Abstract
Objective
We describe a collaboration between the graduate medical education office and the Henry Ford Health System's Office of Clinical Quality and Safety to create an institution-wide communication skills curriculum pertinent to the institution's safety and patient- and family-centered care initiatives.
Methods
A multidisciplinary committee provided oversight for the curriculum design and used sentinel event and other quality and safety data to identify specific target areas. The curriculum consisted of 3 courses: “Informed Consent,” “Sharing Bad News,” and “Disclosure of Unanticipated Events.” Each course included 3 components: a multimedia online module; small group discussions led by the program director that focused on the use of communication scripts; and 2 objective structured clinical examinations (OSCEs) requiring residents to demonstrate use of the communication scripts. All first-year residents (N = 145) and faculty (N = 30) from 20 residency programs participated in this initiative. Evaluation of the residents consisted of a self-assessment; the standardized patients' assessment of the residents' performance; and faculty assessment of resident performance with verbal feedback.
Results
Survey data showed that residents found the courses valuable, with residents identifying communication scripts they would use in clinical settings. Focus groups with faculty highlighted that the resident debriefing sessions provided them with insight into a resident's communication skills early in their training.
Conclusion
Our institutional curriculum was developed in a collaborative manner, and used an evidence-based approach to teach communication skills relevant to institutional safety and quality initiatives. Other institutions 5 wish to adopt our strategy of departmental collaboration and alignment of resident education with institutional initiatives.
Editor's Note: The online version of this article contains a detailed description of the 3 courses developed in this curriculum: Informed Consent, Sharing Bad News, and Disclosure of Unanticipated Events (25KB, doc) . The authors/HFHS are agreeable to sharing this curriculum in a collaborative partnership with other institutions.
Background
Physician communication is an important component of effective patient care.1–4 The Accreditation Council for Graduate Medical Education (ACGME) mandates that residency programs teach and assess residents' interpersonal and communication skills during training.5 The Joint Commission, along with other national quality and safety organizations, now requires hospitals to provide patient- and family-centered care, disclose errors, develop standardized handoff strategies, and use translators for non-English–speaking patients.6 This environment offers rich opportunities to design institutional curricula in communications skills for residents that link ACGME accreditation mandates with national safety and patient- and family-centered care initiatives.
A variety of strategies have been offered for teaching these communication skills;7–11 recommendations include using “teach back” during informed consent,12,13 adopting standardized handoff techniques to enhance the communication of critical patient information during transitions of care,12 and disclosing unanticipated events and errors to patients and their families.11 Residency program directors and faculty often feel challenged to teach communication skills because historically they have not been trained to teach this competency domain.14 In this article we describe the collaboration between Henry Ford Health System (HFHS) Graduate Medical Education (GME) Office and the Office of Clinical Quality and Safety (OCQS) in creating an institution-wide communication skills curriculum for 20 diverse residency programs that addressed HFHS safety initiatives. Our curriculum adapted existing online multimedia modules developed by OCQS and was aligned with institutional initiatives to ensure sustainability.
Methods
Needs Assessment
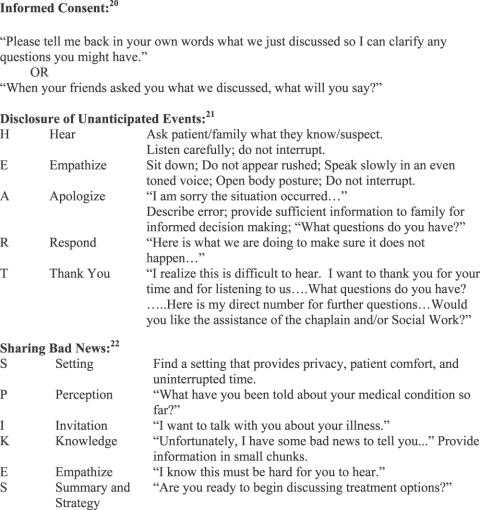
In 2008, HFHS launched the “No Harm Campaign” designed to reduce harm events throughout the system by 50% over the course of 3 years. A multidisciplinary committee comprising residents, program directors, and representatives from quality and safety, nursing education, service excellence, and GME was formed. The committee agreed that courses consisting of an OCQS multimedia online module, small group discussion, and OSCE experience should be developed for the topics of “Informed Consent,” “Disclosure of Unanticipated Events,” and “Sharing Bad News” because those topic areas linked directly to the HFHS No Harm Campaign. The curriculum was mandatory for first-year residents in 20 residency programs (N = 145) and used communication scripts to teach these skills to residents (figure). Program director buy-in was obtained by demonstrating a clear link to ACGME accreditation standards and by engaging them in the initial design process.
FIGURE.
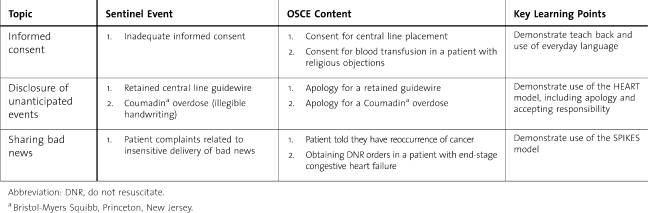
Example Communication Scripts
A literature review revealed OSCEs were one of the most effective ways to measure communication skills; therefore, we established a partnership with Wayne State University Standardized Patient Program to provide standardized patients.15,16 The OSCE scenarios were adapted from sentinel events at HFHS and focused on key communication issues that occurred in the 3 identified areas (table 1). Residents completed a course evaluation form, and at the conclusion of the 3 courses, representative faculty from each program (N = 30) attended 1 of 3 hour-long focus groups during which they discussed the strengths and weakness of the 3 courses. The HFHS Institutional Review Board (IRB) approved this retrospective analysis.
TABLE 1.
Examples of Objective Structured Clinical Examination (OSCE) Scenarios
Overview of Curriculum Design and Content
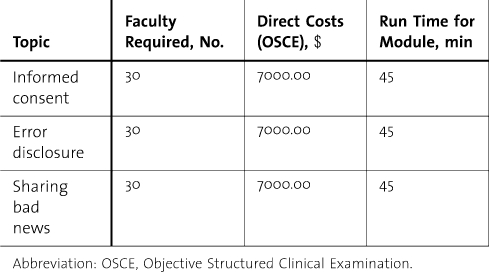
Within a week after completing the OCQS multimedia module, residents participated in a program-director–led small group discussion and completed 2 OSCE cases. The small group discussions focused on specialty-specific scenarios related to the 3 course topics and engaged the learner and faculty in more deliberate learning around the communication skill sets (table 1). The courses were given in a specific sequence (Informed Consent, Disclosure of Unanticipated Events, and Sharing Bad News), in keeping with the concept that teaching communication scripts provides novices with a framework for difficult conversations.17 The time frame for completing all 3 courses varied depending on space in our simulation center and program schedules. table 2 displays feasibility information.
TABLE 2.
Feasibility of Institutional Curriculum
What was known
Communicating with patients about informed consent, “bad news,”? and unanticipated events are critical skills for physicians.
What is new
An institution-wide communication skills curriculum includes modules for these circumstances.
Limitations
Outcomes are limited to resident acceptance of the curriculum.
Bottom line
Other institutions 5 consider adopting or adapting this evidence-based curriculum relevant to quality and patient safety.
Assessment
The OSCE cases were generic to allow residents from 20 different specialties to use the communication script. The OSCE scenarios were adapted from sentinel events that occurred at HFHS (table 3). After each OSCE, residents completed a self-assessment using the Kalamazoo Essential Elements Communication Checklist (Adapted) (KEECC-A).18 Standardized patients also assessed resident performance and provided verbal feedback by using the KEECC-A. During the debriefing session, faculty completed the KEECC-A on the resident's performance. The results have been described in an earlier article.19 The resident's faculty mentor was able to review all assessments and discuss with the resident their performance and opportunities for improvement. This provided faculty with critical knowledge of each resident's communication skills early in the first year.
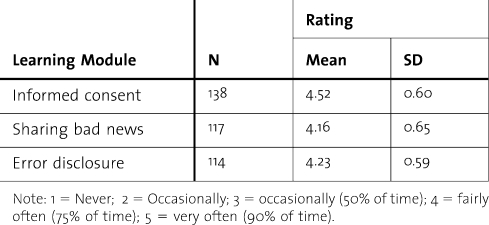
TABLE 3.
Residents' Effectiveness Ratings for 3 Learning Modules
The KEECC-A was chosen to evaluate residents' communications skills because of its established reliability and validity in measuring communication skills.19 After completion of the 3 modules, program directors received a portfolio containing each resident's average score on the OSCE, departmental average, and an institutional average.
Faculty Development
Faculty development sessions were offered to assist faculty (N = 30) in understanding more deeply the initiative and assessment tool. Faculty were provided debriefing guides containing key learning points to emphasize the importance of accurate ratings and behavioral anchors for the KEECC-A to help them accurately rate residents. They reported that the facilitator and debriefing guides were the most helpful components because they provided them with explicit talking points and responses to possible questions from the residents.
Results
Program Evaluation and Improvement
Qualitative and quantitative methods were used for curricular evaluation and improvement. Residents (N = 138) completed a course evaluation after each of the modules launched in the 2008–2009 academic year, using separate 11-item scales for each of 3 modules: Informed Consent, Bad News, and Error Disclosure. Residents rated the effectiveness of the components of each module by using a 7-item questionnaire with a Likert scale. Four additional questions asked residents to estimate how frequently they would use the skill addressed in the module and to estimate their skill before and after the module.
Residents' mean ratings of the effectiveness of the entire curriculum was 4.32 (SD = 0.49) on a 5-point scale. Separate effectiveness ratings for the 3 modules are presented in table 3. Within-subjects ANOVA identified significant differences in residents' mean ratings of the effectiveness of the 3 modules (F2,210 = 24.79, P < .001). Repeated contrasts revealed that residents rated the informed consent module higher than the error disclosure module (P < .001); however, there was no significant difference in effectiveness ratings of the error disclosure versus bad news modules (P = .07).
Paired samples t tests revealed significant improvements in residents' self-assessment of their skills for each module (table 4). Residents consistently reported a greater sense of skill and knowledge across the domains after completing the modules. Furthermore, residents indicated that they would frequently use the skill addressed by each module (table 5), and specifically, that they would use the informed consent techniques on nearly a daily basis.
TABLE 4.
Comparison of Residents' Mean Self-Ratings of Their Knowledge/Skill Before Versus After 3 Learning Modules (Course Evaluation Data)
TABLE 5.
Residents' Ratings of How Frequently They Will Use the Skill Addressed in Each Module
Focus groups with teaching faculty provided additional qualitative data. Faculty reported, in general, that the 3 modules were valuable and the use of communication scripts helped residents develop language for challenging conversations. Faculty also gained insight into residents' communication skills, since these courses were given early during the first year. Faculty reported that they learned new information about key communication scripts and skills as a result of teaching the course. Scheduling the educational module was the faculty's biggest challenge and they suggested paying more careful attention to scheduling to accommodate clinic schedules. In addition, faculty recommended that 2 OSCEs per module were sufficient for the resident's exposure to the communication scripts.
Discussion
This article highlights a successful multidisciplinary collaboration between HFHS GME and the OCQS to develop unique curricula that reflect broader institutional and national agendas related to quality of care, patient safety, and interpersonal and communication skills. Curricular components adapted OCQS multimedia modules and added a small group discussion and a set of OSCEs. Communication scripts offered residents the necessary language for these conversations. Residents found these courses valuable. The curriculum allowed faculty to deepen their knowledge and skills in teaching communication skills, and faculty found these educational modules valuable, and the debriefing sessions provided them with insight into residents' communication skills early in their training.
The development and implementation of this curriculum provided a variety of important lessons. The incorporation and utilization of existing resources within HFHS opened doors to increased collaboration between GME and other departments within the hospital. The process of launching an institutional curriculum was initially daunting, but by paying attention to details, incorporating early feedback from program directors, and customizing education to the medical culture through the use of small group discussion and faculty teachers, we were able to achieve early successes. Developing educational experiences that linked directly to ACGME accreditation requirements was a “win” for program directors. This initiative also increased resident familiarity with institutional initiatives in the areas of quality and safety and patient- and family-centered care. Future research initiatives will be tied to identifying appropriate direct observation experiences that can link this training directly to residents' bedside performances.
This curriculum was launched within the context of a health care system supportive of quality and safety initiatives and resident education. The lack of such system-wide infrastructure or leadership support 5 make launching an institutional curriculum daunting and 5 limit the generalizability of this study in other institutions. Other institutions 5 consider reducing interdepartmental silos by collaborating with others to capitalize on existing resources. The infrastructure will be different at each institution, but other institutions 5 wish to adopt our strategy of collaborating across departments to use existing institutional educational resources and aligning resident education with institutional initiatives.
Footnotes
Barbara L. Joyce, PhD, is Associate Professor of Biomedical Science and Director of Curriculum Evaluation at Oakland University William Beaumont School of Medicine. She was at Henry Ford at the time of writing of this article; Eric Scher, MD, is Chair Internal Medicine Henry Ford Health System; Vice President of Medical Education Henry Ford Health System; Designated Institutional Official and Clinical Associate Professor in Internal Medicine at Wayne State University; Timothy Steenbergh, PhD, is Professor of Psychology at Indiana Wesleyan University in Marion; and Mary J. Voutt-Goos, BScN, RN, CCRN, is Director of Patient Safety Initiatives, Clinical Care Design, Office of Clinical Quality and Safety, at Henry Ford Health System.
Funding: This project was funded by Henry Ford Hospital Department of Medical Education and no outside funding was received.
References
- 1.Chen JY, Tao ML, Tisnado D, et al. Impact of physician-patient discussions on patient satisfaction. Med Care. 2008;46(11):1157–1162. doi: 10.1097/MLR.0b013e31817924bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schoenthaler A, Chaplin WF, Allegrante JP, et al. Provider communication effects medication adherence in hypertensive African Americans. Patient Educ Couns. 2009;75(2):185–191. doi: 10.1016/j.pec.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heisler M, Tierney E, Ackermann RT, et al. Physicians' participatory decision-making and quality of diabetes care processes and outcomes: results from the triad study. Chronic Illn. 2009;5(3):165–176. doi: 10.1177/1742395309339258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Accreditation Council of Graduate Medical Education. Common Program Requirements. http://www.acgme.org/outcome/comp/compCPRL.asp. Accessed 10 30, 2010. [Google Scholar]
- 6.The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient-and Family-Centered Care: A Roadmap for Hospitals. Oakbrook Terrace, IL: The Joint Commission; 2010. [Google Scholar]
- 7.Kaldjian LC, Jones EW, Wu BJ, Forman-Hoffman VL, Levi BH, Rosenthal GE. Disclosing medical errors to patients: attitudes and practices of physicians and trainees. J Gen Intern Med. 2007;22(7):988–996. doi: 10.1007/s11606-007-0227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClean KL, Card SE. Informed consent skills in internal medicine residency: how are residents taught, and what do they learn. Acad Med. 2004;79(2):128–133. doi: 10.1097/00001888-200402000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Phipps LL, Cuthill JD. Breaking bad news: a clinician's view of the literature. Ann R Coll Physicians Surg Can. 2002;35(5):287–293. [PubMed] [Google Scholar]
- 10.Sherman HB, McGaghie WC, Unti SM, Thomas JX. Teaching pediatrics residents how to obtain informed consent. Acad Med. 2005;80(10 suppl):S10–S13. doi: 10.1097/00001888-200510001-00006. [DOI] [PubMed] [Google Scholar]
- 11.White AA, Bell SK, Krauss MJ, et al. How trainees would disclose medical errors: educational implications for training programmes. Med Educ. 2011;45(4):372–380. doi: 10.1111/j.1365-2923.2010.03875.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Quality Forum. Safe Practices for Better Health Care-2010 Update: A Consensus Report. Washington, DC: NQF; 2010. [Google Scholar]
- 13.Wu H, Nishimi R, Page-Lopez C, Kizer K, editors. Improving Patient Safety Through Informed Consent for Patients with Limited Health Literacy. Washington, DC: National Quality Forum; 2005. [Google Scholar]
- 14.Perron NJ, Sommer J, Hudelson P, et al. Clinical supervisors' perceived needs for teaching communication skills in clinical practice. Med Teach. 2009;31(7):e316–e322. doi: 10.1080/01421590802650134. [DOI] [PubMed] [Google Scholar]
- 15.Accreditation Council of Graduate Medical Education. ACGME/ABMS toolbox of assessment methods. http://www.acgme.org/Outcome/assess/Toolbox.pdf. Accessed 4 13, 2011. [Google Scholar]
- 16.Duffy FD, Gordon GH, Whelan G, et al. Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med. 2004;79(6):495–507. doi: 10.1097/00001888-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Headly A. Communication skills: a call for teaching to the test. Am J Med. 2007;120(10):912–915. doi: 10.1016/j.amjmed.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 18.Rider EA, Nawotniak RH, Smith G. A Practical Guide to Teaching and Assessing the ACGME Core Competencies. Marblehead, MA: HCPro, Inc: 2007. pp. 1–85. [Google Scholar]
- 19.Joyce B, Steenbergh T, Scher E. Use of the Kalamazoo Essential Elements Communication Checklist (Adapted) in an Institutional Interpersonal and Communication Skills Curriculum. J Grad Med Educ. 2010;2(2):165–169. doi: 10.4300/JGME-D-10-00024.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss B. Health Literacy and Patient Safety: Helping Patients Understand. Chicago, IL: AMA Foundation; 2007. [Google Scholar]
- 21.Williamson S. Tools for building satisfied patients. Inside Duke. 2004;13(7):1–3. [Google Scholar]
- 22.Baile W, Buckman R, Lenzi R, Glober G, Beale E, Kudelk A. SPIKES—a six step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]