Abstract
Background
The Accreditation Council for Graduate Medical Education 2011 duty hour standards became effective on 7 1, 2011. One of the new standards allows residents to exceed the limit on continuous duty hours in unusual circumstances relating to patient or family need or rare educational opportunities. There are no data about how often or in what circumstances residents would consider exceeding their duty hour limits using this new provision in the standards. We surveyed internal medicine residents to explore these questions.
Methods
We conducted an anonymous cross-sectional survey of internal medicine residents at a midwestern tertiary-care hospital to determine how often they had considered exceeding duty hour limits in the preceding 2 weeks. We analyzed responses using descriptive statistics and χ2 tests for comparisons.
Results
We obtained responses from 51 of 86 residents (59%). Of those residents, 69% (35/51) indicated that they had wanted to exceed duty hour limits at least once in the prior 2 weeks. The most common reason cited was to provide continuity of care for a patient. The 24 + 6–hour rule was the standard most likely to be broken (cited by 66%; 23/35).
Conclusions
Program leadership should anticipate that residents will commonly identify situations in which they will consider exceeding duty hour limits. It will be important to provide guidance to residents early in the year about the situations that would be appropriate for the application of this new standard.
Editor's note: The online version of this article contains the survey instrument used in this study (29KB, doc) .
Introduction
The Accreditation Council for Graduate Medical Education (ACGME) duty hour standards1 that went into effect on 7 1, 2011, included language that allows residents to decide whether they will exceed the limit on continuous duty hours when their presence is “required for continuity for a severely ill or unstable patient, academic importance of the events transpiring, or humanistic attention to the needs of a patient or family.”1(p17),2 Residents must hand over care of all of their other patients, attend to only the specific issue or patient for whom they have stayed, and document the situation in writing to their program director. This is a change from the ACGME 2003 standards, which stated that residents 5 be on duty for 24 hours with an additional 6 hours for hand offs and didactics, “24 + 6.”
We sought to explore the potential frequency and reasons residents might exceed their duty hour limits under the ACGME new standards.
Methods
Instrument
We designed the survey instrument around the 2011 ACGME requirement that allows residents to stay beyond duty hour limits in certain situations. We revised the survey based on feedback from within the study group and presented it to a larger group of faculty for readability.
The survey included a cover sheet with the ACGME duty hour requirement verbatim.1 In addition to demographic questions, our instrument (provided as online supplemental material) included 4 questions asking whether and why the respondent had considered staying beyond the duty hours in the previous 2-week period. The study was reviewed and approved by the Institutional Review Board at the Medical College of Wisconsin.
Participants and Setting
We recruited study participants via e-mail, and sent reminders (e-mail, signs in the team rooms, and announcements at the weekly intern and resident meeting) to complete the survey. Between 10 and 12 2010, we surveyed internal medicine and preliminary-year interns and residents at a single tertiary-care hospital affiliated with a freestanding medical college. We included residents rotating in general medicine, cardiology, nephrology, or the intensive care unit; these services typically have 12 to 15 patients. We asked participants to complete our survey one time.
Procedure and Data Analysis
We distributed the surveys over 2 days at least 14 days into each month. The surveys were anonymous, and participants were instructed to place the completed surveys in a box in each team's “team room.” The surveys were picked up within 48 hours after being distributed.
We generated simple descriptive statistics and tested for differences between groups using χ2 analyses. All analyses were performed using Excel (Microsoft Corp., Redmond, WA).
Results
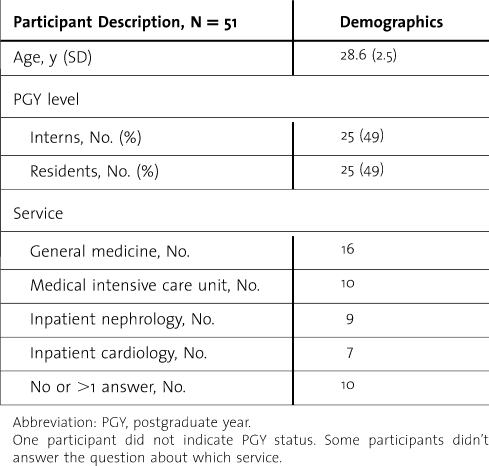
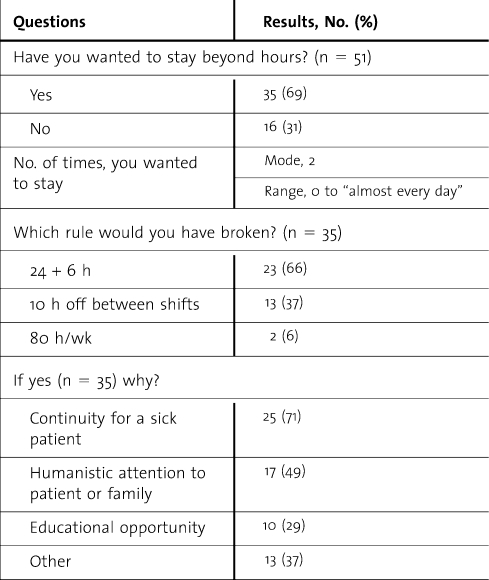
Of 86 residents, 51 participants (59%) completed the survey (table 1). More than two-thirds (69%; 35/51) reported at least one instance in the 2 prior weeks when they wanted to exceed current duty hour limits, with most reporting more than one instance. Most of those who reported wanting to exceed limits (23/35; 66%) would have broken the ACGME 2003 “24 + 6” requirement, although more than half of the respondents would have exceeded more than one restriction. The most common reason (25/35; 71%) for wanting to exceed limits was to provide continuity for an unstable patient (table 2). Although it was not one of the given answer choices in our survey, residents commonly mentioned workload as a reason to exceed limits (11 of 13 who chose “other”; 85%). Level of training was not significantly associated with reporting an episode that made them want to stay (P > .05).
TABLE 1.
Demographics and Participant Description
TABLE 2.
Survey Responses
Discussion
More than two-thirds of participants identified at least one time in the preceding 2 weeks in which they wanted to exceed current duty hour limits. This desire to stay beyond duty hour limits affected interns and residents alike and occurred in all services that we surveyed. Although they should choose to stay beyond their duty hour limits only in “unusual circumstances,”1 residents 5 view these situations as usual circumstances.
The 2011 duty hour limits state that the maximum shift length is 24 + 4 hours for second- and third-year residents, and a strict 16-hour maximum for interns.1 In our study, the requirement that would most often have been violated was the 24 + 6 rule. This suggests that we 5 be underestimating the number of times residents would stay beyond their duty hour limits, given that the new rules are even more restrictive.
The ACGME 2011 duty hour limits respond to the possibility that rigidly preventing interns and residents from acting in a manner they consider best for a patient's care 5 hinder full professional development.2 Our results are consistent with this. The most common reason for wanting to stay beyond duty hour limits was to provide continuity of care for a critically ill patient. These results 5 offer some reassurance to concerns about the effect of the 2003 duty hour reform on residents' professionalism.3,4
Workload also appears to be a common reason cited for staying beyond duty hours. This raises concern about work compression,5 especially give that the admission caps are not changing, even though the maximum shift length for interns is. Having less time to complete the same amount of work could be exacerbated with the new duty hour limits.
Our study limitations include a small sample size and single-site intervention, which limit generalizability. Also, it is possible that respondents who wanted to exceed the limits were more likely to respond. The way that we phrased our questions 5 have influenced the answers that we received. For example, we could have asked the respondents how often they felt that they needed to stay beyond the hour limits. Additionally, we acknowledge that what residents want to do is likely different from what they actually do. We chose not to ask the respondents about actual work hour violations because we did not want to risk having nonresponders based on concern about loss of anonymity with such an admission.
Conclusions
We believe that our results should compel leaders of internal medicine programs to plan for how they will respond to a potentially large number of instances in which residents will want to exceed duty hour limits. It will be important for program directors to offer guidance to residents about when and how to interpret this standard, beginning in orientation. Open discussions between program leadership and residents to come to a common understanding of the program's expectations will be necessary. Continuous tracking and feedback to residents will also be necessary to ensure that this standard is being interpreted appropriately.
Footnotes
Kathlyn E. Fletcher, MD, MA, is Director of the VA Hospitalist Program at the Clement J Zablocki Veterans Administration Medical Center, and Associate Professor of Medicine at the Medical College of Wisconsin; Sarah Nickoloff, MD, is a Palliative Care fellow at the Medical College of Wisconsin; Jeff Whittle, MD, MPH, is a Staff Physician at the Clement J Zablocki Veterans Administration Medical Center, and Professor of Medicine at the Medical College of Wisconsin; Jeffrey L. Jackson, MD, MPH, is the Chief of General Internal Medicine at the Clement J Zablocki Veterans Administration Medical Center, and Professor of Medicine at the Medical College of Wisconsin; Michael Frank, MD, is the Program Director of the Internal Medicine Residency Program and Professor of Medicine at the Medical College of Wisconsin; and at the time of writing Marilyn M. Schapira, MD, MPH, was Professor of Medicine at the Clement J Zablocki Veterans Administration Medical Center, and at the Department of Medicine, Medical College of Wisconsin. She is now at the Department of Medicine at the University of Pennsylvania's Perelman School of Medicine and the Philadelphia VAMC.
Funding: The authors report no external funding source.
References
- 1.Accreditation Council for Graduate Medical Education. Common program requirements. http://www.acgme-2010standards.org/pdf/Common_Program_Requirements_07012011.pdf. Accessed 2 24, 2011. [Google Scholar]
- 2.Nasca T. An open letter to the GME community. 2 2009. http://acgme.org/acWebsite/home/nascalettercommunity2_2009.pdf. Accessed March 23, 2011. [Google Scholar]
- 3.Charap M. Reducing resident work hours: unproven assumptions and unforeseen outcomes [see comments, Ann Intern Med. 2004;140(10):838–839, 141(9):740–742] Ann Intern Med. 2004;140(10):814–815. [PubMed] [Google Scholar]
- 4.Barone JE, Ivy ME. Resident work hours: the five stages of grief [see comment, Acad Med. 2004;79(5):377–378] Acad Med. 2004;79(5):379–380. doi: 10.1097/00001888-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Bellini LM, Katz JT, Fried ED, et al. Beyond duty hour reform: redefining the learning environment. 2009 http://www.im.org/AcademicAffairs/PSI/Documents/09-06-04 Beyond Duty Hour Reform FINAL Report.pdf. Accessed 2 24, 2011. [Google Scholar]