Abstract
The four dengue virus (DENV) serotypes cause dengue fever (DF) and dengue hemorrhagic fever/dengue shock syndrome. Although severe disease has been associated with heterotypic secondary DENV infection, most secondary DENV infections are asymptomatic or result in classic DF. The role of cross-reactive immunity in mediating cross-protection against secondary heterotypic DENV infection is not well-understood. DENV infection of interferon-α/β and -γ receptor-deficient (AG129) mice reproduces key features of human disease. We previously demonstrated a role in cross-protection for pre-existing cross-reactive antibodies, maintained by long-lived plasma cells (LLPCs). Here we use a sequential infection model, infecting AG129 mice with DENV-1 followed by DENV-2 6–8 weeks later. We find that increased DENV-specific avidity during acute secondary heterotypic infection is mediated by cross-reactive memory B cells, as evidenced by increased numbers of DENV-1-specific cells by ELISPOT and higher avidity against DENV-1 of supernatants from polyclonally-stimulated splenocytes isolated from mice experiencing secondary DENV-2 infection. However, increased DENV-specific avidity is not associated with increased DENV-specific neutralization, which appears to be mediated by naïve B cells. Adoptive transfer of DENV-1-immune B and T cells into naïve mice prior to secondary DENV-2 infection delayed mortality. Mice depleted of T cells developed signs of disease but recovered after secondary DENV infection. Overall, we found that protective cross-reactive antibodies are secreted by both LLPCs and memory B cells and that both cross-reactive B cells and T cells provide protection against a secondary heterotypic DENV infection. Understanding the protective immunity that develops naturally against DENV infection may help design future vaccines.
Introduction
Dengue, caused by four dengue virus serotypes (DENV-1-4), is the most prevalent mosquito-borne viral disease in humans. Clinical disease ranges from asymptomatic infection and classic dengue fever (DF) to more severe forms, dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS). Approximately 40 million cases of dengue and 250,000 to 450,000 DHF/DSS cases are estimated to occur each year (1). While previous infection with one DENV serotype induces long-lasting protective humoral and T cell responses against the same serotype, reinfection with a different serotype has been associated with more severe disease (2–6). Cross-reactive antibodies (Abs) acting through Ab-dependent enhancement (ADE) (7–9), as well as cross-reactive T cells (6, 10–13) have been implicated in increased disease severity after secondary (2°) infection. However, most 2° infections are asymptomatic or result in classic DF, indicating that cross-reactive immunity can be protective (3). Cross-reactive Abs have been correlated with less severe disease in humans (14, 15), and we have previously shown in a mouse model of dengue that passive transfer of cross-reactive Abs resulted in reduced viral load in multiple organs after a subsequent non-lethal heterotypic DENV infection (16).
In terms of the cellular immune response, it is still unclear what are the specific roles of memory B cells and memory T cells in DENV cross-protection. Different B cell compartments can be identified according to their phenotype (17). Affinity-matured memory B cells persist as non-Ab-secreting cells, but maintain their immunoglobulin as membrane-bound and are the precursors of the rapid cellular response to antigen (Ag) recall (17). Upon Ag recall, memory B cells differentiate into short-lived plasma cells (PCs) and long-lived plasma cells (LLPCs). LLPCs are terminally differentiated, non-dividing cells, which home to the bone marrow and are responsible for the long-term humoral response (17). Both long-lasting specific Ab responses, attributed to LLPCs, and long-lived memory B cells contribute to long-term protective immunity (18, 19). Maintenance of LLPCs has been shown to be independent of memory B cells (20), indicating that LLPCs are sufficiently long-lived to sustain Ab titers for a long period of time. Moreover, in humans a lack of linear correlation between tetanus toxin-specific memory B cells and serum titers of tetanus toxin-specific IgG over time (18) indicates that memory B cells and LLPCs represent independent forms of immunological memory.
We have developed an interferon-α/β and -γ receptor-deficient (AG129) mouse model of dengue that reproduces both ADE and Ab-mediated protection (7, 16, 21). DENV infection of AG129 mice recapitulates key features of human disease, including vascular leak, low platelet counts and increased levels of serum cytokines such as IL-10 and TNF-α. Tropism studies identified DENV in relevant tissues and cells, such as dendritic cells (DCs) and macrophages (22). All four DENV serotypes replicate efficiently in AG129 mice after administration of DENV by either a sub-cutaneous (s.c.) or intravenous (i.v.) route. The generation of a more virulent and lethal DENV strain, DENV-2 D2S10, allowed us to study pathogenesis of severe disease in vivo (7, 23, 24). The two mutations that differentiate D2S10 from the parental PL046 DENV-2 strain, N124D and K128E in the virus envelope protein, decrease heparan sulfate binding and consequently reduce clearance of the virus, thus increasing viremia and resulting in the lethal disease phenotype (25). AG129 mice infected with high doses of D2S10 develop signs of vascular leak, low platelet counts, and high levels of serum cytokines, including increased IL-10 and TNF-α, and exhibit mortality within 4–5 days due to a non-paralytic syndrome (23). We previously demonstrated a role for the cross-reactive cellular immune response and for pre-existing cross-reactive Abs during 2° DENV using Cyclophosphamide (CP). CP is an alkylating agent and immunosuppressive drug that primarily affects proliferating cells (26, 27) and thus eliminates the proliferating cellular immune response during a 2° DENV infection. CP-treated naïve mice exhibited mortality from a primary (1°) DENV-2 D2S10 sub-lethal infection 3–4 days earlier than DENV-1-immune mice treated with CP (21). Naïve mice have no pre-existing anti-DENV Abs, as compared to DENV-1-immune mice, which have pre-existing cross-reactive Abs. Thus, this experiment demonstrates the contribution of pre-existing cross-reactive Abs to protection during the early phase of DENV infection (21). These data are consistent with experiments that showed that passive transfer of heterotypic serum prior to DENV infection reduces viral load in several tissues (16). The fact that DENV-1-immune mice treated with CP prior to a 2° DENV-2 D2S10 sub-lethal infection experienced lethal disease (21) demonstrates a role for the cellular immune response in protection. Morbidity and mortality in these mice correlated with increased viremia 24 hours prior to death as compared to CP-untreated controls (21). In addition, adoptive transfer of immune splenocytes into naïve mice prior to infection demonstrated that the cellular immune compartment contributes to the control of DENV viral load as measured in several tissues during a 2° heterotypic DENV infection (16). The T cell response, and more specifically homotypic anti-DENV CD8+ T cells, have been reported to protect mice against a 1° DENV infection (28). CD4+ T cells were found to be dispensable for the induction of DENV-specific CD8+ T cells and Ab response during a 1° infection, but were found to have cytolytic activity in vivo against DENV-infected cells and to increase the cytolytic activity of CD8+ T cells after vaccination, indicating a role for these cells during a 2° response (29). Together these data demonstrate a role for CD4+ and CD8+ T cells in homotypic protection. However, it is still not clear whether cross-reactive T cells can be protective during a 2° heterotypic DENV infection.
In this study, we first characterized the murine B cell and humoral response during 2° heterotypic DENV-2 infection by measuring B cell proliferation, DENV-specific neutralization capacity, and DENV-specific avidity of serum and supernatants of polyclonally-stimulated splenocytes using a modified urea-wash ELISA. We also measured the number of DENV-specific memory B cells and PCs by ELISPOT. Subsequently, we dissected the role of the cellular immune response by adoptively transferring different cellular subsets and by using monoclonal Abs (mAbs) to deplete distinct immune cell subsets in vivo. In summary, we show that pre-existing cross-reactive Abs and Abs newly secreted by cross-reactive memory B cells participate in cross-protection against a 2° heterotypic DENV infection. In addition, we demonstrate that cross-reactive B and T cells as well as innate immune cells all participate in protection against a lethal 2° heterotypic DENV infection and that T cells are necessary for full protection in this model.
Materials and Methods
Viruses and cell lines
DENV was propagated in Aedes albopictus cell line C6/36 (gift from P. Young, University of Queensland, Australia) in M199 medium (Invitrogen) with 10% Fetal Bovine Serum (Denville Scientific Inc.) at 28°C. Cell supernatants were collected on days 5, 6, 7 and 8 post-infection (p.i.) and either frozen at −80°C directly or after concentration. Concentrated virus was prepared by either ultracentrifugation of the supernatants (26,000×g for 2 hours (h) at 4°C) or by centrifugation through Amicon filters (Millipore, 50 kDa, 3,250×g for 20 minutes (min) at 4°C). DENV-2 strain D2S10 (passage 4) is a peripherally passaged mouse-adapted strain derived in our laboratory from the parental DENV-2 PL046 Taiwanese strain as described elsewhere (23). DENV-1 strain 98J (passage 7) was isolated in our laboratory from a patient from Guyana in 1998 (30). Virus titers were obtained by plaque assay on baby hamster kidney cells (BHK21, clone 15) as previously described (31). U937-DC-SIGN cells (gift from A. de Silva, University of North Carolina, Chapel Hill) were grown in RPMI (Invitrogen) with 2% Fetal Bovine Serum, at 37°C in 5% CO2 for use in neutralization assays (32).
Infection of mice
AG129 mice lacking receptors for IFN-α/β and -γ were obtained from M. Aguet (Swiss Institute for Experimental Cancer Research, Epalinges, Switzerland) and bred in the University of California (UC) Berkeley Animal Facility. All experimental procedures were pre-approved by the UC Berkeley Animal Care and Use Committee and were performed according to the guidelines of the UC Berkeley Animal Care and Use Committee. Experiments were initiated with 6–8 week-old mice. Sub-cutaneous (s.c.) injections, in a total volume of 200µl, were performed under the skin of the ventral hindlimbs; tail vein i.v. injections were performed using a total volume of 100µl, and intra-peritoneal (i.p.) injections, using 100–200µl, were performed through the lower left abdominal wall. For 1° infections, mice were infected s.c. with 105 plaque-forming units (PFU) of DENV-2 D2S10. For 2° infections, mice were infected first with 105 PFU of DENV-1 98J s.c. then, 6 to 8 weeks later, were infected a second time with 107 PFU of DENV-2 D2S10 i.v.. Mock-infected control mice (post-1°/pre-2°) were injected with uninfected C6/36 supernatant. A129 mice, lacking the IFN-γ receptor, were obtained from Dr. H. Virgin (Washington University School of Medicine, St. Louis, MO), and wild type (WT) 129 mice were obtained from Taconic Farms (taconic.com). For adoptive transfer experiments (see below), AG129, A129 and WT129 mice were infected s.c. with 105 PFU of DENV-1 98J then, 6 to 8 weeks later, spleens were collected, pooled, and used to isolate B and T cells. In order to assess morbidity associated with DENV infection, mice were scored on a scale from 1 to 5 as follows: (1) healthy; (2) displaying mild signs of lethargy, some fur ruffling, no hunched posture; (3) displaying mild signs of lethargy, fur ruffling and hunched posture; (4) displaying increased signs of lethargy and limited mobility, fur ruffling, hunched posture; (5) moribund. Mice were euthanized when moribund per UC Berkeley animal care guidelines.
In vivo T cell depletion
AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks later on day 0 were infected i.v. with 107 PFU of DENV-2 D2S10. On days −1, 0, 1, and 2 p.i., mice were treated i.p. with 200µg of anti-CD4 Ab (clone GK1.5, IgG2b) and on days −1, 0, 1, 2 and 7 p.i. were treated i.p. with 400µg of anti-CD8 Ab (clone 2.43, IgG2a). Control mice received either isotype control Ab (IgG2a for depletions of CD8+ T cells and IgG2b for depletions of CD4+ T cells) or PBS i.p.. Morbidity and mortality were monitored for 10 days. Mice were euthanized at day 10 post-2° infection, and spleen cells were harvested to test the efficacy of T cell depletion by flow cytometry using anti-CD3 PECy5 (clone 17A2), anti-CD4 PECy7 (RM4–5), and anti-CD8 FITC Abs (clone 53–6.7).
In vivo B cell depletion
AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks later on day 0 were infected i.v. with 107 PFU of DENV-2 D2S10. On day −8, mice were treated i.v. with 250µg of anti-CD20 Ab (clone 18B12, IgG2a, Biogen Idec Inc.). Control mice received either isotype control Ab (IgG2a) or PBS i.v.. Morbidity and mortality were monitored for 10 days. Whole blood collected by eye bleed prior to 2° infection was used to determine the efficacy of B cell depletion. Flow cytometry was performed on whole blood cells using anti-CD19 PE, anti-B220 PECy7, and anti-IgD PB Abs 8 days after depletion.
Adoptive transfer of T cells
A129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks later, spleens were harvested and pooled. CD4+ and CD8+ T cells were isolated using magnetic-activated cell sorting (MACS) bead CD4+ and CD8+ T cell negative selection isolation kit (Miltenyi). The purity of cells was assessed by flow cytometry using anti-CD3 PECy5, anti-CD4 PECy7, and anti-CD8 FITC Abs. Isolated cells (2×105) were adoptively transferred i.v. into naïve AG129 mice and, 24h later, mice were infected i.v. with 107 PFU of DENV-2 D2S10. Mice were monitored for morbidity and mortality for 10 days.
Adoptive transfer of B cells
AG129 or WT129 mice were infected s.c. with 105 PFU of DENV-1 98J and, 6 to 8 weeks later, spleens were harvested and pooled. Total B cells were isolated using a MACS bead B cell negative selection isolation kit (Miltenyi). Cell purity was evaluated by flow cytometry using anti-CD19 PE and anti-B220 PECy7 Abs. Isolated cells (30×106) were adoptively transferred i.v. into AG129 naïve mice and, 24h later, mice were infected i.v. with 107 PFU of DENV-2 D2S10. Mice were monitored for morbidity and mortality for 10 days.
Flow cytometry
On days 3, 6, and 9 after 2° DENV infection, spleens were collected, and single-cell suspensions were prepared for flow cytometry. Cells were stained with anti-IgD PB, anti-B220 PECy7, anti-CD79b FITC, and anti-CD138 APC. Proliferating memory B cells in the spleen were quantified using anti-Ki-67 (BD Pharmingen) (33). Results were analyzed using FlowJo software, version 7.2.5 (TreeStar Software).
ELISPOT
To quantify the number of DENV-specific B cells and PCs, total splenocytes or bone marrow cells were analyzed by ELISPOT ex vivo (reflecting the PC compartment producing Ab in vivo at the time of collection) or after in vitro stimulation (reflecting the memory B cell compartment present in vivo at the time of collection). For the bone marrow, two femurs per mouse were harvested. The cell count obtained from the two femurs was then multiplied by 7.9 in order to estimate the total number of bone marrow cells per mouse (34). For in vitro stimulation, splenocytes were polyclonally stimulated in vitro for 6 days with pokeweed mitogen extract (0.1 µg/mL, PWM, Sigma), CpG oligonucleotide (1 µg/mL), 1/10,000 fixed S. aureus Cowan (Sigma), and LPS (10 µg/mL, Sigma) to generate Ab-secreting cells (ASCs) (35). For the ELISPOT, 96-well filter plates were coated with DENV-1 98J or DENV-2 D2S10 cellular Ag prepared from infected C6/36 cells. To detect total IgG-secreting cells, wells were coated with goat anti-mouse IgG (2.5 µg/mL, Jackson ImmunoResearch Inc.). To prepare cellular Ag, C6/36 cells were infected with DENV-1 98J or DENV-2 D2S10 at an MOI of 0.1, collected 7 days p.i., and submitted to seven cycles of freeze/thaw; cell lysates were then suspended in 1% Tween-20 and 50% glycerol and stored at −80°C. Uninfected cells were submitted to the same procedure to produce mock-infected control cellular Ag. Ag-coated plates were incubated for 5–6h with Ab-producing cells to allow formation of Ab-Ag complexes. Cells were removed, and plates were washed and incubated with anti-mouse IgG HRP-conjugated Ab overnight (1/1,000, Sigma), followed by substrate (Amino-9 ethyl-carbazole, Sigma). Resulting spots, representing DENV-specific Ab-producing B cells or total IgG Ab-producing cells, were counted by visual inspection using an inverted microscope. The number of spots counted in the control wells, coated with mock-infected control cellular Ag, was subtracted from the number of spots counted in each test well coated with DENV-specific cellular Ag.
Neutralization assay
Serum was diluted using eight 4-fold dilutions, beginning at 1:20 to 1:327,680. 6×102 PFU of D2S10 in 30 µl was mixed with 10 µl of each serum dilution and incubated for 45 min at 37°C. This viral titer was selected to satisfy the assumptions of the law of mass action (36). The virus/serum combinations were mixed with 5×104 cells and incubated for 18–24h at 37°C. The cells were then fixed and stained both intracellularly for the virus using a fluorescently tagged DENV-specific mAb (4G2-Alexa488) and extracellularly for DC-SIGN (anti-CD209 PECy5, clone DCN46). The cells were processed by flow cytometry, and the percentage of cells positive for DC-SIGN and infected with DENV was determined. To analyze the U937-DC-SIGN neutralization data, raw data was expressed in GraphPad as percent infection versus log10 of the serum dilution. A sigmoidal dose-response curve with a variable slope was used to determine the serum dilution at which a 50% reduction in infection was observed compared to the no-serum control and was expressed as the 50% neutralization titer (NT50).
Avidity assay
Serum avidity was measured using a modified ELISA protocol with urea washes (37, 38). 96-well plates were coated overnight with either DENV-1 or DENV-2 recombinant envelope protein (Hawaii Biotech) at 1 µg/ml, blocked, and incubated for 1h with serum samples from 1° and 2° DENV infections. The plates were washed for 10min with 6 to 9M urea or PBS before adding biotin-conjugated goat anti-mouse IgG, Streptavidin-Alkaline Phosphatase and p-Nitrophenyl Phosphate (PnPP) substrate. Optical density was measured at 405 nm using KC Junior software. Background from the no-Ag coated wells was subtracted from each sample. The percentage of IgG bound was calculated by dividing the optical density after the urea wash by the optical density after the PBS wash.
Statistical analysis
Kaplan-Meier survival curves were used to display mortality data, and log rank analyses were used to determine statistical significance between experimental groups. Non-parametric analyses were performed using the the Mann-Whitney U test for unpaired comparisons. Calculations were performed in GraphPad Prism 5.0 software.
Results
DENV-1-immune mice are protected against a lethal heterotypic secondary DENV-2 infection
DENV-2 D2S10 resulted in 90% mortality in naïve AG129 mice by day 5 p.i. by a characteristic “vascular-leak” syndrome when administered at a high inoculum (107 PFU i.v.) (Figure 1A) (7, 23). In contrast, mice infected first with DENV-1 98J (105 PFU s.c.) were completely protected against a 2° infection with a lethal dose of DENV-2 D2S10 6 to 8 weeks after the 1° infection (Figure 1A). DENV-1-immune mice did not show any signs of disease during 15 days of observation, nor any fluid accumulation in the visceral organs or increased viral load as measured by plaque assay (no detectable plaques in liver, bone marrow, small intestine, spleen and white blood cells) and by quantitative RT-PCR (in serum, data not shown) at day 3.5 post-2° infection with DENV-2 D2S10. In comparison, naïve mice infected with a lethal dose of D2S10 displayed an increase in viral load in several tissues 12h prior to death (day 3.5 p.i.) (7). In addition, platelet count, which decreases after infection with a lethal dose of DENV-2 D2S10 in naïve mice, and plasma levels of IL-10, which increase under these conditions (7), remained normal after a 2° infection with a lethal dose of DENV-2 D2S10 in DENV-1-immune mice (data not shown). Therefore, a 1° infection with DENV-1 provided complete protection from a 2° infection with DENV-2, with reduced viral load, no symptoms and no resulting mortality.
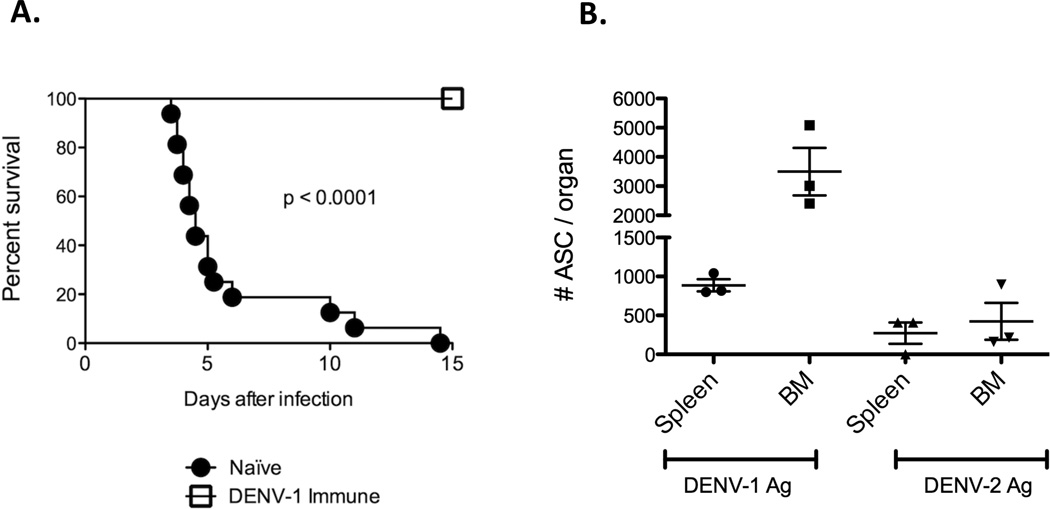
Figure 1. Protection of DENV-1-immune AG129 mice against a lethal 2° DENV-2 infection.
A. Survival of AG129 mice after 1° and 2° DENV infection. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J (DENV-1-immune, n=14) or injected s.c. with C6/36 cell supernatant (Naïve, n=16). Eight weeks post infection (p.i.), the mice were infected i.v. with a lethal dose of DENV-2 D2S10 (107 PFU). Statistical analysis was performed using the Wilcoxon rank-sum test. Survival of DENV-1 immune mice infected with DENV-2 D2S10 was significantly different from Naïve mice infected with DENV-2 D2S10. B. DENV-specific B cell ELISPOT after 1° DENV-1 infection. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J (n=3). Six to eight weeks p.i., spleen and bone marrow were collected and cell suspensions prepared. Cells were tested ex vivo by ELISPOT using DENV-1 and DENV-2 cellular Ag to detect DENV-1 and DENV-2-specific PCs. The number of spots from control wells coated with Mock-Ag was subtracted from the number of spots counted in DENV-coated wells. Statistical analysis was performed using the Mann-Whitney U test. No significant difference in the number of antibody-secreting cells was found between cells tested in the spleen and bone marrow.
We hypothesized that the protective immunity was mediated at least partially by memory B cells and/or LLPCs. Thus, six to eight weeks after a 1° DENV-1 infection, we performed an ELISPOT ex vivo using splenocytes and bone marrow cells (Figure 1B) to measure DENV-specific ASC. The highest numbers of anti-DENV-1 ASC were found in the bone marrow. Representative photographs of the B cell ELISPOT are provided in Figure S1A. These cells are PCs, as ELISPOT assays performed ex vivo identifies PCs, in contrast to ELISPOT assays performed after polyclonal in vitro stimulation, which identifies memory B cells. As these PCs home to the bone marrow and are found several weeks p.i., they are most likely LLPCs (39). Thus, the long-term anti-DENV Ab response, mostly to DENV-1, is sustained by LLPCs. Of note, a substantial number of DENV-specific PCs was also found in the spleen (886 ± 78.4 serotype-specific PCs/spleen and 252 ± 136 serotype cross-reactive PCs/spleen) (Figure 1B). These cells are most probably semi-long-lived PCs that originate or migrate to the spleen after a 1° infection before becoming LLPCs (40).
B cells and CD8+ T cells proliferate upon a heterotypic secondary DENV infection
In order to characterize B cell and T cell immune responses after 2° DENV infection, spleens were collected 3, 6 and 9 days after heterotypic 2° infection, and B and T cell subsets were analyzed by flow cytometry. We detected increased proliferation of the memory B cell component (B220+, CD79b+, CD138−, IgD−) by day 6 post-2° infection in the spleen, using Ki67 as a proliferation marker (post-1°/pre-2° = 0.54 ± 0.11% Ki67+ vs. mean day 6 p.i. = 1.52 ± 0.42% Ki67+, p=0.09) (Figure 2A and 2B). Increased absolute numbers of memory B cells were detected in the spleen at day 9 post-2° infection (mean post-1°/pre-2° = 9.08×105 ± 4.22×105 cells/mL vs. mean day 9 p.i. = 32.3×105 ± 4.20×105 cells/mL, p=0.008) (Figure 2C). The increase in absolute number of PCs (B220low/−, CD79b+, CD138+, IgD−) in the spleen preceded the increase in absolute number of memory B cells, with a significant increase evident by day 6 p.i. (mean post-1°/pre-2°= 4.90×105 ± 2.14×105 cells/mL vs. mean day 6 p.i. = 13.4×105 ± 0.81×105 cells/mL, p=0.049) (Figure 2C). Among T cells, CD4+ T cell numbers, though not significant, increased two fold after 2° heterotypic infection (mean post-1°/pre-2° = 9.88×106 ± 2.18×106 cells/mL vs. mean day 9 p.i. = 18.9×106 ± 7.0×106 cells/mL, p=0.20). We also detected a significant increase in absolute CD8+ T cell numbers by day 9 p.i. when compared to post-1°/pre-2° control mice (mean post-1°/pre-2° = 5.58×106 ± 1.03×106 cells/mL vs. mean day 9 p.i. = 12.9×106 ± 4.13×106 cells/mL; p=0.04) (Figure 2D), with increased proliferation detectable by day 3 p.i. (mean post-1°/pre-2° = 0.86 ± 0.35% Ki67+ vs. mean day 3 p.i. = 4.80 ± 2.31% Ki67+, p=0.38).
Figure 2. Proliferation of memory B cells and PCs after a 2° heterotypic DENV infection.
A. Flow cytometry analysis of Ki67+ memory B cells. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks p.i. were infected i.v. with 107 PFU of DENV-2 D2S10. A control group was infected with DENV-1 98J and mock-infected with C6/36 cell supernatant (post1°/pre2°). After 3, 6 and 9 days, splenocytes were harvested and stained with anti-B220 PECy7, anti-CD79b FITC, anti-CD138 PerCP Cy5.5, anti-IgD Pacific Blue, and anti-Ki67-PE or isotype control-PE. Cells were gated on B220+, CD79b+, CD138−. One representative flow cytometry staining of nine independent experiments is shown. B. Percentage of Ki67+ memory B cells. The percentage of cells that were PE positive using the isotype control Ab were subtracted from the percentage of Ki67-positive cells for each sample to obtain the percentage increase relative to isotype control. Data were pooled from 9 independent repeated experiments with a total of n=19 mice for post1°/pre2°, n=13 mice for day 3, n=15 mice for day 6, and n=6 mice for day 9. Statistical analysis was performed using the Mann-Whitney U test to compare each time-point to the post1°/pre2° samples, and p-value is shown in the graph. No significant difference was found among the groups. C. Absolute number of plasma cells and memory B cells. Splenocytes were treated as in Figure A. Absolute numbers of plasma cells (B220low/−, CD79b+, IgD−, CD138+) and memory B cells (B220+, CD79b+, IgD−, CD138−) in the spleen before and after 2° infection are shown. Data were pooled from 6 independent repeated experiments with a total of n=10 mice for post1°/pre2°, n=11 mice for day 3, n=3 mice for day 6 and n=6 mice for day 9. Statistical analysis was performed using the Mann-Whitney U test to compare each time-point to the post1°/pre2° samples, and p-values are shown below the graph. A statistically significant difference was found in the absolute numbers of PCs at day 6 and in the absolute number of memory B cells at day 9 p.i. when compared to the post1°/pre2° samples. D. Absolute numbers of CD4+ and CD8+ T cells. Splenocytes were treated as in Figure A. Absolute numbers of CD4+ T cells (CD3+, CD4+, CD8−) and CD8+ T cells (CD3+, CD4−, CD8+) in the spleen before and after 2° infection are shown. Data were pooled from 9 independent repeated experiments with a total of n=16 mice for post1°/pre2°, n=14 mice for day 3, n=10 mice for day 6 and n=5 mice for day 9. Statistical analysis was performed using the Mann-Whitney U test to compare each time-point to the post1°/pre2° samples, and p-values are shown beneath the graph. A statistically significant difference was observed in the absolute numbers of CD8+ T cells at day 9 p.i. when compared to the post1°/pre2° samples.
The DENV-specific neutralization capacity of serum increases between day 3 and day 6 post-secondary heterotypic infection and after day 6 post-primary infection
We used a U937-DC-SIGN flow cytometry-based assay to measure the neutralization titer of sera against DENV-2 on days 3, 6 and 9 after 2° heterotypic infection. As shown in Figure 3A, the NT50 against DENV-2 D2S10 significantly increased between day 3 and day 6 after 2° infection (p<0.0001). A similar increase in neutralization titer was also observed between day 3 and day 6 after 1° infection with a sub-lethal dose of DENV-2 D2S10 (Figure 3B). Thus, the increase in neutralization titer can be attributed to either cross-reactive memory B cells induced by the first DENV-1 infection or to naïve B cells responding to the DENV-2 D2S10 infection during the 2° heterotypic infection. Of note, we did not observe an increase in neutralization against DENV-1 on days 3, 6 and 9 after 2° heterotypic infection (Figure 3C), suggesting that naïve B cells are the cells responsible for the increase in neutralization against DENV-2 during the 2° heterotypic infection.
Figure 3. DENV-specific neutralization capacity of serum after 1° and 2° heterotypic DENV infection.
A. Neutralizing antibody titers after 2° DENV infection. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks p.i. were infected i.v. with 107 PFU of DENV-2 D2S10. A control group was infected with DENV-1 98J and mock-infected for the second infection (post1°/pre2°). After 3, 6 or 9 days, serum was collected and tested in a U937-DC-SIGN flow cytometry-based neutralization assay against DENV-2 D2S10. The dashed line corresponds to 50% neutralization, and the 50% neutralization titers (NT50) are shown in the legend. For each time-point, the neutralization data are pooled from 4 to 6 mice were pooled from 2 independent repeated experiments. Statistical analysis was performed using the Mann-Whitney U test in order to compare the NT50 of each time-point to the NT50 of the post1°/pre2° serum. A statistically significant difference in NT50 titer was found at day 6 and day 9 post-2° infection when compared to the NT50 of the post1°/pre2° serum; p-values are shown in the symbol figure legend. B. Neutralizing antibody titers after 1° DENV infection. AG129 mice were infected i.v. with 105 PFU of DENV-2 D2S10. A control group of mice was mock-infected with C6/36 cell supernatant (Naïve). After 3 and 6 days, serum was collected from DENV-2 D2S10-infected and naïve mice and tested in a U937-DC-SIGN flow cytometry-based neutralization assay against DENV-2 D2S10. The dashed line corresponds to 50% neutralization, and the 50% neutralization titers (NT50) are shown in the legend. For each time-point, data were pooled from 3 to 6 mice from 2 independent repeated experiments. Statistical analysis was performed using the Mann-Whitney test. Each time-point (day 6, day 9 and day 14) was compared to the day 3 serum. A statistically significant difference in NT50 was found at day 6 post-infection when compared to the NT50 of day 3 serum; p-values are shown in the symbol legend. C. DENV-1-specific neutralization capacity of serum after 2° heterotypic DENV infection. Neutralizing antibody titers after 2° DENV infection are shown. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks p.i. were infected i.v. with 107 PFU of DENV-2 D2S10. A control group was infected with DENV-1 98J and mock-infected for the second infection (post1°/pre2°). After 3, 6 or 9 days, serum was collected and tested in a U937-DC-SIGN flow cytometry-based neutralization assay against DENV-1 98J. The dashed line corresponds to 50% neutralization, and the 50% neutralization titers (NT50) are shown in the symbol legend. For each time point, data are pooled from 5 to 6 mice from 2 independent experiments. Statistical analysis was performed using the Mann-Whitney U test to compare the NT50 of each time point to the NT50 of the post1°/pre2° serum. No significant difference was found among the different time-points.
Cross-reactive memory B cells mediate an increase in DENV-specific serum avidity between day 3 and day 6 post-secondary heterotypic DENV infection
We measured the avidity of Abs produced in serum 6 to 8 weeks after a 1° DENV-1 infection (post-1°/-pre-2°), reflecting the Abs produced by LLPCs, and compared it to the avidity of the Abs produced during the acute phase of a 2° heterotypic DENV-2 infection, using a modified ELISA assay involving urea washes (Figure 4A to 4D). As expected, serum avidity decreased with increasing concentrations of urea (Figure 4A to 4D). Based on these experiments, a single concentration of 7M urea was then selected and used to compare avidity in the serum and in the supernatants of polyclonally stimulated splenocytes to DENV-1 versus DENV-2 Ag. The avidity of Abs in serum against both DENV-1 and DENV-2 increased significantly 6 days after 2° infection when compared to pre-infection serum (Figure 4E), and this increase in avidity was greater against DENV-1 than against DENV-2, suggesting an increase in cross-reactive Abs during the acute phase of the 2° heterotypic infection. Of note, avidity against DENV-1 or DENV-2 could not be measured 3, 6 or 9 days after a 1° infection as the level of Abs was below the limit of detection of the assay. Thus, the increase in serum avidity can be attributed to Abs secreted by memory B cells rather than activated naïve B cells.
Figure 4. DENV-specific avidity of serum and supernatant of polyclonally-stimulated splenocytes after a 2° heterotypic DENV infection.
A. DENV-specific avidity of serum measured by ELISA using different concentrations of urea. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks later were mock-infected with C6/36 cell supernatant (post1°/pre2°). Serum was harvested on days 6 and 9 p.i. and tested in a urea-based ELISA assay using 6 to 9M urea and recombinant E protein from DENV-1 or DENV-2 as antigen to measure avidity against DENV-1 and DENV-2, respectively. Data are pooled from 3 to 5 mice from 2 independent experiments. B. DENV-specific avidity of serum measured by ELISA using different concentrations of urea at day 3 p.i.. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks later were infected i.v. with 107 PFU of DENV-2 D2S10. Serum was harvested on day 3 p.i. and tested in a urea-based ELISA assay using 6 to 9M urea and recombinant E protein from DENV-1 or DENV-2 as antigen to measure avidity against DENV-1 and DENV-2, respectively. Data are pooled from 6 mice from 2 independent experiments. C. DENV-specific avidity of serum measured by ELISA using different concentrations of urea at day 6 p.i.. Mice were infected as in Figure 4B. Serum was harvested at day 6 p.i. and processed as in Figure 4B. Data are pooled from 12 mice from 4 independent experiments. D. DENV-specific avidity of serum measured by ELISA using different concentrations of urea at day 9 p.i.. Mice were infected as in Figure 4B. Serum was harvested at day 9 p.i. and processed as in Figure 4B. Data are pooled from 12 mice from 4 independent experiments. E. DENV-specific serum avidity measured by ELISA using 7M urea. AG129 mice were infected s.c. with 105 PFU of DENV-1 98J and 6 to 8 weeks p.i. were infected i.v. with 107 PFU of DENV-2 D2S10. A control group was infected with DENV-1 98J and mock-infected with C6/36 cell supernatant (post1°/pre2°). Serum was harvested on days 3, 6 and 9 p.i. and tested in an urea-based ELISA assay using 7M urea and recombinant E protein from DENV-1 or DENV-2 as antigen to measure avidity against DENV-1 and DENV-2, respectively. Data are pooled from 10 to 22 mice for each group from 9 repeated independent experiments. Statistical analysis was performed using the Mann-Whitney U test to compare the % of IgG bound after urea washes at each time-point to the % of IgG bound after urea washes of the post1°/pre2° serum. A statistically significant difference in % of IgG bound in serum was found at day 6 and day 9 post-2° infection when compared to the % of IgG bound in the post1°/pre2° serum for both DENV-1 and DENV-2 Ag; p-values are shown below the graphs. F. DENV-specific avidity in supernatants from polyclonally-stimulated splenocytes measured by ELISA using 7M urea. Mice were infected as in Figure 4E. Spleens were harvested on days 3 and 6 p.i.. Splenocytes were polyclonally stimulated with PWM extract, CpG oligonucleotide, fixed S. aureus Cowan, and LPS, and supernatants were collected 5–6 days post-stimulation. Supernatants were tested in a urea-based ELISA assay using 7M urea and recombinant E protein from DENV-1 or DENV-2 as antigen to measure avidity against DENV-1 and DENV-2, respectively. Data are pooled from 5 to 7 mice for each group from 3 repeated independent experiments. Statistical analysis was performed using the Mann-Whitney U test to compare the % of IgG bound after urea washes at each time-point to the % of IgG bound after urea washes of the post1°/pre2° supernatants. No significant difference was found for either DENV-1 or DENV-2 Ag.
We then measured the avidity of supernatants from polyclonally stimulated splenocytes collected after 2° heterotypic DENV infection using 7M urea in the ELISA washes. The Abs found in these supernatants are not secreted by PCs, as PCs do not usually survive polyclonal stimulation in cell culture (41). In addition, we measured the amount of Abs in the supernatant of splenocytes maintained in culture for 24h only, which might contain Abs from PCs, and the amount of these Abs was below the assay’s limit of detection. We also could not detect any Abs in supernatants from splenocytes collected up to 9 days after a 1° DENV-2 infection, indicating that there was no Ab secreted by stimulated naïve B cells that could be detected in this assay. Thus, the Abs detected in the supernatants reflect the Abs produced by memory B cells. As shown in Figure 4F, the avidity of the splenocyte supernatant cultures increased only against DENV-1 and not DENV-2, suggesting that cross-reactive memory B cells, generated during the 1° DENV-1 infection, are the ones that proliferate and contribute to increased avidity of the serum after a 2° heterotypic infection. Overall, these results indicate that Abs secreted by cross-reactive memory B cells are responsible for the increase in serum avidity observed during the acute phase of a 2° heterotypic infection.
Cross-reactive memory B cells generated after primary infection increase in number during a secondary heterotypic DENV infection
To quantify the number of DENV-specific B cells, total splenocytes were analyzed by ELISPOT ex vivo or after in vitro stimulation to generate ASCs. Representative pictures of the B cell ELISPOT are shown in Figure S1B. After in vitro stimulation, the ASCs reflect the DENV-specific memory B cells present at the time of collection, while the ex vivo ELISPOT reflects the DENV-specific PC population, which should be actively secreting Ab at the time of collection. After a 2° heterotypic infection with DENV-2 D2S10 following a DENV-1 98J 1° infection, DENV-1 and DENV-2-specific memory B cells increased by ELISPOT between day 3 and day 6 post-2° infection (Figure 5A and 5B). This increase in the number of DENV-specific memory B cells correlates with the increased proliferation and increased absolute cell numbers of the memory B cell compartment detected by flow cytometry at day 6 post-2° infection (Figure 2A–C). Of note, DENV-1-specific memory B cells were present in greater numbers than DENV-2-specific memory B cells at day 6 post-2° infection (81.8 ± 26.8 DENV-1-specific ASC/106 splenocytes vs. 23.3 ± 7.6 DENV-2-specific ASC/106 splenocytes, p=0.003).
Figure 5. Number of DENV-specific memory B cells and PCs after 1° and 2° heterotypic DENV infection.
A. DENV-1-specific memory B cells detected by ELISPOT. AG129 mice were infected either with 105 PFU of DENV-2 D2S10 i.v. (1° infection) or with 105 PFU of DENV-1 98J s.c. (1° infection) then 6 to 8 weeks p.i., infected i.v. with 107 PFU of DENV-2 D2S10 (2° infection). A control group was mock-infected (Naïve or Post1°/Pre2°). After 3, 6, 9 and 14 days, splenocytes were harvested and polyclonally stimulated in vitro for 6 days to obtain ASCs. ASCs against DENV-1 were tested by ELISPOT using cellular Ag to detect DENV-1-specific memory B cells. The number of spots from control wells coated with Mock-Ag was subtracted from the number of spots counted in DENV-coated wells. Statistical analysis was performed using the Mann-Whitney test to compare the number of DENV-1-specific memory B cells at each time-point to the number of DENV-1-specific memory B cells from naïve or post1°/pre2° mock-infected mice. A statistically significant difference was found at day 9 and day 14 post-1° infection; p-values are shown below each graph. B. DENV-2-specific memory B cells detected by ELISPOT. Cells were prepared as in Figure 5A and were tested by ELISPOT using DENV-2 cellular Ag to detect DENV-2-specific memory B cells. Statistical analysis was performed using the Mann-Whitney U test to compare the number of DENV-2-specific memory B cells at each time-point to the number of DENV-2-specific memory B cells from naïve or post1°/pre2° mock-infected mice. A statistically significant difference was found at day 9 and day 14 post-1° infection and at day 6 and day 9 post-2° infection; p-values are shown below each graph. C. DENV-1-specific PCs detected by ELISPOT. Cells were prepared as in Figure 5A and tested ex vivo by ELISPOT using DENV-1 cellular Ag to detect DENV-1-specific PCs. Statistical analysis was performed using the Mann-Whitney U test to compare the number of DENV-1-specific PCs at each time-point to the number of DENV-1-specific PCs from naïve or post1°/pre2° mock-infected mice. A statistically significant difference was found at day 6, day 9 and day 14 post-1° infection and at day 6 and day 9 post-2° infection; p-values are shown below each graph. D. DENV-2-specific PCs detected by ELISPOT. Cells were prepared as in Figure 5A and were tested by ELISPOT ex vivo using DENV-2 cellular Ag to detect DENV-2-specific PCs. Statistical analysis was performed using the Mann-Whitney U test to compare the number of DENV-2-specific PCs at each time-point to the number of DENV-2-specific PCs from naïve or post1°/pre2° mock-infected mice. A statistically significant difference was found at day 6, day 9 and day 14 post-1° infection and at day 9 post-2° infection; p-values are shown below each graph.
After a 1° infection with a sub-lethal dose of 105 PFU of DENV-2 D2S10, only 14.5 ± 4.6 DENV-2-specific ASC/106 splenocytes and 37.2 ± 10.0 DENV-2-specific ASC/106 splenocytes were detected at days 9 and 14 p.i., respectively (Figure 5B). Thus, the immune response takes 14 days to generate the same number of DENV-2-specific ASCs from naïve B cells after a 1° infection with DENV-2 D2S10 (37.2 ASC/106 splenocytes) as detected by day 9 post-2° infection (32.7 ASC/106 splenocytes), suggesting that the increase in DENV-2-reactive memory B cells during a 2° heterotypic infection is attributable to cross-reactive memory B cells induced by the first DENV-1 infection rather than naïve B cells responding to the second DENV-2 infection.
After a 2° heterotypic infection with DENV-2 D2S10 following a DENV-1 98J 1° infection, DENV-1-specific PCs, as measured by ex vivo ELISPOT, peaked at day 6 post-2° infection in the spleen (149.3 ± 82.7 ASC/106 splenocytes; Figure 5D) while the DENV-2 specific PCs peaked at day 9 post-2° infection with lower numbers (26.3 ± 9.0 ASC/106 splenocytes; Figure 5C), suggesting that cross-reactive PCs generated from cross-reactive memory B cells or from cross-reactive semi-long-lived PCs are the main cells implicated in the humoral response after a 2° heterotypic infection as compared to homotypic PCs generated by naïve B cells responding to the second infection.
After a 1° DENV-2 infection, a large number of homotypic and cross-reactive PCs are detected in the spleen (Figure 5C and 5D). Thus, naïve B cells can respond within 6 days of a 1° DENV infection by differentiating into PCs producing antibodies against DENV-2 and cross-reactive antibodies against DENV-1. Of interest, the peak of DENV-2 specific PCs was detected at day 6 post-1° DENV-2 infection, whereas it was detected later, at day 9, post-2° DENV-2 infection (Figure 5D). This suggests that DENV Ag may be more readily captured by DENV-1-specific memory B cells or by anti-DENV-1 pre-formed Abs, thereby preventing binding and activation of naïve B cells during a 2° infection. This would be expected, as memory B cells display a higher-avidity B cell receptor than naïve B cells, and suggests that DENV-2-specific PCs detected after a 2° infection arise primarily from the DENV-1-specific memory B cell pool rather than from newly-stimulated DENV-2-specific naïve B cells.
B cells contribute to protection against a 2° lethal heterotypic DENV infection, but are neither necessary nor sufficient for protection against lethality
AG129 immune DENV-1 mice were depleted of B cells using anti-CD20 mAb. Of note, CD20 is not expressed by PCs. Efficacy of depletion was tested prior to 2° infection in whole blood cells isolated from an eye bleed. Less than 1% of the PBMCs were found to be CD19+ B220+ B cells in B cell-depleted mice (data not shown). At day 8 post-depletion, mice were infected a second time with a lethal dose of 107 PFU of DENV-2 D2S10. All the mice survived (Figure 6A) and did not show any signs of morbidity (Figure 6B), indicating that B cells are dispensable for protection against a lethal 2° heterotypic DENV infection. Of note, while B cells were completely depleted as observed by flow cytometry, and while the number of DENV-specific PCs and memory B cells decreased after B cell depletion, we could still detect DENV-specific PCs and memory B cells 6 days after a 2° heterotypic DENV infection (Figure S2A and S2B), suggesting that the B cell depletion was not absolute and even though less than 1% of the PBMCs were CD19+ B220+, there were non-depleted B cells in the tissues.
Figure 6. Mortality and morbidity after B and T cell depletions during 2° heterotypic DENV infection.
A. Survival after B and T cell depletions. AG129 mice were infected s.c. with 105 DENV-1 98J then 6 to 8 weeks p.i. were infected i.v. with 107 PFU of DENV-2 D2S10. T cell-depleted mice (n=7) were treated with anti-CD4 and anti-CD8 mAb as described in Material and Methods. B cell-depleted mice (n=4) were treated with anti-CD20 mAb as described in Material and Methods. Four mice were depleted of both B and T cells. DENV-1-immune control mice were injected with PBS (n=7) or isotype control (n=3). Naïve mice (n=4) were infected i.v. with 107 PFU of DENV-2 D2S10. Data were pooled from 2 independent experiments. Statistical analysis was performed using the Wilcoxon rank sum test to compare the different experimental groups to the naïve group. No significant differences were found. B. Morbidity after B and T cell depletions. The same mice as in Figure 6A were scored for morbidity. An event was counted as soon as the mice were recorded as sick (score = 2) as described in Material and Methods. Statistical analysis was performed using the Wilcoxon rank sum test to compare the different experimental groups to the naïve group. No significant differences were found.
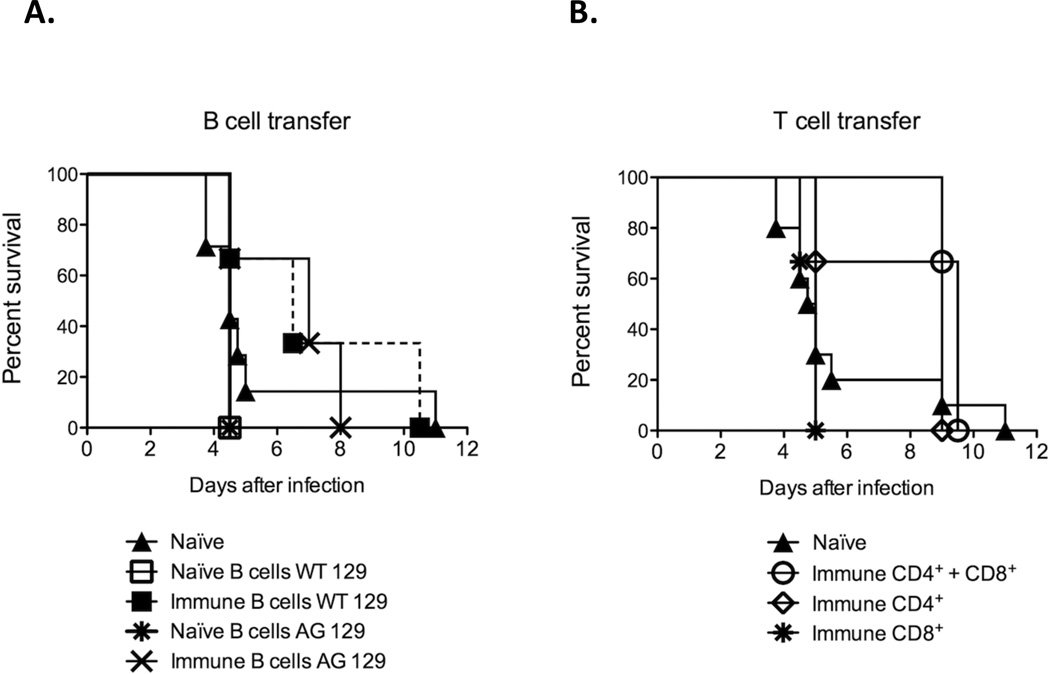
B cells isolated from AG129 or WT129 DENV-1-immune mice were adoptively transferred into AG129 naïve mice that were infected 24h later with a lethal dose of DENV-2 D2S10. We isolated B cells from WT129 in addition to AG129 mice since the absence of IFN-α/β receptor could conceivably affect the recall response of memory B cells (42). The purity of the isolated B cells varied between 95% to 98%. Although not significant, a delay in mortality was observed when comparing mice receiving B cells isolated from DENV-1-immune mice to mice receiving B cells isolated from naïve mice (median survival 6.5 days (DENV-1 immune) vs. 4.5 days (naïve) for B cells isolated from WT129 mice and 7 days (DENV-1 immune) vs. 4.5 days (naïve) for B cells isolated from AG129 mice)(Figure 7A). Of note, although mortality was delayed, mice died of vascular leak syndrome and not paralysis. Thus, cross-reactive immune B cells contribute to protection but were neither sufficient nor necessary for full protection against a 2° lethal heterotypic infection.
Figure 7. Protection against a lethal DENV-2 infection mediated by B and T cell adoptive transfers.
A. Adoptive transfer of B cells. 30×106 B cells from AG129 or WT129 naïve or DENV-1-immune mice were adoptively transferred into naïve AG129 mice (3 mice/group). Control naïve mice (n=7) received PBS with no cells. Twenty-four hours after transfer, mice were infected i.v. with 107 PFU of DENV-2 D2S10. Statistical analysis was performed using the Wilcoxon rank sum test to compare the different experimental groups to the naïve group. No significant differences were found. B. Adoptive transfer of T cells. 2×105 CD4+ T cells, CD8+ T cells, or a mixture of CD4+ and CD8+ T cells isolated from DENV-1-immune A129 mice were adoptively transferred into naïve AG129 mice (3 mice/group). Control naïve mice (n=10) received PBS with no cells. Twenty-four hours after transfer, mice were infected i.v. with 107 PFU of DENV-2 D2S10. Data shown were from one experiment. Statistical analysis was performed using the Wilcoxon rank sum test to compare the different experimental groups to the naïve group. No significant differences were found.
T cells contribute to protection against a 2° lethal heterotypic DENV infection, but are neither necessary nor sufficient for protection against lethality
AG129 DENV-1-immune mice were depleted of CD4+ and CD8+ T cells using mAbs prior to a 2° DENV-2 D2S10 lethal infection. Efficacy of depletion was tested by flow cytometry of splenocytes isolated at day 10 p.i. after observing the mice for morbidity and mortality. No CD4+ or CD8+ T cells were found in the spleen at day 10 p.i. (data not shown). Six out of seven T cell depleted mice (85%) survived the lethal challenge (Figure 6A) and displayed mild signs of morbidity including lethargy, some fur ruffling but no hunched posture between day 3 and day 6 post-2° infection (Figure 6B). In contrast, T cell non-depleted DENV-1 immune mice did not show any signs of disease with lethal DENV-2 challenge. Overall, there was no significant difference in survival between T cell-depleted and T cell-non-depleted (PBS or isotype control) DENV-1-immune mice (p=0.35). Thus, T cells contribute to protection after a 2° heterotypic DENV infection, but are not essential for protection against lethality.
CD4+, CD8+ or a mixture of CD4+ and CD8+ T cells isolated from A129 DENV-1-immune mice were adoptively transferred into AG129 naïve mice, which were infected 24h later with a lethal dose of DENV-2 D2S10. We isolated T cells from A129 mice instead of AG129 mice, as the absence of IFNγ receptor in AG129 mice could conceivably affect the recall response of memory T cells (43). The purity of the isolated T cells varied between 76.5% to 90.5% (data not shown). No significant difference in survival was observed in mice receiving different subsets of isolated T cells when compared to naïve AG129 mice injected with PBS (Figure 7B); however, delayed mortality was observed after CD4+ T cell or a mixture of CD4+ and CD8+ T cell transfers (median survival 9.0 days (DENV-1 immune) vs. 4.9 days (naïve) for CD4+ T cell and 9.5 days (DENV-1 immune) vs. 4.9 days (naïve) for CD4+ and CD8+ T cells). In contrast, transfer of CD8+ T cells alone did not delay mortality when compared to naïve mice receiving PBS (median survival 5 days (DENV-1 immune) vs. 4.9 days (naïve)). Thus, immune cross-reactive CD4+ T cells can delay mortality against a heterotypic DENV infection but are not sufficient to protect AG129 naïve mice against a lethal heterotypic infection.
Innate cellular immune response contributes to the control of initial secondary DENV heterotypic infection
AG129 DENV-1-immune mice were depleted of B and T cells using anti-CD20, anti-CD4 and anti-CD8 mAbs. Efficacy of B cell depletion was tested prior to 2° infection in whole blood cells isolated via eye bleed, and efficacy of T cell depletion was tested by flow cytometry of splenocytes isolated at day 10 p.i. after observing the mice for morbidity and mortality (data not shown). Efficacy of B cell and T cell depletions were similar to that described above. After infection with a lethal dose of DENV-2 D2S10, five out of seven mice (71%) survived (Figure 6A) and displayed only mild signs of lethargy, some fur ruffling and no hunched posture between days 3 and 6 post-2° infection (Figure 6B). In contrast, mice receiving CP treatment died at day 7.5–8.5 p.i. (21). B and T cell depletion does not affect the innate cellular immune response, whereas CP treatment does; therefore, these results suggest that innate immune cells are also implicated in the control of a 2° heterotypic infection.
Discussion
Epidemiological studies have demonstrated the association between 2° heterotypic DENV infections and severe disease (2–5). However, most 2° infections are asymptomatic or present as classic DF, suggesting a protective role for cross-reactive Abs and the cross-reactive cellular immune response. We have previously shown that pre-existing cross-reactive Abs participate in cross-protection against a 2° heterotypic DENV infection (16, 21). Here we show that DENV-1-immune mice survive a lethal infection with the mouse peripherally-adapted DENV-2 D2S10 strain. We found that pre-existing cross-reactive Abs, which play a role in protection as shown by previous experiments with CP (21), were maintained by LLPCs homing to the bone marrow as shown here by the ELISPOT assay. During the acute phase of a 2° heterotypic DENV infection, Abs with high neutralization capacity and avidity against both DENV-1 and DENV-2 were also produced. While highly neutralizing Abs were most probably secreted by naïve B cells, highly avid Abs, as shown by our avidity assay, were most likely cross-reactive Abs produced by cross-reactive memory B cells generated after the first infection against the 1° infecting serotype. These data are in accordance with the ELISPOT data that showed a greater increase in cross-reactive memory B cells and PCs during acute 2° DENV heterotypic infection as compared to homotypic cells. Of note, no direct correlation has been shown between highly neutralizing Abs and high serum avidity thus far, to our knowledge. In fact, no correlation has been found between affinity and neutralization capacities of anti-DENV mAbs (44) (K. Williams and E. Harris, unpublished data). Thus, as indicated by our neutralization and avidity assays, cross-reactive memory B cells appear to induce high-avidity Abs during a 2° heterotypic DENV infection, while naïve B cells induce highly neutralizing Abs in response to the second DENV infection. Finally, we show that T cells and the immune innate response contribute as well to full protection against a 2° DENV heterotypic infection.
The AG129 dengue mouse model exhibits several parallels with human DENV infection and disease. The DENV-2 strain D2S10 is a mouse peripherally-adapted strain that at high doses causes a lethal infection in AG129 mice by a TNF-α dependent ‘vascular-leak’ syndrome, accompanied by low platelet counts, high serum cytokines, such as TNF-α and IL-10, and high levels of soluble NS1 during DENV infection (S. Balsitis and E. Harris, unpublished) (7, 23). In this mouse model, clinical isolates from all four DENV serotypes replicate efficiently in spleen, lymph node, and bone marrow (7, 22). DENV infects relevant cells, such as macrophages, DCs, hepatocytes and bone marrow-derived myeloid cells. Thus, the AG129 model is a relevant model to study DENV pathogenesis. Although the AG129 mice lack both IFN-α/β and -γ receptors, this model reproduces both Ab-mediated protection and Ab-mediated enhancement of DENV (7, 16, 45). AG129 mice develop DENV-specific Abs that are long-lasting and protective against homologous and heterologous viral challenge (16). In addition, we have shown that the IgG isotype composition of the Abs produced by AG129 is balanced (IgG1:IgG2a:IgG2b = 1:4:1) and similar to what has been reported in wild type mice (21). Thus, the AG129 model is appropriate to study the B cell response to DENV infection in vivo. The T cell response has not been extensively characterized in these mice; however it is known that IFN-γ is necessary for a correct recall of the memory T cell response (43). Despite this, we have previously demonstrated IFN-γ production from restimulated splenocytes collected after 2° DENV infection (16), which could be attributed to T cells. In addition, we show a certain degree of T cell functionality in our model, as depletion of T cells prior to a 2° DENV infection induced morbidity, while non-depleted mice were fully protected and showed no signs of infection.
Infection with DENV confers life-long protection against infection with the same serotype, but may protect against or enhance infection with a heterologous serotype (2–5). The phenomenon of ADE (46) has been proposed, where cross-reactive anti-DENV Abs facilitate entry of DENV into Fcγ receptor (FcγR)-bearing cells (47–49), contributing to higher viremia and disease severity. Multiple factors govern the requirements for virus neutralization, including Ab affinity/serum avidity, epitope specificity, and maturation state of the virus, as well as the interaction between specific Ab isotypes, complement and FcγR (50). Thus, the same cross-reactive Abs can mediate either protection or enhancement, depending on the factors present at the time of acute 2° DENV heterotypic infection. We have previously shown that passive transfer of cross-reactive Abs are protective against a 2° DENV heterotypic infection (16) and that pre-existing cross-reactive Abs can partially mediate protection during the early phases of a 2° DENV heterotypic infection (21). We show here that neutralizing capacity of serum increases greatly after a 2° DENV heterotypic infection and that this increase is mediated by naïve B cells.
Using a modified ELISA with urea washes, we also demonstrated that serum avidity increased after a 2° DENV heterotypic infection, but this avidity was greater against the 1° infecting serotype, suggesting that cross-reactive Abs mediate this increase in avidity. Avidity is the result of Ab affinity and valency, together with the density of viral epitopes accessible for Ab binding. Ab avidity plays an important role in the immune response against viruses and correlates with the neutralizing efficacy of antibodies in vitro (51, 52). Low-avidity Abs, measured by a modified ELISA including urea washes, have been shown to provide insufficient protection against measles and respiratory syncytial virus, resulting in severe disease upon viral challenge (37, 38). Avidity ELISAs have been used to discriminate between 1° and 2° acute DENV infections in humans, as the avidity of serum to DENV increases after a 2° DENV infection (53–55). Recently, an ELISA-based competition assay measuring Ab avidity was used to characterize “original antigenic sin” in the sera of patients experiencing 1° or 2° DENV infection (56), demonstrating an increased avidity against the 1° infecting serotype. Thus, our findings of increased DENV-specific serum avidity against the 1° infecting serotype after a 2° heterotypic DENV infection is in accordance with these human studies. In addition to the studies of serum avidity, we also investigated avidity in supernatants obtained after polyclonal stimulation of splenocytes collected from mice infected with a 2° heterotypic serotype. In these supernatants, avidity increased only against the 1° infecting serotype, suggesting that these highly avid Abs, responding to the second infection, are secreted by cross-reactive memory B cells generated during the first infection. These data are in accordance with previous findings showing that after a 1° response to the hapten 4-hydroxy-3-nitrophenyl acetyl (NP), low-affinity memory B cells, potentially cross-reactive, persist in the splenic compartment, as only 65% of the splenic memory B cells were able to produce high affinity Abs (57). These findings correlate with our ELISPOT data showing a greater and earlier increase in DENV-1-specific memory B cells and PCs when compared to DENV-2-specific memory B cells, suggesting that cross-reactive memory B cells and PCs are active in the humoral response after a 2° heterotypic DENV infection by increasing DENV-specific avidity of the serum.
We demonstrate some amount of protection mediated by cross-reactive B cells in adoptive transfer experiments, but did not pinpoint which sub-cellular B cell component was implicated. The MACS sorting method used for the B cell adoptive transfer experiment did not discriminate among B cell populations, and naïve, memory B cells as well as PCs were present in the final preparation. While long-term ASC, most probably LLPCs, are found in the bone marrow, we detected DENV-specific PCs in the spleen 6 to 8 weeks after a 1° infection. These cells, most likely semi-long-lived PCs, were present in the cell preparation used for the adoptive transfers. We show that naïve B cells alone did not mediate protection; thus, either cross-reactive memory B cells (58) or cross-reactive semi-long-lived PCs are implicated in this protection. As memory B cells proliferate between day 3 and day 6 post-DENV infection, the delay in lethality observed after B cell adoptive transfer could potentially be attributed to secretion of DENV-specific Abs by the semi-long-lived PCs present in the spleen.
In the depletion studies, we used anti-CD20 mAb and did not observe any morbidity associated with B cell depletion before a 2° heterotypic DENV infection. This could indicate that the combination of pre-existing Abs and immune T cells, in association with innate immune cells, are sufficient to mediate full protection against a 2° lethal DENV infection. However, we also showed that while depletion was effective as measured by flow cytometry at day 8 post-injection in the blood, we could still detect DENV-specific PCs and memory B cells by ELISPOT at day 6 post-2° DENV infection. Thus, we cannot exclude that, while decreased in number, the remaining PCs and memory B cells contributed to the protection against the 2° heterotypic DENV infection observed after B cell depletion. Persistence of PCs and sustained Ab levels after B cell depletion with anti-CD20 mAb has been previously reported both in mouse and human studies (20, 40, 59).
In our model, despite the lack of IFN-γ receptors, we showed that T cells contribute to protection against a 2° heterotypic DENV infection, as shown by mAb-mediated depletion experiments. Our adoptive transfer data are consistent with previous studies. Cross-reactive CD8+ T cells have been implicated in the pathogenesis of severe dengue in humans (10), while only homotypic CD8+ T cells have been shown to be protective in 1° infections in mice (28). In our adoptive transfer experiments, cross-reactive DENV-1 immune CD8+ T cells did not mediate protection against a DENV-2 lethal infection. In contrast, adoptive transfer of CD4+ T cells alone or a mixture of CD4+ and CD8+ T cells mediated protection and delayed mortality. CD4+ T cells have been shown to be beneficial after vaccination, probably by increasing anti-DENV CD8+ T cell and anti-DENV Ab responses (28). Thus, adoptive transfer of immune CD4+ T cells alone could increase the Ab response induced by naïve B cells responding to the infection, resulting in a delay in mortality. Similarly, when we transferred both CD4+ and CD8+ T cells, CD4+ T cells might have increased the anti-DENV CD8+ T cell response mediating cross-protection, even though cross-reactive anti-DENV CD8+ T cells transferred alone were unable to mediate protection. This suggests that, as expected, the cross-reactive anti-DENV CD8+ T cells required CD4+ T cells to be fully activated. We have recently generated a new mouse-adapted DENV-2 strain that induces morbidity and mortality in IFN-α/β receptor KO mice (IFNAR1−/−) in both the 129 and B6 backgrounds (M. Schmid, S. Orozco and E. Harris, unpublished data). This new viral strain will allow additional T cell studies and permit testing our hypothesis about T cell cross-protection in the IFNAR1−/− model.
We have previously shown that the cellular immune response is essential for full protection against a 2° heterotypic DENV infection by treating mice with CP (21). In this report, we find that after B and T cell depletion, although mice showed signs of morbidity, most of the mice treated with the depleting mAbs survived, in contrast to mice treated with CP. In addition to abrogation of the T and B cell response, CP eliminates proliferating cells from the innate immune response, including natural killer cells and macrophages. We are currently analyzing the role of these cells using the IFNAR1−/− mouse model.
In conclusion, this study focused on the B cell response and should be relevant for studies in human populations and research on dengue vaccines. Previous epidemiological studies have suggested immune cross-protection mediated by cross-reactive Abs (14, 15, 60). Here we show that cross-reactive Abs, induced by cross-reactive memory B cells, are important for protection against heterotypic DENV infection. To extend this work, we have recently adapted our ELISPOT assay to measure DENV-specific PCs and memory B cells from PBMCs in humans (S. Zompi, M. Montoya Cruz and E. Harris, unpublished data). This current study suggests that effective vaccines should induce both robust and sustained LLPC and memory B cell responses, and analysis by ELISPOT could be explored as a correlate of protection in vaccine studies. In addition, we have shown that T cells are necessary for full protection against a 2° heterotypic DENV infection and that innate immune cells are also implicated in this protection, suggesting a complicated interplay of the different subsets of the cellular immune response. Thus, cross-reactive B cell and T cell subsets are implicated in providing cross-protection against a 2° heterotypic DENV infection, and the appearance of disease or severe disease is most probably associated with an imbalance among these immune cell subsets rather than a result of the deficiency of only one subset or the over-stimulation of another.
Supplementary Material
Acknowledgments
The authors thank Ritela Gonzalez, Ruben Lachica, Susana Orozco, and Hector Nolla for experimental assistance; Sondra Schlesinger, Katherine L. Williams and Michael A. Schmidt for scientific input in preparing the manuscript; Barbara Hibner, from Millenium Pharmaceuticals Inc., for providing Bortezomib; and Marylin Kehry, from Biogen Idec Inc., for providing the anti-CD20 mAb.
Footnotes
This work was supported by NIH grant R01A1085607 (to EH).
Nonstandard abbreviations
DENV: Dengue Virus; DF: Dengue Fever; DHF: Dengue Hemorrhagic Fever; DSS: Dengue Shock Syndrome; ADE: Antibody-Dependent Enhancement; PC: Plasma Cell; LLPC: Long-Lived Plasma Cell; DC: Dendritic Cell; CP: CycloPhosphamide; p.i.: post-infection; UC: University of California; WT: Wild-type; ASC: Antibody-Secreting Cell; NT50: 50% Neutralization Titer.
References
- 1.Gubler DJ. Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol. 2002;10:100–103. doi: 10.1016/s0966-842x(01)02288-0. [DOI] [PubMed] [Google Scholar]
- 2.Guzman MG, Kouri GP, Bravo J, Soler M, Vazquez S, Morier L. Dengue hemorrhagic fever in Cuba, 1981: a retrospective seroepidemiologic study. Am. J. Trop. Med. Hyg. 1990;42:179–184. doi: 10.4269/ajtmh.1990.42.179. [DOI] [PubMed] [Google Scholar]
- 3.Sabin AB. Research on dengue during World War II. Am. J. Trop. Med. Hyg. 1952;1:30–50. doi: 10.4269/ajtmh.1952.1.30. [DOI] [PubMed] [Google Scholar]
- 4.Sangkawibha N, Rojanasuphot S, Ahandrik S, Viriyapongse S, Jatanasen S, Salitul V, Phanthumachinda B, Halstead SB. Risk factors in dengue shock syndrome: a prospective epidemiologic study in Rayong, Thailand. I. The 1980 outbreak. Am. J. Epidemiol. 1984;120:653–669. doi: 10.1093/oxfordjournals.aje.a113932. [DOI] [PubMed] [Google Scholar]
- 5.Thein S, Aung MM, Shwe TN, Aye M, Zaw A, Aye K, Aye KM, Aaskov J. Risk factors in dengue shock syndrome. Am. J. Trop. Med. Hyg. 1997;56:566–572. doi: 10.4269/ajtmh.1997.56.566. [DOI] [PubMed] [Google Scholar]
- 6.Rothman AL. Cellular immunology of sequential dengue virus infection and its role in disease pathogenesis. Curr. Top. Microbiol. Immunol. 2010;338:83–98. doi: 10.1007/978-3-642-02215-9_7. [DOI] [PubMed] [Google Scholar]
- 7.Balsitis SJ, Williams KL, Lachica R, Flores D, Kyle JL, Mehlhop E, Johnson S, Diamond MS, Beatty PR, Harris E. Lethal antibody enhancement of dengue disease in mice is prevented by Fc modification. PLoS Pathog. 2010;6:e1000790. doi: 10.1371/journal.ppat.1000790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guzman MG, Kouri G, Valdes L, Bravo J, Alvarez M, Vazques S, Delgado I, Halstead SB. Epidemiologic studies on Dengue in Santiago de Cuba, 1997. Am. J. Epidemiol. 2000;152:793–799. doi: 10.1093/aje/152.9.793. discussion 804. [DOI] [PubMed] [Google Scholar]
- 9.Kliks SC, Nimmanitya S, Nisalak A, Burke DS. Evidence that maternal dengue antibodies are important in the development of dengue hemorrhagic fever in infants. Am. J. Trop. Med. Hyg. 1988;38:411–419. doi: 10.4269/ajtmh.1988.38.411. [DOI] [PubMed] [Google Scholar]
- 10.Mongkolsapaya J, Dejnirattisai W, Xu XN, Vasanawathana S, Tangthawornchaikul N, Chairunsri A, Sawasdivorn S, Duangchinda T, Dong T, Rowland-Jones S, Yenchitsomanus PT, McMichael A, Malasit P, Screaton G. Original antigenic sin and apoptosis in the pathogenesis of dengue hemorrhagic fever. Nat. Med. 2003;9:921–927. doi: 10.1038/nm887. [DOI] [PubMed] [Google Scholar]
- 11.Imrie A, Meeks J, Gurary A, Sukhbataar M, Kitsutani P, Effler P, Zhao Z. Differential functional avidity of dengue virus-specific T-cell clones for variant peptides representing heterologous and previously encountered serotypes. J. Virol. 2007;81:10081–10091. doi: 10.1128/JVI.00330-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangada MM, Rothman AL. Altered cytokine responses of dengue-specific CD4+ T cells to heterologous serotypes. J. Immunol. 2005;175:2676–2683. doi: 10.4049/jimmunol.175.4.2676. [DOI] [PubMed] [Google Scholar]
- 13.Beaumier CM, Mathew A, Bashyam HS, Rothman AL. Cross-reactive memory CD8(+) T cells alter the immune response to heterologous secondary dengue virus infections in mice in a sequence-specific manner. J. Infect. Dis. 2008;197:608–617. doi: 10.1086/526790. [DOI] [PubMed] [Google Scholar]
- 14.Kliks SC, Nisalak A, Brandt WE, Wahl L, Burke DS. Antibody-dependent enhancement of dengue virus growth in human monocytes as a risk factor for dengue hemorrhagic fever. Am. J. Trop. Med. Hyg. 1989;40:444–451. doi: 10.4269/ajtmh.1989.40.444. [DOI] [PubMed] [Google Scholar]
- 15.Kochel TJ, Watts DM, Halstead SB, Hayes CG, Espinoza A, Felices V, Caceda R, Bautista CT, Montoya Y, Douglas S, Russell KL. Effect of dengue-1 antibodies on American dengue-2 viral infection and dengue haemorrhagic fever. Lancet. 2002;360:310–312. doi: 10.1016/S0140-6736(02)09522-3. [DOI] [PubMed] [Google Scholar]
- 16.Kyle JL, Balsitis SJ, Zhang L, Beatty PR, Harris E. Antibodies play a greater role than immune cells in heterologous protection against secondary dengue virus infection in a mouse model. Virology. 2008;380:296–303. doi: 10.1016/j.virol.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McHeyzer-Williams LJ, McHeyzer-Williams MG. Antigen-specific memory B cell development. Annu. Rev. Immunol. 2005;23:487–513. doi: 10.1146/annurev.immunol.23.021704.115732. [DOI] [PubMed] [Google Scholar]
- 18.Leyendeckers H, Odendahl M, Lohndorf A, Irsch J, Spangfort M, Miltenyi S, Hunzelmann N, Assenmacher M, Radbruch A, Schmitz J. Correlation analysis between frequencies of circulating antigen-specific IgG-bearing memory B cells and serum titers of antigen-specific IgG. Eur. J. Immunol. 1999;29:1406–1417. doi: 10.1002/(SICI)1521-4141(199904)29:04<1406::AID-IMMU1406>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 19.Amanna IJ, Slifka MK. Mechanisms that determine plasma cell lifespan and the duration of humoral immunity. Immunol. Rev. 2010;236:125–138. doi: 10.1111/j.1600-065X.2010.00912.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahuja A, Anderson SM, Khalil A, Shlomchik MJ. Maintenance of the plasma cell pool is independent of memory B cells. Proc. Natl. Acad. Sci. U. S. A. 2008;105:4802–4807. doi: 10.1073/pnas.0800555105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams KL, Zompi S, Beatty PR, Harris E. A mouse model for studying dengue virus pathogenesis and immune response. Ann. N. Y. Acad. Sci. 2009;1171 Suppl 1:E12–E23. doi: 10.1111/j.1749-6632.2009.05057.x. [DOI] [PubMed] [Google Scholar]
- 22.Kyle JL, Beatty PR, Harris E. Dengue virus infects macrophages and dendritic cells in a mouse model of infection. J. Infect. Dis. 2007;195:1808–1817. doi: 10.1086/518007. [DOI] [PubMed] [Google Scholar]
- 23.Shresta S, Sharar KL, Prigozhin DM, Beatty PR, Harris E. Murine model for dengue virus-induced lethal disease with increased vascular permeability. J. Virol. 2006;80:10208–10217. doi: 10.1128/JVI.00062-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balsitis SJ, Coloma J, Castro G, Alava A, Flores D, McKerrow JH, Beatty PR, Harris E. Tropism of dengue virus in mice and humans defined by viral nonstructural protein 3-specific immunostaining. Am. J. Trop. Med. Hyg. 2009;80:416–424. [PubMed] [Google Scholar]
- 25.Prestwood TR, Prigozhin DM, Sharar KL, Zellweger RM, Shresta S. A mouse-passaged dengue virus strain with reduced affinity for heparan sulfate causes severe disease in mice by establishing increased systemic viral loads. J. Virol. 2008;82:8411–8421. doi: 10.1128/JVI.00611-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loveless SE, Ladics GS, Smith C, Holsapple MP, Woolhiser MR, White KL, Jr, Musgrove DL, Smialowicz RJ, Williams W. Interlaboratory study of the primary antibody response to sheep red blood cells in outbred rodents following exposure to cyclophosphamide or dexamethasone. J. Immunotoxicol. 2007;4:233–238. doi: 10.1080/15476910701385687. [DOI] [PubMed] [Google Scholar]
- 27.Miyauchi A, Hiramine C, Tanaka S, Hojo K. Differential effects of a single dose of cyclophosphamide on T cell subsets of the thymus and spleen in mice: flow cytofluorometry analysis. Tohoku J. Exp. Med. 1990;162:147–167. doi: 10.1620/tjem.162.147. [DOI] [PubMed] [Google Scholar]
- 28.Yauch LE, Zellweger RM, Kotturi MF, Qutubuddin A, Sidney J, Peters B, Prestwood TR, Sette A, Shresta S. A protective role for dengue virus-specific CD8+ T cells. J. Immunol. 2009;182:4865–4873. doi: 10.4049/jimmunol.0801974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yauch LE, Prestwood TR, May MM, Morar MM, Zellweger RM, Peters B, Sette A, Shresta S. CD4+ T cells are not required for the induction of dengue virus-specific CD8+ T cell or antibody responses but contribute to protection after vaccination. J. Immunol. 2010;185:5405–5416. doi: 10.4049/jimmunol.1001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holden KL, Stein DA, Pierson TC, Ahmed AA, Clyde K, Iversen PL, Harris E. Inhibition of dengue virus translation and RNA synthesis by a morpholino oligomer targeted to the top of the terminal 3' stem-loop structure. Virology. 2006;344:439–452. doi: 10.1016/j.virol.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 31.Shresta S, Kyle JL, Robert Beatty P, Harris E. Early activation of natural killer and B cells in response to primary dengue virus infection in A/J mice. Virology. 2004;319:262–273. doi: 10.1016/j.virol.2003.09.048. [DOI] [PubMed] [Google Scholar]
- 32.Kraus AA, Messer W, Haymore LB, de Silva AM. Comparison of plaque- and flow cytometry-based methods for measuring dengue virus neutralization. J. Clin. Microbiol. 2007;45:3777–3780. doi: 10.1128/JCM.00827-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lindsey NP, Schroeder BA, Miller ER, Braun MM, Hinckley AF, Marano N, Slade BA, Barnett ED, Brunette GW, Horan K, Staples JE, Kozarsky PE, Hayes EB. Adverse event reports following yellow fever vaccination. Vaccine. 2008;26:6077–6082. doi: 10.1016/j.vaccine.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 34.Benner R, van Oudenaren A, Koch G. Induction of antibody formation in mouse bone marrow. New York: Academic Press; 1981. [Google Scholar]
- 35.Crotty S, Aubert RD, Glidewell J, Ahmed R. Tracking human antigen-specific memory B cells: a sensitive and generalized ELISPOT system. J. Immunol. Methods. 2004;286:111–122. doi: 10.1016/j.jim.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 36.Pierson TC, Sanchez MD, Puffer BA, Ahmed AA, Geiss BJ, Valentine LE, Altamura LA, Diamond MS, Doms RW. A rapid and quantitative assay for measuring antibody-mediated neutralization of West Nile virus infection. Virology. 2006;346:53–65. doi: 10.1016/j.virol.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 37.Delgado MF, Coviello S, Monsalvo AC, Melendi GA, Hernandez JZ, Batalle JP, Diaz L, Trento A, Chang HY, Mitzner W, Ravetch J, Melero JA, Irusta PM, Polack FP. Lack of antibody affinity maturation due to poor Toll-like receptor stimulation leads to enhanced respiratory syncytial virus disease. Nat. Med. 2009;15:34–41. doi: 10.1038/nm.1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Polack FP, Hoffman SJ, Crujeiras G, Griffin DE. A role for nonprotective complement-fixing antibodies with low avidity for measles virus in atypical measles. Nat. Med. 2003;9:1209–1213. doi: 10.1038/nm918. [DOI] [PubMed] [Google Scholar]
- 39.Slifka MK, Ahmed R. Long-lived plasma cells: a mechanism for maintaining persistent antibody production. Curr. Opin. Immunol. 1998;10:252–258. doi: 10.1016/s0952-7915(98)80162-3. [DOI] [PubMed] [Google Scholar]
- 40.Slifka MK, Antia R, Whitmire JK, Ahmed R. Humoral immunity due to long-lived plasma cells. Immunity. 1998;8:363–372. doi: 10.1016/s1074-7613(00)80541-5. [DOI] [PubMed] [Google Scholar]
- 41.Cenci S, Mezghrani A, Cascio P, Bianchi G, Cerruti F, Fra A, Lelouard H, Masciarelli S, Mattioli L, Oliva L, Orsi A, Pasqualetto E, Pierre P, Ruffato E, Tagliavacca L, Sitia R. Progressively impaired proteasomal capacity during terminal plasma cell differentiation. EMBO J. 2006;25:1104–1113. doi: 10.1038/sj.emboj.7601009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanzavecchia A, Bernasconi N, Traggiai E, Ruprecht CR, Corti D, Sallusto F. Understanding and making use of human memory B cells. Immunol. Rev. 2006;211:303–309. doi: 10.1111/j.0105-2896.2006.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sercan O, Stoycheva D, Hammerling GJ, Arnold B, Schuler T. IFN-gamma receptor signaling regulates memory CD8+ T cell differentiation. J. Immunol. 2010;184:2855–2862. doi: 10.4049/jimmunol.0902708. [DOI] [PubMed] [Google Scholar]
- 44.Gromowski GD, Barrett AD. Characterization of an antigenic site that contains a dominant, type-specific neutralization determinant on the envelope protein domain III (ED3) of dengue 2 virus. Virology. 2007;366:349–360. doi: 10.1016/j.virol.2007.05.042. [DOI] [PubMed] [Google Scholar]
- 45.Zellweger RM, Prestwood TR, Shresta S. Enhanced infection of liver sinusoidal endothelial cells in a mouse model of antibody-induced severe dengue disease. Cell Host Microbe. 2010;7:128–139. doi: 10.1016/j.chom.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Halstead SB. Immune enhancement of viral infection. Prog. Allergy. 1982;31:301–364. [PubMed] [Google Scholar]
- 47.Halstead SB, O'Rourke EJ. Dengue viruses and mononuclear phagocytes. I. Infection enhancement by non-neutralizing antibody. J. Exp. Med. 1977;146:201–217. doi: 10.1084/jem.146.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Halstead SB, O'Rourke EJ. Antibody-enhanced dengue virus infection in primate leukocytes. Nature. 1977;265:739–741. doi: 10.1038/265739a0. [DOI] [PubMed] [Google Scholar]
- 49.Parren PW, Burton DR. The antiviral activity of antibodies in vitro and in vivo. Adv. Immunol. 2001;77:195–262. doi: 10.1016/S0065-2776(01)77018-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pierson TC, Fremont DH, Kuhn RJ, Diamond MS. Structural insights into the mechanisms of antibody-mediated neutralization of flavivirus infection: implications for vaccine development. Cell Host Microbe. 2008;4:229–238. doi: 10.1016/j.chom.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burton DR. Antibodies, viruses and vaccines. Nat. Rev. Immunol. 2002;2:706–713. doi: 10.1038/nri891. [DOI] [PubMed] [Google Scholar]
- 52.Dowd KA, Pierson TC. Antibody-mediated neutralization of flaviviruses: a reductionist view. Virology. 2011;411:306–315. doi: 10.1016/j.virol.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Souza VA, Fernandes S, Araujo ES, Tateno AF, Oliveira OM, Oliveira RR, Pannuti CS. Use of an immunoglobulin G avidity test to discriminate between primary and secondary dengue virus infections. J. Clin. Microbiol. 2004;42:1782–1784. doi: 10.1128/JCM.42.4.1782-1784.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Matheus S, Deparis X, Labeau B, Lelarge J, Morvan J, Dussart P. Use of four dengue virus antigens for determination of dengue immune status by enzyme-linked immunosorbent assay of immunoglobulin G avidity. J. Clin. Microbiol. 2005;43:5784–5786. doi: 10.1128/JCM.43.11.5784-5786.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Matheus S, Deparis X, Labeau B, Lelarge J, Morvan J, Dussart P. Discrimination between primary and secondary dengue virus infection by an immunoglobulin G avidity test using a single acute-phase serum sample. J. Clin. Microbiol. 2005;43:2793–2797. doi: 10.1128/JCM.43.6.2793-2797.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Midgley CM, Bajwa-Joseph M, Vasanawathana S, Limpitikul W, Wills B, Flanagan A, Waiyaiya E, Tran HB, Cowper AE, Chotiyarnwon P, Grimes JM, Yoksan S, Malasit P, Simmons CP, Mongkolsapaya J, Screaton GR. An in-depth analysis of original antigenic sin in dengue virus infection. J. Virol. 2011;85:410–421. doi: 10.1128/JVI.01826-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith KG, Light A, Nossal GJ, Tarlinton DM. The extent of affinity maturation differs between the memory and antibody-forming cell compartments in the primary immune response. EMBO J. 1997;16:2996–3006. doi: 10.1093/emboj/16.11.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hebeis BJ, Klenovsek K, Rohwer P, Ritter U, Schneider A, Mach M, Winkler TH. Activation of virus-specific memory B cells in the absence of T cell help. J. Exp. Med. 2004;199:593–602. doi: 10.1084/jem.20030091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cambridge G, Leandro MJ, Edwards JC, Ehrenstein MR, Salden M, Bodman-Smith M, Webster AD. Serologic changes following B lymphocyte depletion therapy for rheumatoid arthritis. Arthritis Rheum. 2003;48:2146–2154. doi: 10.1002/art.11181. [DOI] [PubMed] [Google Scholar]
- 60.Sabin AB. The dengue group of viruses and its family relationships. Bacteriol. Rev. 1950;14:225–232. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.