In 2001, early goal-directed therapy (EGDT) resulted in a 16% reduction in hospital mortality and, post hoc, a higher lactate clearance in severe sepsis and septic shock.1 Multiple studies have confirmed the validity and generalizability of EGDT, resulting in its adoption into the Surviving Sepsis Campaign Guidelines.2,3 Nguyen et al4,5 examined early lactate clearance and found a significant retrospective association with inflammation, apoptosis, coagulation, organ dysfunction, and mortality. Following this rationale, Jones et al6 modified the EGDT protocol in 2010 using a noninferiority study design and concluded that lactate clearance is equivalent to central venous oxygen saturation (Scvo2) in the management of individual patients.
Before applying the findings of Jones et al6 to one’s next patient, compare the baseline characteristics, early hemodynamic patterns, and therapeutic interventions between those of Jones et al6 and the EGDT study.1 Further, review the complexities of lactate kinetics and the weaknesses of a noninferiority study design.7 Based on these facts, it is clear that lactate clearance and Scvo2 are not equivalent, but complementary goals for the individual patient.
The Hemodynamic Phases of Severe Sepsis and Septic Shock
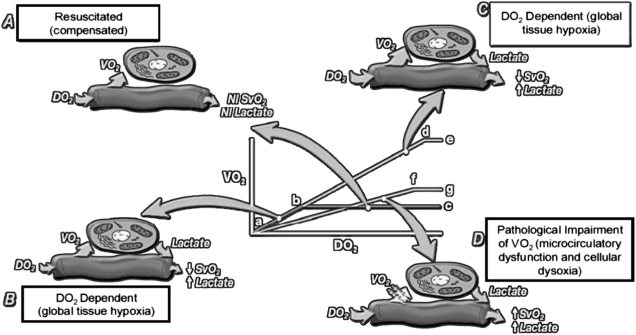
The early stages of sepsis are accompanied by circulatory insufficiency that results from hypovolemia, vasomotor dysfunction, myocardial depression, and increased metabolic demands. In the systemic oxygen delivery (Do2)-dependent (hypodynamic) phase, a decrease in Do2 results in a decrease in Scvo2/mixed venous oxygen saturation (Svo2) and usually an increase in systemic oxygen extraction (OER) or 1 − Scvo2/Svo2 (Fig 1,8 Table 1). When the limits of the OER (anaerobic threshold) are reached, lactate is produced, signifying the development of global tissue hypoxia (GTH). There is significant individual variation in the anaerobic threshold leading to variable lactate production.9 This gives rise to why some patients may require normal or elevated Do2 in order to resolve GTH (decreased Scvo2/Svo2 and increased lactate) (Fig 1, Table 1). GTH is associated with increased morbidity and mortality if not adequately treated.10,11 Because GTH can occur with normal vital signs, it has been termed “cryptic shock.”12 GTH or cardiovascular insufficiency is a significant part of the natural history of sepsis and responsible for the sudden cardiopulmonary deterioration seen in 12% to 21% of patients.13,14 EGDT is associated with a 50% reduction in this adverse event, an issue not addressed by Jones et al.6
Figure 1.
The hemodynamic phases of sepsis. DO2 = systemic oxygen delivery; NI = normal; SvO2 = mixed venous oxygen saturation; VO2 = oxygen consumption. Reprinted with permission from Kruse.8
Table 1.
—Hemodynamic Phases of Sepsis
| Stage | Hemodynamic Picture | SBP | CVP | Treatment and Comments |
| B | Hypovolemia | Variable | ↓ | Volume |
| Myocardial suppression | Variable | ↑ | Correct anemia, inotropic therapy | |
| A | Resuscitated, compensated, and vasodilatory | Variable | Normal | Vasopressors, low-dose corticosteroids |
| C | Supranormal Do2 dependency | Variable | ↑ to normal | Increased o2 after augmentation of Do2 |
| D | Impairment of tissue O2 utilization | Variable | Normal | r-APC |
| Decreased o2 | Variable | Normal | Resuscitated |
CVP = central venous pressure; Do2 = systemic oxygen delivery; r-APC = recombinant activated protein C; SBP = systolic BP; SvO2 = mixed venous oxygen saturation; o2 = oxygen consumption.
With adequate volume therapy and myocardial reserve, a hyperdynamic or compensated phase follows. During this compensated phase, Do2 is in the normal or elevated range, systemic oxygen consumption (o2) is increased, and vascular resistance is generally decreased. In contrast to the hypodynamic phase (patients in the Rivers et al1 study), Jones et al6 enrolled patients in this phase with a lower systolic BP, normal central venous pressure (CVP), normal Scvo2, lower lactate levels, and triple the frequency of vasopressor dependence (Fig 1; Tables 1, 2). These patients also had corresponding Simplified Acute Physiology Score II scores and predicted mortality that was nearly 14% lower than that in patients receiving EGDT (34.8% vs 48.4%) and other studies.2
Table 2.
| Jones et al6 |
Rivers et al1 |
|||
| Lactate Clearance | Scvo2 Guided | Standard Therapy | EGDT | |
| Comorbidities | ||||
| Congestive heart failure | … | … | 30.2 | 36.7 |
| Coronary artery disease | … | … | 23.5 | 26.5 |
| Liver disease | … | … | 23.5 | 23.1 |
| Alcohol use | … | … | 38.7 | 38.5 |
| Baseline hemodynamics | ||||
| Lactate,a mmol/L | 3.9±3.1 | 4.2±3.1 | 6.9±4.5 | 7.7±4.7 |
| CVP,a mm Hg | 11±6.5 | 11±6.2 | 6.1±7.7 | 5.3±9.3 |
| Systolic BP,a mm Hg | 91±24.6 | 92±21.0 | 109±34 | 106±36 |
| Scvo2a | … | 74±12.3 | 49.2±13.3 | 48.6±11.2 |
| Treatments (0-6-h ranges) | ||||
| RBC transfusions | 7 | 3 | 18.5 | 64.1 |
| P Value | .2 | … | < .001 | … |
| Vasopressorsa | 72 | 75 | 30.3 | 27.4 |
| Inotropes | 3 | 5 | 0.8 | 13.7 |
| P Value | .57 | … | < .001 | … |
| Mechanical ventilationa | 27 | 26 | 53.8 | 53.0 |
| 6 h hemodynamics | ||||
| Lactate, mmol/L | … | … | 4.9±4.7 | 4.3±4.2 |
| P Value | .01 | |||
| Lactate clearance (0-6 h) | … | … | 29 | 44.2 |
| P Value | .01 | |||
| CVP, mm Hg | … | … | 11.8±6.8 | 13.8±4.4 |
| P Value | .007 | |||
| Scvo2 | … | … | 66.0±15.5 | 77.3±10.0 |
| P Value | < .001 | |||
| Sudden cardiopulmonary collapse | … | … | 21.0 | 10.3 |
| P Value | .02 | |||
| SAPS II scores (baseline)a | 44.8±18.4 | 44.1±17.3 | 48.8±11.1 | 51.2±11.1 |
| Predicted mortality (approximate) | 34.8 | 32.8 | 48.4 | 48.7 |
| Actual in-hospital mortality | 23 | 17 | 46.5 | 30.5 |
| P Value | NS | … | .009 | … |
Data are presented as mean ± SD or %. EGDT = early goal-directed therapy; NS = not significant; SAPS = Simplified Acute Physiology Score; Scvo2 = central venous oxygen saturation. See Table 1 legend for expansion of other abbreviations.
No statistical significance.
Pathological Do2 dependency is a result of a progressive impairment of OER, which is accompanied by a markedly increased Scvo2/Svo2 (venous hyperoxia) and a hyperdynamic circulation. When Do2 is insufficient, o2 decreases, and increased lactate levels accompany venous hyperoxia. The phase of tissue dysoxia can be the result of microcirculatory dysfunction causing maldistribution of blood flow or mitochondrial dysfunction with defects in substrate utilization. In this phase, improvement in Do2 may not result in improvement in o2.
Sepsis may consist of four hemodynamic phases where a decreased Scvo2/Svo2 always precedes the appearance of lactate, making them complementary and nonexclusive end points, (Fig 1, Table 1). These hemodynamic phases are not always distinct and may overlap depending on the timing and quality of the resuscitation. By characterizing these phases in hemodynamic outcome studies, future trials can be conducted with the appropriate research design and interpreted with clarity, facilitating generalizability and external validation in clinical management.15
Lactate Kinetics Are Complex and Limit the Interpretation of Lactate Levels and Lactate Clearance in the Individual Patient
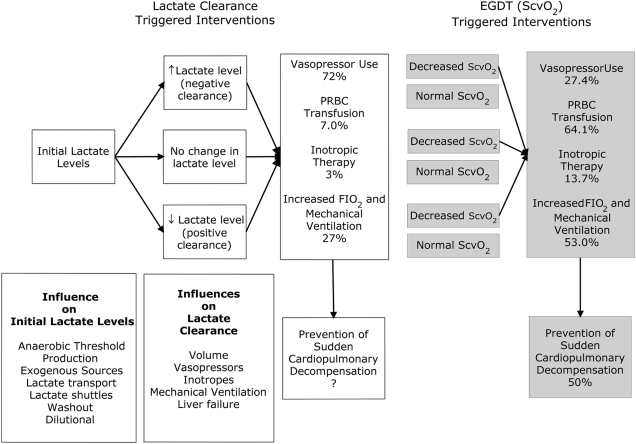
Lactate elevation may indicate stress-induced upregulation in epinephrine-stimulated sodium-potassium adenosine triphosphatase activity in skeletal muscle and inhibition of pyruvate metabolism rather than, or in addition to, the traditionally implicated cellular hypoxia. Other confounding influences may include exogenous lactate sources (Ringers lactate or packed RBC transfusions), lactate shuttles and transport, delayed washout from underperfused tissue, variable lactate clearance by a number of organs, and dilution (large-volume resuscitations) (Fig 2). These interactions are not in a steady state and depend on the pathophysiology, timing, and quality of the resuscitation in the individual case.16
Figure 2.
The kinetics, diagnostic, and therapeutic clinical scenarios of lactate. EGDT = early goal-directed therapy; PRBC = packed RBC; ScvO2 = central venous oxygen saturation. See Figure 1 legend for expansion of other abbreviation.
Normal lactate levels occur in up to 45% of cases of septic shock, and although there is significant variability, the associated mortality can be up to 52%.9,17-19 In fact, many patients develop multisystem organ failure and die without ever having increased lactate levels.9 Thus, lactate has limitations as a tool for risk stratification and as a guide for resuscitation in individual patients. In the Jones et al6 study, the lactate clearance goal was at least 10% at ≥2 h or normality of both initial and subsequent lactates. Nguyen et al,20 however, found an optimal lactate clearance cutoff of <10% after 6 h of intervention to have a sensitivity of 44.7%, specificity of 84.4%, and accuracy of only 67.6% for predicting in-hospital mortality. Additionally, lactate clearance was less predictive of outcome in septic shock, the predominant feature of the patients in the Jones et al6 study. Because of the variable expression of lactate, its complicated kinetics, and the limited accuracy of lactate clearance, Nguyen et al20 did not recommend lactate clearance as a sole therapeutic end point. Serum lactate levels may rise or fluctuate during therapy. Of patients with increased initial lactate levels, 41% have delayed peak values (20±12 h) after the initial presentation.11,17 Of patients with normal initial lactates, 15% will later demonstrate elevations. These patients have abnormal Scvo2 (66.7%±8.6%) at baseline compared with their counterparts with normal levels.17 Lactate levels over time can increase (negative clearance), stay the same, or decrease (positive clearance) after intervention (Fig 2). Not only is the direction of clearance important but also the magnitude of change. There are significantly different clinical and outcome implications in patients whose lactate levels decrease from 10 to 9 mmol/L vs 4 to 3.6 mmol/L. Although both represent clearance of 10%, the implications for illness severity and prognostic significance are much different.
What if the Patient Requires More Than Fluid and Vasopressors and the Lactate Is Still High?
Optimization of preload (CVP) and afterload (mean arterial pressure) were addressed by Jones et al6; however, the remaining components of EGDT, including optimizing Do2 (oxygen carrying capacity [supplemental oxygen and hemoglobin], cardiac output) and decreasing o2 (mechanical ventilation and sedation) to prevent delayed cardiopulmonary complications, were not elicited or examined.15 Over the past decade, numerous studies have validated the clinical utility of Scvo2 in recognizing supply dependency, need for a transfusion, detection of myocardial dysfunction, response to oxygen and mechanical ventilation, early cardiopulmonary complications, and overall influence on mortality. To establish noninferiority, lactate clearance has to be appropriately examined in these scenarios in order to be generalizable to all hemodynamic phases of sepsis and these facets of care.7 The discrepancy between Scvo2-triggered interventions in the Rivers et al1 study vs the 30 interventions (10% of patients) guided by lactate clearance reflects significant differences in hemodynamic phases, patient populations, and frequency and timing of interventions (Fig 2). This undermines the conclusion of equivalency from a noninferiority research design.7 Patients more likely to require inotropes (congestive heart failure or coronary artery disease) or patients with reduced lactate clearance (liver failure) were not described by Jones et al6 (Table 2). This lower number of interventions reflects a lower illness severity compared with other studies,2 the possibility of poor compliance to the protocol, or a study design that is not equivalent to EGDT. The threefold greater use of vasopressors by Jones et al6 may have resulted in higher lactate levels (catecholamines), CVP (increased afterload and venous tone), and Scvo2 (decreased OER). As a result, triggers for more fluid administration, RBC transfusion, inotropes, and mechanical ventilation may have been obscured by catecholamines. In this vasodilatory phase of sepsis, one would expect a higher use of corticosteroids3; however, they were only used in 37% and 35% of eligible patients in the lactate clearance and Scvo2 groups, respectively.
Real-World Clinical Practice
Central venous catheterization is recommended for patients with septic shock, and this was indeed the practice in the Jones et al6 study. However, this study often is misinterpreted to imply that lactate clearance precludes the need for central venous catheterization altogether. This could result in a delay in a safer route for administration of vasopressors and achievement of EGDT goals within 6 h. The Surviving Sepsis Campaign recommendations include intermittent or continuous Scvo2 sampling.3 It is a simple matter to add intermittent Scvo2 to lactate measurements in the absence of continuous monitoring. Bundle compliance and socioeconomic costs improve significantly with continuous monitoring.21
Conclusions
Scvo2 provides immediate feedback to the o2/Do2 relationship but requires interpretation that depends on the phase of sepsis. Lactate is a delayed indicator of tissue perfusion and is subject to complex kinetics that are never clear in the individual case. Lactate levels may be normal or fluctuate, leading to inappropriate risk stratification and therapy. Lactate clearance and Scvo2, therefore, are complementary and not mutually exclusive end points.
Footnotes
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: In the past 3 years, Dr Rivers has received funding from the National Institutes of Health, Aggennix AG, and Alere Corporation. He has been a one-time consultant for Aggennix AG; Eisai Co, Ltd; Idaho Technologies Inc; AstraZeneca; Massimo; and Sangard. He is a consultant to the Institute of Medicine, National Academies. The EGDT study was performed without external industry support or funding of any kind. Any intellectual properties associated with Dr Rivers’ research are exclusively owned by Henry Ford Hospital. Dr Rivers holds no past or present intellectual properties and has never received royalties or stock interest related to technologies in EGDT research and practice. Dr Elkin has received funding from the Gordon and Betty Moore Foundation, been a one-time consultant for Eisai Co, Ltd, and participated on the speaker’s bureau for Edwards Lifesciences LLC on three occasions. Dr Cannon has been a one-time consultant for Aggennix AG and Eisai Co, Ltd.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
Contributor Information
Emanuel P. Rivers, Detroit, MI.
Ronald Elkin, San Francisco, CA.
Chad M. Cannon, Kansas City, KS.
References
- 1.Rivers E, Nguyen B, Havstad S, et al. Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 2.Rivers EP. Point: adherence to early goal-directed therapy: does it really matter? Yes. After a decade, the scientific proof speaks for itself. Chest. 2010;138(3):476–485. doi: 10.1378/chest.10-1405. [DOI] [PubMed] [Google Scholar]
- 3.Dellinger RP, Levy MM, Carlet JM, et al. International Surviving Sepsis Campaign Guidelines Committee; American Association of Critical-Care Nurses; American College of Chest Physicians; American College of Emergency Physicians; Canadian Critical Care Society; European Society of Clinical Microbiology and Infectious Diseases; European Society of Intensive Care Medicine; European Respiratory Society; International Sepsis Forum; Japanese Association for Acute Medicine; Japanese Society of Intensive Care Medicine; Society of Critical Care Medicine; Society of Hospital Medicine; Surgical Infection Society; World Federation of Societies of Intensive and Critical Care Medicine. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen HB, Rivers EP, Knoblich BP, et al. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32(8):1637–1642. doi: 10.1097/01.ccm.0000132904.35713.a7. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen HB, Loomba M, Yang JJ, et al. Early lactate clearance is associated with biomarkers of inflammation, coagulation, apoptosis, organ dysfunction and mortality in severe sepsis and septic shock. J Inflamm (Lond) 2010;7:6. doi: 10.1186/1476-9255-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA Emergency Medicine Shock Research Network (EMShockNet) Investigators. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303(8):739–746. doi: 10.1001/jama.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJ CONSORT Group. Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement. JAMA. 2006;295(10):1152–1160. doi: 10.1001/jama.295.10.1152. [DOI] [PubMed] [Google Scholar]
- 8.Kruse J. Lactic acidosis, part 1: understanding pathogenesis and causes. As mechanisms are elucidated, some assumptions are being revised. J Crit Illness. 1999;14(8):456–466. [Google Scholar]
- 9.Levraut J, Ichai C, Petit I, Ciebiera JP, Perus O, Grimaud D. Low exogenous lactate clearance as an early predictor of mortality in normolactatemic critically ill septic patients. Crit Care Med. 2003;31(3):705–710. doi: 10.1097/01.CCM.0000045561.85810.45. [DOI] [PubMed] [Google Scholar]
- 10.Astiz ME, Rackow EC, Kaufman B, Falk JL, Weil MH. Relationship of oxygen delivery and mixed venous oxygenation to lactic acidosis in patients with sepsis and acute myocardial infarction. Crit Care Med. 1988;16(7):655–658. doi: 10.1097/00003246-198807000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Rivers EP, Kruse JA, Jacobsen G, et al. The influence of early hemodynamic optimization on biomarker patterns of severe sepsis and septic shock. Crit Care Med. 2007;35(9):2016–2024. doi: 10.1097/01.ccm.0000281637.08984.6e. [DOI] [PubMed] [Google Scholar]
- 12.Rady MY, Rivers EP, Nowak RM. Resuscitation of the critically ill in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. Am J Emerg Med. 1996;14(2):218–225. doi: 10.1016/s0735-6757(96)90136-9. [DOI] [PubMed] [Google Scholar]
- 13.Brun-Buisson C, Doyon F, Carlet J, et al. French ICU Group for Severe Sepsis. Incidence, risk factors, and outcome of severe sepsis and septic shock in adults. A multicenter prospective study in intensive care units. JAMA. 1995;274(12):968–974. [PubMed] [Google Scholar]
- 14.Carr GE, Edelson DP, Yuen TC, et al. In-hospital cardiac arrest among patients with coexisting pneumonia: a report from the American Heart Association’s Get With The Guidelines–Resuscitation Program. Am J Respir Crit Care Med. 2011;183:A6339. [Google Scholar]
- 15.Sevransky JE, Nour S, Susla GM, Needham DM, Hollenberg S, Pronovost P. Hemodynamic goals in randomized clinical trials in patients with sepsis: a systematic review of the literature. Crit Care. 2007;11(3):R67. doi: 10.1186/cc5948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mizock BA. The hepatosplanchnic area and hyperlactatemia: A tale of two lactates. Crit Care Med. 2001;29(2):447–449. doi: 10.1097/00003246-200102000-00047. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez G, Castro R, Romero C, et al. Persistent sepsis-induced hypotension without hyperlactatemia: is it really septic shock? J Crit Care. 2010;26(4):435.e9–e14. doi: 10.1016/j.jcrc.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Dugas A, Joyce N, et al. Prevalence and characteristics of non-lactate and lactate expressors in septic shock [abstract] Crit Care Med. 2009;37:A227. doi: 10.1016/j.jcrc.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cannon CM Multicenter Severe Sepsis and Septic Shock Collaborative Group. The GENESIS Project (GENeralization of Early Sepsis InterventionS): a multicenter quality improvement collaborative. Acad Emerg Med. 2010;17(11):1258. [Google Scholar]
- 20.Nguyen HB, Rivers EP, Havstad S, et al. Critical care in the emergency department: a physiologic assessment and outcome evaluation. Acad Emerg Med. 2000;7(12):1354–1361. doi: 10.1111/j.1553-2712.2000.tb00492.x. [DOI] [PubMed] [Google Scholar]
- 21.Ising P, Smith TW, Simpson SQ. Effect of intermittent vs continuous ScvO2 monitoring on sepsis bundle compliance and mortality [abstract] Chest. 2009;136(4):21S. [Google Scholar]