Abstract
Background
Fast-track (FT) programmes represent a series of multimodal concepts that may reduce surgical stress and speed up convalescence after surgery. The aim of this systematic review was to evaluate FT programmes for patients undergoing hepatopancreatic surgery.
Methods
PubMed, Embase and the Cochrane Library databases were searched for studies of FT vs. conventional recovery strategies for liver and pancreatic resections.
Results
For liver surgery, three cohort studies were included. Primary hospital stay was significantly reduced after FT care in two of the three studies. There were no significant differences in rates of readmission, morbidity and mortality. For pancreatic surgery, three cohort studies and one case-control study were included. Primary hospital stay was significantly shorter after FT care in three out of the four studies. One study reported a significantly decreased readmission rate (7% vs. 25%; P = 0.027), and another study showed lower morbidity (47.2% vs. 58.7%; P < 0.01) in favour of the FT group. There was no difference in mortality between the FT and control groups.
Conclusions
FT rehabilitation for liver and pancreatic surgical patients is feasible. Future investigation should focus on optimizing individual elements of the FT programme within the context of liver and pancreatic surgery.
Keywords: liver, pancreas, resection, fast track, enhanced recovery, safety, effectiveness
Introduction
‘Enhanced recovery’ or ‘fast-track’ (FT) programmes are structured interdisciplinary strategies that have been introduced to optimize peri-operative care and accelerate post-operative recovery. The main aim of the FT protocol is to reduce the metabolic and inflammatory response to surgical stress and preserve vital functions.1 First developed by Kehlet et al,2–4 these protocols presently include key elements such as pre-operative counselling, the limited use of drains and nasogastric tubes, optimal pain relief, early nutrition and enhanced patient mobilization.5 Apart from elective colorectal surgery, FT programmes have been proposed in other surgical fields, such as gastro-oesophageal,6 musculoskeletal7 and aortic8 surgery. To date, however, the principles of enhanced recovery have rarely been applied to liver and pancreatic surgery.9,10
Hepatopancreatic resections represent major abdominal operations with high risks, carried out with increasing frequency, and most often for malignant conditions.11–13 Nonetheless, both morbidity and mortality associated with these procedures have decreased over the years.12,14 The aim of this systematic review was to assess the evidence for FT peri-operative care in patients undergoing hepatopancreatic resections.
Methods
Search strategy
Pubmed, Embase and the Cochrane Library databases were searched on 31 May 2011 by the first author, using the following search string for titles and abstracts: [(‘fast track’ OR ‘enhanced recovery’ OR ‘eras’ OR ‘early discharge’ OR ‘clinical pathways’ OR ‘clinical pathway’ OR ‘critical pathways’ OR ‘critical pathway’) AND (‘liver’ OR ‘hepatic’ OR ‘hepatectomy’ OR ‘pancreas’ OR ‘pancreatic’ OR ‘pancreatectomy’ OR ‘pancreaticoduodenectomy’ OR ‘whipple’)]. Titles and abstracts were reviewed and relevant papers identified. Reference lists of retrieved articles were used to complete the search.
Inclusion and exclusion criteria
Studies were included if they fulfilled all of the following criteria: (i) adult patients undergoing elective liver or pancreatic resection for benign or malignant disease, (ii) comparison of a FT multimodal strategy with conventional care, (iii) reporting at least four FT items and (iv) reporting at least one of the following outcome measures: length of stay, readmission, morbidity and mortality. Trials investigating transplantation were excluded. Only clinical studies published in English, German or French were included. No unpublished data or conference abstracts were included. If studies proved to have an overlap in patient population, only the largest publication was included. To date, there are 20 recognized protocol elements that make up the FT programme.5 In this review, a total of 18 FT items were scored, as two items, i.e. writing an audit (applicable to all included studies) and the use of suprapubic catheters for pelvic surgery, were considered not relevant.
Outcomes of interest
Primary outcome parameters were length of hospital stay, readmission rate, morbidity and mortality. Secondary outcomes included bowel function, cost-effectiveness and quality of life. The level of evidence was rated according to the Oxford Centre for Evidence-based Medicine Levels of Evidence.15
Results
A total of 518 publications were identified, of which 18 were relevant. Five studies16–19,21 lacked a traditional care group (control). Four studies20,22–24 were excluded because of failure to apply a minimum of four FT elements, and one trial25 did not describe details of the FT protocol. Furthermore, one study26 was excluded because part of the data had been used in another publication. Finally, seven trials comparing FT peri-operative care with traditional care were identified (Fig. 1).
Figure 1.
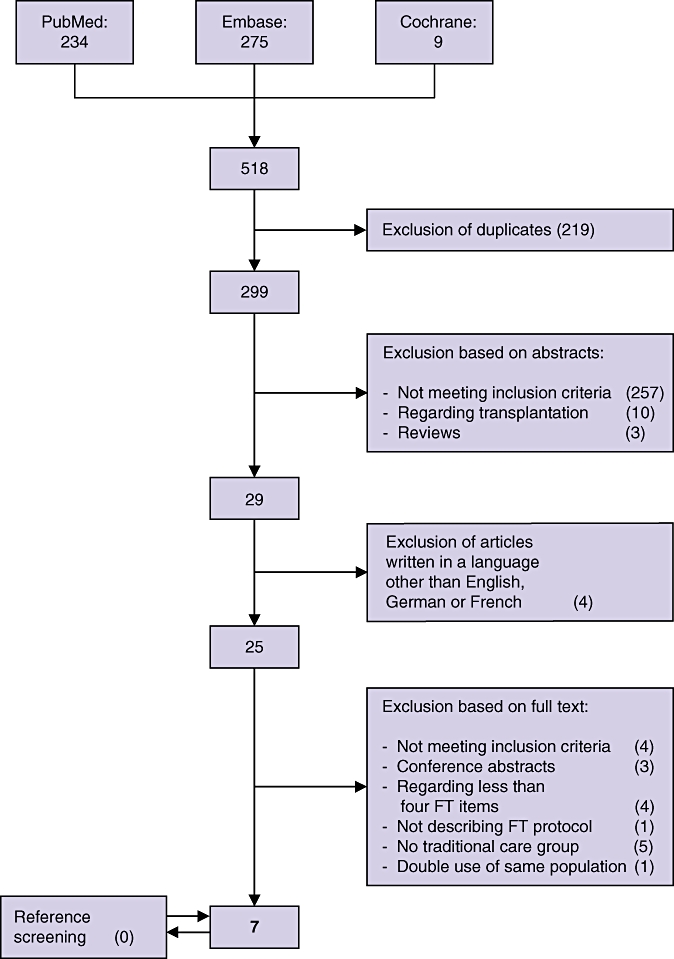
Search strategy
Three articles described outcomes for patients who underwent liver resection for primary or secondary tumours,10,27,28 whereas four studies described patients who underwent pancreatic surgery9,29–31 (Table 1). Included trials were published between 2006 and 2011. Median population size in the FT group was 61 (range 12–252) patients. All trials used a prospective intervention group and a retrospective control group. They had evidence level 2b or 3b on the Oxford Level of Evidence scale.
Table 1.
Characteristics of included studies
| Study (year) | Type of surgery | Population FT/C | Study type | LOS FT/C | Readmission FT/C | Morbidity FT/C | Mortality FT/C | E |
|---|---|---|---|---|---|---|---|---|
| van Dam et al. (2008)10 | Liver | 61/100 | CS | 6/8 (P < 0.001) median | 13%/10% (P = 0.543) | 41%/31% (P = 0.197) | 0%/2% (P = 0.526) | 2B |
| OL | ||||||||
| Stoot et al. (2009)28 | Liver | 13/13 | CS | 5/7 (P = 0.305) median | 0%/0% | 15%/15% (P = 1.0) | 0%/0% | 2B |
| LL | ||||||||
| Lin et al. (2011)27 | Liver | 56/61 | CS | 7/11 (P < 0.01) median | 7.1%/3.3% (P = 0.424) | 46.4/44.3 (P = 0.814) | 1.8/1.6 (P = 0.706) | 2B |
| OL | ||||||||
| Wichmann et al. (2006)31 | Pancreas | 12/12 | CCS | 12.9/20 (NS) mean | – | 8.3%/8.3% | – | 3B |
| PR | ||||||||
| Kennedy et al. (2007)30 | Pancreas | 91/44 | CS | 7/13 (P < 0.0001) median | 7.7%/7.0% (NS) | 37%/44% (NS) | 1.1%/2.3% (NS) | 2B |
| PD | ||||||||
| Balzano et al. (2008)9 | Pancreas | 252/252 | CS | 13/15 (P < 0.001) median | 7.1%/6.3% (P = 0.865) | 47.2%/58.7% (P < 0.01) | 3.6 % vs. 2.8% (P = 0.798) | 2B |
| PD | ||||||||
| Kennedy et al. (2009)29 | Pancreas | 71/40 | CS | 6.7/10.2 (P < 0.037) mean | 7%/25% (P < 0.027) | 15.7%/37.5% (NS) | 1.1%/2.3% (NS) | 2B |
| DP | ||||||||
OL, open liver resection; LL, laparoscopic liver resection; PD, pancreaticoduodenectomy; DP, distal pancreatectomy; PR, any pancreatic resection; FT, fast-track; C, control; CS, cohort study; CCS, case-control study; LOS, length of hospital stay in days; E, level of evidence; NS, not significant; –, not described.
Fast-track items
There was some clinical heterogeneity regarding specific FT interventions used in the studies. The number of included FT items ranged from 5 to 18 with a median of 7. Post-operative nutritional care and early mobilization were the commonest FT interventions, whereas laparoscopic surgery and minimal incisions were reported infrequently (Table 2).
Table 2.
Number of fast-track items used in included studies
| van Dam et al. (2008)10 | Stoot et al. (2009)28 | Lin et al. (2011)27 | Wichmann et al. (2006)31 | Kennedy et al (2007)30 | Balzano et al. (2008)9 | Kennedy et al. (2009)29 | |
|---|---|---|---|---|---|---|---|
| Preadmission counselling | + | + | + | + | + | + | |
| No bowel preparation | + | + | + | + | |||
| Pre-operative fasting and pre-operative carbohydrate loading | + | + | + | + | |||
| No pre-anaesthetic medication | + | + | + | ||||
| Thromboembolic prophylaxis | + | + | + | + | + | + | |
| Prophylactic antibiotics | + | + | + | + | + | + | |
| Epidural analgesia | + | + | + | + | + | ||
| Prevention of post-operative nausea and vomiting | + | + | + | ||||
| Laparoscopic surgery | + | ||||||
| Minimal incisions | + | ||||||
| No standard nasogastric tubes post-operatively | + | + | + | ||||
| Prevention of intra-operative hypothermia | + | + | + | ||||
| Fluid restriction | + | + | + | + | + | ||
| No surgical drains | + | + | + | ||||
| Prevention of post-operative ileus | + | + | |||||
| No systemic opioids | + | + | + | ||||
| Post-operative nutritional care | + | + | + | + | + | + | + |
| Early mobilization | + | + | + | + | + | + | + |
Liver resection
Primary outcome measures were reported in all studies. Primary hospital stay was significantly reduced after FT care in two out of the three studies.10,27 In one study, median hospital stay was 6 days in the FT group compared with 8 days in the control group (P < 0.001).10 In the other study, primary hospital stay was reduced from 11 days to 7 days (P < 0.01).27 There were no significant differences in rates of readmission, morbidity and mortality between FT and control groups (Table 1).
Gastrointestinal function was reported in two studies.10,28 One trial found a significantly shorter time to successful resumption of a normal diet in the FT group (1 post-operative day for FT patients vs. 3 days for the control group).10 In the only study that reported on cost-effectiveness data, the mean charges per hospital stay were Renminbi (RMB) 26 626 for the control group and RMB 21 004 for the FT group (P < 0.05).27
Pancreatic resection
All four studies reported on primary hospital stay and this was significantly shorter after FT care in three out of the four studies.9,29,30 Readmission rates were reported in three studies. In one study, the readmission rate was reduced in favour of the FT patients (7% vs. 25%; P = 0.027).29 However, the effect on readmission must be interpreted with caution. The control group was operated before the recruitment of a team focused on pancreatic surgery. The team was encouraged to increase the case load but were not given additional bed days. Furthermore, the surgical volume increased from an average of 1.2 cases per month pre-FT to 3.2 cases per month post-FT, as a result of, e.g. tertiary referrals. Morbidity rates were reported in all studies. In one study, management within an FT pathway led to significantly fewer post-operative complications (47.2% vs. 58.7%; P < 0.01).9 Mortality was reported in three of the studies and was not significantly different between the FT and control groups (Table 1).
Two studies assessed gastrointestinal function.9,31 In one study, the FT group had earlier oral intake and first bowel movement post-operatively as compared with the control group.31 In the other study, patients undergoing a pancreaticoduodenectomy and managed with a FT pathway had a reduced incidence of delayed gastric emptying (13.9% vs. 24.6%; P = 0.004).9 The cost-effectiveness of FT protocols was reported in two trials.29,30 In one study, the mean total hospital charges were significantly decreased for FT patients, from $240 242 ± $32 490 to $126 566 ± 4883 (P≤ 0.0001).30
Discussion
The principles of enhanced recovery have been proven to be safe and effective in several surgical settings.7,8,32 This systematic review examined the evidence for FT protocols when compared with standard care in elective liver and pancreatic surgery using data from cohort and case-control studies as there are no randomized control trials (RCTs) in this area. The results suggest that FT programmes can enhance post-operative recovery and reduce the length of hospital stay with no increase in adverse events, such as readmissions, morbidity and mortality.
The length of hospital stay after hepatopancreatic surgery is typically a minimum of 1 week. In liver surgery, the median length of stay with traditional care pathways ranges from 7 to 11 days.12,33 For pancreatic resections, the hospital stay is between 9 and 15 days.11,13,34 Of the seven studies identified, all reported a shorter hospital stay in FT patients. This difference was statistically significant in five of the studies,9,10,27,29,30 but failed to reach statistical significance in two studies,28,31 perhaps as a result of limited study populations. The use of hospital stay as a marker for FT programme success may be inappropriate, as it has been shown that functional recovery of patients undergoing FT colonic35 and liver28 surgery is attained days before patient discharge.
As none of the studies reported a difference in mortality and the only significant difference in morbidity that was detected actually favoured FT surgery,10 one could at least argue that safety seemingly is not impaired when using an enhanced recovery programme.
Nevertheless, a suggested disadvantage of FT surgery has been a possibly higher readmission rate. Although there have been some reports on FT programmes for colorectal surgery with increased readmission rates noted,36–39 the total number of days in hospital, when also including the added stay for readmissions, remained lower when applying FT surgery.36–39 Furthermore, the available studies on hepatopancreatic surgery have not reported an increased readmission rate after FT recovery.9,10,27–31 It is also important to consider that these protocols aim at an earlier recovery, ideally applying a check list for discharge criteria, and thus supposedly initiate patient discharge after adequate recovery and not simply earlier than is done with ‘traditional’ care.
In addition to abovementioned primary outcomes, there were also some promising results found in terms of secondary outcomes. Four studies analysed the recovery of gastrointestinal function,9,10,28,31 three of them detecting a difference, and all in favour of FT surgery.9,10,31 In terms of cost-effectiveness, three studies reported an improvement with enhanced recovery programmes,27,29,30 although not significant in one study29. These are additional data supporting the use of FT surgery.
None of the selected articles reported measurements of quality of life. In colorectal surgery, no difference in quality of life after surgery has been shown when comparing patients with FT and conventional care.40,41 However, during the first weeks after surgery, the quality of life deteriorates after colorectal,41 as well as after liver surgery.42 It can be argued that a FT protocol also should include measures to be carried out even when the patient has left the hospital.43
The structure of this review meant that one important study of FT peri-operative care had to be excluded because it did not compare outcome data with traditional care. The previous study by Hendry et al.18 is an RCT in liver resection that addressed the role of oral nutritional supplements (ONS) and magnesium hydroxide alone and in various combinations within a multimodal FT programme. It included the full FT protocol, but focused on the individual roles of magnesium oxide and ONS. This previous study demonstrates the success of individual protocol elements.
This systematic review has its limits because of the low number of eligible studies, most with small sample sizes. There were no RCTs among the seven studies evaluated and all used a historical control group. Patient care, other than the treatment being investigated, may have changed over time and thus potentially affects the final results. There was large heterogeneity regarding outcome measures, number of FT items and discharge criteria.
However, based on the reviewed evidence, FT programmes for hepatopancreatic resections appear to be safe and associated with a reduction in length of hospital stay. Drawing from previous experience of FT implementation in colorectal surgery, further investigation of FT vs. traditional care in hepatopancreatic surgery is probably unnecessary. Future investigation should focus on optimizing individual elements of the FT programme within the context of liver and pancreatic surgery, and identifying any procedure-specific modifications that may be needed.
Conflicts of interest
None declared.
References
- 1.Varadhan KK, Lobo DN, Ljungqvist O. Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin. 2010;26:527–547. doi: 10.1016/j.ccc.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Basse L, Hjort Jakobsen D, Billesbolle P, Werner M, Kehlet H. A clinical pathway to accelerate recovery after colonic resection. Ann Surg. 2000;232:51–57. doi: 10.1097/00000658-200007000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–617. doi: 10.1093/bja/78.5.606. [DOI] [PubMed] [Google Scholar]
- 4.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–641. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 5.Lassen K, Soop M, Nygren J, Cox PB, Hendry PO, Spies C, et al. Consensus review of optimal perioperative care in colorectal surgery: enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144:961–969. doi: 10.1001/archsurg.2009.170. [DOI] [PubMed] [Google Scholar]
- 6.Cerfolio RJ, Bryant AS, Bass CS, Alexander JR, Bartolucci AA. Fast tracking after Ivor Lewis esophagogastrectomy. Chest. 2004;126:1187–1194. doi: 10.1378/chest.126.4.1187. [DOI] [PubMed] [Google Scholar]
- 7.Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S, et al. Effects of clinical pathways in the joint replacement: a meta-analysis. BMC Med. 2009;7:32. doi: 10.1186/1741-7015-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muehling BM, Halter G, Lang G, Schelzig H, Steffen P, Wagner F, et al. Prospective randomized controlled trial to evaluate ‘fast-track’ elective open infrarenal aneurysm repair. Langenbecks Arch Surg. 2008;393:281–287. doi: 10.1007/s00423-008-0284-8. [DOI] [PubMed] [Google Scholar]
- 9.Balzano G, Zerbi A, Braga M, Rocchetti S, Beneduce AA, Di Carlo V. Fast-track recovery programme after pancreatico- duodenectomy reduces delayed gastric emptying. Br J Surg. 2008;95:1387–1393. doi: 10.1002/bjs.6324. [DOI] [PubMed] [Google Scholar]
- 10.van Dam RM, Hendry PO, Coolsen MM, Bemelmans MH, Lassen K, Revhaug A, et al. Initial experience with a multimodal enhanced recovery programme in patients undergoing liver resection. Br J Surg. 2008;95:969–975. doi: 10.1002/bjs.6227. [DOI] [PubMed] [Google Scholar]
- 11.Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006;244:10–15. doi: 10.1097/01.sla.0000217673.04165.ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–406. doi: 10.1097/01.SLA.0000029003.66466.B3. discussion 406–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, et al. Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg. 2004;139:718–725. doi: 10.1001/archsurg.139.7.718. discussion 725–717. [DOI] [PubMed] [Google Scholar]
- 14.Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000;232:786–795. doi: 10.1097/00000658-200012000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oxford Centre for Evidence-based Medicine Levels of Evidence. [WWW document] 2009. URL http://www.cebm.net[accessed on 25 January 2011]
- 16.Berberat PO, Ingold H, Gulbinas A, Kleeff J, Muller MW, Gutt C, et al. Fast track–different implications in pancreatic surgery. J Gastrointest Surg. 2007;11:880–887. doi: 10.1007/s11605-007-0167-2. [DOI] [PubMed] [Google Scholar]
- 17.di Sebastiano P, Festa L, De Bonis A, Ciuffreda A, Valvano MR, Andriulli A, et al. A modified fast-track program for pancreatic surgery: a prospective single-center experience. Langenbecks Arch Surg. 2011;396:345–351. doi: 10.1007/s00423-010-0707-1. [DOI] [PubMed] [Google Scholar]
- 18.Hendry PO, van Dam RM, Bukkems SF, McKeown DW, Parks RW, Preston T, et al. Randomized clinical trial of laxatives and oral nutritional supplements within an enhanced recovery after surgery protocol following liver resection. Br J Surg. 2010;97:1198–1206. doi: 10.1002/bjs.7120. [DOI] [PubMed] [Google Scholar]
- 19.MacKay G, O'Dwyer PJ. Early discharge following liver resection for colorectal metastases. Scott Med J. 2008;53:22–24. doi: 10.1258/rsmsmj.53.2.22. [DOI] [PubMed] [Google Scholar]
- 20.French JJ, Mansfield SD, Jaques K, Jaques BC, Manas DM, Charnley RM. Fast-track management of patients undergoing proximal pancreatic resection. Ann R Coll Surg Engl. 2009;91:201–204. doi: 10.1308/003588409X391893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koea JB, Young Y, Gunn K. Fast track liver resection: the effect of a comprehensive care package and analgesia with single dose intrathecal morphine with gabapentin or continuous epidural analgesia. HPB Surg. 2009;2009:271986. doi: 10.1155/2009/271986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pratt WB, Steinbrook RA, Maithel SK, Vanounou T, Callery MP, Vollmer CM., Jr Epidural analgesia for pancreatoduodenectomy: a critical appraisal. J Gastrointest Surg. 2008;12:1207–1220. doi: 10.1007/s11605-008-0467-1. [DOI] [PubMed] [Google Scholar]
- 23.Pratt WB, Vollmer CM, Callery MP. Outcomes in pancreatic resection are negatively influenced by pre-operative hospitalization. HPB (Oxford) 2009;11:57–65. doi: 10.1111/j.1477-2574.2008.00012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanounou T, Pratt W, Fischer JE, Vollmer CM, Jr, Callery MP. Deviation-based cost modeling: a novel model to evaluate the clinical and economic impact of clinical pathways. J Am Coll Surg. 2007;204:570–579. doi: 10.1016/j.jamcollsurg.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 25.Porter GA, Pisters PW, Mansyur C, Bisanz A, Reyna K, Stanford P, et al. Cost and utilization impact of a clinical pathway for patients undergoing pancreaticoduodenectomy. Ann Surg Oncol. 2000;7:484–489. doi: 10.1007/s10434-000-0484-0. [DOI] [PubMed] [Google Scholar]
- 26.Bruns C, Wichmann MW, Kreis ME, Jauch K. Fast track pancreatic cancer surgery. Chir Prax. 2007;67:203–210. [Google Scholar]
- 27.Lin DX, Li X, Ye QW, Lin F, Li LL, Zhang QY. Implementation of a fast-track clinical pathway decreases postoperative length of stay and hospital charges for liver resection. Cell Biochem Biophys. 2011 doi: 10.1007/s12013-011-9203-7. DOI: 10.1111/j.1582-4934.2011.01301.x [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stoot JH, van Dam RM, Busch OR, van Hillegersberg R, De Boer M, Olde Damink SW, et al. The effect of a multimodal fast-track programme on outcomes in laparoscopic liver surgery: a multicentre pilot study. HPB (Oxford) 2009;11:140–144. doi: 10.1111/j.1477-2574.2009.00025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kennedy EP, Grenda TR, Sauter PK, Rosato EL, Chojnacki KA, Rosato FE, et al. Implementation of a critical pathway for distal pancreatectomy at an academic institution. J Gastrointest Surg. 2009;13:938–944. doi: 10.1007/s11605-009-0803-0. [DOI] [PubMed] [Google Scholar]
- 30.Kennedy EP, Rosato EL, Sauter PK, Rosenberg LM, Doria C, Marino IR, et al. Initiation of a critical pathway for pancreaticoduodenectomy at an academic institution–the first step in multidisciplinary team building. J Am Coll Surg. 2007;204:917–923. doi: 10.1016/j.jamcollsurg.2007.01.057. discussion 923–914. [DOI] [PubMed] [Google Scholar]
- 31.Wichmann MW, Roth M, Jauch KW, Bruns CJ. A prospective clinical feasibility study for multimodal ‘fast track’ rehabilitation in elective pancreatic cancer surgery. Rozhl Chir. 2006;85:169–175. [PubMed] [Google Scholar]
- 32.Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, Ubbink DT, et al. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006;93:800–809. doi: 10.1002/bjs.5384. [DOI] [PubMed] [Google Scholar]
- 33.Dimick JB, Wainess RM, Cowan JA, Upchurch GR, Jr, Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. J Am Coll Surg. 2004;199:31–38. doi: 10.1016/j.jamcollsurg.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Brooks AD, Marcus SG, Gradek C, Newman E, Shamamian P, Gouge TH, et al. Decreasing length of stay after pancreatoduodenectomy. Arch Surg. 2000;135:823–830. doi: 10.1001/archsurg.135.7.823. [DOI] [PubMed] [Google Scholar]
- 35.Maessen JM, Dejong CH, Kessels AG, von Meyenfeldt MF. Length of stay: an inappropriate readout of the success of enhanced recovery programs. World J Surg. 2008;32:971–975. doi: 10.1007/s00268-007-9404-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jakobsen DH, Sonne E, Andreasen J, Kehlet H. Convalescence after colonic surgery with fast-track vs conventional care. Colorectal Dis. 2006;8:683–687. doi: 10.1111/j.1463-1318.2006.00995.x. [DOI] [PubMed] [Google Scholar]
- 37.Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA. A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg. 2007;245:867–872. doi: 10.1097/01.sla.0000259219.08209.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nygren J, Hausel J, Kehlet H, Revhaug A, Lassen K, Dejong C, et al. A comparison in five European Centres of case mix, clinical management and outcomes following either conventional or fast-track perioperative care in colorectal surgery. Clin Nutr. 2005;24:455–461. doi: 10.1016/j.clnu.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 39.Stephen AE, Berger DL. Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery. 2003;133:277–282. doi: 10.1067/msy.2003.19. [DOI] [PubMed] [Google Scholar]
- 40.Delaney CP, Zutshi M, Senagore AJ, Remzi FH, Hammel J, Fazio VW. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. 2003;46:851–859. doi: 10.1007/s10350-004-6672-4. [DOI] [PubMed] [Google Scholar]
- 41.King PM, Blazeby JM, Ewings P, Longman RJ, Kipling RM, Franks PJ, et al. The influence of an enhanced recovery programme on clinical outcomes, costs and quality of life after surgery for colorectal cancer. Colorectal Dis. 2006;8:506–513. doi: 10.1111/j.1463-1318.2006.00963.x. [DOI] [PubMed] [Google Scholar]
- 42.Wiering B, Oyen WJ, Adang EM, van der Sijp JR, Roumen RM, de Jong KP, et al. Long-term global quality of life in patients treated for colorectal liver metastases. Br J Surg. 2011;98:565–571. doi: 10.1002/bjs.7365. [DOI] [PubMed] [Google Scholar]
- 43.Wennstrom B, Stomberg MW, Modin M, Skullman S. Patient symptoms after colonic surgery in the era of enhanced recovery–a long-term follow-up. J Clin Nurs. 2010;19:666–672. doi: 10.1111/j.1365-2702.2009.03099.x. [DOI] [PubMed] [Google Scholar]


