Abstract
Objectives
To study short- and long-term effects of experiencing a disaster in repatriated injured survivors and the differential effect of injury, need for medical treatment, loss of loved ones and danger to life on both physical and mental health.
Design
Prospective online study.
Setting
Open online survey among Dutch survivors of the 2004 Asian tsunami.
Participants
Of the estimated total of 464 Dutch survivors, the authors recruited 144 unique respondents (59 men and 85 women) with a total of 175 assessments made in various time periods.
Main outcome measures
Health outcomes were Symptom Checklist 90 (SCL-90), Impact of Event Scale (original version, in Dutch) and Beck Depression Inventory II. Correlations were calculated with socio-demographic as well as disaster-related factors: physical injury, medical care, loss of loved ones and duration of threat to life. Assessments were clustered in four post-disaster time periods (0–3, 4–6, 7–30 and 31–48 months).
Results
Across these periods, SCL-90 scores were significantly higher than the reference population (p<0.001), with a significant linear downward trend between the groups over time (p=0.001). The same pattern occurred for the Impact of Event Scale (p<0.001) and the Beck Depression Inventory II (p=0.002). Physical injury, medical care or loss of loved ones was not associated with higher total SCL-90 scores or somatic subscores. Both duration of threat to life and female sex were correlated with all measured outcome parameters.
Conclusions
Exposure to the 2004 Asian tsunami had significant short- and long-term impacts on health complaints in a group of repatriated Dutch tsunami victims. Cross-sectionally, there was a trend towards recovery over 4 years, although 22% still reported high psychological and physical distress 4 years post-disaster. Duration of danger to life and female sex were associated with more physical and mental health complaints. In this study, neither disaster-related injury nor loss of loved ones resulted in negative health outcomes.
Article summary
Article focus
Disasters are traumatic events that may result in a wide range of physical and mental health consequences. The aim of this paper was to study short- and long-term effects in injured disaster survivors.
Our hypothesis was that physical injury and psychological trauma (eg, loss of loved ones) would be determinants for physical and mental health outcomes after the disaster.
Key messages
Despite a trend towards recovery between the cross-sectional groups over 4 years, the 2004 tsunami had significant short- and long-term impacts on health complaints in a Dutch group of tsunami victims.
Physical injury or loss of loved ones did not necessarily result in negative health outcomes.
Duration of danger to life was a predictor for traumatic stress symptoms, general health complaints as well as depressive symptoms over a 4-year period.
Strengths and limitations of this study
One of the few studies of long-term physical and mental health impact of natural disasters and the differential effects of being wounded, danger to life and loss of loved ones.
Combined approach: research on physical as well as mental health—unique set up with a survey on an online post-disaster web service, combined with other features.
Limitations: post-disaster study limited options for longitudinal research.
Introduction
Disasters are traumatic events that may result in a wide range of physical and mental health consequences. In addition to despair and grief, as well as sadness and anger in the case of lost or missing loved ones, injured survivors of disaster typically face challenges in the immediate aftermath of disaster, such as danger to life, injury, displacement from home, transportation and seeking rapid and adequate medical help. A proportion of victims will present in a hospital for disaster-related physical injury to receive medical care. It has been indicated that those who are physically injured would eventually be in worse physical and mental shape when compared with a non-injured group.1–3 The same could be true for the loss of loved ones. However, the predictive value of being wounded, needing medical care or losing loved ones on the long-term mental and physical outcome has not often been studied. Studies on post-disaster health effects typically focus on post-traumatic stress disorder (PTSD). This is the most commonly studied mental disorder that can occur in the aftermath of disasters.3–5 Millions of people were affected by the 2004 Asian tsunami and an estimated 227 898 people died.6 Particular to this disaster was that many tourists were visiting the area. Most of them returned to their unaffected home environment. The impact of the 2004 Asian tsunami on these repatriated victims has been studied in survivors living in Scandinavian countries; however, this also mainly focused on PTSD.7–9
Many post-disaster studies emphasise the need for long-term follow-up to eventually better understand trajectories of illness and recovery and identify situational and personal risk factors for long-term complaints.3 5 10
In a previous, prospective follow-up study, in a small cohort of injured survivors of the 2004 tsunami, we demonstrated that the long-term impact of exposure to the Asian tsunami on physical and emotional status, as well as on healthcare use and daily activities, was considerable.11 The current study presents new data on physical and mental effects collected in a larger cohort of Dutch survivors of the 2004 tsunami over a 4-year time span. Our goal was to examine the impact of exposure to this disaster on short-term (first months), middle-term and long-term (4 years) health complaints in an affected population. We were interested in finding predictors of negative health outcome and, in particular, the predictive value of disaster-related factors (injury, loss of loved ones, danger to life). Furthermore, we were interested in the differential effect of physical injury and the physical burden of experiencing both physical and psychological trauma.
Awareness of and insight into the impact of disasters on health complaints in the short and long term could provide opportunities for surveillance and early treatment. It could contribute to the recognition of eventual late health consequences.
Methods
Study design and participants
The registered count of Dutch visitors that were present in the affected area is 500, of whom 36 died during the disaster. In collecting data from this Dutch affected population, we employed a novel approach through a web-based service that contained an open online survey on the physical and mental health status of survivors. In January 2005, 2 weeks after the disaster, a web service (http://www.tisei.org) was launched to foster (community) support in the aftermath of the disaster.12 13 The website was unique in combining several functionalities aimed at empowerment of survivors utilising (1) information services with news feeds selected for the target population, (2) an online survey with self-assessment questionnaires, (3) an open forum and (4) optional e-consultation service.
In the long run, the web portal also served as a memorial archive for anniversary meetings and follow-up incentives. We reported elsewhere on the traffic that the web portal generated and the usability of the web service.12 13 This current report focuses on the results of the 4-year follow-up survey of the Dutch population.
Patient recruitment for the survey was performed by an announcement on the website and postings in national and local media. A link to the web portal was provided on the site of the International Society for Traumatic Stress Studies. Over a 4-year time span, between January 2005 and January 2009, the survey was available by registration to the survivors of the disaster. We collected 175 survey lists from 144 respondents. We grouped the assessments in four time periods (0–3, 4–6, 7–30 and 31–48 months after the disaster).
Subjects needed to be at least 18 years old to qualify for participation. Prior to participating in the survey, participants gave informed consent and registered to receive a password by email to enter the survey. The institutional review board of the University Medical Centre Utrecht and the MIH approved the study after an expedited review. All data were stored anonymously in accordance with European law. The self-assessment/survey was accompanied by an optional e-consult service for participant safety, as focusing on details of these topics could potentially exacerbate distress in an already distressed participant.14 In the Dutch portal, all questionnaires that were used were translated versions into Dutch (Babel Translations, Utrecht).
Measurements
The survey consisted of nine questionnaires, with a total of 271 questions. These were divided into 6–34 items per viewing page, with the exception of one section that contained 90 questions. The number of screens (viewing pages) was 14. Respondents were able to review and change their answers using a back button.
Demographics and disaster-related factors
The survey started with questions about details of exposure to the disaster and situational information (eg, type of injury, closeness to the sea, endangerment of life, loss of loved ones). Duration of danger to life was qualified in four categories as: none, minutes, half hour to hours and one or several day(s). These questionnaires also contained questions about physical injury to the participant, as well as their relatives, including eventual death. When appropriate, questions were accompanied by space for free text.
Disaster-related questions were followed by questions on socio-demographic details. The following socio-demographic and lifestyle characteristics were measured: sex, age, marital status (single/with partner), children, living situation (with parents/alone/with partner/other), employment status (having a job or studying) and education level. The latter was divided into three groups: low (no formal education, elementary school, lower vocational education or lower general secondary education), middle and high (college or university). Furthermore, information regarding medical and mental health status as well as medical history was gathered together with medication, smoking and alcohol use.
Psychological and physical distress
The Symptom Checklist 90 (SCL-90-R)15 16 was used to assess physical and psychological symptoms. This checklist contains 90 questions with a 5-point rating scale on physical and emotional complaints. Respondents were asked to rate how much discomfort each symptom has caused them in the past week (including today), ranging from ‘not at all’ (score 1) to ‘extremely’ (score 5). Outcome scores were divided into nine symptom subscales or dimensions: agoraphobia (AGO, range 7–35), anxiety (ANX, range 10–50), depression (DEP, range 16–80), somatisation (SOM, range 12–60), insufficient thinking and handling (IN, range 9–45), distrust and interpersonal sensitivity (SEN, range 18–90), hostility (HOS, range 6–30), sleeping disorders (SLE, range 3–15) and a rest subscale (REST, range 9–45). The total score (SCL-90-TOT, range 90–450) was calculated by adding the scores of the subscales. This quantified the general level of symptomatic psychological and physical distress. The Dutch SCL-90 has shown to have good psychometric properties.17 Dimension scores and the total SCL-90 scores were compared with the established references for the general Dutch population (norm group II, n=2368), adjusted for sex.16
Impact of the event
The Impact of Event Scale (IES)18 19 was used to assess the degree of intrusions and avoidance reactions related to the traumatic event, in a window of the previous 7 days. The Dutch version consists of 15 questions with a 4-point Likert scale on frequency and intensity of symptoms (none=0, rarely=1, sometimes=3 and often=5). An overall score (range 0–75) was calculated by adding the scores on the individual items. The Dutch IES is well validated.19 A cut-off score of >25 was used to identify victims with relatively severe intrusion and avoidance symptoms.20
Depression
For assessment of depressive symptoms, the Beck Depression Inventory (BDI-II)21 was used, a 21-questionmultiple-choice self-report inventory that quantifies the severity of depression. Scores ranged from ‘no symptoms’ to ‘very severe’ symptoms, with a maximum of 3 points for each question. The scores ranged from 0 to 63. A score of 0–13 was regarded as minimal symptoms of depression, 14–19 mild, 20–28 moderate severe and 29–63 marked as severe depression.21 22 Questions were divided into three dimensions or subscales (cognitive, somatic and affective). The BDI has good psychometric properties.23
Statistical analysis
The interval between the disaster and the moment of entry into the survey varied substantially among respondents. Therefore, we chose to stratify the data into four post-disaster time periods. The first two were relatively short (3 months) and the last two covered a longer time span (24 and 18 months, respectively). The time periods were labelled as months post-disaster: 0–3 months (T1), 4–6 months (T2), 7–30 months (T3) and 31–48 months (T4). Time period (four nominal categories) and gender (male/female) were dealt with as stratification factors in the statistical analyses.
Raw summary statistics (mean and SD) of the continuous outcome variables SCL-90 (total scale and subscales), IES and BDI (total scales) were presented for the entire group and for the groups by time period. Also raw relative frequency distributions were presented per time period after a relevant categorisation of those outcome variables. In order to account for repeated assessments of participants that completed the survey more than once, the continuous outcome variables were also analysed using linear mixed modelling. A compound symmetry structure was imposed on the (co)variances of the repeated measures. A first simple mixed model analysis only involved time period and gender as explanatory factors in order to present gender-adjusted means and their confidence limits; also a test against trend in time was carried out using this simple model.
In a more elaborate mixed model analysis, the following explanatory demographic, outcome and disease-related factors were entered simultaneously in the linear mixed model, along with time period and gender: age (numeric trend of four ordinal levels), education (numeric trend of three ordinal levels), employment (yes/no), marital status (single/partner), physical history (yes/no), psychological history (yes/no), physical disaster-related injury (DRI) (yes/no), medical care (yes/no), loss of loved ones (yes/no) and duration of danger to life (numeric trend of four ordinal levels). The effects of the last four explanatory variables were also tested one-by-one against modification by time period at the more stringent significance level of 0.01 than the level of 0.05 used otherwise.
Deviations in observed SCL-90 scales in male and female respondents from the corresponding, assumedly fixed, means of the Dutch normal reference population (16) were also analysed using linear mixed modelling with time period (T1–T4) as an explanatory factor.
Internal consistency of the SCL-DEP and BDI-II scores, both testing for depressive symptoms, was quantified by using the partial correlation coefficient with adjustment for time period and gender.
All calculations were performed with the PASW/SPSS® statistics 18.0 software (IBM®).
Results
Respondents and trauma
Over 4 years, 175 surveys were completed, which could be anonymously linked to 144 unique respondents. Of these 144 respondents, 120 respondents completed the survey assessment once, 18 respondents filled in two assessments at different times, five respondents participated in three assessments and one respondent completed four assessments. The completion rate of all questionnaires of the entire survey was 93%. Sixty-seven (38%) of the survey lists were filled in by 59 men and 108 (62%) surveys by 85 women. The majority of the respondents fell within the age range 25–60 years. Nine respondents were younger and two were older than 60 years. Between the different time periods, there were no significant differences in age distribution and gender. The education level was high and 90% were employed. Also, the group was relatively healthy. Of all respondents, 17% were taking medication and 28% were smokers. For socio-demographic details of the respondents see table 1. Of the respondents, 74% were on vacation and 6% were in the area for work at the time of the tsunami. The respondents vacationed in Thailand (81), Sri Lanka (43), India (18) and Indonesia (2). Only 13 (9%) of the respondents were travelling alone and the rest were either with family or friends.
Table 1.
Socio-demographic details of all 144 participants
| Gender | n | % |
| Males | 59 | 41 |
| Females | 85 | 59 |
| Age group | ||
| 18–25 | 9 | 6 |
| 25–40 | 74 | 51 |
| 40–60 | 59 | 41 |
| >60 | 2 | 1 |
| Marital status | ||
| Single | 29 | 20 |
| Married | 115 | 80 |
| Children | ||
| Yes | 53 | 37 |
| No | 91 | 63 |
| Educational level | ||
| Low | 8 | 7 |
| Middle | 42 | 30 |
| High (college or university degree) | 90 | 63 |
| Unavailable | 4 | |
| Employment | ||
| No work/study | 15 | 10 |
| Work/study | 129 | 90 |
| Health history (before disaster) | ||
| Physical history | 29 | 20 |
| History psych/emotional complaints | 45 | 31 |
| Medication | 25 | 17 |
| Smoking | 41 | 28 |
| Alcohol | 88 | 61 |
Italic font signifies the percentage of participants.
When asked about disaster-specific experiences, one-third of the respondents reported that they had seen the sea pulling back and only one-third was not on the beach during the event. Respondents reported that they were pulled by the wave (32), ran from it (35) or had been hiding on a roof (6). Almost half of the respondents (40%) had been some time under water. Some of the most frequent reported experiences at the time of the disaster included the roaring noise of the wave, screaming people, seeing collapsing buildings, seeing dead people, panic and the feeling that you could die any moment. Seventy-four per cent of the respondents reported negative experiences and 86% also reported positive experiences, such as the resiliency of the Thai people, brotherhood and hospitality.
Forty-nine of the respondents (34%) reported that they had been wounded as a result of the tsunami and 46 (32%) needed medical care. Thirty-one (22%) of the respondents had a loved one that was killed in the tsunami. The majority of the respondents had experienced danger to life, ranging from minutes to hours and for 13 respondents this lasted more than a day. A minority of 27 respondents (20%) had not been in danger of losing their life during the disaster. For details and distribution of disaster-related trauma factors in the time periods, see table 2.
Table 2.
Disaster-related factors: injury, situational factors and representation in the time periods
| Total group |
Total group |
T1 (%), 0–3 months |
T2 (%), 4–6 months |
T3 (%), 7–30 months |
T4 (%), >30 months |
|||||||
| 144 Participants |
175 Lists |
59 |
28 |
51 |
37 |
|||||||
| Injured | 49 | 34% | 66 | 38% | 16 | 27% | 11 | 39% | 23 | 45% | 16 | 43% |
| Medical care | 46 | 32% | 59 | 34% | 13 | 22% | 10 | 36% | 21 | 41% | 15 | 41% |
| Missing/died loved ones | 31 | 22% | 38 | 22% | 11 | 19% | 8 | 29% | 11 | 22% | 8 | 22% |
| Danger to life | ||||||||||||
| None | 27 | 20% | 32 | 20% | 13 | 22% | 4 | 16% | 6 | 13% | 9 | 32% |
| Minutes | 50 | 38% | 63 | 40% | 18 | 31% | 13 | 52% | 21 | 45% | 11 | 39% |
| 1/2 hour to hour(s) | 43 | 30% | 49 | 31% | 21 | 36% | 7 | 28% | 14 | 30% | 7 | 25% |
| Day(s) | 13 | 10% | 14 | 9% | 6 | 10% | 1 | 4% | 6 | 13% | 1 | 4% |
| Unavailable | 11 | 17 | 1 | 3 | 4 | 9 | ||||||
Italic font signifies the percentage of participants.
General distress; psychological and physical symptoms (SCL-90)
For male respondents, the mean overall SCL-90-TOT score was 142.8 (SD 53.0). For female respondents, the mean was 149.3 (SD 54.2). Across the whole group, in any time period, the mean SCL-90 of the study population was significantly higher than that in the reference population,16 accounting for sex (p<0.0005).
There were 12 respondents who caused 12 missing values on the SCL-90. Their profiles did not differ significantly in age, gender or exposure from the rest of the group.
Raw summary statistics of the SCL-90, IES and BDI (175 lists) and the representation in the different time periods can be found in table 3. Table 4 shows the percentages of participants with high scores across the time periods, including SCL-90 subscales.
Table 3.
Mean SCL-90, IES and BDI scores across the time periods (raw summary statistics of all 175 lists)
| Total |
T1, 0–3 months |
T2, 4–6 months |
T3, 7–30 months |
T4, 31–48 months |
||||||
| 175 |
59 |
28 |
51 |
37 |
||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| SCL-90-TOT | ||||||||||
| Males | 142.8 | 53.0 | 160.2 | 68.1 | 126.1 | 35.5 | 142.7 | 50.5 | 130.6 | 34.2 |
| Females | 149.3 | 54.2 | 165.9 | 61.1 | 170.7 | 56.1 | 132.0 | 37.4 | 135.8 | 50.4 |
| Unavailable | 12 | 3 | 3 | 5 | 1 | |||||
| IES | 30.1 | 15.9 | 36.1 | 15.1 | 30.3 | 17.5 | 38.9 | 15.5 | 21.6 | 12.7 |
| Unavailable | 5 | 1 | 0 | 1 | 3 | |||||
| BDI | 11.6 | 8.6 | 14.8 | 9.3 | 10.2 | 7.4 | 10.1 | 8.0 | 9.3 | 8.0 |
| Unavailable | 12 | 3 | 3 | 4 | 2 | |||||
BDI, Beck Depression Inventory II; IES, Impact of Event Scale; SCl-90, Symptom Checklist 90.
Table 4.
Physical complaints, high general distress (SCL-90), high avoidance and intrusion reactions (IES) and degree of depressive complaints (categorical BDI scores) (raw summary frequencies of all 175 lists) by time period
| Total 175 lists | T1, 0–3 months |
T2, 4–6 months |
T3, 7–30 months |
T4, >30 months |
||||||
| Total | 59 |
28 |
51 |
37 |
||||||
| Physical complaints | 81 | 46% | 30 | 51% | 12 | 43% | 25 | 49% | 14 | 38% |
| High general distress (SCL-90, >mean+1 SD) | ||||||||||
| TOT | 52 | 32% | 23 | 41% | 10 | 40% | 11 | 24% | 8 | 22% |
| SLA | 51 | 31% | 25 | 45% | 8 | 32% | 14 | 30% | 4 | 11% |
| HOS | 36 | 22% | 13 | 23% | 9 | 36% | 8 | 17% | 6 | 17% |
| SEN | 28 | 17% | 11 | 20% | 6 | 24% | 6 | 13% | 5 | 14% |
| IN | 62 | 38% | 30 | 54% | 10 | 40% | 12 | 26% | 10 | 28% |
| SOM | 38 | 23% | 20 | 36% | 4 | 16% | 8 | 17% | 6 | 17% |
| DEP | 62 | 38% | 28 | 50% | 11 | 44% | 15 | 33% | 8 | 22% |
| ANG | 47 | 29% | 21 | 38% | 8 | 32% | 11 | 24% | 7 | 19% |
| AGO | 64 | 39% | 27 | 48% | 9 | 36% | 16 | 35% | 12 | 33% |
| Unavailable | 12 | 3 | 3 | 5 | 1 | |||||
| Severe avoidance and intrusion (IES) | ||||||||||
| IES>25 | 170 | 57% | 43 | 74% | 14 | 50% | 28 | 56% | 12 | 35% |
| Unavailable | 5 | 1 | 0 | 1 | 3 | |||||
| Depressive complaints (BDI-II) | ||||||||||
| Minimal (0–13) | 104 | 64% | 30 | 54% | 15 | 60% | 33 | 70% | 26 | 74% |
| Mild (14–19) | 28 | 17% | 11 | 20% | 6 | 24% | 6 | 13% | 5 | 14% |
| Moderate to severe (20–28) | 23 | 14% | 8 | 14% | 4 | 16% | 8 | 17% | 3 | 9% |
| Severe (29–63) | 8 | 5% | 7 | 13% | 0 | 0% | 0 | 0% | 1 | 3% |
| Unavailable | 12 | 3 | 3 | 4 | 2 | |||||
SCL-90 scores are defined as high when they exceed the sex-specific mean +1 SD taken from the reference population. A cut-off score of the IES of >25 is used to identify victims with relatively severe intrusion and avoidance symptoms.20 The BDI is divided in four categories of severity of depressive symptoms.21 22
BDI, Beck Depression Inventory II; IES, Impact of Event Scale; SCl-90, Symptom Checklist 90.
Italic font signifies the percentage of participants.
Estimated mean SCL-90-TOT scores and their 95% CIs by time period and gender, resulting from linear mixed modelling, are presented in table 5. The pooled within-SD equals 52.4. Average significant downward trends with time period were found in men and women: 9.9 points per time period in men (95% CI –18.3 to –1.5, p=0.022) and 6.9 points per time period in women (95% CI –11.8 to –2.0, p=0.007).
Table 5.
Estimated mean SCL-90-TOT, IES and BDI by time period and gender using linear mixed modelling
| SCL-90-TOT |
IES |
BDI |
||||
| Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | |
| Time period 1, male | 159.7 | 141.7 to 177.7 | 35.0 | 28.5 to 41.4 | 14.1 | 10.7 to 17.4 |
| Time period 1, female | 163.7 | 150.3 to 177.2 | 37.5 | 32.7 to 42.3 | 16.0 | 13.5 to 18.6 |
| Time period 2, male | 140.1 | 118.1 to 162.1 | 29.8 | 22.1 to 37.6 | 10.0 | 6.0 to 14.0 |
| Time period 2, female | 145.6 | 119.9 to 171.4 | 28.5 | 20.4 to 36.6 | 11.6 | 6.7 to 16.4 |
| Time period 3, male | 135.9 | 118.2 to 153.5 | 27.4 | 21.2 to 33.7 | 11.2 | 8.0 to 14.5 |
| Time period 3, female | 132.3 | 114.3 to 150.4 | 28.7 | 23.1 to 34.4 | 9.6 | 6.5 to 12.7 |
| Time period 4, male | 130.1 | 104.8 to 155.3 | 19.1 | 7.4 to 30.8 | 7.6 | 2.5 to 12.7 |
| Time period 4, female | 145.3 | 131.8 to 158.7 | 24.4 | 19.0 to 29.8 | 9.9 | 7.2 to 12.6 |
BDI, Beck Depression Inventory II; IES, Impact of Event Scale; SCl-90, Symptom Checklist 90.
Of the demographics and disaster-related factors, only the duration of danger to life had a significantly negative effect on SCL-90-TOT: there is an average increase of 8.3 (SE 3.9) points in SCL-90-TOT per category of longer duration. None of the other factors had a significant effect on SCL-90-TOT. There was no indication that the effect of longer duration of danger was modified by time period (p=0.12). None of the other three factors that were tested against effect modification by time period reached significance.
Of the SCL subscales, significant main effects of the demographics and disaster-related factors were only seen on SCL-HOS (hostility) and SCL-SLE (sleep) subscales. Respondents who had received medical care had a 2.60 point (SE 0.79, p=0.002) higher score on SCL-HOS than those without medical care, the effect of which was not significantly modified by time period (p=0.42). A longer duration of danger to life resulted in a 0.63 point (SE 0.31, p=0.044) higher score on SCL-SLE (sleep) per category of duration length. No significant modification of this effect by time period was seen (p=0.11).
All SCL subscales showed a downward trend with time period, although not all subscales reached significance in this respect. On none of the SCL subscales, could a significant effect of gender be observed.
Somatic complaints (SCL-SOM) were only significantly higher than the reference population in the first time period T1 (difference of +4.6 points, p<0.0005, 95% CI 2.5 to 6.3). This was not observed in later time periods. The entire group (not stratified in time periods), as a whole, also scored higher on the SCL-SOM than the reference group (+2.01 points, p=0.003, 95% CI 0.7 to 3.4) and the somatic subscale also showed a significant linear downward trend (p=0.002).
Avoidance and intrusion (IES)
Estimated mean IES scores and their 95% CIs, by time period and gender resulting from linear mixed modelling, are presented in table 5. Five respondents had a missing IES list. The mean IES was 30.1 (SD 15.9). The pooled within-SD equalled 15.5. Significant downward trend effects with time period (T1 to T4) were found in men and women: on average 4.3 points per time period in men (95% CI –7.9 to –0.7, p=0.018) and 4.3 points per time period in women (95% CI –6.5 to –2.1, p<0.0005).
Singles scored 7.7 points (SE 3.5, p=0.032) higher on IES than those with a partner. We found an average increase of 3.0 points (SE 1.5, p=0.042) in IES per category of duration length of danger to life. None of the other disaster-related factors had a significant effect on IES. Also no significant effect modifications by time period at the 0.01 level were found. Both time period (as a categorical variable) and gender did not have significant main effects on IES (respective p values 0.096 and 0.30).
Depressive complaints (BDI)
Estimated mean BDI scores and their 95% CIs, by time period and gender resulting from linear mixed modelling, are presented in table 5. The pooled within-SD equalled 8.5. Significant downward trends with time period were found in men and women: on average 1.7 points per time period in men (95% CI –3.4 to –0.0, p=0.048) and 2.3 points per time period in women (95% CI –3.2 to –1.1, p<0.0005).
Some disease and injury-related factors had a significant effect on BDI scores. Physical injury resulted in a 3.95 point (SE 1.74, p=0.032) higher BDI score. Having received medical care resulted in a 3.93 point (SE 1.79, p=0.044) lower BDI score. Per category higher duration of danger gave a 1.58 point (SE 0.71, p=0.035) higher BDI score.
We found no indication that these effects on BDI were modified by time period (respective p values: 0.45, 0.65 and 0.071). Time after the disaster (T1–T4) had a significant main effect on BDI (p=0.004) but gender did not (p=0.99).
The partial correlation between the SCL-DEP and the BDI, corrected for time period and gender, was 0.85, which indicated a good internal consistency of the data.
Discussion
This study is among the first studies27 28 to use a web portal and to collect data from a community in order to assess the long-term impact of a (natural) disaster on health complaints over a long time span.
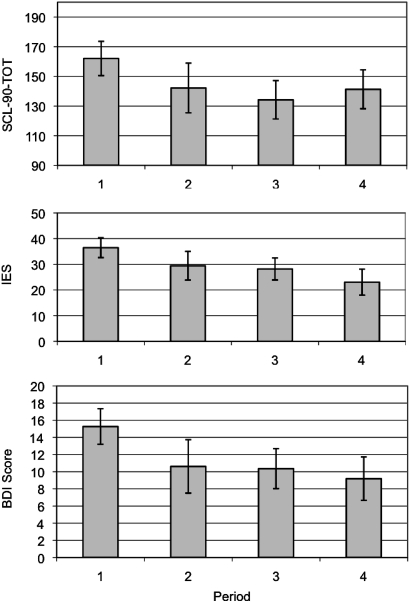
The data show that the Dutch tourists in this study, which were exposed to a major natural disaster and repatriated to their unaffected home environments, had elevated scores on somatic as well as psychological symptoms. Remarkably, over time, there was a significant drop in scores across all symptom scales (figure 1), but all scores remained elevated in comparison to norm scores in the long run.16–20 With reference to the initial hypothesis, it could not be demonstrated that DRI or death of loved ones correlated with negative outcome scores or with more somatisation. Duration of danger to life showed to be a predictor for worse health-related outcome scores at all time points. Furthermore, when comparing gender outcomes, it appears that women have higher scores (SCL-90) than men.
Figure 1.
Mean Symptom Checklist 90 (SCl-90)-TOT, Impact of Event Scale (IES) and Beck Depression Inventory (BDI) II across the time periods. Gender-adjusted mean SCL-90-TOT, IES and BDI scores with 95% CIs estimated using linear mixed modelling. There is a significant downward trend of the gender-adjusted means (p=0.001, p<0.0005 and p=0.002, tests against trend).
These data are remarkably similar to a recent postal survey among disaster-exposed repatriated Scandinavian tourists. Participants were categorised according to disaster exposure: danger exposed (caught by waves), non-danger exposed (other disaster-related stressors) and non-exposed. It appeared that danger-exposed subjects reported more post-traumatic stress than non-danger-exposed individuals and symptoms attenuated by 14-month follow-up.7 In their sample, female gender and low education predicted higher levels of symptoms. Yet, based on a smaller Norwegian sample, the authors reported that recall amplification of perceived life threat needed to be accounted for. Recalled life-threat intensity increased from 6 to 24 months, which questioned diagnostic validity of PTSD symptom improvement.29 Recall amplification was associated with a lack of PTSD symptom improvement. This does not apply to the sample in this study as, while remaining high, health symptoms improved over time.
Although with these data individual trajectories of recovery cannot be studied, in this data set, a trend of recovery between the groups in the time periods is visible. Over a time span of 4 years, the affected group, as a whole, demonstrated an attenuation of reported physical and mental health complaints. This was observed with all outcome parameters (IES, BDI and SCL-90). Evidence of a general decline of incidence of PTSD can also be found in the literature3 but is not so well documented for overall psychological and physical well-being as measured with the SCL-90. There are not many long-term (several years) post-disaster follow-up studies.3 Even though symptoms attenuated, 4 years after the tsunami, 22% of all respondents still reported high levels of general distress and 12% were moderately to severely depressed. On intrusions and avoidance reactions, 35% of the respondents in the last time period scored higher than the cut-off for severity.
The hypothesis was that the health complaints would be related to being wounded, the need of receiving medical care at the time of the disaster or the loss of loved ones, in accordance with the literature on PTSD after disasters, where physical injury and loss of a close family member are indicated as risk factors for the development of PTSD.3 This could not be confirmed for either of these parameters on outcomes of mental and physical distress, somatic subscale, impact of events and depression. A significant number of respondents (34%) reported that they had been wounded as a result of the tsunami; a similar sized group needed medical care for their injuries. They fell into a category that was labelled as DRIs, varying from wounds and fractures to concussion and lung injury. Yet, none of these contributed to a worse outcome on short- and long-term health assessment. In an earlier study, similar findings were reported in a small group of injured victims that were medically repatriated because of their injuries. Twenty-five per cent of this cohort rated their health, 4 years after the disaster, as worse than before and a third of the group still felt hindered in their daily activities 4 years post-disaster.11 Surprisingly, DRI failed to demonstrate lower quality of life scores at 6 months and 4 years in comparison to a reference population.11 30 31
In this current study, female gender appears to be a risk factor for negative outcomes of physical and mental health. This is consistent with the literature that indicates female gender as a risk factor for PTSD.5
There are only a few studies on the influence of physical injury on general psychological and physical status in disaster-exposed patients, and therefore, comparison with the current data is limited. Although PTSD study outcomes will not be the same as outcomes in studies on general physical and psychological distress, they could provide indications about factors that might affect the SCL-90. The rates of post-disaster PTSD should be used with caution as they are identified in different studies using different diagnostic criteria and methods.32 A recent study of Thai tsunami victims by Thavichachart et al described factors associated with PTSD. They reported that ‘injury’ and ‘being in the direct affected area’ were found to be correlated with psychological factors.33 Although they used the SCL-90 in their survey, their outcomes for this parameter are not available in their report for comparison with the results of this study. Although some earlier studies indicated that injury1 3 and loss of loved ones could be regarded as factors of influence on development of PTSD,3 33 in this sample, no relationship was found between these factors and general psychological and physical well-being (not equalling PTSD) as measured by the SCL-90.
While the body of research has focused on PTSD and other psychiatric disorders among disaster victims, some studies also document other symptoms, for example somatic complaints.34 In a study in Puerto Rico, exposure to a natural disaster was related to a high prevalence of medically unexplained physical symptoms, particularly gastrointestinal and pseudoneurological symptoms. This and other studies are suggestive of clinically important new somatisation after disasters.25 34 The results from this study also show significantly elevated scores on the somatic subscale of the SCL-90, predominantly caused by high somatic complaints in the acute phase. In this study, DRI among these victims did not result in higher scores on the somatisation dimension of the SCL-90. van den Berg et al35 showed that medically unexplained symptoms are common in survivors of disasters and are more prevalent in those affected by disasters compared with the general population. In some studies, medically unexplained symptoms had been measured by the somatisation scale of the SCL-90.35
One important limitation of the interpretation of this dimension must be highlighted. Although this scale was designed to assess somatic complaints, the diagnosis of somatisation (disorder) would require the ability to rule out medically based explanations of the reported symptoms 25, and this was not done in this study.
Thirty-six Dutch tourists did not survive the tsunami. Of all respondents, 22% were related to one of this group of 36. When looking at the impact of the loss of loved ones on somatic and mental health, no significant effect could be attributed to this factor. The group that was affected by this loss did not demonstrate a significant difference in outcome scores in comparison to the group that did not suffer from such a loss.
Duration of danger to life, however, proved to be a good predictor of health outcome, while actual injury was not. In many PTSD studies, ‘the degree of exposure to the disaster’ is associated with the likelihood of PTSD,5 which is highest with direct exposure to the disaster.3 In a systematic review by Neria et al,3 this is mentioned as the most consistently documented determinant of the risk of PTSD. Exposure is measured differently in several studies and therefore difficult to compare. Mostly it is defined by distance to the scene or observed ‘things’ rather than in (duration of) endangerment to one's own life. In this study, injury (thus direct proximity to disaster) was not correlated to worse outcomes but duration of danger to life was. The majority of the respondents (80%) had experienced danger to life, ranging from minutes to hours and in some this lasted more than a day. This factor appeared to have strong predictive value for non-specific reported health complaints. There was no specific cluster of health complaints that could be identified to account for this. In a study after Turkish earthquakes by Basoglu et al,36 fear of danger to life was also found to be a determinant. This could indicate that fear for one's own life could be the determinant factor in exposure that causes higher scores in people that were close the disaster.
Study limitations
There are several limitations to the current study that have to be taken into account. First, the sample studied is a self-selected sample of convenience from the total affected Dutch population. This is a recognised potential limitation of the disaster literature.1 It was not possible, for obvious reasons, to compare the responding tsunami survivors participating in the online survey with a non-responding group of survivors. Selective non-response, based on socioeconomic and psychosocial variables influencing the result, can therefore not be ruled out. As in almost every survey after a disaster, participants form a volunteer sample rather than a probability sample.26 Yet, given the fact that at the time of the tsunami approximately 500 Dutch people were present in the disaster areas, a considerable part of the target population volunteered to participate in the survey. Notwithstanding that this was a study with a sample of convenience, the cross-sectional analysis demonstrates a trend of recovery. It is known from other studies that trajectories of recovery can be long; however, few empirical studies exist. This study, with data collected over a considerable time span, makes a valuable contribution to the literature. Selective attrition may have been minimised because the web portal also contained a forum, information and an online survey, so this also attracted participants that did not seek professional help, in contrast to interview studies among (self) referred patients.37 38 As for reliability of internet-based questionnaires, several studies have shown that sensitive topics, such as assessment of psychiatric symptoms, are more likely to be reported in self-reported assessments than in interview-based assessments and that computerised forms are a good alternative. Although not confirmed in all studies,39 web-based data collection, therefore, has a potential to reduce social desirability bias.40–42
Second, the difficulty of matching respondents in time, caused by technical aspects of survey setup, negatively influenced the research opportunities of the site. The site was launched within 3 weeks after the tsunami. Within ample time, a template for the site, study design, selection and adaptation of questionnaires, and approval of institutional review board were obtained. Several issues, such as copyrights, securing patient information and data, as well as referral systems, resulted in compromises between feasibility and study demand.
This study reveals that 31% (144/500−36) of the Dutch tsunami survivors could be reached for voluntary participation in the open survey through the TISEI site with no renumeration.
Secure logins with passwords were sent to participants by email when they participated in the survey. These theoretically could be used for long-term follow-up, but due to the method of anonymisation (required by European law) that was used, independent entries at a particular time could not automatically be matched to the same patient. For the same reasons, recruitment of survivors to participate in different time periods proved complicated. True longitudinal follow-up was not possible, and we were forced to analyse the results cross-sectionally with multiple time point assessment.13
Earlier online initiatives in the aftermath of disasters and the terrorist attack of 9/11,28 reviewed in surveys by Silver et al,27 43 indicate the great potential of the internet for health- and disaster-related research. Further development of techniques should be able to facilitate this in future online initiatives.
Third, pre-disaster measurements of this population were not available and, therefore, there is no prospective data as to their pre-existent psychiatric morbidity. Introversion, neuroticism and a history, or family history, of psychiatric disorder are known premorbidity factors significantly associated with the development of chronic mental health problems after natural disaster.5 24 Thirty-one per cent of the participants reported previous psychological or emotional problems in the post-disaster self-report. Since this group was mostly in the area for vacation or business, it may be assumed that they were a resilient group.
Finally, studies of responses to disaster mostly have a necessarily observational and post-event nature, which makes it difficult to identify true causal relationships between exposure and observed outcomes. Although this survey will therefore not provide causal incidence data, empirical evidence and qualitative research on the impact of disaster exposure will aid clinicians in designing interventions for individuals coping with negative outcome.44
Future perspectives and conclusions
Using a web service for long-term cross-sectional research among subjects after exposure to a natural disaster proved a feasible opportunity for support as well as research. Emerging Web 2.0 technologies, with social media and applications, are providing web users and health workers with a new approach for information sharing and knowledge dissemination, as well as, research opportunities. Internet social networking tools, being immediate, two-way and large scale, can be successfully utilised as a solution in emergency response during disasters,45 as well as for patient empowerment and long-term follow-up of survivors.13 With greatly improved technology and use of social media, long-term longitudinal research through an internet survey has many promising prospects. The identification of individuals at risk for health complaints following a disaster may help organisations decrease both human and economic costs. Awareness of and insight into the impact of disasters on health complaints, in the short and long term, can provide opportunities for surveillance and early treatment.
In conclusion, even though there is a group-wise trend of recovery of physical and mental health over a 4-year time period, high psychological and physical distress was seen in tourists exposed to a natural disaster. Despite significant improvement over the collected time periods, one of five participants reported persistent somatic complaints, while one of three reported high avoidance and intrusion scores 4 years after exposure. One of seven participants still reported moderate to severe depression scores. Duration of danger to life served as a predictor for all health-related outcome measures. DRI and loss of loved ones, however, did not necessarily result in negative outcomes in short- and long-term health.
The data from this study highlight that the long-term impacts of mass disaster merit a joint care approach since they impact both physical and mental health. This requires trans disciplinary care and emphasises that the field of disaster medicine should embrace both domains of expertise.
Supplementary Material
Acknowledgments
We thank the participants who took part in the web survey. The University Medical Center Utrecht, Major Incident Hospital and Faculty of Social Sciences of University Utrecht provided core support for the study. The authors wish to thank the web designers, computer technicians, research scientists, volunteers, managers and clinicians. We thank Luc Taal for technical assistance in the project and all other members of the project group, in particular Cobie Groenendijk and Rolf Kleber for contributing time and effort to realise this project. We thank Crossing Channels for resources and setting up the service in collaboration with Microsoft, Hewlett Packard and Intel. We also thank Arq Foundation, Institute for Psychotrauma and Jos Bouman for their valuable assistance.
Footnotes
To cite: Marres GMH, Leenen LPH, de Vries J, et al. Disaster-related injury and predictors of health complaints after exposure to a natural disaster: an online survey. BMJ Open 2011;1:e000248. doi:10.1136/bmjopen-2011-000248
Funding: The initiative for TISEI was supported by the Major Incident Hospital (http://www.calhosp.nl) and the Central Military Hospital (http://www.cdc.nl/mgfb/cmh) and was carried out via the University Medical Center Utrecht (http://www.umcutrecht.nl) in close collaboration with the Department of Social Sciences of the University Utrecht. The longitudinal arm of the TISEI initiative was supported by donations from the ARQ Foundation (http://www.arq.nl). No grant numbers available. A further extension of the project was enabled by a grant from M&ICT, Ministry of Economic Affairs to the NGO Echoes Online http://www.echoesonline.org. This organisation is carrying out web services in the interest of survivors of traumatic incidents. Researchers were independent from the funders.
Competing interests: None.
Ethics approval: The Institutional Review Board of the University Medical Centre Utrecht and the MIH approved the study after an expedited review.
Contributors: All authors approved the final version of the manuscript GMHM organised the data collection, was in charge of all aspects of organisation and provided input on drafts of this paper; LPHL provided scientific input on all aspects of the study design, analysis and reporting and provided input on drafts of this paper; JdV and PGHM had overall responsibility for statistical analyses and carried out statistical analyses and provided input on drafts of this paper. EV was the lead applicant for grant funding; was responsible for the overall design of measurement protocols, data collection and analysis; organised the ethical procedures and liaised with the funding body; and provided input on drafts of this paper.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Cannot be offered as consent was not obtained for data sharing and participants might be identifiable.
References
- 1.Briere J, Elliott D. Prevalence, characteristics, and long-term sequelae of natural disaster exposure in the general population. J Trauma Stress 2000;13:661–79 [DOI] [PubMed] [Google Scholar]
- 2.Hull AM, Alexander DA, Klein S. Survivors of the Piper Alpha oil platform disaster: long-term follow-up study. Br J Psychiatry 2002;181:433–8 [DOI] [PubMed] [Google Scholar]
- 3.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med 2008;38:467–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norris FH, Friedman MJ, Watson PJ, et al. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry 2002;65:207–39 [DOI] [PubMed] [Google Scholar]
- 5.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev 2005;27:78–91 [DOI] [PubMed] [Google Scholar]
- 6.Survey USG U.S. Geological Survey. http://earthquake.usgs.gov/earthquakes (accessed 12 Aug 2010).
- 7.Heir T, Rosendal S, Bergh-Johannesson K, et al. Tsunami-affected Scandinavian tourists: disaster exposure and post-traumatic stress symptoms. Nord J Psychiatry 2011;65:9–15 [DOI] [PubMed] [Google Scholar]
- 8.Jensen TK, Dyb G, Nygaard E. A longitudinal study of posttraumatic stress reactions in norwegian children and adolescents exposed to the 2004 tsunami. Arch Pediatr Adolesc Med 2009;163:856–61 [DOI] [PubMed] [Google Scholar]
- 9.Johannesson KB, Michel PO, Hultman CM, et al. Impact of exposure to trauma on posttraumatic stress disorder symptomatology in Swedish tourist tsunami survivors. J Nerv Ment Dis 2009;197:316–23 [DOI] [PubMed] [Google Scholar]
- 10.Silove D, Bryant R. Rapid assessments of mental health needs after disasters. JAMA 2006;296:576–8 [DOI] [PubMed] [Google Scholar]
- 11.Marres GMH, Vermetten E, Van der Laan L. Disaster-related injuries and quality of life; a five year prospective follow-up in a non-residential sample after the 2004 Tsunami. In review 2010.
- 12.Vermetten E, van Middelkoop CJ, et al. Online psychotrauma intervention in the aftermath of the tsunami: a community-building effort. In: Carll EK, ed Trauma Psychology: Issues in Violence, Disaster, Health, and Illness. Westport, CT: Praeger Publishers, 2007:255–71 [Google Scholar]
- 13.Marres GMH, Leenen LPH, Van der Slikke JW, et al. Use of a Web Portal for Support and Research After a Disaster—Opportunities and Lessons Learned. iJMR; [serial on the Internet]. 2010. http://knol.google.com/k/g-m-h-marres/use-of-a-web-portal-for-support-and/306jme3os9s2x/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schlenger WE, Jordan BK, Cadell JM, et al. Epidemiologic methods for assessing trauma and PTSD. In: Wilson JP, Keane TM, eds. Assessing Psychological Trauma and PTSD. 2nd edn New York: Guilford Press, 2004:226–61 [Google Scholar]
- 15.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale—preliminary report. Psychopharmacol Bull 1973;9:13–28 [PubMed] [Google Scholar]
- 16.Arrindell W, Ettema J. SCL-90, Manual for a Multidimensional Psychopatholgy Indicator [in Dutch]. Lisse, The Netherlands: Swets & Zeitlinger, 1986 [Google Scholar]
- 17.Arrindell W, Ettema H. Dimensional structure, reliability and validity of the Dutch version of the Symptom Checklist (SCL-90): Data based on a phobic and a “normal” population. Ned Tijdschr Psychol 1981;36:77–108 [Google Scholar]
- 18.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41:209–18 [DOI] [PubMed] [Google Scholar]
- 19.van der Ploeg E, Mooren TT, Kleber RJ, et al. Construct validation of the Dutch version of the impact of event scale. Psychol Assess 2004;16:16–26 [DOI] [PubMed] [Google Scholar]
- 20.Brom D, Kleber RJ. De Schokverwerkings Lijst. Ned Tijdschr Psychol 1985;40:164–8 [Google Scholar]
- 21.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory -II. San Antonio: Psychological Corporation, 1996 [Google Scholar]
- 22.Beck AT, Steer R, Brown GK. BDI-II-NL. Handleiding. De Nederlandse versie van de Beck Depression Inventory. [Manual. The Dutch version of the Beck depression Inventory - in Dutch] 2nd edn In: van der Does A, ed Lisse: Swets Test Publishers, 2002 [Google Scholar]
- 23.Beck AT, Steer RA, Carbin MG. Psychometric properties of the beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev 1988;8:77–100 [Google Scholar]
- 24.McFarlane A. The aetiology of post-traumatic stress disorders following a natural disaster. Br J Psychiatry 1988;152:116–21 [DOI] [PubMed] [Google Scholar]
- 25.North CS. Somatization in survivors of catastrophic trauma: a methodological review. Environ Health Perspect 2002;110:637–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schlenger WE, Silver RC. Web-based methods in terrorism and disaster research. J Trauma Stress 2006;19:185–93 [DOI] [PubMed] [Google Scholar]
- 27.Silver RC, Holman EA, McIntosh DN, et al. Nationwide longitudinal study of psychological responses to September 11. JAMA 2002;288:1235–44 [DOI] [PubMed] [Google Scholar]
- 28.Neria Y, Gross R, Litz B, et al. Prevalence and psychological correlates of complicated grief among bereaved adults 2.5-3.5 years after September 11th attacks. J Trauma Stress 2007;20:251–62 [DOI] [PubMed] [Google Scholar]
- 29.Heir T, Piatigorsky A, Weisaeth L. Longitudinal changes in recalled perceived life threat after a natural disaster. Br J Psychiatry 2009;194:510–14 [DOI] [PubMed] [Google Scholar]
- 30.Busschbach J, Rabin R, de Charro F, eds. Using the Internet to collect EQ-5D Norm Scores: A Valid Alternative? 24th Scientific Plenary Meeting of the Euroquolgroup, The Hague, The Netherlands, 13–15 September 2007:2009:153–65 [Google Scholar]
- 31.Lamers LM, McDonnell J, Stalmeier PF, et al. The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ 2006;15:1121–32 [DOI] [PubMed] [Google Scholar]
- 32.Wang X, Gao L, Shinfuku N, et al. Longitudinal study of earthquake-related PTSD in a randomly selected community sample in north China. Am J Psychiatry 2000;157:1260–6 [DOI] [PubMed] [Google Scholar]
- 33.Thavichachart N, Tangwongchai S, Worakul P, et al. Posttraumatic mental health establishment of the Tsunami survivors in Thailand. Clin Pract Epidemol Ment Health 2009;5:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Escobar J, Canino G, Rubio-Stipec M, et al. Somatic symptoms after a natural disaster: a prospective study. Am J Psychiatry 1992;149:965–7 [DOI] [PubMed] [Google Scholar]
- 35.van den Berg B, Grievink L, Yzermans J, et al. Medically unexplained physical symptoms in the aftermath of disasters. Epidemiol Rev 2005;27:92–106 [DOI] [PubMed] [Google Scholar]
- 36.Başoglu M, Kılıç C, Şalcıoglu E, et al. Prevalence of posttraumatic stress disorder and comorbid depression in earthquake survivors in turkey: an epidemiological study. J Trauma Stress 2004;17:133–41 [DOI] [PubMed] [Google Scholar]
- 37.Eysenbach G, Wyatt J. Using the Internet for surveys and health research. J Med Internet Res 2002;4:E13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rhodes SD, Bowie DA, Hergenrather KC. Collecting behavioural data using the world wide web: considerations for researchers. J Epidemiol Community Health 2003;57:68–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Risko EF, Quilty LC, Oakman JM. Socially desirable responding on the web: investigating the candor hypothesis. J Pers Assess 2006;87:269–76 [DOI] [PubMed] [Google Scholar]
- 40.Krantz JH, Dalal R. Validity of Web-based Psychological Research. Psychological Experiments on the Internet. San Diego: Academic Press, 2000:35–60 [Google Scholar]
- 41.Graham AL, Papandonatos GD, Bock BC, et al. Internet- vs. telephone-administered questionnaires in a randomized trial of smoking cessation. Nicotine Tob Res 2006;(8 Suppl 1):S49–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joinson A. Social desirability, anonymity, and Internet-based questionnaires. Behav Res Methods Instrum Comput 1999;31:433–8 [DOI] [PubMed] [Google Scholar]
- 43.Holman EA, Silver RC, Poulin M, et al. Terrorism, acute stress, and cardiovascular health: a 3-year national study following the September 11th attacks. Arch Gen Psychiatry 2008;65:73–80 [DOI] [PubMed] [Google Scholar]
- 44.Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry 2002;65:240–60 [DOI] [PubMed] [Google Scholar]
- 45.Huang CM, Chan E, Hyder A. Web 2.0 and internet social networking: a new tool for disaster management?—lessons from Taiwan. BMC Med Inform Decis Mak 2010;10:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.