicle of the flap, is taken along with the flap. The flap is elevated by dissecting in the plane between the rectus muscle and the posterior rectus sheath by cutting at the place of meeting of anterior and posterior sheaths of the rectus muscle. Thus the flap will have about 120–150° of turn at the pedicle level when it is taken to the recipient area. Since the defect of the donor site is below the level of the arcus semilunaris, a polypropylene mesh is always used to create strength for the abdominal wall, there by preventing the development of hernia.
Fig. 1.
Incision for TRAM flap. a Classical incision at the level of umbilicus, b Modified incision below the level of umbilicus
Fig. 2.
Modified technique of raising TRAM flap
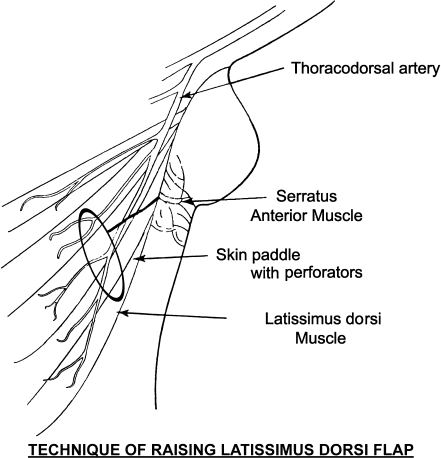
Technique of Raising LD Flap
Incision is put as shown in the Fig. 3, depending on the area of skin needed for the cover. The slantingly placed vertical incision, along the posterior axillary fold, is deepened first to identify the muscle and then the skin flaps are raised to find the anterior border of the latissimus dorsii muscle which is raised off the lateral chest wall. The island of skin already marked along with the underlying tissues including the muscle is harvested to be placed to the recipient area of the mastectomy site.
Fig. 3.
a Modified technique of raising TRAM flap, b Technique of raising latissimus dorsi flap
Results
In the 13-year period from January 1996 to December 2008, we have operated 2932 cases of carcinoma breast, of which 546 (18.62%) patients had primary reconstruction using different procedures (Tables 1 and 2). Breast reconstruction was done using mainly TRAM flap and LD flap was used infrequently.
Table 1.
Age distribution of patients undergoing mastectomy
| Age groups (Years) | No. of cases | No. of cases opted for IBR | Percentage |
|---|---|---|---|
| 10−19 | 3 | 3 | 100.00% |
| 20−29 | 23 | 20 | 86.96% |
| 30−39 | 672 | 264 | 39.29% |
| 40−49 | 1025 | 214 | 20.88% |
| 50−59 | 756 | 45 | 5.95% |
| 60−69 | 392 | 0 | 0 |
| 70−79 | 58 | 0 | 0 |
| 80−89 | 3 | 0 | 0 |
| Total | 2932 | 546 | 18.62% |
Table 2.
Table showing no.of patients underwent MRM OR MRM with IBR
| Type of surgery | Percentage | |
|---|---|---|
| No. of patients opted for MRM only | 2386 | 81.38% |
| Number of patients opted for MRM with IBR | 546 | 18.62% |
| Total | 2932 |
We have used TRAM flap to reconstruct breast in 528 (96.7%) patients and LD flap in 18 (3.3%) patients. Nipple reconstruction over TRAM flap was done in 3 (0.55%) patients (Table 3). We never had total flap failure. But superficial skin necrosis and partial flap failure were seen in 24 (4.55%) patients with TRAM flap and 3 (16.6%) patients in LD flap (Table 4).
Table 3.
Different types of reconstruction
| Type of reconstruction | Percentage | |
|---|---|---|
| TRAM flap | 528 | 96.7% |
| LD flap | 18 | 3.3% |
| TRAM flap with nipple reconstruction | 3 | 0.55% |
| LD flap with nipple reconstruction | 0 | 0 |
| Total | 546 |
Table 4.
Post operative complications
| TRAM | LD | |
|---|---|---|
| Total flap failure | 0 | 0 |
| Superficial skin necrosis | 18 (3.40%) | 2 (11.11%) |
| Partial flap failure | 3 (0.57%) | 1 (5.55%) |
| Total | 21 (3.98%) | 3 (5.40%) |
Discussion
Post mastectomy immediate breast reconstruction has definite advantages over mastectomy alone by providing good cosmesis thereby imparting psychological benefits to the woman.
The appreciation of oncologic safety has lead to immediate reconstruction of breast in a single anaesthesia over the past few years. . Skin sparing mastectomy and further sparing of nipple areola complex has improved the final appearance.
Between TRAM and LD flaps, aesthetically TRAM flap is better, as it provides better bulk of tissues and also helps to achieve a reasonable abdominoplasty in most women. The main disadvantage of LD flap is that, it provides only a limited volume of tissues and hence requires the concomitant use of a breast implant to achieve a volume match with the opposite breast. This is expensive in our economic setting. Hence we use L.D flap in very limited situations alone, for breast reconstructions. As stated by many authors, we also observed that preserving infra-mammary fold, offers the definite advantage in IBR towards achieving a better cosmesis.
Over all hospital stay in our patients was about 7–8 days and it is comparable to other authors [9]. We had about 21(3.98%) flap related complication in TRAM flap group, which is comparable to other studies [13]. Among donor site complication we had occasional seromas but never had abdominal hernias or weakness. This may be due to the routine use of mesh for abdominal closures. Both flaps never hindered adjuvant local Radiotherapy if indicated or detection of local recurrence to any extent..
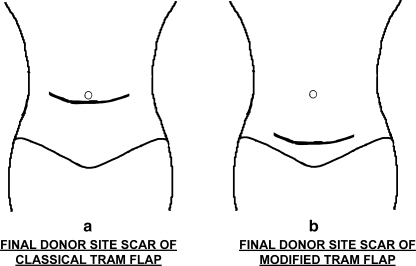
In initial cases we used to harvest TRAM flaps at the level of the umbilicus. Currently we harvest the skin of the TRAM flap from much lower down to close the wound finally close to a Pfannensteil incision to have a more acceptable scar (Fig. 4).
Fig. 4.
a Final donor site scar of classical TRAM flap, b Final donor site of modified TRAM flap
Post Mastectomy Reconstruction
Conclusion
Immediate reconstruction of post mastectomy breast should be undertaken whenever possible.
TRAM flap is the best choice for immediate breast reconstruction.
Immediate reconstruction never comes in the way adjuvant therapy.
References
- 1.Halstead WS, editor. Surgical papers, vol, 2. Baltimore: Johns Hopkins; 1924. [Google Scholar]
- 2.Goldwyn R. Vincenz Czerny and the beginnings of breast reconstruction. Plast Reconstr Surg. 1978;61:673–681. doi: 10.1097/00006534-197805000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Bostwick J, 3rd, Schelfan M. The Latissmus dorsii musculo-cutaneous flap: a one stage breast reconstruction. Clin Plast Surg. 1980;7:71–78. [PubMed] [Google Scholar]
- 4.Mendelson BC. The evolution of breast reconstruction. Med J Aust. 1982;1:7–8. doi: 10.5694/j.1326-5377.1982.tb132095.x. [DOI] [PubMed] [Google Scholar]
- 5.Manchot C. Die Hautarterien des Menschilchen Korpers. Leipzig: Vogel; 1889. [Google Scholar]
- 6.Georginde G, Georginde N, McCarty KS, Jr, Seister HF. Rationale for immediate reconstruction of the breast following modified radical mastectomy. Ann Plast Surg. 1982;8:20. doi: 10.1097/00000637-198201000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Khoo A, Kroll SS, Reece GP, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg. 1998;101:964. doi: 10.1097/00006534-199804040-00011. [DOI] [PubMed] [Google Scholar]
- 8.Baildam AD. Oncoplastic surgery of the breast. Br J Surg. 2002;89:532–533. doi: 10.1046/j.1365-2168.2002.02077.x. [DOI] [PubMed] [Google Scholar]
- 9.Bostwick J, Carlson GW. Reconstruction of the breast. Surg Oncol Cli North Am. 1997;6:71–89. [PubMed] [Google Scholar]
- 10.Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast reconstruction Surg. 1982;69:216. doi: 10.1097/00006534-198202000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Grotting JC, Urist MM, Maddox WA, Vasconez LO. Conventional TRAM flap versus free microsurgical TRAM flap for immediate breast reconstruction. Plast Reconstr Surg. 1989;83:828. doi: 10.1097/00006534-198905000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Joseph JD, Jeanne AP. Rehabilitation after treatment for caner of the breast. In: Devita VT, Samuel H Jr, Rosenberg SA, editors. Cancer principles and practice of oncology. Philidelphia: Lippincott, Williams and Wilkins; 2001. pp. 1717–1720. [Google Scholar]
- 13.John SM, Bradon J, Wilhelmi, Linda GP. Breast reconstruction. In: Townsend CM, Beuchamp RD, Evers BM, Mattox KL, editors. Sabiston text book of surgery—the biological basis of modern surgical practice. New Delhi: Replica Press Pvt. Ltd; 2001. p. 597. [Google Scholar]
- 14.Iglehart JD, Kaelin CM. Breast. In: Townsend CM, Beuchamp RD, Evers BM, Mattox KL, editors. Sabiston text book of surgery—the biological basis of modern surgical practice. New Delhi: Replica Press Pvt. Ltd; 2001. p. 597. [Google Scholar]
- 15.Geoffrey LR. Reconstructive surgery. In: Buzdar AV, Freedman RS, editors. M.D. Anderson Cancer care series breast cancer. India: Springer, Replika press Pvt. Ltd; 2003. pp. 247–248. [Google Scholar]