Abstract
AIM
To develop a dosing equation for tacrolimus, using genetic and clinical factors from a large cohort of kidney transplant recipients. Clinical factors and six genetic variants were screened for importance towards tacrolimus clearance (CL/F).
METHODS
Clinical data, tacrolimus troughs and corresponding doses were collected from 681 kidney transplant recipients in a multicentre observational study in the USA and Canada for the first 6 months post transplant. The patients were genotyped for 2 724 single nucleotide polymorphisms using a customized Affymetrix SNP chip. Clinical factors and the most important SNPs (rs776746, rs12114000, rs3734354, rs4926, rs3135506 and rs2608555) were analysed for their influence on tacrolimus CL/F.
RESULTS
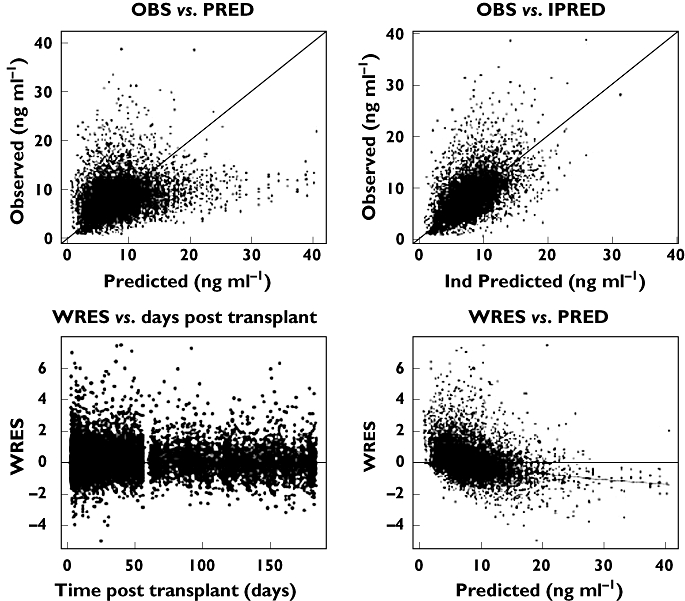
The CYP3A5*1 genotype, days post transplant, age, transplant at a steroid sparing centre and calcium channel blocker (CCB) use significantly influenced tacrolimus CL/F. The final model describing CL/F (l h−1) was: 38.4 ×[(0.86, if days 6–10) or (0.71, if days 11–180)]×[(1.69, if CYP3A5*1/*3 genotype) or (2.00, if CYP3A5*1/*1 genotype)]× (0.70, if receiving a transplant at a steroid sparing centre) × ([age in years/50]−0.4) × (0.94, if CCB is present). The dose to achieve the desired trough is then prospectively determined using the individuals CL/F estimate.
CONCLUSIONS
The CYP3A5*1 genotype and four clinical factors were important for tacrolimus CL/F. An individualized dose is easily determined from the predicted CL/F. This study is important towards individualization of dosing in the clinical setting and may increase the number of patients achieving the target concentration. This equation requires validation in an independent cohort of kidney transplant recipients.
Keywords: CYP3A5, kidney transplantation, pharmacogenetics, pharmacogenomics, pharmacokinetics, tacrolimus
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Patients with low tacrolimus troughs are at a higher risk of rejection while those with high troughs are at an increased risk for toxicity. Therefore, achieving the therapeutic range is important.
CYP3A5 genotype and days post transplant have been previously shown individually to be associated with tacrolimus troughs.
WHAT THIS STUDY ADDS
This paper presents the first dosing model for tacrolimus using a combination of genetic and clinical factors in adult kidney transplant recipients. It was developed from one of the largest tacrolimus pharmacogenetic studies conducted to date (681 subjects and 11 823 trough concentrations).
We found that CL/F was significantly influenced by days post transplant, CYP3A5 genotype, transplantation at a steroid sparing centre, recipient age and the use of a calcium channel blocker.
Our large sample size enabled us to define the distinct differences in tacrolimus CL/F between three CYP3A5 genotype groups (*1/*1, *1/*3 and *3/*3).
This study is an important step towards using pharmacogenetic information in the clinical setting.
Introduction
Tacrolimus is the most widely used calcineurin inhibitor in kidney transplantation [1]. It has a narrow therapeutic window with wide inter-individual variability in pharmacokinetics and clearance (CL) [2, 3]. Higher troughs are associated with increased risk of toxicity whereas lower troughs are associated with increased risk of rejection [4]. Two recent studies showed that with contemporary immunosuppressive regimens (tacrolimus, mycophenolate and steroids ± antibody induction) low tacrolimus troughs in the first week post transplant were associated with a greater risk of acute rejection [5, 6]. To tailor therapy better, multiple clinical factors have been explored to determine their effects on tacrolimus pharmacokinetics. It is generally acknowledged that drug interactions, haematocrit, corticosteroid therapy, days post transplant, and race affect tacrolimus pharmacokinetics [3, 7–10]. It is also established that the cytochrome P4503A5 (CYP3A5)*1 allele is associated with significantly higher tacrolimus CL and lower systemic exposure [11–15]. However, because tacrolimus troughs are routinely monitored and dose adjusted based on trough measurements the effect of these factors are not regarded in a consistent manner by centres and a trial and error approach to dosing is still common practice. These factors have not been used to guide dosing primarily due to the lack of robust, clinically feasible dosing models that combine important factors. Because of the growing use of steroid sparing or avoidance protocols, the importance of early immunosuppression intensity provided by the calcineurin inhibitors and/or other immunosuppressive exposure is considered important in minimizing acute rejection [16].
A recent randomized trial studied CYP3A5 genotype guided tacrolimus dosing in kidney transplant recipients [17]. In the genotype guided group, patients with one or more CYP3A5*1 alleles received an initial tacrolimus dose of 0.3 mg kg−1 day−1 and those without a *1 allele received a dose of 0.15 mg kg−1 day−1. The non-genotype guided group was administered 0.2 mg kg−1 day−1. In the genotype guided group, 43.2% of subjects achieved the trough target compared with 29.1% in non-genotype guided group (P = 0.03). Although using genotype guided dosing was significantly better, the overall proportion of patients achieving the therapeutic range may not be sufficient to justify the cost of incorporating genotyping into clinical practice. It is possible that addition of clinical factors and/or other genotypes to dosing models may further improve the initial dose estimates and the number of patients achieving the therapeutic target. However, defining these factors and the development of a robust dosing model for clinical use requires a large study population. Therefore, we studied the effect of clinical and genetic factors on tacrolimus apparent clearance (CL/F) in a large kidney transplant population through a multicentre study. Our objective was to define the important clinical and genetic factors pertinent towards tacrolimus CL/F and develop a dosing model which would be suitable for the clinical setting.
Methods
Subjects for this analysis were obtained from the first 1000 patients with end-stage renal dysfunction undergoing kidney or kidney–pancreas transplant enrolled in the Deterioration of Kidney Allograft Function (DeKAF) Genomics study between 2006 and 2008. This was a multicentre observational trial to define genetic and clinical determinants associated with clinical outcomes after kidney transplant. Details of the trial have been published elsewhere and are registered at http://www.clinicaltrials.gov (NCT00270712). A total of 681 patients, ≥18 years of age, who received tacrolimus at any time in the first 6 months post transplant were selected for this analysis. The remaining subjects received ciclosporin and were not studied. Institutional Review Board Human Subjects Committee approval was obtained at each participating centre. All recipients provided written informed consent.
Tacrolimus trough concentrations (n = 11 823) in 681 patients were obtained during oral administration in the first 6 months post transplant. All patients were administered tacrolimus (Prograf) either once or twice daily. Troughs were obtained as part of clinical care at the treating centre. The initial tacrolimus dosing was based on an individual's body weight and subsequent doses were adjusted based on trough concentrations using institution-specific targets. In general, troughs of 8–12 ng ml−1 were targeted in the first 3 months post transplant and of 6–10 ng ml−1 were desired in the months 3–6 post transplant. Trough concentrations, if available, were obtained twice in each of weeks 1–8 post transplant and twice in each of months 3, 4, 5 and 6 post transplant. There were a mean of 17 trough concentrations per patient (range 1–24). To ensure that tacrolimus was at or near steady-state, only trough concentrations measured after day 2 post transplant were used in this analysis. Trough concentrations were measured in the clinical laboratories of the participating centres. The majority (97.1%) of tacrolimus whole blood concentrations were obtained from centres using liquid chromatography-mass spectroscopy to measure trough concentrations. All troughs were measured in centres using CLIA certified assays or CLIA quality assays.
Recipient and donor demographics and clinical characteristics were obtained from medical records and are listed in Table 1. Baseline clinical factors collected were recipient age, weight, gender and race (African American (AA) or non-AA), donor type (living or deceased), donor gender, pre-emptive transplant, number of prior transplants, immunosuppressive regimen and enrolling centre. The concomitant use of a calcium channel blocker (CCB) and days post transplant at the time of each trough measurement was also obtained.
Table 1.
Characteristics in all subjects, non-African Americans (AA) and AA
| Clinical characteristics | All subjects (Non-AA and AA) | Non-AA | AA |
|---|---|---|---|
| Number of subjects | 681 | 540 (79.3%) | 141 (20.7%) |
| Age (years) of recipient* | 50.2 ± 12.2 | 50.1 ± 12.2 | 46.9 ± 11.5 |
| Baseline weight (kg) of recipient* | 81.3 ± 18.7 | 81.1 ± 18.8 | 81.9 ± 17.9 |
| Gender of recipient (Male/Female) | 429 (63%)/252 (37%) | 338 (63%)/202 (37%) | 91 (65%)/50 (35%) |
| Number of transplants | |||
| 1 | 550 (81%) | 417 (77%) | 133 (94%) |
| ≥2 | 130 (19%) | 122 (23%) | 8 (6%) |
| Number transplanted at a steroid sparing centre | 205 (30%) | 197 (36.5%) | 8 (5.5%) |
| Living donor | 398 (59%) | 355 (66%) | 43 (31%) |
| Number of troughs | 11 823 | 9523 | 2300 |
| Mean tacrolimus daily dose in mg kg−1† | 0.08 ± 0.05 | 0.07 ± 0.05 | 0.09 ± 0.04 |
| Mean tacrolimus trough in ng ml−1† | 8.31 ± 3.48 | 8.66 ± 3.37 | 6.82 ± 3.51 |
| Number of patients with troughs <8 ng ml−1 | |||
| Week 1 | 413 (75%) | 307 (69%) | 106 (96%) |
| Week 2 | 331 (55%) | 228 (48%) | 103 (82%) |
| Calcium channel blocker use‡ | 5082 (43%) | 3915 (41%) | 1167 (51%) |
| CYP3A5 genotype | |||
| *1/*1 | 72 (11%) | 9 (2%) | 63 (45%) |
| *1/*3 | 129 (19%) | 70 (13%) | 59 (42%) |
| *3/*3 | 476 (70%) | 457 (85%) | 19 (13%) |
Reported age and baseline weight are those measured at the time of transplant and are mean ± SD
doses and troughs are over the 6-month study period and are mean ± SD
calcium channel blocker use at the time of trough collection.
Genotyping and selection of variants for analysis
Recipient pre-transplant DNA was obtained from the lymphocytes isolated from peripheral blood. DNA was genotyped for 2724 variants primarily using a customized Affymetrix GeneChip (Affymetrix, Santa Clara, CA, USA) [18, 19]. Additional variants were genotyped using the SNPlex (Applied Biosystems, Foster City, CA, USA) and Sequenom (Sequenom, San Diego, CA, USA) systems. In a prior analysis, these variants were evaluated for their association with dose-normalized tacrolimus concentrations using standard regression analysis [20]. As it was not feasible to evaluate 2724 variants and their combinations in a population pharmacokinetic approach to estimate CL/F, the SNPs with a P value < 0.01 from the AA and non-AA populations from the regression analysis, were selected for this analysis. The variants evaluated towards tacrolimus were rs776746, rs12114000, rs3734354, rs4926, rs3135506 and rs2608555. The variants and their allele frequencies are given in Table 2.
Table 2.
Analysed variants and their allele frequencies in all subjects, non-African Americans (AA) and AA
| Reference sequence (rs) number | Gene name | Allele | Overall allele frequency* (%) | Non-AA allele frequency† (%) | AA allele frequency‡ (%) |
|---|---|---|---|---|---|
| rs776746 | CYP3A5 | A | 20.16 | 8.21 | 65.60 |
| rs12114000 | CYP3A4 | A | 3.82 | 0.09 | 18.09 |
| rs3734354 | SIM1 | A | 11.40 | 13.45 | 3.55 |
| rs4926 | SERPING1 | A | 23.45 | 26.63 | 11.35 |
| rs3135506 | APOA5 | C | 6.12 | 6.33 | 5.32 |
| rs2608555 | GAN | T | 16.45 | 15.93 | 18.44 |
Allele frequency in the whole population
allele frequency in the non-African American
allele frequency in the African America.
Population modelling of troughs
The data were analysed by a non-linear mixed-effects approach using the NONMEM software (Version 7.1, NONMEM Project Group, GloboMax LLC, MD, USA) with a Visual Fortran compiler (Professional Edition for Windows 11.1, Intel®) and PdxPop (Version 4.0, ICON Development Solutions). R 2.4.1 was used for the generation of diagnostic plots. Given the long half-life of tacrolimus (12 h) [21, 22] relative to the dosing intervals, and the absence of pharmacokinetic sampling at times other than the troughs, the concentrations were analysed according to a steady-state infusion model. It was assumed that the trough concentrations (Cmin) were well approximated by the average steady-state plasma concentration (Css,av) of tacrolimus due to its long elimination half-life and were related to the tacrolimus dose through (CL/F)*:
where Cobs is the observed tacrolimus trough concentration and dosing rate is the total daily dose of tacrolimus (in mg) divided by 24 h. The (CL/F)* is a regression parameter that predicts the trough concentrations. It approximates CL/F when Cmin ≈ Css,av, as in the case of drugs that have a long half-life such as tacrolimus. Using (CL/F)* as an approximation to CL/F has the advantage of giving the regression parameter clinically relevant meaning in terms of magnitude, units and interpretation. However, we caution the reader that the apparent clearance we describe in the manuscript is only an approximation of the actual apparent tacrolimus clearance.
The first order conditional approximation estimation with interaction (FOCE-I) was utilized. The pharmacokinetic parameter obtained was the CL/F for tacrolimus. The inter-individual variability (IIV) in CL/F was modeled using an exponential error model as shown in the following equation:
where TVCL represents the typical value of CL/F in the population and η(1) represents the IIV in tacrolimus CL/F, η∼N (0, ω2). An additive error model was utilized to characterize the residual unexplained variability (RUV) as shown in the following equation:
where Cij is the jth observed concentration in the ith individual, Cpred,ij is the jth predicted concentration in the ith individual and εij is the RUV in tacrolimus CL/F, ε∼N (0, σ2).
The clinical factors and the six variants described in Tables 1 and 2 were tested for their influence on tacrolimus CL/F in the model building phase. Forward inclusion and backward elimination were used to analyse the covariates. A decrease in objective function value (OFV, a goodness-of-fit statistic) of 6.63 or more (P < 0.01) was considered significant (χ2: 1 degree of freedom, d.f.) in the forward inclusion step. Backward elimination was performed using a more stringent increase in OFV of 10.83 or more (P < 0.001, 1 d.f.). Clinical factors that were tested included categorical covariates (days post transplant of trough, recipient gender, race, donor type, donor gender, pre-emptive transplant, number of prior transplants and enrolling centre) and continuous covariates (age and weight). Race (Caucasian, AA, Asian, Native American/Aleut/Inuit and Hawaiian/Pacific Islander) was categorized as AA or non-AA. Centres were designated as using a steroid sparing immunosuppressive regimen if they administered steroids for ≤7 days post transplant. Age was tested by standardizing it by the median age (50 years) in the population. Days post transplant were converted to an ordered categorical covariate and classified as: immediate post transplant (days 3–5), early post transplant (days 6–10) and late post transplant (days 11–180). Categorization was done as the model failed to converge when days post transplant was modelled as a continuous function (such as a simple continuous function, Bateman function, Emax model, etc.). The concomitant use of a CCB at the time of the trough measurement was also analysed. Variants were initially classified as homozygous for the major allele, heterozygous for the minor allele or homozygous for the minor allele. However, the frequency of homozygous variant carriers in five of the six variants was ≤5%. Therefore, for these five variants, the genotypes were categorized as two variables (carriers or non-carriers of the minor allele). The minor allele frequency (MAF) of CYP3A5*1 was high and, therefore, we were able to categorize the genotypes as CYP3A5*3/*3, CYP3A5*1/*3, or CYP3A5*1/*1.
Model building
The covariates were tested in a step-wise manner. In the first step, the OFV for the base model (pharmacokinetic model with no covariates) was observed. The covariates were analysed next by forward inclusion by the following procedure: (a) univariate analysis was performed, (b) the insignificant covariates were removed from further consideration, (c) the significant covariates (OFV >6.63 for 1 d.f.) were ranked in terms of their significance towards tacrolimus CL/F, as assessed by the magnitude of drop in the OFV, (d) the covariate with the highest rank (i.e. most significant), was included into an updated model and (e) the remaining significant covariates were tested for significance by adding them univariately to the updated model. Steps (b) through (e) were repeated until all the significant covariates were included into the forward inclusion model and all insignificant covariates were discarded. Backward elimination was then performed by removing each group within a covariate at a time (e.g. days 6–10 and 11–180 separately). An increase in OFV (>10.83 for 1 d.f.) was used to obtain the final model.
Model evaluation
For the purpose of model evaluation, a non-parametric bootstrap approach was employed. A single bootstrap run generated a new dataset, by random sampling with replacement from the original dataset. Bootstrap runs (n = 1 000) were performed and non-parametric statistics, median and 2.5th and 97.5th percentile were obtained from successful bootstrap runs (successful was defined as achieving both convergence and covariance step). A close agreement between the non-parametric statistics and the estimates from the original dataset (≤10%) was indicative of the stability and performance of the population model.
Results
Tacrolimus troughs (n = 11 823) from 681 adult kidney transplant recipients obtained in the first 6 months post transplant were studied. Patient characteristics, tacrolimus doses and troughs are given in Table 1. The mean ± SD daily doses over the 6 months period for the non-AA and AA were 0.07 ± 0.05 and 0.09 ± 0.04 mg kg−1, respectively. The mean ± SD troughs for the non-AA and AA patients were 8.66 ± 3.37 and 6.82 ± 3.51 ng ml−1, respectively. A majority (59%) of the subjects received a living donor transplant and 21% of the population was AA. In our study, in the first week post transplant, 75% (n = 413) of all transplant recipients, 69% (n = 307) of non-AA and 96% (n = 106) of AA, had a trough concentration <8 ng ml−1. In the second week post transplant, 55% (n = 331) of all transplant recipients, 48% (n = 228) of non-AA and 82% (n = 103) of AA, had a trough <8 ng ml−1. The six genetic factors and their allele frequencies are shown in Table 2. Factors affecting tacrolimus CL/F in order of their importance were days post transplant, presence of CYP3A5*1 allele (rs776746), transplantation at a steroid sparing centre, recipient age and CCB use (Table 3). The typical value of CL/F was 38.4 l h−1 and decreased by 14% (0.86) in days 6–10 post transplant and by 29% (0.71) in days 11–180 post transplant, relative to the days 3–5 post transplant. Patients who carried one or more CYP3A5*1 alleles had lower troughs than those with the CYP3A5*3 allele. Troughs and dose requirements by genotype are shown in Figure 1 (panels A and B). CL/F was increased by 69% (1.69) in subjects with the CYP3A5*1/*3 genotype and by 100% (2.00) in subjects with the CYP3A5*1/*1 genotype. CL/F was reduced by 30% (0.70) in patients undergoing transplantation at a centre using a steroid sparing immunosuppressive regimen and by 6% (0.94) when a CCB was co-administered compared with no CCB. CL/F increased until the median age of 50 years and then decreased thereafter. Recipient weight, gender, race, donor type and gender, pre-emptive transplant, number of prior transplants, and the variants rs12114000, rs3734354, rs4926, rs3135506 and rs2608555 were not significant. The following equation describes the final model for estimation of tacrolimus CL/F in the first 6 months post transplant.
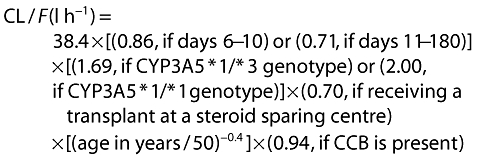 |
The total daily dose (TDD) requirement is then calculated from the estimated tacrolimus CL/F above and the desired goal trough concentration.
 |
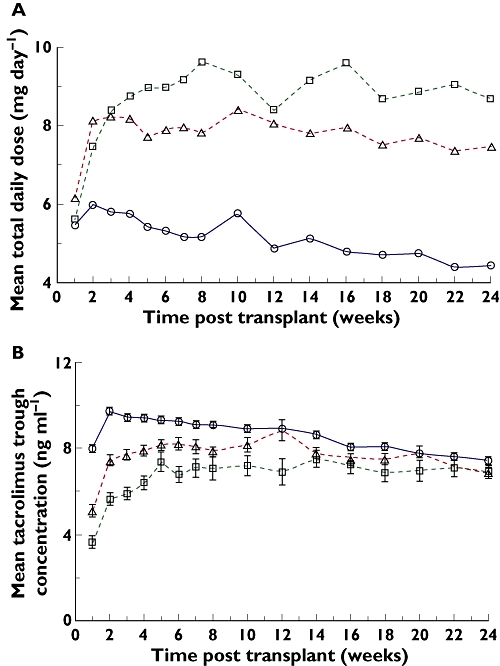
The base model had an IIV of 52.3% in CL/F. The final model had an IIV of 40.1% in CL/F. Thus, the final model was able to explain 23.2% of the relative IIV in CL/F. Plots of the observed (OBS) concentrations vs. the model predicted (PRED) concentrations and OBS vs. the individual predicted (IPRED) concentrations are shown in Figure 2. A plot of the weighted residuals (WRES) vs. time shows that most of the data lies within 3 units from the zero-ordinate (Figure 2). In addition, the mean parameter estimates from the study population and the 989 successful bootstrap runs are highly comparable, thereby confirming the accuracy and precision of the estimates as well as stability of the final model (Table 3). The post hoc estimates of CL/F from the final model by the three different genotypes are shown in Figure 3.
Table 3.
Final parameter estimates and effect of genetic and clinical factors on tacrolimus CL/F
| Study population1 | Bootstrap analysis2 | |||
|---|---|---|---|---|
| Parameter | Estimate (%RSE)3 | 95% CI4 | Median | 2.5th–97.5th percentiles |
| Tacrolimus CL/F5 | 38.4 (4.14) | 35.3, 41.5 | 38.3 | 35.5, 41.7 |
| Factors affecting CL/F | ||||
| 6–10 DPT6 | 0.86 (4.13) | 0.80, 0.93 | 0.86 | 0.80, 0.93 |
| 11–180 DPT6 | 0.71 (4.14) | 0.66, 0.77 | 0.72 | 0.66, 0.77 |
| CYP3A5*1/*3 | 1.70 (3.99) | 1.56, 1.82 | 1.69 | 1.56, 1.82 |
| CYP3A5*1/*1 | 2.00 (5.90) | 1.77, 2.23 | 1.99 | 1.77, 2.23 |
| Steroid sparing centre | 0.70 (3.50) | 0.65, 0.75 | 0.70 | 0.65, 0.75 |
| (Age/50)θ | −0.40 (13.5) | −0.50, −0.30 | −0.39 | −0.50, −0.29 |
| CCB use7 | 0.94 (2.43) | 0.89, 0.98 | 0.94 | 0.90, 0.99 |
| IIV8 for CL/F, %CV | 40.1 | 37.4, 43.6 | 40.0 | 37.4, 43.6 |
| RUV9, additive, SD | 3.19 | 3.07, 3.32 | 3.19 | 3.08, 3.32 |
681 patients analysed in this study
results from 989 bootstrap runs with successful convergence and successful covariance step
per cent relative standard error
confidence interval: estimate ± (1.96*standard error of estimate)
typical value of CL/F in l h−1
days post transplant
calcium channel blocker use at the time of trough measurement
inter-individual variability
random unexplained variability.
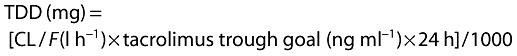
Figure 1.
Tacrolimus doses and troughs by CYP3A5 genotype (○ CYP3A5*3/*3, ▵ CYP3A5*1/*3, □ CYP3A5*1/*1) over the first 6 months post transplant. (A) Total daily doses by CYP3A5 genotype. (B) Trough concentrations by CYP3A5 genotype (mean ± SE)
Figure 2.
Goodness-of-fit plots for the final tacrolimus model: IPRED, individual predicted concentrations (ng ml−1); WRES, weighted residuals
Figure 3.
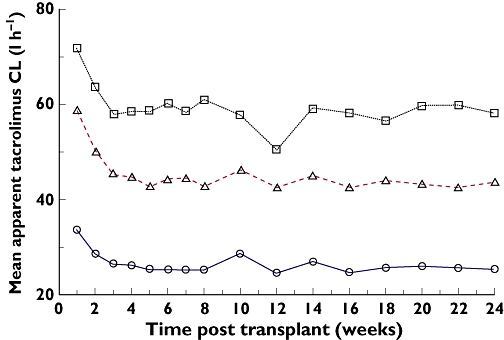
Post hoc estimates of tacrolimus CL/F from the final model over the first 6 months post transplant by CYP3A5 genotype (○ CYP3A5*3/*3, ▵ CYP3A5*1/*3, □ CYP3A5*1/*1)
Discussion
We report here the first dosing model for tacrolimus using a combination of genetic and clinical factors in adult kidney transplant recipients that was developed from one of the largest tacrolimus pharmacogenetics studies (n = 681) conducted to date. We found that CL/F was significantly influenced by days post transplant, CYP3A5 genotype, transplantation at a steroid sparing centre, recipient age and the use of a CCB. The population CL/F was 38.4 l h−1 and is close to estimates from other pharmacokinetic studies (ranging from 21 to 35 l h−1) [10, 23, 24]. Our estimate of CL/F is slightly larger than previously reported studies. This is expected because, as stated earlier, we modelled (CL/F)*, an approximation to the tacrolimus apparent clearance. In addition, differences in patient populations between the studies cannot be ignored, nor can the influence of covariates that have been included in our model.
In our study, 75% (n = 413) and 55% (n = 331) of the transplant recipients had tacrolimus trough concentrations <8 ng ml−1 in the first week and second week post transplant, respectively. These troughs are below the usual trough goal in centres participating in this study (8–12 ng ml−1 in the first 3 months). These troughs were achieved through the use of the typical mg kg−1 dosing and it is possible that a higher number of patients would achieve troughs >8 ng ml−1 if dose individualization using clinical and genetic factors had been used.
Days post transplant was the most significant clinical factor affecting tacrolimus CL/F and has been previously shown to be associated with CL/F[9, 10, 25–27]. Tacrolimus CL/F decreased by 14% in days 6–10 post transplant and by 29% in days 11–180 post transplant, relative to the immediate post-transplant period (days 3–5). This decrease in CL/F is consistent with previous findings [10, 26]. A decrease in CL/F may be attributable to an increase in tacrolimus bioavailability over time as the patients clinical status improves. CL/F may also decrease due to an increase in haematocrit and albumin concentrations with time as kidney function is restored.
The CYP3A5 genotype was also highly associated with CL/F. Individuals who carry one or more CYP3A5*1 alleles express the CYP3A5 enzyme [28, 29]. Tacrolimus is a substrate for CYP3A5 and it is well established that individuals carrying one or more *1 alleles have a higher tacrolimus CL and lower trough concentrations [11–14, 17]. Several previous studies have highlighted the differences in CL/F and dose requirements for the CYP3A5*1 carriers compared with individuals with the CYP3A5*3/*3 genotype [24, 30–34]. In a study involving paediatric kidney transplant recipients, tacrolimus CL/F was about 50% higher in children with the CYP3A5*1/*1 or *1/*3 genotype as compared with the CYP3A5*3/*3 genotype [8]. A recent pharmacokinetic study found tacrolimus CL/F to be about twofold higher in CYP3A5 expressors (*1/*1 or *1/*3 genotype) as compared with the CYP3A5 non-expressors (*1/*1 genotype) [31]. In an earlier study on the pharmacokinetics of tacrolimus in healthy Japanese subjects, CL/F was about 1.5 times higher in the CYP3A5*1 carriers (*1/*1 or *3/*3 genotype) as compared with the CYP3A5*3/*3 genotype [35]. Most studies have combined genotype groups (*1/*1 with *1/*3) due to sample size limitations [13–15, 36]. Given our large sample size, we were able to define the differences in tacrolimus CL/F between three CYP3A5 genotype groups. In our study, subjects with the CYP3A5*1/*3 and *1/*1 genotypes had a CL/F that was 70% and 100% higher, respectively, than those with the CYP3A5*3/*3 genotype. These data demonstrate for the first time that the three CYP3A5 genotypes have distinctive CL/F estimates and dose requirements. The majority (85%) of our non-AA population had the CYP3A5*3/*3 genotype, whereas the majority (87%) of the AAs had the CYP3A5*1/*1 or CYP3A5*1/*3 genotype. Despite this, race was insignificant in our final dosing model most likely due to collinearity between CYP3A5 genotype and race. Although the CYP3A5 genotype is associated with tacrolimus CL/F, it is not associated with acute rejection [37–39]. The lack of association is not surprising given that multiple factors increase the risk of rejection (i.e. donor type, recipient age, HLA compatibility, low calcineurin inhibitor concentrations). Importantly though, data show that patients with the CYP3A5*1/*3 or *1/*1 genotype have earlier acute rejection and are slower to achieve target concentrations [14].
Our analysis found an important centre effect. Centres were categorized by the use of a steroid sparing immunosuppressive regimen or not. A steroid sparing immunosuppressive protocol administers corticosteroids for a short period of time (typically 7–14 days) in the early post-transplant period whereas non-sparing centres maintain steroids throughout the first 6 months or longer [40, 41]. We found that CL/F was decreased by 30% in patients transplanted at a steroid sparing centre. We hypothesize that the centre effect is related to steroid use and that continuous therapy leads to an induction of CYP enzymes and higher tacrolimus CL/F. Various studies have demonstrated an induction of CYP3A enzymes by corticosteroid therapy [42–44]. Although controversial, studies have identified corticosteroid therapy as a significant factor towards tacrolimus CL/F[9, 27, 45–47]. Clinical practice varies substantially between centres. Therefore, the attribution of the effect to steroids cannot be confirmed in our study and must be directly tested in future analyses.
Age and CCB use were also identified as significant covariates towards CL/F. CL/F increased progressively up to age 50 years and then decreased thereafter. The concomitant use of a CCB was associated with a small (6%) decrease in tacrolimus CL/F. Multiple CCBs were used in our study and we did not collect the specific CCB prescribed. The CCB, diltiazem, is a well-known potent inhibitor of the CYP3A enzyme and decreases tacrolimus CL/F[48, 49]. Other CCBs (such as amlodipine) are not potent inhibitors of CYP3A [50]. Therefore, the inhibitory effects of some CCBs may be overestimated whereas the effect of diltiazem is likely underestimated.
As this study is based on a large population, we expect the estimates from this study to be fairly reliable. However, the data for this analysis came from an observational study where supervision of trough measurements was conducted by the clinical teams. Haematocrit and aspartate aminotransferase (AST) have been previously shown to be important clinical factors [10] and neither was collected in our study. Future studies should also consider concomitant administration of anti-fungals given the potential for drug interactions [51, 52].
The dosing equation which we developed is simple and uses common clinical factors and one genotype. The availability of this equation now allows for the testing of clinical and genetic factor guided vs. traditional weight-based initial dosing. As the achievement of therapeutic concentrations early post transplant is of importance, we would expect the use of individualized dosing to result in a higher proportion of patients within the target range and thereby lower the risk for acute rejection. This model was developed from data in adult individuals within the first 6 months post transplant. Whether it can be extrapolated beyond this time frame is not known. An advantage with our equation is that any tacrolimus trough may be targeted including patients where it is desirable to provide a higher level of immunosuppression as well as those who may be candidates for calcineurin sparing.
An example of how this model is applied clinically is as follows. Suppose we wish to determine prospectively the oral tacrolimus dose in a 50-year-old, 85 kg kidney transplant recipient on day 3 post transplant with a goal tacrolimus trough of 10 ng ml−1 and a genotype of CYP3A5*1/*1, in a steroid using centre, receiving a CCB.
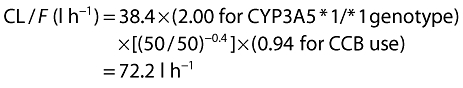 |
The total daily dose (TDD) requirement is:
The daily dose is 17.5 mg or 8.5–9 mg twice daily. Should this patient have received a typical weight-based dosing (0.1 mg kg−1 day−1) the estimated dose would be 8.5 mg day−1 or 4–4.5 mg twice daily which would have likely under-dosed this patient.
As another example, let us suppose that we wish to determine the oral tacrolimus dose in a 50-year-old, 85 kg kidney transplant recipient on day 100 post transplant with a goal tacrolimus trough of 8 ng ml−1 and a genotype of CYP3A5*3/*3, who underwent transplantation at a steroid sparing centre, and is not receiving a CCB.
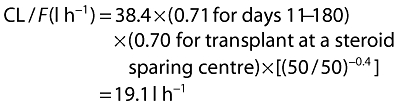 |
The total daily dose (TDD) requirement is:
The daily dose is 3.6 mg or 1.5–2 mg twice daily. Should this patient have received our typical weight-based dosing (0.1 mg kg−1 day−1) the estimated dose would be 8.5 mg day−1 or 4–4.5 mg twice daily which would have likely overdosed this patient.
This model now requires confirmation in an independent population and prospective testing.
Acknowledgments
We appreciate the critical review of this manuscript by Smita Kshirsagar, PhD.
This project was supported by grant number (5U19-AI070119) from the National Institute of Allergy and Infectious Disease (PJ, WO).
Competing Interests
Chaitali Passey, Angela K. Birnbaum, William S. Oetting and Pamala A. Jacobson have no conflict of interest. Richard C. Brundage owns stocks in Glaxo Smith Kline.
REFERENCES
- 1.Bowman LJ, Brennan DC. The role of tacrolimus in renal transplantation. Expert Opin Pharmacother. 2008;9:635–43. doi: 10.1517/14656566.9.4.635. [DOI] [PubMed] [Google Scholar]
- 2.Wallemacq P, Armstrong VW, Brunet M, Haufroid V, Holt DW, Johnston A, Kuypers D, Le Meur Y, Marquet P, Oellerich M, Thervet E, Toenshoff B, Undre N, Weber LT, Westley IS, Mourad M. Opportunities to optimize tacrolimus therapy in solid organ transplantation: report of the European consensus conference. Ther Drug Monit. 2009;31:139–52. doi: 10.1097/FTD.0b013e318198d092. [DOI] [PubMed] [Google Scholar]
- 3.Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet. 2004;43:623–53. doi: 10.2165/00003088-200443100-00001. [DOI] [PubMed] [Google Scholar]
- 4.Laskow DA, Vincenti F, Neylan JF, Mendez R, Matas AJ. An open-label, concentration-ranging trial of FK506 in primary kidney transplantation: a report of the United States Multicenter FK506 Kidney Transplant Group. Transplantation. 1996;62:900–5. doi: 10.1097/00007890-199610150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Borobia AM, Romero I, Jimenez C, Gil F, Ramirez E, De Gracia R, Escuin F, Gonzalez E, Sansuan AJ. Trough tacrolimus concentrations in the first week after kidney transplantation are related to acute rejection. Ther Drug Monit. 2009;31:436–42. doi: 10.1097/FTD.0b013e3181a8f02a. [DOI] [PubMed] [Google Scholar]
- 6.O'Seaghdha CM, McQuillan R, Moran AM, Lavin P, Dorman A, O'Kelly P, Mohan DM, Little P, Hickey DP, Conlon PJ. Higher tacrolimus trough levels on days 2-5 post-renal transplant are associated with reduced rates of acute rejection. Clin Transplant. 2009;23:462–8. doi: 10.1111/j.1399-0012.2009.01021.x. [DOI] [PubMed] [Google Scholar]
- 7.Floren LC, Bekersky I, Benet LZ, Mekki Q, Dressler D, Lee JW, Roberts JP, Hebert MF. Tacrolimus oral bioavailability doubles with coadministration of ketoconazole. Clin Pharmacol Ther. 1997;62:41–9. doi: 10.1016/S0009-9236(97)90150-8. [DOI] [PubMed] [Google Scholar]
- 8.Zhao W, Elie V, Roussey G, Brochard K, Niaudet P, Leroy V, Loirat C, Cochat P, Cloarec S, Andre JL, Garaix F, Bensman A, Fakhoury M, Jacqz-Aigrain E. Population pharmacokinetics and pharmacogenetics of tacrolimus in de novo pediatric kidney transplant recipients. Clin Pharmacol Ther. 2009;86:609–18. doi: 10.1038/clpt.2009.210. [DOI] [PubMed] [Google Scholar]
- 9.Antignac M, Barrou B, Farinotti R, Lechat P, Urien S. Population pharmacokinetics and bioavailability of tacrolimus in kidney transplant patients. Br J Clin Pharmacol. 2007;64:750–7. doi: 10.1111/j.1365-2125.2007.02895.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Staatz CE, Willis C, Taylor PJ, Tett SE. Population pharmacokinetics of tacrolimus in adult kidney transplant recipients. Clin Pharmacol Ther. 2002;72:660–9. doi: 10.1067/mcp.2002.129304. [DOI] [PubMed] [Google Scholar]
- 11.Quteineh L, Verstuyft C, Furlan V, Durrbach A, Letierce A, Ferlicot S, Taburet AM, Charpentier B, Becquemont L. Influence of CYP3A5 genetic polymorphism on tacrolimus daily dose requirements and acute rejection in renal graft recipients. Basic Clin Pharmacol Toxicol. 2008;103:546–52. doi: 10.1111/j.1742-7843.2008.00327.x. [DOI] [PubMed] [Google Scholar]
- 12.Staatz CE, Goodman LK, Tett SE. Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: Part I. Clin Pharmacokinet. 2010;49:141–75. doi: 10.2165/11317350-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Renders L, Frisman M, Ufer M, Mosyagin I, Haenisch S, Ott U, Caliebe A, Dechant M, Braun F, Kunzendorf U, Cascorbi I. CYP3A5 genotype markedly influences the pharmacokinetics of tacrolimus and sirolimus in kidney transplant recipients. Clin Pharmacol Ther. 2007;81:228–34. doi: 10.1038/sj.clpt.6100039. [DOI] [PubMed] [Google Scholar]
- 14.MacPhee IA, Fredericks S, Tai T, Syrris P, Carter ND, Johnston A, Goldberg L, Holt DW. The influence of pharmacogenetics on the time to achieve target tacrolimus concentrations after kidney transplantation. Am J Transplant. 2004;4:914–9. doi: 10.1111/j.1600-6143.2004.00435.x. [DOI] [PubMed] [Google Scholar]
- 15.Zhang X, Liu ZH, Zheng JM, Chen ZH, Tang Z, Chen JS, Li LS. Influence of CYP3A5 and MDR1 polymorphisms on tacrolimus concentration in the early stage after renal transplantation. Clin Transplant. 2005;19:638–43. doi: 10.1111/j.1399-0012.2005.00370.x. [DOI] [PubMed] [Google Scholar]
- 16.Pascual J, Galeano C, Royuela A, Zamora J. A Systematic Review on Steroid Withdrawal Between 3 and 6 Months After Kidney Transplantation. Transplantation. 2010;90:343–9. doi: 10.1097/TP.0b013e3181e58912. [DOI] [PubMed] [Google Scholar]
- 17.Thervet E, Loriot MA, Barbier S, Buchler M, Ficheux M, Choukroun G, Toupance O, Touchard G, Alberti C, Le Pogamp P, Moulin B, Le Meur Y, Heng AE, Subra JF, Beaune P, Legendre C. Optimization of initial tacrolimus dose using pharmacogenetic testing. Clin Pharmacol Ther. 2010;87:721–6. doi: 10.1038/clpt.2010.17. [DOI] [PubMed] [Google Scholar]
- 18.Van Ness B, Ramos C, Haznadar M, Hoering A, Haessler J, Crowley J, Jacobus S, Oken M, Rajkumar V, Greipp P, Barlogie B, Durie B, Katz M, Atluri G, Fang G, Gupta R, Steinbach M, Kumar V, Mushlin R, Johnson D, Morgan G. Genomic variation in myeloma: design, content, and initial application of the Bank On A Cure SNP Panel to detect associations with progression-free survival. BMC Med. 2008;6:26. doi: 10.1186/1741-7015-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardenbol P, Baner J, Jain M, Nilsson M, Namsaraev EA, Karlin-Neumann GA, Fakhrai-Rad H, Ronaghi M, Willis TD, Landegren U, Davis RW. Multiplexed genotyping with sequence-tagged molecular inversion probes. Nat Biotechnol. 2003;21:673–8. doi: 10.1038/nbt821. [DOI] [PubMed] [Google Scholar]
- 20.Jacobson PA, Oetting WS, Brearley A, Leduc R, Guan W, Schladt D, Matas AJ, Lamba V, Julian B, Mannon R, Israni I. Novel polymorphisms associated with tacrolimus trough concentrations: results from a Multicenter Kidney Transplant Consortium. Transplantation. 2011;91:300–8. doi: 10.1097/TP.0b013e318200e991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jusko WJ, Piekoszewski W, Klintmalm GB, Shaefer MS, Hebert MF, Piergies AA, Lee CC, Schechter P, Mekki QA. Pharmacokinetics of tacrolimus in liver transplant patients. Clin Pharmacol Ther. 1995;57:281–90. doi: 10.1016/0009-9236(95)90153-1. [DOI] [PubMed] [Google Scholar]
- 22.Wallemacq PE, Furlan V, Moller A, Schafer A, Stadler P, Firdaous I, Taburet AM, Reding R, De Clety C, De S, De Goyet J, Sokal E, Lykavieris L, Van Leeuw V, Bernard O, Otte JB, Undre NA. Pharmacokinetics of tacrolimus (FK506) in paediatric liver transplant recipients. Eur J Drug Metab Pharmacokinet. 1998;23:367–70. doi: 10.1007/BF03192295. [DOI] [PubMed] [Google Scholar]
- 23.Staatz CE, Willis C, Taylor PJ, Lynch SV, Tett SE. Toward better outcomes with tacrolimus therapy: population pharmacokinetics and individualized dosage prediction in adult liver transplantation. Liver Transpl. 2003;9:130–7. doi: 10.1053/jlts.2003.50023. [DOI] [PubMed] [Google Scholar]
- 24.Tada H, Tsuchiya N, Satoh S, Kagaya H, Li Z, Sato K, Miura M, Suzuki T, Kato T, Habuchi T. Impact of CYP3A5 and MDR1(ABCB1) C3435T polymorphisms on the pharmacokinetics of tacrolimus in renal transplant recipients. Transplant Proc. 2005;37:1730–2. doi: 10.1016/j.transproceed.2005.02.073. [DOI] [PubMed] [Google Scholar]
- 25.Pou L, Brunet M, Andres I, Rodamilans M, Lopez R, Corbella J. Influence of posttransplant time on dose and concentration of tacrolimus in liver transplant patients. Transpl Int. 1998;11(Suppl. 1):S270–1. doi: 10.1007/s001470050476. [DOI] [PubMed] [Google Scholar]
- 26.Lee JY, Hahn HJ, Son IJ, Suh KS, Yi NJ, Oh JM, Shin WG. Factors affecting the apparent clearance of tacrolimus in Korean adult liver transplant recipients. Pharmacotherapy. 2006;26:1069–77. doi: 10.1592/phco.26.8.1069. [DOI] [PubMed] [Google Scholar]
- 27.Antignac M, Fernandez C, Barrou B, Roca M, Favrat JL, Urien S, Farinotti R. Prediction tacrolimus blood levels based on the Bayesian method in adult kidney transplant patients. Eur J Drug Metab Pharmacokinet. 2011;36:25–33. doi: 10.1007/s13318-011-0027-z. [DOI] [PubMed] [Google Scholar]
- 28.Lamba JK, Lin YS, Schuetz EG, Thummel KE. Genetic contribution to variable human CYP3A-mediated metabolism. Adv Drug Deliv Rev. 2002;54:1271–94. doi: 10.1016/s0169-409x(02)00066-2. [DOI] [PubMed] [Google Scholar]
- 29.Xie HG, Wood AJ, Kim RB, Stein CM, Wilkinson GR. Genetic variability in CYP3A5 and its possible consequences. Pharmacogenomics. 2004;5:243–72. doi: 10.1517/phgs.5.3.243.29833. [DOI] [PubMed] [Google Scholar]
- 30.Hesselink DA, van Schaik RH, van der Heiden IP, van der Werf M, Gregoor PJ, Lindemans J, Weimar W, van Gelder T. Genetic polymorphisms of the CYP3A4, CYP3A5, and MDR-1 genes and pharmacokinetics of the calcineurin inhibitors cyclosporine and tacrolimus. Clin Pharmacol Ther. 2003;74:245–54. doi: 10.1016/S0009-9236(03)00168-1. [DOI] [PubMed] [Google Scholar]
- 31.Benkali K, Rostaing L, Premaud A, Woillard JB, Saint-Marcoux F, Urien S, Kamar N, Marquet P, Rousseau A. Population pharmacokinetics and bayesian estimation of tacrolimus exposure in renal transplant recipients on a new once-daily formulation. Clin Pharmacokinet. 2010;49:683–92. doi: 10.2165/11535950-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 32.Tsuchiya N, Satoh S, Tada H, Li Z, Ohyama C, Sato K, Suzuki T, Habuchi T, Kato T. Influence of CYP3A5 and MDR1 (ABCB1) polymorphisms on the pharmacokinetics of tacrolimus in renal transplant recipients. Transplantation. 2004;78:1182–7. doi: 10.1097/01.tp.0000137789.58694.b4. [DOI] [PubMed] [Google Scholar]
- 33.Zhao Y, Song M, Guan D, Bi S, Meng J, Li Q, Wang W. Genetic polymorphisms of CYP3A5 genes and concentration of the cyclosporine and tacrolimus. Transplant Proc. 2005;37:178–81. doi: 10.1016/j.transproceed.2005.01.077. [DOI] [PubMed] [Google Scholar]
- 34.Wang P, Mao Y, Zhou X, Wong TS, Patel S, Elliott E, Shea E, Wu HA, Gaber AO. Using genetic and clinical factors to predict tacrolimus dose in renal transplant recipients. Pharmacogenomics. 2010;11:1389–402. doi: 10.2217/pgs.10.105. [DOI] [PubMed] [Google Scholar]
- 35.Suzuki Y, Homma M, Doki K, Itagaki F, Kohda Y. Impact of CYP3A5 genetic polymorphism on pharmacokinetics of tacrolimus in healthy Japanese subjects. Br J Clin Pharmacol. 2008;66:154–5. doi: 10.1111/j.1365-2125.2008.03162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woillard JB, de Winter BC, Kamar N, Marquet P, Rostaing L, Rousseau A. Population pharmacokinetic model and Bayesian estimator for two tacrolimus formulations – twice daily Prograf and once daily Advagraf. Br J Clin Pharmacol. 2011;71:391–402. doi: 10.1111/j.1365-2125.2010.03837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Satoh S. CYP3A5 1 allele associated with tacrolimus trough concentrations but not subclinical acute rejection or chronic allograft nephropathy in Japanese renal transplant recipients. Eur J Clin Pharmacol. 2009;65:473–81. doi: 10.1007/s00228-008-0606-3. [DOI] [PubMed] [Google Scholar]
- 38.Hesselink DA. CYP3A5 genotype is not associated with a higher risk of acute rejection in tacrolimus-treated renal transplant recipients. Pharmacogenet Genomics. 2008;18:339–48. doi: 10.1097/FPC.0b013e3282f75f88. [DOI] [PubMed] [Google Scholar]
- 39.Israni A, Leduc R, Holmes J, Jacobson PA, Lamba V, Guan W, Schladt D, Chen J, Matas AJ, Oetting WS. Single-nucleotide polymorphisms, acute rejection, and severity of tubulitis in kidney transplantation, accounting for center-to-center variation. Transplantation. 2010;90:1401–8. doi: 10.1097/TP.0b013e3182000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matas AJ. Minimization of steroids in kidney transplantation. Transpl Int. 2009;22:38–48. doi: 10.1111/j.1432-2277.2008.00728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li L, Weintraub L, Concepcion W, Martin JP, Miller K, Salvatierra O, Sarwal MM. Potential influence of tacrolimus and steroid avoidance on early graft function in pediatric renal transplantation. Pediatr Transplant. 2008;12:701–7. doi: 10.1111/j.1399-3046.2007.00884.x. [DOI] [PubMed] [Google Scholar]
- 42.Guengerich FP. Cytochrome P-450 3A4: regulation and role in drug metabolism. Annu Rev Pharmacol Toxicol. 1999;39:1–17. doi: 10.1146/annurev.pharmtox.39.1.1. [DOI] [PubMed] [Google Scholar]
- 43.El-Sankary W, Plant NJ, Gibson GG, Moore DJ. Regulation of the CYP3A4 gene by hydrocortisone and xenobiotics: role of the glucocorticoid and pregnane X receptors. Drug Metab Dispos. 2000;28:493–6. [PubMed] [Google Scholar]
- 44.McCune JS, Hawke RL, LeCluyse EL, Gillenwater HH, Hamilton G, Ritchie J, Lindley C. In vivo and in vitro induction of human cytochrome P4503A4 by dexamethasone. Clin Pharmacol Ther. 2000;68:356–66. doi: 10.1067/mcp.2000.110215. [DOI] [PubMed] [Google Scholar]
- 45.Undre NA, Schafer A. Factors affecting the pharmacokinetics of tacrolimus in the first year after renal transplantation. European Tacrolimus Multicentre Renal Study Group. Transplant Proc. 1998;30:1261–3. doi: 10.1016/s0041-1345(98)00234-6. [DOI] [PubMed] [Google Scholar]
- 46.Lam S, Partovi N, Ting LS, Ensom MH. Corticosteroid interactions with cyclosporine, tacrolimus, mycophenolate, and sirolimus: fact or fiction? Ann Pharmacother. 2008;42:1037–47. doi: 10.1345/aph.1k628. [DOI] [PubMed] [Google Scholar]
- 47.Velickovic-Radovanovic R, Catic-Djordjevic A, Milovanovic JR, Djordjevic V, Paunovic G, Jankovic SM. Population pharmacokinetics of tacrolimus in kidney transplant patients. Int J Clin Pharmacol Ther. 2010;48:375–82. doi: 10.5414/cpp48375. [DOI] [PubMed] [Google Scholar]
- 48.Li JL, Wang XD, Chen SY, Liu LS, Fu Q, Chen X, Teng LC, Wang CX, Huang M. Effects of diltiazem on pharmacokinetics of tacrolimus in relation to CYP3A5 genotype status in renal recipients: from retrospective to prospective. Pharmacogenomics J. 2010 doi: 10.1038/tpj.2010.42. doi: 10.1038/tpj.2010.42. [DOI] [PubMed] [Google Scholar]
- 49.Hebert MF, Lam AY. Diltiazem increases tacrolimus concentrations. Ann Pharmacother. 1999;33:680–2. doi: 10.1345/aph.18356. [DOI] [PubMed] [Google Scholar]
- 50.Ma B, Prueksaritanont T, Lin JH. Drug interactions with calcium channel blockers: possible involvement of metabolite-intermediate complexation with CYP3A. Drug Metab Dispos. 2000;28:125–30. [PubMed] [Google Scholar]
- 51.Capone D, Tarantino G, Gentile A, Sabbatini M, Polichetti G, Santangelo M, Nappi R, Ciotola A, D'Alessandro V, Renda A, Basile V, Federico S. Effects of voriconazole on tacrolimus metabolism in a kidney transplant recipient. J Clin Pharm Ther. 2010;35:121–4. doi: 10.1111/j.1365-2710.2009.01070.x. [DOI] [PubMed] [Google Scholar]
- 52.Paterson DL, Singh N. Interactions between tacrolimus and antimicrobial agents. Clin Infect Dis. 1997;25:1430–40. doi: 10.1086/516138. [DOI] [PubMed] [Google Scholar]


