Editor's Note: The ACGME News and Views section of JGME includes data reports, updates, and perspectives from the ACGME and its review committees. The decision to publish the article is made by the ACGME.
Introduction
As a result of the decisions made in the Summer of 2011 to increase the federal debt limit of the United States,1 the Joint Select Committee on Deficit Reduction (the “Super Committee”) was formed to recommend to the Congress by 12 2011 reductions in federal spending to be accomplished over the next 10 years. Among the entitlement program elements being examined by the Super Committee, Medicare reimbursement for Graduate Medical Education (GME), the primary source of GME funding in the United States, has been identified as an opportunity for spending reductions. Specifically, the Medicare Payment Advisory Commission (MedPAC) has indicated that approximately 50% of the Indirect GME Reimbursement is not “empirically justified” on the basis of current costs of teaching hospitals intended to be covered by that reimbursement.2 This is seen by many as an opportunity for reduction. Furthermore, the Simpson Bowles Commission recommended a reduction in total GME funding in excess of 50% ($60 billion over 10 years) as a component of a comprehensive strategy to reduce federal deficit spending.3
This discussion occurs in the context of a predicted physician shortage, a mounting surge in the number of domestic graduates of schools of allopathic and osteopathic medicine designed to remedy that anticipated physician shortage,4 and slow growth in GME output over the past decade.5 However, this increase in medical school output must be accompanied by an increase in Graduate Medical Education, which is the required final pathway to entry into the unsupervised practice of medicine in the United States. As the body charged by the public and the profession with accreditation oversight of the vast majority of the GME programs in the United States, and to measure the quality of educational opportunities for physicians as they seek to prepare to meet the needs of the American public, the Accreditation Council for Graduate Medical Education (ACGME) attempted to estimate the impact of reductions in GME funding of the magnitude under discussion in our nation's capital on the educational pipeline for physicians.
Methods
The ACGME contacted all Designated Institutional Officials (DIOs, respondents) (n = 680) of ACGME accredited residency and fellowship programs by e-mail on 8 16, 2011, and requested that they complete an 18 question survey. Reminder e-mails were sent at approximate 2 week intervals, and the survey closed on 9 16, 2011. The 2 reminder emails urged all sponsoring institutions to participate and stressed the importance of each DIO's response. Programs were assured that individual institutional responses would not be disclosed.
A 128-bit secured website, which ensured the safe transfer of information, provided access to the survey. The survey consisted of 12 forced-choice questions and 6 open-ended questions. The questionnaire is attached to this article in an Appendix. While the reporting window remained open, the DIOs could change their responses at any time. This permitted review of the questions with other institutional leadership before committing to the final submission.
The survey asked DIOs to indicate how future federal funding would affect their institutions' programs and positions. Three different funding scenarios were presented: funding to remain stable at 2011 levels, funding to be reduced by 33%, and funding to be reduced by 50%. DIOs were asked to identify the potential impact on programs and positions under each scenario. Data gathered in the survey were combined with other information (such as size, location, number, and type of programs sponsored), and these were used in the analyses.
To assess the scope of program closures and reduction in positions in each of the 3 scenarios, we weighted the responses numerically. “Slight reductions” were calculated at 10% reduction; and “significant reductions” at 33%. If sponsors indicated they would close all sponsored programs, we assigned a weight of 100% to estimate position reductions. This process allowed us to apply the DIOs' responses to the individual configuration of their particular institutions. Finally, data from respondents were extrapolated to nonresponders based on the type of institution (multisite and single site sponsors), to assess the total impact of funding reductions nationally.
Results
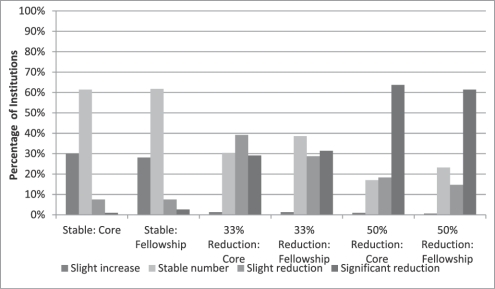
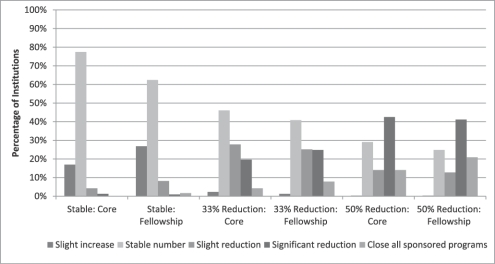
We received complete responses from 306 (45% response rate overall) sponsoring institutions; 236 respondents were from multisite sponsors, representing a 61% response rate in that group. The 306 respondents represent 68.9% of all accredited programs, and 68.4% of all resident positions in the United States in academic year 2011. A total of 118 respondents indicated that their sponsor is a university-based institution. Nearly all responding DIOs (94.8%) indicated that they have been following the discussions in Washington DC regarding reduction in GME funding. The results of the survey can be seen graphically in figures 1 and 2.
FIGURE 1.
Effect on Residency Positions
FIGURE 2.
Effect on Residency Programs
Impact on the number of accredited programs and their positions: stable funding
Were GME funding to remain stable at 2011 levels, the majority of responding sponsors (61%) would sponsor the same number of core (also known as “specialty”) and subspecialty positions. Additionally, 77.5% of these sponsors would keep the same number of core programs and 62.4% would sponsor the same number of subspecialty programs. While very few responding sponsors (1.6%) would close subspecialty programs, 26.8% indicated that they would increase the number of subspecialty programs.
Under this “stable” scenario, a minority of responding sponsors would increase the number of core residency programs (17.0%) and residency positions (30.1%) sponsored. No sponsor reported that they would close core residency programs.
Impact on the number of accredited programs and their positions: 33% reduction
Under this scenario, a majority of responding sponsors (68.3%) would slightly or significantly reduce the number of core residency positions and 60.3% would reduce the number of subspecialty fellowship positions. With this level of funding reduction, 4.3% of responding sponsors would close all core residency programs and 7.8% would close all subspecialty programs. These sponsors represent 339 programs (102 core and 237 subspecialties) and 3934 positions (2783 core and 1151 subspecialty positions). While the number of affected core residency programs is smaller than that of subspecialty programs, the majority of positions lost would be in core residency programs. Of the core residency positions lost, the majority would be in the medical specialties (59.5%).
Impact on the number of accredited programs and their positions: 50% reduction
With a 50% reduction in funding, 82.3% of responding sponsors would slightly or significantly reduce the number of core residency positions, and 76.2% would reduce the number of subspecialty fellowship positions. With this level of funding reduction, 14.0% of responding sponsors would close all core residency programs and 20.9% would close all subspecialty programs. These sponsors represent 538 programs (193 core and 345 subspecialties) and 6630 positions (5003 core and 1627 subspecialty positions). Again, the medical specialties would be most affected (3037 positions).
Alternative Funding
The majority of responding sponsors would seek private funding (45.1%) followed by community or other hospital support (37.2%) and faculty practice plan support (35.9%) to replace or augment reduced federal support for GME.
Measuring the impact on the number of programs and positions
Using the weights described above in Methods (“slightly reduced” at 10%, “significantly reduced” at 33%, and “close all programs” at 100%), we applied these percentages to the number of programs and residency positions represented by the DIOs responding to the survey. Under the 33% reduction scenario, the combined loses in the responding sponsors would be 1136 programs and 13 662 positions.
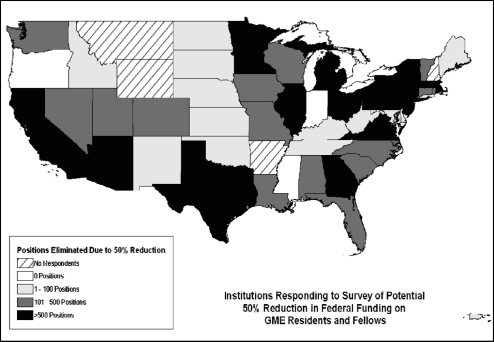
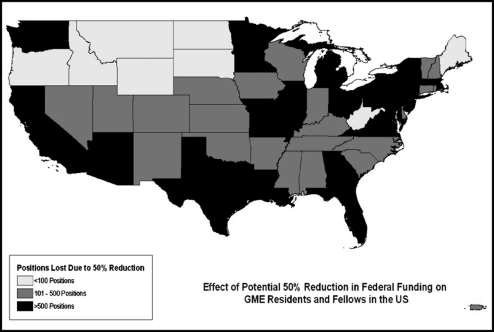
Under the 50% reduction scenario, 1749 programs would close in the responding sponsors, representing 22 411 positions. The closure of programs and loss of positions would vary by state. Significant losses in GME programs and positions would occur across the country. At least 12 states would lose over 500 positions (as shown below in figure 3).
FIGURE 3.
Estimated Reductions in Positions (Resident and Fellow) in Responding
Institutions
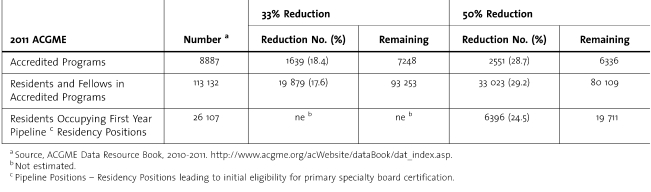
Extrapolating from the 69% sample to the entire population of sponsors, as described in the Methods, we estimate the following reductions in programs and positions. Among all ACGME-accredited programs, we estimate that under the 33% reduction, 1639 programs would close (18.4% of all residency/fellowship programs) and 19 879 positions would be lost. Under the 50% reduction, we estimate that 2551 programs would close, and 33 023 positions (29.2% of all GME positions) would be lost. Using projections from those sponsors who said they would close all programs at their institutions, we estimate that 35.9% of the closing programs would be core residency programs and 24.5% percent of the core residency positions would be lost. The estimated impact on residency and fellowship programs and positions, and specifically pipeline positions, can be seen in table 1.
TABLE 1.
Estimated National Impact of Proposed GME Funding Reductions
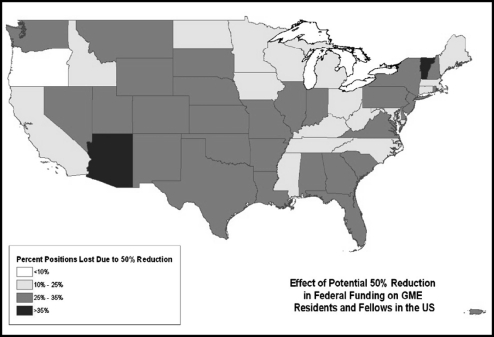
The maps contained in figures 4 and 5 (below) show the estimated impact of a 50% reduction in federal funding by state in residency and fellowship positions lost, and percentage loss of current resident and fellow positions within each state.
FIGURE 4.
Estimated Number of Residency/Fellowship Positions Lost, 50% Reduction in Federal Funding of GME
FIGURE 5.
Estimated Percentage of States' Residency/Fellowship Positions Lost, 50% Reduction in Federal Funding of GME
Discussion
We examined the estimated impact of 3 potential funding scenarios on the magnitude and dimensions of the GME operations of the ACGME-accredited sponsoring institutions in the United States. Collectively in 2011, these 680 institutions sponsor 8887 residency and fellowship programs, and have enrolled 113 132 physicians in training.
The potential impact of such reductions in positions is placed in stark relief when one considers medical school enrollment. The Association of American Medical Colleges projects that in 2020-2021, 20 222 individuals will matriculate into the first-year class across all Liaison Committee on Medical Education accredited medical schools.5 Were a 50% reduction in GME funding to occur, and the 68% sample to be representative of the entire GME effort in the United States, we would have 19 711 positions available for that class when they graduate. This impact is magnified when one considers that currently there are over 2500 graduates of osteopathic medical schools, and over 7100 International Medical Graduates (approximately 3500 of those are US citizens) currently enrolled in ACGME-accredited entry level pipeline positions.6 Finally, the impact of these reductions does not fall solely on states with high numbers of GME programs and positions. The impact will be felt across the entire nation, as can be seen in figures 4 and 5.
The limitations of this study include its response rate. While the respondents represent nearly 70% of all residency and fellowship programs and positions, the response rate is weighted towards sponsors that offer more than one residency or fellowship programs. Thus, it 5 underestimate the impact on small, often rural primary care residency programs, especially in Family Medicine and General Internal Medicine. Other limitations relate to the respondent DIO. Although he/she is the chief academic administrative officer of the GME programs in each sponsor, he/she 5 not have full access to the range of local factors that will influence the decisions to sustain, reduce, or eliminate GME programs and positions in the context of a reduction in federal funding. However, 94.8% of respondents indicated that they had been involved in discussions with colleagues in their institution concerning the impact of funding reductions on the scope and magnitude of the sponsored GME effort.
Finally, the respondents provided comment on the impact of reductions in funding on the patient care mission of the institution (data not shown). Remarks about the safety net, decreased access for the poor or underserved, and ability to care for the underserved with access to the institution indicate that residents continue to serve the public extensively, and often provide access and care to the least advantaged in our society.
The profession, as a component of its responsibility as a public trust, must work with society to assure that we are able to fulfill their expectation of medicine to prepare the next generation of physicians to serve the American public.7
Footnotes
All authors are at the Accreditation Council for Graduate Medical Education (ACGME). Thomas J. Nasca, MD, MACP, is the Chief Executive Officer; Rebecca S. Miller, MS, is the Senior Vice President of Applications and Data Analysis; and Kathleen D. Holt, PhD, is Senior Analyst and Director of Special Projects.
Reference
- 1. The Budget Control Act of 2011. Public Law 112-25 of the 112th United States Congress. Title 4. The Joint Select Committee on Deficit Reduction. http://www.gpo.gov/fdsys/pkg/PLAW-112publ25/pdf/PLAW-112publ25.pdf Last accessed 10/13/2011. [Google Scholar]
- 2. Graduate medical education financing: Focusing on educational priorities. (Chapter 4). Medicare Payment Advisory Commission Report to Congress: Aligning Incentives. 103-122. 6, 2010. Washington, DC. Available at http://www.medpac.gov/chapters/Jun10_Ch04.pdf. [Google Scholar]
- 3. The Moment of Truth. REPORT OF THE NATIONAL COMMISSION ON FISCAL RESPONSIBILITY AND REFORM. Section 3.3.5 Reduce excess payments to hospitals for medical education. Page 37. 12 2010. Available at: http://www.fiscalcommission.gov/sites/fiscalcommission.gov/files/documents/TheMomentofTruth12_1_2010.pdf Last accessed 10/13/2011. [Google Scholar]
- 4.Iglehart J. The Uncertain Future of Medicare and Graduate Medical Education. NEJM 2011. 365(14):1340–1345. doi: 10.1056/NEJMhpr1107519. [DOI] [PubMed] [Google Scholar]
- 5.ACGME Data Resource Book. Academic Year 2010-2011, Chicago, IL. Available at http://www.acgme.org/acWebsite/dataBook/dat_index.asp. Last accessed 10/13/2011. [Google Scholar]
- 6.ACGME Data Resource Book. Academic Year 2010-2011. Chicago, IL. Available at http://www.acgme.org/acWebsite/dataBook/dat_index.asp. Last accessed 10/13/2011. [Google Scholar]
- 7.Nasca T. J. To Teach, Or Not To Teach: GME Financing and the Ethical Implications for all Physicians. Virtual Mentor. in Press [Google Scholar]