Abstract
Otitis media is an important and a highly prevalent disease of the middle ear and poses serious health problem world wide especially in developing countries where large percentage of the population lack specialized medical care, suffer from malnutrition and live in poor hygienic environmental conditions. It has been a general view that the hearing loss increases with the size of the perforation, more so if it is in the posterio inferior quadrant. It was found that the maximum average loss occurred at 250 Hz. The hearing loss is less in small perforations (less than 2 mm diameter) then in larger ones; less in perforations touching the manubrium than in those away from it, and also less in perforations of the anterioinferior quadrant than in those on posterio-inferior quadrant. A normally functioning eustachian tube is also an essential physiologic requirement for a healthy middle ear and normal hearing.
Keywords: Tubotympanic CSOM, Tympanic membrane perforation, Eustachian tube function, Three flap tympanoplasty
Introduction
Otitis media is an important and a highly prevalent disease of the middle ear and poses serious health problem world wide especially in developing countries where large percentage of the population lack specialized medical care, suffer from malnutrition and live in poor hygienic environmental conditions.
It has been a general view that the hearing loss increases with the size of the perforation, more so if it is in the posterio inferior quadrant. It was found that the maximum average loss occurred at 250 Hz. The hearing loss is less in small perforations (less than 2 mm diameter) then in larger ones; less in perforations touching the manubrium than in those away from it, and also less in perforations of the anterio inferior quadrant than in those on posterio-inferior quadrant. A normally functioning eustachian tube is also an essential physiologic requirement for a healthy middle ear and normal hearing. To sum up, because of the high incidence of conductive hearing loss caused by central perforations of tympanic membrane, the conflicting reports regarding the effect of perforations on hearing loss, and of the importance of normal eustachian tube function in tympanoplasty operations, this project has been under taken to study the clinical profile of CSOM; effects of site and size of tympanic membrane perforation on degree of hearing loss, eustachian tube function and assessment of improvement in hearing following tympanoplasty operations.
The present study is an effort to test the validity of above concepts.
Aims and Objectives
To study the clinical profile of CSOM
To study the predisposing factors for development of CSOM.
Correlation of hearing loss with size and site of TM perforation and ossicular damage/pathology.
To find out commoner causative organisms from discharging ear.
To study the effect of Eustachian tube function on result of tympanoplasty.
Correlation of Eustachian tube function findings between antibiotic ear drop instillation, auscultation tube and ETF by tympanometry.
To assess the result of surgical treatment of tubotympanic chronic suppurative otitis media.
Materials and Methods
This is a prospective study carried out in the department of E.N.T. & Head and Neck Surgery.
All cases of tubotympanic type of CSOM in the age group 15–60 years attending E.N.T. & H.N.S. out patient department were included in this study. All the cases underwent detailed history taking followed by a general physical examination and examination of Ear, Nose and Throat. The relevant details were recorded and cases were then subjected to following investigations. Complete blood count and urine analysis was done in all the cases.
Specific Investigations
Audiological tests
Pure tone audiometry (PTA)
Speech discrimination score (SDS)
Eustachian tube function (ETF)
Eustachian tube function was assessed by three ways:
(a) Instillation of antibiotic ear drop
(b) Auscultation tube test.
(c) ET functions by tympanometry.
Otomicroscopy
Aural swab for culture sensitivity
Patch test
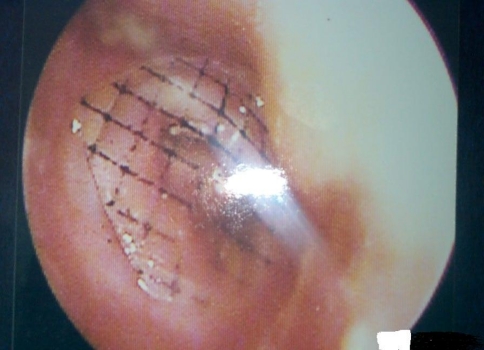
To measure the size of perforation, thin and transparent plastic paper were used and over it graphs of 1 mm2 were drawn, oval pieces of about 9 mm × 8 mm size is cut and sterilized by keeping in cidex, under operating microscope with magnification ×15 sterile plastic with graph imprinted on it is kept over the TM perforation number of square occupying the perforation will be directly counted, if half or more of any square is within the perforation it is taken to be one square and if less than half of a square is within the perforation, it is not counted (Fig. 1).
Fig. 1.
Measurement of size of perforation of tympanic membrane, thin and transparent plastic paper were used and over it graphs of 1 mm2 were drawn
All the patients with discharging ear were treated conservatively using Antibiotics, Antihistaminic, Decongestants and topical ear drops to be instilled by displacement method and once a dry ear was achieved
Tympanoplasty or Myringoplasty was performed. Preoperative assessment of status of ear before surgery (quiescent/inactive), ET function, type of hearing loss (conductive/mixed/SNHL) were done and recorded.
Surgical Procedure was planned according to size of perforation.
For small perforations, modified inlay method was used.
For small to moderate perforations, routine underlay procedure was used.
For large to subtotal perforations or total perforation, three flap technique was used.
For anterior perforations with small margin, bucket handle technique was used.
Three follow up visits at 21, 45 days and 3 months during which assessment of graft uptake by otoscopy, subjective evaluation (hearing, tinnitus, and any other complaints); otoscopy and repeat PTA and ETF were done. These findings were then evaluated and compared with preoperative findings.
Observations
The present study was carried out in 50 patients (64 ears) with unilateral or bilateral perforation of tympanic membrane for a period of 2 years. All cases of tubotympanic type of CSOM were included in the study and followed up to 3 months of surgical treatment (Table 1).
Table 1.
Site of tympanic membrane perforation according to quadrant involved by perforation (n = 64)
| Site of perforation according to quadrant | No. of ears | Percentage |
|---|---|---|
| AI | 3 | 4.68 |
| PI | 3 | 4.68 |
| AS + AI | 10 | 15.62 |
| PS + PI | 6 | 9.37 |
| AI + PI | 12 | 18.75 |
| AS + AI + PI | 9 | 14.06 |
| AS + AI + PS + PI | 21 | 32.8 |
Age wise, majority of the patients belonged to the age group ranging from 21 to 30 years with a slight female predominance.
Most of tympanic membrane perforations i.e. 59 (92.18%) were infective in origin. In the remaining 5 (7.82%) cases trauma was the cause of tympanic membrane perforation (pricking of ear in 3 cases, slap on ear in 1 case and loud sound (fire cracker) in 1 case.
Otorrhoea was the commonest complaint 52 (81.25%) with which patients presented to hospital, followed by hearing impairment in 40 (62.50%), itching in the ear in 6 (9.37%), tinnitus in 12 (18.75%), Trauma to the ear was seen in 5 (7.81%) cases and pain in the ear in 2 (3.12%) cases.
An otological examination revealed thirty-four (68%) patients had a dry tympanic membrane perforation, out of which 10 were bilateral perforation. 16 (32%) patients had discharging ear out of which 4 had bilateral perforation. The left ear was predominantly involved in 21 (58.33%).
On ascertaining the size of tympanic membrane perforation it was observed that out of 64 ears, 6 (9.37%) were having small TM perforation, 28 (43.75%) were having moderate TM perforation, 9 (14.06%) were having large TM perforation and 21 (32.81%) were having subtotal or total TM perforation.
Maximum number of tympanic membrane perforations, involved all the four quadrants 21 (32.8%). Out of the 16 discharging ears maximum number showed a growth of Pseudomonas aeruginosa 8 (50%), followed by Coagulase positive Staphylococcus in 2 (12.5%) cases and Klebsiella pneumoniae also in 2 (12.5%) cases, Escherichia coli in 1 (6.26%) case on aural swab culture.
On assessing hearing loss on pure tone Audiometry it was observed that most of the patients included in the study were having pure conductive hearing loss 59 (92.18%), 5 (7.82%) ears had mixed hearing loss and none of the ears had pure sensorineural hearing loss.
The total effective surface area of the tympanic membrane was taken to be 55 mm2 and the sizes of perforation were categorized as:
1–14 mm2, i.e. <25% of total effective tympanic membrane surface area involved by perforation.
15–27 mm2, i.e. 25–50% of total effective tympanic membrane surface area perforated.
28–41 mm2, i.e. 50–75% of effective tympanic membrane surface area perforated and
42–55 mm2, i.e. 75–100% of effective tympanic membrane surface area involved by the perforation.
Maximum numbers of ear i.e. 28 were having size of tympanic membrane perforation between 15 and 27 mm (25–50%) of effective tympanic membrane surface area with an average hearing loss of 35 dB while larger perforations involving 42–55 mm (75–100%) of effective tympanic membrane surface area suffered from an average loss of 44 dB (Table 2).
Table 2.
Hearing loss according to tympanic membrane involvement, i.e. area occupied by perforation (n = 64)
| Size of perforation (mm2) | % of TM involved by perforation | No. of ears | Average hearing loss (dB) |
|---|---|---|---|
| 1–14 | <25 | 6 | 28.23 |
| 15–27 | 25–50 | 28 | 32.42 |
| 28–41 | 50–75 | 9 | 36.26 |
| 42–55 | 75–100 | 21 | 44.62 |
It was observed that maximum numbers of ears had all the four quadrants involved by the perforation i.e. in 21 (32.8%) ears, and on correlating the hearing loss according to site of tympanic membrane perforation, maximum average hearing loss 44.6 dB was in the perforations involving all the four quadrants, followed by three quadrant perforations i.e., (AS + AI + PI) and PS + PI perforation (Table 3).
Table 3.
Hearing loss according to site of tympanic membrane perforation (n = 64)
| Site | Quadrant | No. of ears | Percentage | Average hearing loss (dB) |
|---|---|---|---|---|
| Single | AI | 3 | 4.68 | 26.6 |
| PI | 3 | 4.68 | 32.4 | |
| Two quadrant | AS + AI | 10 | 15.62 | 28.6 |
| PS + PI | 6 | 9.37 | 36.6 | |
| AI + PI | 12 | 18.75 | 32 | |
| Three quadrant | AS + AI + PI | 9 | 14.06 | 36.6 |
| Four quadrant | AS + AI + PS + PI | 21 | 32.8 | 44.6 |
Out of 64 ears 7 ears had ossicular chain pathology, handle of malleus was eroded in 4 (6.25%) cases and long process of incus was eroded in 3 (4.68%) cases. An average hearing loss was 46.6 dB in perforations with handle of malleus erosion and 54.3 dB in ears with long process of incus erosion was observed. We also observed that malleolar perforations had significantly greater hearing loss than non malleolar perforations. In perforations occupying <25% of TM surface area, the difference is mean average hearing losses of malleolar and non malleolar perforations was 3.41 dB which was statistically significant (z = 2.72; P < 0.01). It was 3.8 dB in cases of perforations occupying 25–50% of effective surface area of TM which was also statistically significant (z = 5; P < 0.01).
The assessments of eustachian tube function by antibiotic ear drop instillation, auscultation of tube and ETF by Impedance audiometer were compared. It was observed that out of 50 ears, 38 ears had normal ETF by all the three methods i.e. antibiotic ear drop instillation, auscultation tube and ETF by impedance audiometry. Out of 12 ears with Eustachian tube dysfunction, 4 had ETD by all the three methods, 6 ears by means of Impedance audiometry and 2 by only antibiotic instillation.
It was observed that out of 38 ears with normal Eustachian tube function, graft was accepted in 34 (89.47%) of cases and rejected in 4 (10.52%) of cases probably because of severe URTI and incompliance of the patient to proper post operative care advised on discharge.
Whereas in case of ears with Eustachian tube dysfunction i.e. 12 ears, graft was accepted in 6 (50%) cases and rejected in 6 (50%) cases
During the study period 50 tympanoplasties were performed by the same ENT surgeon and in the same setup and result was assessed according to
Graft Uptake Rate
Out of 50 patients who underwent tympanoplasty during the study period, graft was accepted in 40 (80%) patients and rejected in 10 (20%) patients. On assessing the cause of graft rejection in 10 patients it was observed that 6 patients were having eustachian tube dysfunction, 2 patients were having middle ear risk index score of 7–12 i.e. severe disease, and 2 patient developed post operative upper respiratory tract infection.
Improvement in Hearing Following Surgery
Pre operative and post operative audiometric pattern of 40 patients with healed graft were compared and the amount of air bone gap closure achieved was noted. It was observed that maximum number of ears 33 (82.5%) achieved air bone gap closure of 0–10 dB.
On correlating average hearing gain postoperatively with eustachian tube function in the ears with healed graft i.e. 40 ears. It was observed that in ears with normal eustachian tube function post operative hearing gain was 62.4% whereas in ears with eustachian tube dysfunction post operative hearing gain was 51.8%.
Of the 50 tympanoplasties performed, 26 were done by endaural approach using three flap technique, 16 were done by post aural approach using routine underlay technique, 5 was done by post aural approach using bucket handle technique and 3 were done modified inlay technique (Table 4).
Table 4.
Result of tympanoplasty by different techniques used (n = 50)
| Technique | No of ears | % | Graft accepted | % | Graft rejected | % |
|---|---|---|---|---|---|---|
| Three flap | 26 | 52 | 21 | 80.76 | 5 | 19.23 |
| Routine underlay | 16 | 32 | 12 | 75.00 | 4 | 25.00 |
| Bucket handle | 5 | 10 | 4 | 80.00 | 1 | 20.00 |
| Modified inlay | 3 | 6 | 3 | 100 | 0 | 0 |
Discussion
A study on clinical profile of CSOM tubotympanic type with special reference to audiometric pattern in relation with site and size of tympanic membrane perforation and surgical management with special reference to three flap technique of tympanoplasty was carried out in 50 patients (64 ears).
Studies that investigated the relationship between age and otitis media reported that otitis media has its peak incidence and prevalence in preschool years and it decreased as age increased. Cases below 10 years were not included as they would not have cooperated in the measurement of hearing, size of tympanic membrane perforation and Eustachian tube function.
The maximum number of patients in our study i.e. 19 (38%) were in the age group of 21–30 years and minimum number of patients i.e. 1 (2%) were in the age group of 61–70 and 71–80 years. The number of patients decreased as age increased.
Both sexes were almost equally affected with slight female preponderance. 48% patients were male and 52% patients were female in this study. However, several studies reported that otitis media was more common among males than females Our study is very well in agreement with another reports which showed figures of 91.3% infective, 4.6% traumatic and 4.1% unknown causes of permanent tympanic membrane perforation (Sade and Halevy 1976).
Pseudomonas aeruginosa was the commonest organism grown (50%) followed by Coagulase positive Staphylococcus and K. pneumoniae (12.5%). This finding is parallel with some other reports where P. aeruginosa was isolated as the commonest organism in CSOM.
The commonest complaint was observed to be otorrhoea, followed by hearing impairment which is very well with the view of many authors. Unilateral involvement of ears in the entire study group was seen in 72% cases while bilateral involvement was seen in 28% of patients. These figures are approximate to other reported figures viz. 77.1 and 22.9, 80.95 and 19.05%. Out of the unilaterally involved ears, it was seen that left ear was more commonly involved in our study (58.33%).
The average hearing losses, measured on pure tone audiometry, of the entire study group were in the range of 26–70 dB, most of the patients having conductive hearing loss (92.18%), however some of them had mixed hearing loss (7.82%). This is in agreement with the general concept that in safe type of CSOM with simple perforation of loss is mostly of conductive type. In this study most of the hearing losses were in the range of 26–40 dB in 50% of patients and between 41 and 55 dB in 42.19% patients. The range of hearing loss is also nearly in agreement with other studies, i.e. <42, 25–40, <50, 20–45, >20 dB.
More recently the occurrence of sensorineural hearing loss in chronic discharging ears has been recognized. This sensorineural loss is in the high frequencies and is thought to result from passage of bacterial toxins across the round window membrane to cochlea. The average hearing loss was 28.23 dB in perforations involving <25% of effective vibrating tympanic membrane surface area, 32.42 dB in perforations involving 25–50%, 36.26 dB in perforations involving 50–75 and 44.62% in perforations involving 75–100% of effective vibratory tympanic membrane surface area. Average hearing loss in perforations involving 25–50% of effective surface area of TM was significantly greater than that of perforations involving <25% TM surface area (P < 0.01). Similar observation were found when average hearing losses of perforations occupying 50–75% of area and 25–50% of TM surface area were compared (P < 0.01), greater the size of tympanic membrane perforation more was the hearing loss. This finding thus supports the previous findings that hearing loss increases with size of the perforation.
In our study, we observed that malleolar perforations had significantly greater hearing loss than non-malleolar perforations. In perforations occupying <25% of TM surface area, the difference is mean average hearing losses of malleolar and non malleolar perforations was 3.41 dB which was statistically significant. (z = 2.72; P < 0.01). It was 3.8 dB in cases of perforations occupying 25–50% of effective surface area of TM and this difference was again statistically significant (z = 5; P < 0.01). This finding does not coincide with the observation made by Pyne and Githler (1951), that hearing loss is greater in perforations not touching manubrium than that of perforations touching it. But our observation is in agreement with that of some authors who also found greater hearing loss in malleolar perforations. The observations can be explained on the basis that when membrane contact with the handle of malleus is lost, the ability of handle of malleus to move is affected. Thus, the tympanic membrane is effective only so far as it communicates its motion through its attachment to the handle of malleus and not otherwise. It follows that a perforation would have a serious effect when it is located in the vicinity of its attachment to the handle of malleus. Hence malleolar perforations will have a greater hearing loss than non-malleolar perforations in which transmission of vibrations to the handle of malleus is more effective.
Perforation involving single quadrants i.e. occupying either AI or PI quadrants, larger sized perforations (>7 mm2) had significantly greater hearing loss than smaller sized perforations (<4 mm2). It was also observed that in identical sized perforations, malleolar perorations had greater hearing loss than the non-malleolar perforations which was in agreement with another report where even in small perorations occupying <10% of TM, malleolar perorations had greater hearing loss than non-malleolar perforations. However, our finding contradicts another finding that a small lesion in the umbo region causes least hearing loss.
The average hearing losses for the same size of perforations in the AI quadrant and PI quadrant were compared and it was seen that hearing loss was more in cases of PI quadrant perforations, however when tested by t test the difference was insignificant (t = 1.04; P > 0.1).
Our findings, in this respect could not confirm conclusively the view of other investigators who stated that site is an important determinant of hearing loss and posterior perforations cause greater hearing loss than anterior perforations. Whereas our findings were more in line with Austin (1978); who upheld an opinion that perforations resulting form disease show little difference in hearing loss due to site of perforation.
This insignificant difference in average hearing losses of AI and PI quadrant perforations might be because the posterior perorations were of small size and confined to posteroinferior quadrants. Besides, round window membrane is located deep within a niche. So these perforations might not have been as effective as larger perforations in removing round window protection and phase difference.
Perforations involving two quadrants located over AS + AI quadrants, those occupying 25–50% of effective vibratory surface area of TM had significantly greater hearing loss than those involving <25% of effective TM surface area (t = 5.33; P < 0.01). In the perforations involving <25% of effective vibratory surface area of TM, those perforations in PS and PI quadrants had significantly greater hearing loss than those perorations in AS + AI quadrants (t = 4.19; P < 0.02). Here this observation goes more in favor of the view that posterior perforations cause more hearing loss than anterior perforations (Table 5).
Table 5.
Comparison of hearing loss in identical size anterioinferior and posteroinferior quadrant perorations
| Size of TM perforation (mm2) | Average hearing loss or the size in anterioinferior (AI) quadrant (dB) | Average hearing loss or the size in posteroinferior (PI) quadrant (dB) |
|---|---|---|
| 2 | 19.65 | 21.66 |
| 4 | 21.9 | 23.9 |
| 7 | 25 | 25 |
| 8 | 25 | – |
| 9 | 28 | 30 |
The perforations in the PS + PI quadrants (i.e., involving two quadrants were larger than those perforations occupying only PI (i.e., single) quadrant in the previous case. These larger sized perforations of the posterior quadrants might cause effective loss of round window protection and phase difference. Thus, hearing loss in large posterior quadrant (s) perforations becomes significantly greater than the same sized anterior quadrant perforations.
In case of perforations located over AI and PI quadrants, those occupying 25–50% of TM surface area had significantly greater hearing loss than those covering <25% of effective vibrating surface area of tympanic membrane (t = 3,8; P < 0.01). Thus, a linear relation between size of perforation and amount of hearing loss was seen again. Another observation which was in parallel with previous findings was that in identical sized perforations, malleolar perforations produced greater hearing loss than the non malleolar perforations.
Perforations involving three quadrants distributed over AS + AI + PI quadrant perforation or occupying PS + PI + AI quadrants could not be found. In this case the difference in mean average hearing losses of perforations involving <25 and 25–50% of effective vibratory surface of TM was insignificant (t = 1.19; P > 0.05). This might be because a little difference in the sizes of perforations was not causing significant difference in hearing especially when the perforations were occupying multiple quadrants.
Perforations involving all four quadrants occupying 50–70% of vibratory surface area of TM had significantly greater hearing loss than those occupying 25–50% of TM surface area (t = 6.32; P < 0.0005). Though the statistical significance could not be calculated, it was seen that perforations occupying 25–50% of TM surface area had greater hearing loss than the perforation (single perforation) covering <25% of TM surface area. All the perforations were malleolar. Here again, it was in agreement with previous findings of many authors.
Fifty ears were subjected to Myringoplasty during the period of study and followed till the fate of grafted TM was evident. It was observed that out of 38 ears with normal Eustachian tube function graft was accepted in 34 (89.47%) of cases and rejected in 4 (10.52%) of cases. Whereas in case of ears with Eustachian tube dysfunction i.e. 12 ears, graft was accepted in 6 (50%) cases and rejected in 6 (50%) cases. Though there were slight differences in observed figures, our inference from this observation can be kept at par with other observations stating a good correlation between preoperative tubal function and results of myringoplasty and good presurgical tubal function generally permitted good surgical result. Thus, it was seen that a high success rate of myringoplasty surely seen in ears having normal Eustachian tube function. On the basis of our observations, we thus disagree with the view that there is no reliable correlation between preoperative Eustachian tube function and result of myringoplasty.
The results of myringoplasty in relation to ET function and technique of operations were also analyzed. It was seen that whatever may be the technique, myringoplasty was unsuccessful in ears having Eustachian tube dysfunction, this observation again strengthen the opinion that Eustachian tube function is an important determinant of result of myringoplasty operation.
Considering the ears with healed graft in cases with normal ET function and with mild ET hypofunction the postoperative hearing gain was better in those ears with normal ET function (62.4%) than that in ears with preoperative mild hypofunction (51.8%). Postoperative hearing gain was better in ears having good preoperative ET function n all the studies. Thus, it is obvious that preoperative tubal function also influences the postoperative hearing improvement.
Out of 50 patients who underwent tympanoplasty during the study period graft was accepted in 40 (80%) patients and rejected in 10 (20%) patients. On assessing the cause of graft rejection in 10 patients it was observed that 6 patients were having eustachian tube dysfunction, 2 patients were having middle ear risk index score of 7–12 i.e. severe disease, and 2 patients developed post operative upper respiratory tract infection.
The endaural incision gives good access to posterior perforations while the post auricular incision gives better anterior exposure. The modified endaural incision used in the present study for three flap technique of tympanoplasty proved to be adequate enough for very large or subtotal perforations and also in ears with anterior bony overhang. Most of the tympanoplasties (52%) were performed by three flap technique. The three flaps used in the present study (superior, anterior, and posterior) produced an adequate exposure in all the cases either in very large or subtotal perforations, in cases with anterior bony overhangs or very anterior rim. The anterior flap can be elevated even in cases with bony overhangs and is not difficult to perform. The annulus cut at the 6 o’ clock position does not create any problem subsequently. In cases where only two flaps are fashioned (Sambaugh 1967), the lower flap may become bulky and create problem particularly in ears with narrow canals. This is not a problem in our three flap technique.
In this study the three flap technique proved to be a better technique (graft uptake—80.76%) as compared to the routine underlay technique for large and subtotal perforations where the graft uptake rate was 75% in our study as well as by bucket handle technique where graft uptake rate was 80%. The superior vascular strip is the principal supply to the majority of the graft, so placement of superior vascular strip is mandatory to prevent graft rejection. For small sized perforation with adequate tympanic membrane remnant all around modified inlay technique proved to be very good with 100% graft uptake rate in our study.
Regarding reporting hearing results, the following guidelines for air bone closure have been recommended: 0–10 dB, excellent; 10–20 dB, good; 20–30 dB, fair; and more than 30 dB, poor.
In the present study, considering the successful cases the post operative air bone gap closure was recorded to be within 0–10 dB that is excellent in 82.5% of cases, within 10–20 dB that is good in 12.5% of cases and within 20–30 dB that is fair in 5% cases. None of the patients were having air bone closure of more than 30 dB that is poor.
Conclusion
Young and middle aged population of low socio-economic class are the most common suffers of suppurative otitis media. Tympanic membrane perforations are long standing and they are poorly treated (usually with ear drops only) by general practitioners in this group.
Unilateral ear involvement (that too on left side in majority of cases) in CSOM has been found more commonly than bilateral ear involvement.
Hearing losses as on PTA in dry TM perforations range from 16 to 46 dB (conductive) and roughly 2/3rd of the cases have mild conductive hearing loss. Average hearing loss has been observed to be greater at lower frequencies than at higher frequencies.
Malleolar perforations reveal greater hearing loss a compared to non-malleolar ones (even if both are of identical size).
Hearing loss increases with the increase in the size of tympanic membrane perforation.
Site of perforation is also an important factor as posterior quadrant pars tensa perforations have greater hearing loss than anterior quadrant perforations.
Roughly 1/3rd cases of safe CSOM with dry TM perforation have normally functioning Eustachian tube and slightly less than 50% have only mild dysfunction as noted by Eustachian tube opening pressure.
It is concluded that a good correlation exists between the functional status of eustachian tube and success of myringoplasty operation. The success rates of myringoplasty in normal ET function (81.8%) an in mild ET hypofunction (72.7%) are significant as compared to failures in the presence of moderate and severe ET hypofunction, whatever may be the technique.
Contributor Information
Nishant Kumar, Phone: +09765544977, Email: drnishant5@yahoo.co.in.
Devashri Chilke, Phone: +09765544988, Email: drnishant5@yahoo.co.in.
M. P. Puttewar, Email: drmpputtewar@gmail.com
Bibliography
- 1.Ahmad SW, Ramani GV. Hearing loss in perforation of the tympanic membrane. J Laryngol Otol. 1979;93:1091–1098. doi: 10.1017/S0022215100088162. [DOI] [PubMed] [Google Scholar]
- 2.Alberti PWRM, Kristensen J. The clinical application of impedance audiometry. Laryngoscope. 1970;80:785. doi: 10.1288/00005537-197005000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Andereasson L, Harris S. Middle ear mechanics and eustachian tube function in tympanoplasty. Acta Otolaryngol. 1979;360:141–147. doi: 10.3109/00016487809123500. [DOI] [PubMed] [Google Scholar]
- 4.Arora MML, Mehra YN, Sharma VL. Mastoid pneumatisation in chronic suppurative otitis media and its clinical significance. J Laryngol Otol. 1978;62:295–398. doi: 10.1017/s0022215100085509. [DOI] [PubMed] [Google Scholar]
- 5.Austin DF. Sound conduction in the diseased ear. J Laryngol Otol. 1978;92:367–392. doi: 10.1017/S0022215100085492. [DOI] [PubMed] [Google Scholar]
- 6.Ballal M, et al. Chronic suppurative otitis media—a bacteriological and mycological study. Indian J Otolaryngol Head Neck. 1992;1:10–13. [Google Scholar]
- 7.Ballenger JJ (1977) Eustachian tube dysfunction. In: Disease of the nose, throat and ear. Lea & Febiger, Philadelphia
- 8.Baruah PC, Aggarwal SC, Arora MML, Mehra YN. Clinical and Microbiological studies in suppurative otitis media in Chandigarh 1965. Indian J Otolaryngol. 1972;24:11–60. [Google Scholar]
- 9.Beales PH. Chronic otitis media-assessment. In: Ballantyne JC, Groves J, editors. Scott Brown’s diseases of ear, nose and throat. London: Butterworths; 1979. pp. 240–241. [Google Scholar]
- 10.Bluestone CD, Cantekin EL, Douglas GS. Eustachian tube function related to the results of tympanoplasty in children. Laryngoscope. 1979;89:450. doi: 10.1288/00005537-197903000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Booth JB. Closure of perforation of tympanic membrane. In: Ballantyne J, editor. Rob and Smith’s operative surgery ear. London: Butterworths; 1976. [Google Scholar]
- 12.Census (1991) Provisional population total: rural urban distribution by Nanda AR, Ministry of Home Affairs, Series 1, Paper 2
- 13.Chandra R, Mishra RN. Some observations on the total and subtotal perforations of tympanic membrane. Indian J Otolaryngol. 1964;8:1–20. [Google Scholar]
- 14.Chaturvedi VN, Grewal BS, Cad MS. Bacterial flora in chronic suppurative otitis media Benghazi. Garyounis Med J. 1980;6(2):161. [Google Scholar]
- 15.Chhangani DL, Goyal OP. Bacteriological study, in chronic suppurative otitis media. Indian J Otolaryngol. 1976;28:41–48. [Google Scholar]
- 16.Cohn AM, Schwaber MK, Anthony LS, Jerger JF. Eustachian tube function and tympanoplasty. Ann Otol Rhinol Laryngol. 1979;88:339–447. doi: 10.1177/000348947908800308. [DOI] [PubMed] [Google Scholar]
- 17.Desai B, Hussain M, Malhotra BR. Chronic suppurative otitis media—a bacteriological study. Indian Pediatr. 1985;22:417. [PubMed] [Google Scholar]
- 18.Dutta NN, Kacker SK, Sinha A. Eustachian tube function in health and disease. Indian J Otolaryngol. 1971;23:169–176. [Google Scholar]
- 19.Ekvall L. Eustachian tube function in tympanoplasty. Acta Otolaryngologica. 1970;263:33–42. doi: 10.3109/00016487009131515. [DOI] [PubMed] [Google Scholar]
- 20.Eliachar Z. Audiologic Manifestations in otitis media. Otolaryngol Clin North Am. 1978;11:769–776. [PubMed] [Google Scholar]
- 21.Farmer JC. Eustachian tube function physiology and role in otitis media. Ann Otol Rhinol Laryngol. 1985;94(Suppl 120):1–6. [PubMed] [Google Scholar]
- 22.Fatma A, Assiry S, Siray ZM (1998) Microbiological evaluation and aspects on management of chronic suppurative otitis media in Riyadh. Indian J Otol 4(3):115–120
- 23.Frootko NJ. Reconstruction of the ear. In: Booth JB, Kerr AG, editors. Scott Brown’s Otolaryngology. 5. London: Butterworth; 1987. pp. 238–263. [Google Scholar]
- 24.Ghosh AK, Mehra YN. Eustachian tube in suppurative otitis media. Indian J Otolaryngol. 1975;27:141–145. [Google Scholar]
- 25.Goycoolea MV, Hueb M, Ruah C. Definations and terminology. Otolaryngol Clin North Am. 1991;24:20. [PubMed] [Google Scholar]
- 26.Gulati SK. Investigative profile in patients of chronic suppurative otitis media. Indian J Otol. 1997;3(2):59–62. [Google Scholar]
- 27.Holmquist J, Lindeman P. Eustachian tube function and hearing after myringoplasty. Otolaryngol Head Neck Surg. 1987;96:80–82. doi: 10.1177/019459988709600114. [DOI] [PubMed] [Google Scholar]
- 28.Kulkarni RD, Dharmadhikari CA, Kulkarni VA, Udgaonkar US, Pawar SG. Bacteriological study of chronic otitis media. Indian J Otolaryngol Head Neck Surg. 1993;2(2):110–112. [Google Scholar]
- 29.Logan Turner . Logan Turner diseases of the nose, throat and ear. London: John Wright and Son’s Ltd; 1988. [Google Scholar]
- 30.Mahajan BK. Methods in biostatistics. New Delhi: Jaypee Brothers; 1989. [Google Scholar]
- 31.Mann SBS, Grewal BS, Nanar MS, Mehra YN, Arora MML. Incidence of chronic suppurative otitis media in general population (a rural survey) Indian J Otolaryngol. 1986;28:5–40. [Google Scholar]
- 32.Mawson SR. Diseases of the ear. 4. London: Edward Annold; 1979. [Google Scholar]
- 33.Mishra RN, Bhatia NL, Bhatia BPR. Investigations of hearing in school children. Indian J Otolaryngol. 1961;13:107–127. [Google Scholar]
- 34.Mittal VK. Assessment of eustachian tube functions in patients with eardrum perforation. Indian J Otolaryngol. 1985;37:23–25. [Google Scholar]
- 35.Paperella MM, Shumrick DA. Otolaryngology. Philadelphia: W.B. Saunders Co; 1973. [Google Scholar]
- 36.Pickles JO. Physiology of the ear. In: Wright D, editor. Scott Brown’s Otolaryngology. 5. London: Butterworths; 1987. [Google Scholar]
- 37.Sen S, Guha S, Biswas A, Ghosh LM. A comparative study of methods of evaluating eustachian tube function in chronic suppurative otitis media. Indian J Otol. 1999;5(2):67–70. [Google Scholar]