Abstract
Social anxiety and eating disorders are highly comorbid. However, it is unknown how specific domains of social anxiety relate to disordered eating. We provide data on these relationships and investigate social appearance anxiety and fear of negative evaluation as potential vulnerabilities linking social anxiety with eating disorders. Specifically, we examined five domains of social anxiety: Social interaction anxiety, fear of scrutiny, fear of positive evaluation, fear of negative evaluation, and social appearance anxiety. Results indicated that social appearance anxiety predicted body dissatisfaction, bulimia symptoms, shape concern, weight concern, and eating concern over and above fear of scrutiny, social interaction anxiety, and fear of positive evaluation. Fear of negative evaluation uniquely predicted drive for thinness and restraint. Structural equation modeling supported a model in which social appearance anxiety and fear of negative evaluation are vulnerabilities for both social anxiety and eating disorder symptoms. Interventions that target these negative social evaluation fears may help prevent development of eating disorders.
Keywords: social appearance anxiety, social anxiety, eating disorders, body dissatisfaction, fear of negative evaluation
1. Introduction
Social anxiety disorder (SAD) and eating disorders (EDs) are highly comorbid (Pallister & Waller, 2008; Godart, Flament, Lecrubier, & Jeammet, 2000). The lifetime prevalence of SAD has been reported as 33.9% among individuals with anorexia nervosa (AN) (Halmi, Eckert, Marchi, & Sampugnaro, 1991) and as 17% among individuals with bulimia nervosa (BN) (Brewerton, Lydiard, Herzog, & Brotman, 1995) whereas the lifetime prevalence rate of SAD in the general public has been reported at 12.1% (Ruscio et al., 2008). SAD has the highest occurrence of all anxiety disorders in individuals with eating disorders: In the largest study to date exploring comorbidity between eating disorders and anxiety disorders, approximately 20% of individuals with an eating disorder also met criteria for SAD (Kaye, Bulik, Thornton, Barbarich, & Masters, 2004). Studies indicate that the onset of anxiety disorders tends to precede the development of eating disorders (Brewerton et al., 1995; Bulik, Sullivan, Fear, & Joyce, 1997; Kaye et al., 2004) and recent prospective research has suggested that social anxiety may have a causal link to eating disorders (Buckner, Silgado, & Lewinsohn, 2010). Additionally, within individuals with EDs, SAD is a barrier for help-seeking, a negative prognostic factor for treatment outcomes, and decreases engagement in effective treatments (Goodwin & Fitzgibbon, 2002).
1.1. Eating disorder risk factors
There are many well established risk factors for eating disorders, including female gender, high levels of body dissatisfaction, negative affect, societal pressure to be thin, and body mass index (for a review please see Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004). Additionally, research has found that fear is a major risk factor for disordered eating (Oliver & Wardle, 1999). Experimental manipulations, such as giving public speeches, have consistently shown that individuals either over eat or under eat in the presence of stress or fear activation (Greeno & Wing, 1994; Gluck, Geliebter, Hung, & Yahav, 2004). In the social anxiety literature, public speaking tasks have been shown produce fears of evaluation and to activate fear processing in the amygdala (LeDoux, 2000; Tillfors et al., 2001). Such results suggest that many tasks that have demonstrated an effect on eating primarily activate fear, and specifically social fears, rather than negative affect more generally. Indeed, current theoretical models of eating disorder development propose that stress from negative social evaluation may play a pivotal role as a cause of eating disorder symptoms such that social evaluation concerns may explain the high occurrence of SAD with EDs (Rieger et al., 2010). Thus, it may be that negative social evaluative fears play a crucial component in SAD and ED comorbidity.
1.2. Social anxiety fears
Individuals with SAD experience many types of social fear. Several of these fears, such as social interaction anxiety, fear of scrutiny, and fear of negative evaluation have a long history of research as domains of social anxiety (e.g., Mattick & Clarke, 1998; Watson & Friend, 1969).
1.2.1. Social interaction anxiety
Social interaction anxiety includes fears stemming from social interactions, such as making friends, attending parties, or initiating conversations (Mattick & Clarke, 1998). Such fears comprise one general category of symptoms of social anxiety disorder, as measured by overall gold-standard measures for clinical levels of social anxiety, such as the Liebowitz Social Anxiety Scale (Liebowitz, 1989), which measures severity of social anxiety symptoms, and the Anxiety Disorders Interview Schedule (DiNardo, Brown, & Barlow, 1994), which primarily assesses diagnosis of social anxiety disorder and also renders a severity score. The other general class of symptoms assessed by these instruments are performance fears or, more generally, fears of scrutiny.
1.2.2. Fear of scrutiny
Fear of scrutiny includes fears stemming from situations, such as writing, eating, or speaking in public (Mattick & Clarke, 1998), in which a person is either performing in public in a formalized way or may be observed while conducting a routine task.
1.2.3. Fear of positive evaluation
Fear of positive evaluation has been theorized to be a component of social anxiety, such that individuals high in social anxiety are more likely to fear any type of evaluation (Weeks et al., 2008). Weeks and colleagues proposed that such fears should be expected because social anxiety is related to fears of incurring the wrath of other people due to successes, in addition to the fears of rejection due to poor performance or lack of appeal, as more typically studied. The latter type of fear is represented by the construct of fear of negative evaluation.
1.2.4. Fear of negative evaluation
In the social anxiety literature, fear of negative evaluation (i.e. the fear that one’s social self will be judged negatively) is conceptualized a cognitive vulnerability or risk factor for social anxiety (Haikal & Hong, 2010; Rapee & Heimberg, 1997). Fear of negative evaluation can be thought of as a core component of social anxiety and as a feared consequence from social situations (Moscovitch, 2009). We conceptualize fear of negative evaluation both as a core vulnerability for further development of social anxiety as well as a general indicator of social evaluative fear.
1.2.5. Social appearance anxiety
Social appearance anxiety is “the fear that one will be negatively evaluated because of one’s appearance” (Hart et al., 2008). Because social appearance anxiety has been proposed more recently than some of the other constructs described above, and additionally might appear to overlap with body image constructs, we will review the evidence that it is a unique construct in more detail. Social appearance anxiety is indeed positively correlated with social interaction anxiety, fear of negative evaluation, fear of scrutiny, and measures of negative body image (Hart et al., 2008). However, it does not appear to represent mere overlap among these other constructs. Instead, social appearance anxiety has been found to be a unique construct highly related to social anxiety that taps into a unique proportion of variability in social anxiety beyond negative body image, depression, personality, and affect (i.e., social appearance anxiety predicts social anxiety when all of the constructs noted above are included in the regression equation) (Hart et al., 2008; Levinson & Rodebaugh, 2011).
More specifically, social appearance anxiety differs from body image concerns because it focuses on fears evoked from being evaluated by others on one’s overall appearance, rather than a general dissatisfaction in one’s self image because of body dissatisfaction. Further, social appearance anxiety has been found to predict social anxiety over and above measures of negative body image (Hart et al., 2008) such as the Appearance Schemas Inventory (Cash & Labarge, 1996), the Body Image Ideal Questionnaire (Cash & Szymanski, 1995), and the Multidimensional Body-Self Relations Scale (Cash, 2000), and higher levels of social appearance anxiety have been found in individuals with bulimia nervosa than in controls (Koskina, Van den Eynde, Meisel, Campbell, & Schmidt, 2011).,
Based on the available evidence, we conceptualize social appearance anxiety as a negative social evaluative fear that is distinct from fear of negative evaluation because it focuses specifically on fears of judgment based on appearance versus negative evaluation fears more generally. That is, we see social appearance anxiety as a specific type of fear of negative evaluation that requires measurement in its own right due to its greater specificity. We are not alone in hypothesizing that such concerns merit specific measurement and theory: Perceived flaws in appearance have been implicated as a possible core fear in social anxiety disorder (Moscovitch, 2009).
1.3. Social anxiety fears and disordered eating
It has been suggested that general fear of negative evaluation may link social anxiety disorder with the eating disorders (Bulik, Beidel, Duchmann, & Weltzin, 1991; Gilbert & Meyer, 2003; Gilbert & Meyer, 2005; VanderWal & Thomas, 2004; Wal, Gibbons, & Grazioso, 2008). However, other fears (e.g., fear of scrutiny) seen in social anxiety disorder have not been thoroughly examined in research regarding eating disorders. Researchers have found that fear of negative evaluation is a risk factor for bulimic symptoms over and above body dissatisfaction, pressure to be thin, thin-idealization, dietary restraint, and negative affect (Utschig, Presnell, Madeley, & Smits, 2010) and that overall social-evaluative fears are a risk factor for eating disorders (Schwalberg, Barlow, Alger, & Howard, 1992). Gilbert & Meyer (2003) tested the cross-sectional relationship between FNE, social comparison, and three measures of disordered eating from the EDI-2: Body dissatisfaction, drive for thinness, and bulimic symptoms. They found that FNE predicted drive for thinness over and above depression and social comparison, whereas social comparison predicted bulimic symptoms. Depression was the only significant predictor of body dissatisfaction. In a prospective design, Gilbert & Meyer (2005) found that FNE predicted bulimic attitudes over time. Wonderlich-Tierney and Vander Wal (2010) were the first (to the best of our knowledge) to examine both fear of negative evaluation and a combination of cognitive, affective, and somatic aspects of social anxiety. These researchers found that only fear of negative evaluation was directly associated with eating disorder symptoms. Although this study was a valuable first step, it did not test all relevant social anxiety constructs (e.g., social appearance anxiety, fear of scrutiny). It seems clear that further study of a wide-range of social anxiety domains is necessary to determine how social anxiety relates to eating disorders. This knowledge may lead to improved treatment (through more appropriate constructs to focus on in treatment) and better understanding of the risk factors for eating disorders.
Given the theorized central role of appearance fears in social anxiety disorder (Moscovitch, 2009) and the emphasis individuals with EDs place on appearance, it seems particularly plausible that social appearance anxiety may play a role in the relationship between social anxiety and eating disorders. To date, most research on appearance anxiety has focused on social physique anxiety (SPA) and has been measured using the Social Physique Anxiety Scale (SPAS; Hart, Leary, & Rejeski, 1989). SPA refers to concerns about one’s body form and structure (e.g., body fat, muscle tone, and general body proportions). The factor structure of the SPAS has undergone much scrutiny (e.g., Eklund, Mack, & Hart, 1996; Eklund, Kelley, & Wilson, 1997) and controversy over an acceptable factor structure remains (Eklund, 1998; Martin, Rejeski, Leary, McAuley, & Bane, 1997; Motl, Conroy, & Horan, 2000). Alternatively, social appearance anxiety is a domain of social anxiety encompassing all of one’s appearance (i.e., not limited to physique). SAA has been measured by the Social Appearance Anxiety Scale (SAAS; Hart, Flora, Palyo, Fresco, Holle & Heimberg, 2008), which has exhibited good factor structure, convergent, and divergent validity, and has been shown to predict state social anxiety experienced from an appearance evaluation, suggesting that the measure is a valid assessment of anxiety experienced from appearance evaluation in social situations (Hart et al., 2008; Levinson & Rodebaugh, 2011). Given the importance of features beyond physique in societal judgments of appearance (Grammer & Thornhill, 1994) and findings that social anxiety disorder is highly comorbid with eating disorders (Kaye et al., 2004), it seems likely that social appearance anxiety may be a missing link between social anxiety and eating disorders.
1.4. Two models of social anxiety and eating comorbidity
Furthermore, it is important to determine not only which social anxiety constructs relate to disordered eating but how social anxiety constructs confer risk. Pallister & Waller (2008) suggest two potential explanations for the high comorbidity between anxiety and eating disorders; (a) anxiety might be a risk factor for EDs or (b) the two kinds of disorders may have common shared vulnerabilities. However, to the best of our knowledge there has been no research examining social anxiety and eating disorder comorbidity in both a mediation model and vulnerability model.
Indeed, most previous studies in this area have used mediation terminology in conceptualizing the relationship between fear of negative evaluation, social anxiety, and eating disorder symptoms (e.g., Wonderlich-Tierney & Vander Wal, 2010), based largely on the assertion that anxiety disorders often precede the development of eating disorders (e.g., Kaye et al., 2004) and that fear of negative evaluation may be a connecting factor between the two disorders. A mediation model would suggest that social anxiety leads to fear of negative evaluation, which then leads to disordered eating. Though there are problems with a mediation model, it has been the most tested model of FNE, social anxiety, and disordered eating in current literature: Thus we test a mediation model here.
In the social anxiety literature, fear of negative evaluation is usually assumed to be primarily a cause of social anxiety symptoms, not primarily an effect as implied in a mediation model (e.g., Rapee & Heimberg, 1997). Available tests suggest that fear of negative evaluation can be construed as a form of vulnerability to social anxiety (e.g., Kotov, Watson, Robles, & Schmidt, 2007). Indeed, Pallister & Waller, (2008) propose both a mediation model and vulnerability model of anxiety and eating disorders, but argue that a vulnerability model may be most plausible given current conceptions of comorbidity that suggest there are overlapping risk factors, such as neuroticism and negative affect, that contribute to the high comorbidity rates between disorders (Hyman, 2003; Fyer & Brown, 2009; Klein, Lewinsohn, Rohde, Seeley, & Shankman, 2003; Wickramaratne & Weissman, 1993; Barlow, 2003; Clark, 2005). Thus, in the current study we tested both a mediation model and vulnerability model, though given previous research and theory a vulnerability model seems most plausible.
1.5. The current study
In the current study, we tested the relationship between the five social fears described above (social appearance anxiety, fear of positive evaluation, fear of negative evaluation, fear of scrutiny, and social interaction anxiety), and indicators of disordered eating (body dissatisfaction, bulimia, drive for thinness, weight concern, eating concern, shape concern, and restraint). We hypothesized that social appearance anxiety and fear of negative evaluation would be the social fears most related to disordered eating. We also evaluated two models of social anxiety, disordered eating, and negative social evaluation fears: (a) a mediation model; fear of negative evaluation and social appearance anxiety would mediate the relationship between components of social anxiety and disordered eating, and (b) a vulnerability model; social appearance anxiety and fear of negative evaluation would serve as vulnerabilities to both social anxiety and eating disorders. If the latter model is supported, it would provide evidence that fear of negative evaluation and social appearance anxiety are shared contributors to both social anxiety and disordered eating (rather than social anxiety causing fear of negative evaluation). We hypothesized that this model would have excellent fit. Additionally, in the following analyses we tested for effects of gender. However, because the literature suggests that risk factors for eating disorders (e.g. body dissatisfaction) do not differ based on gender (Jacobi et al., 2004), we did not restrict our sample to include only women.
2. Method
2.1. Participants
A total of 118 participants filled out a questionnaire packet to receive credit or extra credit as part of their coursework as undergraduates at a Midwestern metropolitan university. Participants were mostly white (n = 84; 71%) women (n = 73; 62%), with a mean age of 19.31 (SD = 1.20). Other ethnicities reported included Asian or Pacific Islander (n = 23; 20%) Black (n = 6; 5%), multiracial (n = 3; 3%), Hispanic (n = 1; 1%), and ethnicity not listed (n = 1; 1%). Participants’ scores on the social interaction anxiety measure (see below) ranged from very low to very high (Range = 1 to 61, M = 24.14). A total score of 34 or higher suggests probable social anxiety disorder (Heimberg, Mueller, Holt, Hope, & Liebowitz, 1992). Scores on disordered eating subscales ranged from very low to very high (Range = 0 to 32; M = 12.60).
2.2. Measures
2.2.1
The Social Appearance Anxiety Scale (SAAS; Hart, Flora, Palyo, Fresco, Holle, & Heimberg, 2008) is a 16-item measure developed to assess anxiety about being negatively evaluated by others because of one’s overall appearance, including body shape. Research on the psychometric properties of the SAAS demonstrated high test-retest reliability, good internal consistency, good factor validity, incremental validity (e.g., it was a unique predictor of social anxiety above and beyond negative body image indicators), and divergent validity (Hart et al., 2008; Levinson & Rodebaugh, 2011). Example items from the SAAS are I am concerned people would not like me because of the way I look, I get nervous when talking to people because of the way I look, I am afraid that people find me unattractive, and I am frequently afraid I would not meet others’ standards of how I should look. In the current study, the SAAS exhibited excellent internal consistency (α = .95).
2.2.2
The Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) is a 20-item measure designed to assess social interaction anxiety. The items describe anxiety-related reactions to a variety of social situations. Example items are I have difficulty talking with other people and I am tense mixing in a group. Overall, research on the scale suggests good to excellent reliability and good construct and convergent validity (see Heimberg & Turk, 2002, for a review). When used for statistical analyses, the three reverse-scored items are omitted here. Available evidence suggests that these items fail to load on the same factor as the other items (Rodebaugh, Woods, Heimberg, Liebowitz, & Schneier, 2006) and appear less related to social anxiety and more related to extraversion than is desirable (Rodebaugh, Woods, & Heimberg, 2007). Removal of the reverse-scored items has no discernible negative effects on the validity of the scale, and generally improves convergent validity (Rodebaugh, Woods, & Heimberg, 2007). In the current study, the straightforward items of the SIAS (S-SIAS) displayed excellent internal consistency (α = .91).
2.2.3
The Brief Fear of Negative Evaluation (BFNE; Leary, 1983) is a twelve item version of the original Fear of Negative Evaluation Scale (Watson & Friend, 1969). The items assess fear of negative evaluation, which has been theorized to be a central component of social anxiety. Example items are I am afraid others will not approve of me and I am usually worried about what kind of impression I am making on someone. The BFNE has been shown to correlate with other measures of social anxiety and has excellent psychometric properties when the four reverse scored items are excluded, as they are here (Rodebaugh et al., 2004). In the current sample the straightforward BFNE (S-BFNE) exhibited excellent internal consistency (α = .93).
2.2.4
Social Phobia Scale (SPS; Mattick & Clarke, 1998) is a 20-item scale designed to assess fear of scrutiny. Items ask about fears of being scrutinized during routine activities such as eating, drinking, or writing. Collectively, these types of fears comprise fear of scrutiny. Example items are I would get tense if I had to carry a tray across a crowded cafeteria and I become anxious if I have to write in front of other people. The SPS has been shown to have high levels of internal consistency, test-retest reliability, and to discriminate between individuals with social phobia and other disorders (i.e., agoraphobia, depression; Mattick & Clarke, 1998). In the current sample the SPS exhibited very good internal consistency (α = .89).
2.2.5
Fear of Positive Evaluation Scale (FPES; Weeks, Heimberg, & Rodebaugh, 2008) is a 10-item measure designed to assess fear of positive evaluation; two items are not scored in the total. Example items are I feel uneasy when I receive praise from authority figures and I generally feel uncomfortable when people give me compliments. The FPES has been shown to have excellent reliability, construct validity, and factorial validity (Weeks et al., 2008; Fergus, Valentiner, McGrath, Stephenson, & Jencius, 2009). In the current sample the FPES exhibited very good internal consistency (α = .85).
2.2.6
Eating Disorder Inventory-2 (EDI-2; Garner, Olmsted, & Polivy, 1983) is a 91-item self-report questionnaire designed to measure psychological features commonly associated with anorexia nervosa and bulimia nervosa. It has been shown to have good internal consistency and good convergent and discriminant validity (Garner et al., 1983) and is frequently used by clinicians for the assessment of eating disorder symptoms (Brookings & Wilson, 1994). Three of the eleven subscales were used for this study: The Drive for Thinness (DT), Body Dissatisfaction (BD), and Bulimia (B) subscales. Example items are I eat when I am upset and I think about dieting. These subscales were used because they assess major vulnerabilities for anorexia nervosa and bulimia nervosa and are the subscales of the measure that are most frequently used for this purpose. The DT subscale includes seven items which assess excessive concern with dieting, preoccupation with weight, and fear of gaining weight. The BD subscale includes nine items which assess dissatisfaction with overall body shape as well as the size of specific regions of the body, such as hips, stomach, and thighs. The B subscale includes seven items which assess bulimic behaviors such as binging and purging. In the current sample, body dissatisfaction (α = .91) exhibited excellent internal consistency and drive for thinness (α = .78) and bulimia (α = .77) exhibited good internal consistency.
2.2.7
Eating Disorder Examination-Q (EDE-Q: Fairburn & Beglin, 1994) is a questionnaire version of the Eating Disorder Examination semi-structured interview (Cooper & Fairburn, 1993) designed to assess cognitive and behavioral features of eating disorders. The EDE-Q has been shown to have good reliability and validity (Cooper & Fairburn, 1993; Luce & Crowther, 1999; Mond, Hay, Rodgers, Owen, & Beumont, 2004). It includes 41 items that are scored on a 7-point, forced-choice rating scheme that focuses on behaviors exhibited in the past 28 days. Example items are Have you had a definite desire for your stomach to be flat and Have you experienced a loss of control over eating? The four subscales of the EDE-Q and estimates of their internal consistency in the current sample are as follows: Restraint (α =.80), Eating Concern (α = .77), Weight Concern (α = .77), and Shape Concern (α = .89).
2.3. Procedure
Participants completed the above measures as part of a study that also examined the psychometric factors of the Social Appearance Anxiety Scale (Levinson & Rodebaugh, 2011); relationships between the SAAS and eating disorder symptomatology were not reported in that study. Tests of indirect effects (i.e., mediation) were conducted using bootstrapping in the Mplus program Version 5.21 (Muthén & Muthén, 1998–2009). As recommended by Hayes (2009), 5000 draws were implemented. For Figures 1 and 2 and for fit indices the maximum likelihood estimator in the Mplus program was used to report standardized path estimates. Model fit was evaluated using the: (a) comparative fit index (CFI; Bentler, 1990), (b) Tucker-Lewis incremental fit index (TLI; Tucker & Lewis, 1973), (c) root mean square error of approximation (RMSEA; Steiger & Lind, 1980), and (d) standardized root mean square residual (SRMR; Bentler, 1990; Jöreskog & Sörbom, 1981). The magnitudes of these indices were evaluated with the aid of recommendations by Hu and Bentler (1999). Essentially, for the CFI and TLI, values of .90 and above were considered adequate, whereas values of .95 or above were considered very good; for the RMSEA and SRMR, values of .08 and below were considered adequate and .05 or less very good. However, for samples of less than 200 cases, RMSEA has been found to be an underestimate of model fit (i.e., it inappropriately rejects models at lower sample sizes that it would accept at higher sample sizes; Curran, Bollen, Chen, Paxton, & Kirby, 2003).
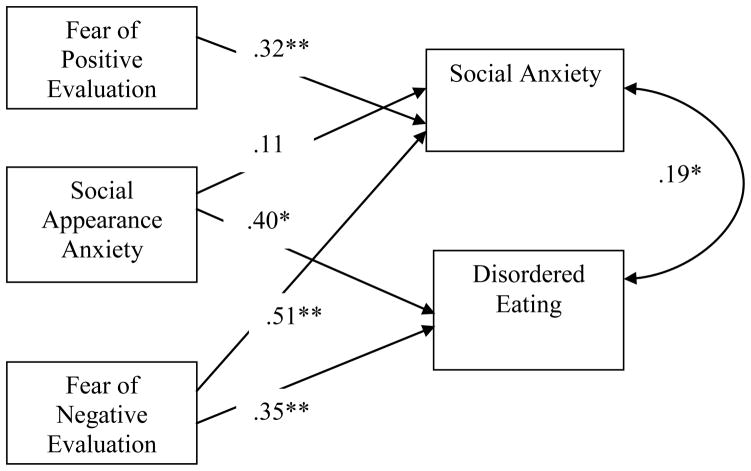
Figure 1.
Model of the relationship between social anxiety, social appearance anxiety, fear of negative evaluation, and disordered eating. Social anxiety is a composite of the S-SIAS and SPS. Disordered eating is a composite of three subscales from the EDI-2 and four subscales from the EDE-Q. The first path between social anxiety and disordered eating is before social appearance anxiety and fear of negative evaluation are added. The second path is with social appearance anxiety and fear of negative evaluation in the model. Standardized Coefficients are shown. ** p < .01, * p <.05.
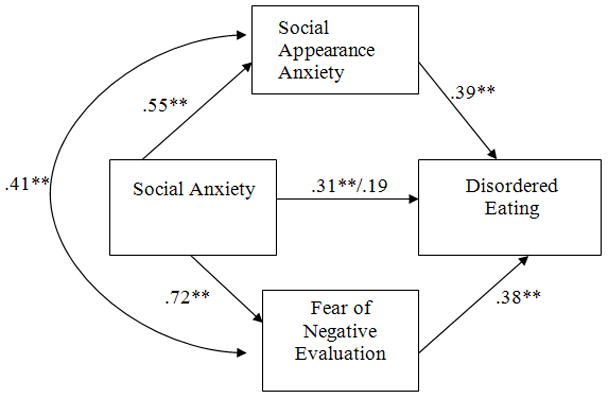
Figure 2.
Model of the relationship between fear of positive evaluation, social appearance anxiety, fear of negative evaluation, social anxiety, and disordered eating. Social anxiety is a composite of the SIAS and SPS. Disordered eating is a composite of three subscales from the EDI-2 and four subscales from the EDE-Q. Standardized Coefficients are shown. ** p < .01, * p <.05.
To test if a mediation model or vulnerability model exhibited better fit, we evaluated comparative model fit using the Information Criterion proposed by Akaike (AIC; Akaike, 1974) and the Bayesian Information Criterion (BIC; Schwarz, 1978). We used these statistics because it was not always possible to use nested chi-square tests to test the two models. Despite having different theoretical bases, both statistics are designed to quantify how well a model approximates the theoretically best model for the data (Kuha, 2004). We used both indices together (as recommended by Kuha, 2004). The rationale for using both statistics is that it is unlikely that both indices are incorrect when they agree on which model should be selected. Lower values of both indices are preferred, with no absolute metric to determine good fit with either index (i.e., they are to be used comparatively).
3. Results
3.1. Zero-order Correlations
Table 1 shows the zero-order correlations between the five domains of social anxiety, measures of disordered eating from the EDI-2 (BD, DT, B), and four subscales of the EDE-Q. As can be seen in Table 1, all of the domains of social anxiety were significantly correlated with the EDI-2 measures with the exception of the relationship between drive for thinness and fear of positive evaluation. Social appearance anxiety, fear of negative evaluation, and fear of positive evaluation were the only domains of social anxiety that were significantly correlated with all four subscales of the EDE-Q.
Table 1.
Correlations between Domains of Social Anxiety, EDI-2, and EDE-Q
| SAAS | S-SIAS | S-BFNE | SPS | FPES | DT | BD | Bulimia | SC | WC | EC | Restraint | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SAAS | .95 | |||||||||||
| S-SIAS | .53* | .91 | ||||||||||
| S-BFNE | .64** | .65** | .93 | |||||||||
| SPS | .50** | .71** | .68** | .89 | ||||||||
| FPES | .36** | .46** | .41** | .57** | .85 | |||||||
| DT | .36** | .19* | .42** | .27** | .18 | .78 | ||||||
| BD | .58** | .38** | .42** | .30** | .35** | .47** | .91 | |||||
| Bulimia | .40** | .26* | .36** | .21* | .27* | .50** | .56** | .77 | ||||
| SC | .54** | .30** | .48** | .36** | .33** | .83** | .70** | .62** | .89 | |||
| WC | .31** | .28** | .33** | .33** | .31** | .80** | .63** | .70** | .91** | .77 | ||
| EC | .44** | .20* | .42** | .18 | .19* | .67** | .60** | .74** | .82** | .82** | .77 | |
| Restraint | .31** | .14 | .36** | .18* | .23* | .75** | .41** | .57** | .72** | .76** | .70** | .80 |
Note. SAAS= Social Appearance Anxiety Scale; S-SIAS = Straightforward Social Interaction Anxiety Scale; S-BFNE = Straightforward Brief Fear of Negative Evaluation scale; SPS = Social Phobia Scale; FPES = Fear of Positive Evaluation Scale; DT = Drive for Thinness; BD = Body Dissatisfaction; SC = Shape Concern; WC = Weight Concern; EC = Eating Concern. The diagonal value is Cronbach’s alpha.
p < .001;
p < .05
3.2. Multiple Regression Analyses
Given the substantial intercorrelations noted above, we turned to simultaneous multiple regression to test which variables had unique relationships. First, we combined all seven facets of eating disorder vulnerability into an overall disordered eating composite to test the omnibus effect on disordered eating for each of the social anxiety measures. We then tested for more specific effects for the individual measures related to disordered eating. This process is analogous to conducting a MANOVA with a series of follow up ANOVAs. To create a measure of disordered eating, we standardized and summed each subscale measuring a form of disordered eating.1 This composite measure of disordered eating had excellent internal consistency (α = .93). We then entered each of the five social anxiety-related predictors and gender into multiple regression to test which social anxiety domains significantly predicted disordered eating. Multiple regression revealed that social appearance anxiety (part r = .31, p = .001), fear of negative evaluation (part r = .28, p = .004), and gender (part r = .44, p < .001) significantly predicted disordered eating over and above social interaction anxiety (part r = −.07, p = .495), fear of scrutiny (part r = −.15, p = .121) and fear of positive evaluation (part r = .15, p = .134). There were no significant interactions between gender and the social anxiety measures predicting disordered eating (all ps > .26). Next, to test which domains of social anxiety related to each specific component of disordered eating we conducted follow up tests for each of the seven components.
In each regression we entered all five of the domains of social anxiety as the independent variables; these were centered to avoid multicollinearity. We used seven separate regressions to test each measure of disordered eating as the dependent variable.2 As can be seen in Table 2, social appearance anxiety was the only significant predictor of body dissatisfaction and bulimia. Additionally, social appearance anxiety significantly predicted weight, shape, and eating concerns. Fear of negative evaluation significantly predicted five out of the seven eating disorder vulnerabilities (with the exception of body dissatisfaction and bulimia). No other domain of social anxiety was a significant predictor of any type of disordered eating.3
Table 2.
Part Correlations for Social Anxiety Predicting Eating Disorder Vulnerabilities
| BD | DT | B | WC | SC | EC | Restraint | |
|---|---|---|---|---|---|---|---|
| SAAS | .43** | .18 | .21* | .33** | .35** | .27* | .13 |
| S-BFNE | .07 | .28* | .19 | .26* | .21* | .28* | .29* |
| FPE | .17 | .01 | .15 | .14 | .12 | .07 | .14 |
| S-SIAS | .07 | −.16 | .02 | −.17 | −.12 | −.09 | −.15 |
| SPS | −14 | .03 | −.14 | −.01 | .02 | −.15 | −.08 |
Note. SAAS = Social Appearance Anxiety Scale; S-BFNE = Brief Fear of Negative Evaluation Scale; FPE = Fear of Positive Evaluation; S-SIAS = Social Interaction Scale; SPS = Social Phobia Scale; BD = Body Dissatisfaction; DT = Drive for Thinness; B = Bulimia; WC = Weight Concern; SC = Shape Concern; EC = Eating Concern.
p < .001;
p < .05.
3.3. Structural Equation Models
We tested two models exploring the relationship between social appearance anxiety, disordered eating, and constructs related to social anxiety. First, and in keeping with typical tests in the literature regarding fear of negative evaluation (VanderWal & Thomas, 2004; VanderWal, Gibbons, & Grazioso, 2008), we tested if the relationship between social anxiety and disordered eating was mediated by social appearance anxiety and fear of negative evaluation. To create a composite of components of social anxiety we standardized and added the scores from the SIAS and SPS. We decided to use this method because composite measures provide a more reliable estimate of the construct (Zeller & Carmines, 1980). Additionally, a composite measure can simplify the number of analyses conducted; this method has been used in previous social anxiety literature (Clark et al., 2003; Clark et al., 2006). Internal consistency was very good (α = .86) for the social anxiety composite. We then tested if the relationship between social anxiety and the composite of disordered eating was mediated by social appearance anxiety and fear of negative evaluation, with social appearance anxiety and fear of negative evaluation permitted to correlate. Mediation analyses indicated that both social appearance anxiety and fear of negative evaluation carried the indirect effects of social anxiety on disordered eating. The 95% confidence interval for the indirect effects carried by social appearance anxiety was .060 to .286. The 95% confidence interval for the indirect effects carried by fear of negative evaluation was .094 to .513. Because this confidence interval did not include 0, these indirect effects were statistically significant at p < .05.
Figure 1 shows the relationship between social anxiety, disordered eating, fear of negative evaluation, and social appearance anxiety presented in a mediation model. As can be seen in Figure 1, the relationship between social anxiety symptoms and disordered eating was no longer significant when social appearance anxiety and fear of negative evaluation were included in the model. Model fit for this model was saturated (i.e., there were no degrees of freedom remaining) and thus fit perfectly by definition. When the relationship between social anxiety and disordered eating was removed fit ranged from adequate to excellent (CFI = .99, TLI = .95. RMSEA= .11, SRMR = .02).
Notably, the above fit indices are based on a model in which fear of negative evaluation and social appearance anxiety are correlated. The inclusion of this correlation is questionable because the model is based on the assumption that social anxiety produces both evaluation fears; therefore, the paths from social anxiety to the evaluation fears should account for any relationship between the variables. However, when we removed the correlation from the model, fit ranged from unacceptable to borderline adequate (CFI = .89, TLI = .33, RMSEA = .42, SRMR = .07). Further, an alternative model, in which disordered eating was the independent variable, social anxiety symptoms was the dependent variable, and social appearance anxiety mediated their relationship, suggested that the indirect effect was again statistically significant at p < .05. However, based on theory and previous research that has found that anxiety proceeds development of eating disorders (Kaye et al., 2004) we do not emphasize this model.
Next, we tested a model in which fear of negative evaluation and social appearance anxiety were vulnerabilities for both social anxiety and eating disorders and fear of positive evaluation was a vulnerability for social anxiety alone (without correlations between social appearance anxiety, fear of positive evaluation, and fear of negative evaluation). We included fear of positive evaluation because it is theorized to act on the same level as fear of negative evaluation and thus might also serve as a vulnerability for social anxiety. Notably, however, it was not uniquely related to disordered eating in these analyses, leading to the expectation that a path between fear of positive evaluation and disordered eating would not be required in this model. Model fit indices were excellent (CFI = 1.0, TLI = 1.0, RMSEA = .01, SRMR = .02). Figure 2 shows the proposed model. Notably, when correlations between the three vulnerabilities were included, there were no changes to model fit.
We also tested a model of vulnerability that did not include fear of positive evaluation so that we could compare the mediation model to the vulnerability model (i.e., this comparison can only be made when the same variables are in the model). This model exhibited excellent fit (CFI = 1.00, TLI = 1.00, RMSEA = 0.00, SRMR = 0.00), which did not change when a correlation between fear of negative evaluation and fear of positive evaluation was added; we therefore compared the vulnerability model without that correlation. We used a chi-square difference test to compare the correlated mediation model and the vulnerability model without fear of positive evaluation (Δχ2(5) = .103, n = 110, p = .999). A nonsignificant chi-square value indicates that the more constrained (and therefore parsimonious) model (i.e., the vulnerability model) is preferred because it does not result in a significant decrease in model fit. We also used the AIC and BIC to compare the mediation model to this model of vulnerability. Values were as follows: Mediation model with correlation (AIC = 2233.478, BIC = 2266.417); mediation model without correlation (AIC = 2253.124; BIC = 2283.318); vulnerability model (AIC = 1067.712, BIC = 1092.648). Both the AIC and BIC suggest that the vulnerability model is preferred as a model of the underlying data (i.e., lower values suggest better fit).
4. Discussion
In support of previous research (Bulik et al., 1991; Wonderlich-Tierney & Vander Wal, 2010; Utschig et al., 2010), we found that fear of negative evaluation was able to predict a composite of disordered eating over and above fear of scrutiny, fear of positive evaluation, and social interaction anxiety. Additionally, fear of negative evaluation predicted five of the seven components of disordered eating (with the exception of body dissatisfaction and bulimia). We also found that social appearance anxiety is an additional domain of social anxiety that correlates with disordered eating.
Social appearance anxiety was able to explain additional variance in the disordered eating composite (in addition to FNE) over and above the other three domains of social anxiety we tested. Social appearance anxiety, along with fear of negative evaluation, predicted a significant amount of variance in weight concern, shape concern, and eating concern. Additionally, social appearance anxiety (but not FNE) had a unique relationship with body dissatisfaction and bulimia. Previous research has found that body dissatisfaction is a major risk factor for eating disorders, especially bulimia nervosa (Attie & Brooks-Gunn, 1989; Killen et al., 1996; Stice & Shaw, 2002) and that body dissatisfaction may be the prodomal stage of development of an eating disorder (Stice, Ng, Shaw, 2010). Our results, combined with this previous research, suggest that elevated social appearance anxiety may be a risk factor for development of eating disorders (perhaps specifically bulimia nervosa)4 through increased body dissatisfaction, whereas fear of negative evaluation may be a risk factor for anorexia nervosa (in addition to bulimia nervosa).
Additionally, we found support for two models linking social appearance anxiety with disordered eating. However, we found that the best fitting model was a model of vulnerability. First, we found that social appearance anxiety and fear of negative evaluation mediated the relationship between social anxiety symptoms and disordered eating. Indeed, the variance shared between the social anxiety symptom composite and the disordered eating composite was no longer significant when social appearance anxiety and fear of negative evaluation were considered. If this model holds in longitudinal data social anxiety may cause individuals to experience anxiety over their appearance. This appearance anxiety may cause individuals to become concerned about their overall appearance, including body image, and seek out methods to avoid their anxiety through appearance change. One way that this may manifest itself is through disordered eating. Thus, it is possible that social anxiety may cause social appearance anxiety which may, in turn, cause individuals to develop disordered eating habits. However, our data is cross sectional and causality cannot be firmly established.
We also found support for an alternative model in which both social appearance anxiety and fear of negative evaluation are vulnerabilities for social anxiety and eating disorders. We suggest that fear of negative evaluation and social appearance anxiety may be vulnerabilities that lead individuals to experience either eating or social anxiety disorders (or potentially both). We emphasize the plausibility of the vulnerability model because previous research and theory has supported fear of negative evaluation as a vulnerability for social anxiety (Haikal & Hong, 2010; Rapee & Heimberg, 1997). In a comparison between the two models, we found that a comparable vulnerability model was more parsimonious than the mediation model by all available indices (AIC, BIC, and chi-square difference test). This result suggests that a vulnerability model should be preferred over a mediation model based on our data. Further, when the correlation between fear of negative evaluation and social appearance anxiety was removed the mediation model did not have good fit. We argue that, in a mediation model based upon cross-sectional data, it should not be necessary for these fears to be correlated. That is, if social anxiety produces both fears (and all constructs are measured at the same time point), there should not be any shared variability remaining in the fears of evaluation. However, in a vulnerability model a correlation between the vulnerabilities was irrelevant to model fit, despite the fact that a correlation would actually be plausible in this case.
Of course, additional tests with data that can support causal inference are required (e.g., longitudinal data). Additionally, in our model we found a significant path from SAA to disordered eating but not social anxiety and a significant path from FPE to social anxiety but not disordered eating. We suggest two potential explanations for this result: (a) the path from SAA to social anxiety may be small but could attain significance in larger samples with greater power or (b) it may be that SAA confers no unique vulnerability for social anxiety symptoms above and beyond fears of evaluation, whereas it does confer unique vulnerability for disordered eating above such fears. Conversely, fear of positive evaluation may confer unique vulnerability for social anxiety but not disordered eating. Future research is needed to test these explanations. Regardless of the results of such tests, we encourage future longitudinal research exploring what additional factors lead certain individuals to develop a particular type of psychopathology (i.e., eating, social anxiety, or both). It may be that social appearance anxiety and fear of negative evaluation interact with other variables (i.e., having negative experiences with body image versus social interactions) to lead to a particular type of disorder.
Of course, the current study is not without limitations. We had a modest sample size that consisted of students. Future research should test if the results found here generalize to larger samples, as well as other populations and cultures. Additionally, one of the major limitations of this study is that our data was cross sectional and causality cannot be clearly determined. Therefore, it is crucial that future longitudinal work more stringently test the directionality of the models presented here. However, we think that as a cross-sectional research was an important first step in understanding negative social evaluation fears, social anxiety, and disordered eating. An additional limitation is that we measured social anxiety with self-report alone. It might be argued that an interview measure, such as the Liebowitz Social Anxiety Scale, would have been preferable. However, available research indicates that the interview and self-report versions of the Liebowitz Social Anxiety Scale correlate very highly (Fresco et al., 2001), suggesting that social anxiety may be as fruitfully assessed with self-report as interview measures. Nevertheless, future research should test the relationship of social anxiety accessed via a variety of modalities with facets of disordered eating, also assessed via a variety of modalities. Finally, it should be noted that we did not test whether social physique anxiety has any incremental contributions in our model. Given problems with the factor structure of the SPAS (Eklund, Mack, & Hart, 1996; Eklund, Kelley, & Wilson, 1997; Eklund, 1998; Martin, Rejeski, Leary, McAuley, & Bane, 1997; Motl, Conroy, & Horan, 2000) and that SPA concentrates only on physique (height, weight, and muscle tone), rather than other aspects of appearance in addition to body shape (i.e., complexion and shape and size of facial features) we chose to focus on how overall social appearance anxiety affects disordered eating. However, we encourage future research to examine how both social appearance and social physique anxiety affect eating disorder symptoms and if the two constructs show interactive effects in predicting psychopathological variables.
Nevertheless, we believe that these results have implications for the treatment of both social anxiety and eating disorders. Exposure therapy is an efficacious treatment for social anxiety disorder (Gould, Buckminster, Pollack, Otto, & Yap, 1997; Feske & Chambless, 1995). Development of exposure therapy that targets social appearance anxiety may decrease levels of social appearance anxiety and prevent development of eating disorders. For example, with therapist assistance, clients could talk with a confederate about a particular part of their appearance that makes them anxious (but which is judged by the clinician to be unlikely to be of concern to others). This in-session exposure would ideally be followed by in vivo exposures in which clients repeat the procedure with people in their lives. Such exposures hold the promise of demonstrating to a client that his or her appearance is unlikely to lead to rejection. Additionally, such exposures could be integrated into current efficient treatments for eating disorders (please see Wilson, 2010).
Future research should explore such treatment options in addition to continued investigation of the plausible proposition that social anxiety leads to eating disorders and/or that both disorders share common vulnerabilities. We believe that the research presented here is a step towards understanding negative social evaluation fears as an important component of social anxiety and eating disorder comorbidity. Further examination of social appearance anxiety and fear of negative evaluation can help inform our understanding of the development of eating disorders and the treatment of individuals with comorbid social anxiety and eating disorders.
Highlights.
Social appearance anxiety predicted disordered eating over and above other social anxiety constructs
Fear of negative evaluation uniquely predicted drive for thinness and restraint
These social evaluation fears may be vulnerabilities for both social anxiety and eating disorders
Acknowledgments
Role of Funding Sources
We have no financial interests to declare in regard to this research.
We acknowledge Reuben Karchem and Alison Cohn for their research assistance. Additionally, we would like to thank Andrea Kass and Juliette McClendon for their helpful comments on a previous draft.
Footnotes
Due to limited power and the large number of analyses we chose not to examine gender in each of the follow-up tests. However, we tested if the interaction between the two significant social anxiety domains (fear of negative evaluation and social appearance anxiety) and gender interacted to predict any of the outcome variables. There were no significant interactions (all ps > .12).
When the composite of disordered eating was conceptualized as only consisting of the Restraint subscale from the EDE-Q and the Bulimia scale from the EDI-2 the results of the mediation model and vulnerability model were unchanged. The results also did not change when disordered eating was conceptualized as the four disordered eating scales (restraint, bulimia, drive for thinness, and body dissatisfaction) that did not include the concern scales (in case of any artificial inflation from overlap between concern and anxiety scales).
When depression (as measured by the Beck Depression Inventory 2; Beck, Steer, & Brown; 1996) is included in all multiple regression analyses the results for SAAS and FNE remained unchanged.
When SAAS was not included in the regression equation (SIAS, SPS, BFNE, and FPE) predicting bulimic symptoms, the BFNE was the only significant predictor of bulimic symptoms (part r = .29, p = .006). This result is consistent with findings from Utschig et al., (2010). The result when the SAAS was included in the model suggests that SAAS is a better predictor of bulimic symptoms than general BFNE.
Conflict of Interest
We have no conflict of interest to declare in regard to this research.
Contributors
Example: Cheri A. Levinson designed the study, wrote the protocol, conducted literature reviews, conducted the statistical analysis, and wrote the first draft of the manuscript. Thomas L. Rodebaugh provided support and assistance on all aspects of the manuscript. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- Attie I, Brooks-Gunn J. Development of eating problems in adolescent girls: A longitudinal study. Developmental Psychology. 1989;25:70–79. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guiliford; 2003. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brewerton TD, Lydiard RB, Herzog DB, Brotman AW. Comorbidity of Axis I psychiatric disorders in bulimia nervosa. Journal of Clinical Psychiatry. 1995;56:77–80. [PubMed] [Google Scholar]
- Brookings JB, Wilson JF. Personality and family-environment predictors of self-reported eating attitudes and behaviors. Journal of Personality Assessment. 1994;63:313–326. doi: 10.1207/s15327752jpa6302_10. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Silgado J, Lewinsohn PM. Delineation of differential temporal relations between specific eating and anxiety disorders. Journal of Psychiatric Research. 2010;44:781–787. doi: 10.1016/j.jpsychires.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: A controlled study. Acta Psychiatrica Scandinavica. 1997;96:101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Beidel DC, Duchmann E, Weltzin TE. An analysis of social anxiety in anorexic, bulimic, social phobic, and control women. Journal of Psychopathology and Behavioral Assessment. 1991;13:199–211. [Google Scholar]
- Cash TF, Szymanski ML. The development and validation of the Body-Image Ideals Questionnaire. Journal of Personality Assessment. 1995;64:466–477. doi: 10.1207/s15327752jpa6403_6. [DOI] [PubMed] [Google Scholar]
- Cash TF, Labarge AS. Development of the Appearance Schemas Inventory: A new cognitive body-image assessment. Cognitive Therapy and Research. 1996;20:37–50. [Google Scholar]
- Cash TF. Unpublished manuscript. Old Dominion University; Norfolk, VA: 2000. Users manual for the Multidimensional Body-Self Relations Questionnaire. [Google Scholar]
- Clark L. Temperament as a Unifying Basis for Personality and Psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, Hackmann A, McManus F, Fennell M, Grey N, …Wild J. Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:568–578. doi: 10.1037/0022-006X.74.3.568. [DOI] [PubMed] [Google Scholar]
- Clark DM, Ehlers A, McManus F, Hackman A, Fennell M, Campbell H, …Louis B. Cognitive therapy versus fluoxetine in generalized social phobia: A randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology. 2003;71:1058–1067. doi: 10.1037/0022-006X.71.6.1058. [DOI] [PubMed] [Google Scholar]
- Cooper MJ, Fairburn CG. Demographic and clinical correlates of selective information-processing in patients with bulimia-nervosa. International Journal of Eating Disorders. 1993;13:109–116. doi: 10.1002/1098-108x(199301)13:1<109::aid-eat2260130113>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bollen KA, Chen F, Paxton P, Kirby JB. Finite Sampling Properties of the Point Estimates and Confidence Intervals of the RMSEA. Sociological Methods & Research. 2003;32(2):208–252. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) San Antonio, TX: The Psychological Corporation; 1994. [Google Scholar]
- Eklund RC. With regard to the Social Physique Scale (conceptually speaking) Journal of Sport & Exercise Psychology. 1998;20:225–227. [Google Scholar]
- Eklund RC, Mack D, Hart E. Factorial validity of the Social Physique Anxiety Scale for females. Journal of Sport and Exercise Psychology. 1996;18:281–295. [Google Scholar]
- Eklund RC, Kelley BC, Wilson P. The Social Physique Anxiety Scale: Men, women, and the effects of modifying item 2. Journal of Sport and Exercise Psychology. 1997;19:188–196. [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;26:695–720. [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Leibowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2001;31:1025–1035. doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Fyer AJ, Brown TA. Stress-induced and fear circuitry disorders: Advancing the research agenda for DSM-V [e-book] Arlington, VA US: American Psychiatric Publishing, Inc; 2009. Stress-induced and fear circuitry anxiety disorders: Are they a distinct group? pp. 125–135. [Google Scholar]
- Garner DM, Olmsted MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–19. [Google Scholar]
- Gluck ME, Geliebter A, Hung J, Yahav E. Cortisol, Hunger, and Desire to Binge Eat Following a Cold Stress Test in Obese Women with Binge Eating Disorder. Psychosomatic Medicine. 2004;66:876–881. doi: 10.1097/01.psy.0000143637.63508.47. [DOI] [PubMed] [Google Scholar]
- Gilbert N, Meyer C. Social anxiety and social comparison: Differential links with restrictive and bulimic attitudes among nonclinical women. Eating Behaviors. 2003;4:257–264. doi: 10.1016/S1471-0153(03)00026-6. [DOI] [PubMed] [Google Scholar]
- Gilbert N, Meyer C. Fear of negative evaluation and the development of eating psychopathology: A longitudinal study among nonclinical women. International Journal of Eating Disorders. 2005;37:307–312. doi: 10.1002/eat.20105. [DOI] [PubMed] [Google Scholar]
- Godart NT, Flament MF, Lecrubier Y, Jeammet P. Anxiety disorders in anorexia nervosa and bulima nervosa: Co-morbidity and chronology of appearance. European Psychiatry. 2000;15:38–45. doi: 10.1016/s0924-9338(00)00212-1. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fitzgibbon ML. Social anxiety as a barrier to treatment for eating disorders. International Journal of Eating Disorders. 2002;32:103–106. doi: 10.1002/eat.10051. [DOI] [PubMed] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4:291–306. [Google Scholar]
- Grammer K, Thornhill R. Human (Homo sapiens) facial attractiveness and sexual selection: The role of symmetry and averageness. Journal of Comparative Psychology. 1994;108:233–242. doi: 10.1037/0735-7036.108.3.233. [DOI] [PubMed] [Google Scholar]
- Greeno CG, Wing RR. Stress-induced eating. Psychological Bulletin. 1994;115:444–464. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- Haikal M, Hong RY. The effects of social evaluation and looming threat on self-attentional biases and social anxiety. Journal of Anxiety Disorders. 2010;24:345–352. doi: 10.1016/j.janxdis.2010.01.007. [DOI] [PubMed] [Google Scholar]
- Halmi KA, Eckert E, Marchi P, Sampugnaro V. Comorbidity of psychiatric diagnoses in anorexia nervosa. Archives of General Psychiatry. 1991;48:712–718. doi: 10.1001/archpsyc.1991.01810320036006. [DOI] [PubMed] [Google Scholar]
- Hart TA, Flora DB, Palyo SA, Fresco DM, Holle C, Heimberg RG. Development and examination of the Social Appearance Anxiety Scale. Assessment. 2008;15:48–59. doi: 10.1177/1073191107306673. [DOI] [PubMed] [Google Scholar]
- Hart EA, Leary MR, Rejeski W. The measurement of social physique anxiety. Journal of Sport & Exercise Psychology. 1989;11:94–104. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Heimberg RG, Mueller GP, Holt CS, Hope DA, Liebowitz MR. Assessment of anxiety in social interaction and being observed by others: The Social Interaction Anxiety Scale and the Social Phobia Scale. Behavior Therapy. 1992;23:53–73. [Google Scholar]
- Heimberg RG, Turk CL. Assessment of social phobia. In: Heimberg RG, Becker E, editors. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York, NY: Guilford Press; 2002. pp. 107–126. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hyman SE. Foreward. In: Philips KA, First MB, Pincus HA, editors. Advancing DSM: Dilemmas in Psychiatric Diagnosis. Washington, DC: American Psychiatric Association; 2003. [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras W. Coming to Terms With Risk Factors for Eating Disorders: Application of Risk Terminology and Suggestions for a General Taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG. Statistical estimation of structural models in longitudinal-developmental investigations. In: Nesselroade JR, Baltes PB, editors. Longitudinal research in the study of behavior and development. New York: Academic Press; 1979. pp. 303–374. [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of Anxiety Disorders with Anorexia and Bulimia Nervosa. The American Journal of Psychiatry. 2004;161:2215–2221. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: A 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde PP, Seeley JR, Shankman SS. Family study of co-morbidity between major depressive disorder and anxiety disorders. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2003;33:703–714. doi: 10.1017/s0033291703007487. [DOI] [PubMed] [Google Scholar]
- Koskina A, Van den Eynde F, Meisel S, Campbell IC, Schmidt U. Social appearance anxiety and Bulimia Nervosa. Eating and Weight Disorders. 2011 doi: 10.1007/BF03325321. manuscript in press. [DOI] [PubMed] [Google Scholar]
- Kotov R, Watson D, Robles JP, Schmidt NB. Personality traits and anxiety symptoms: The multilevel trait predictor model. Behaviour Research and Therapy. 2007;45:1485–1503. doi: 10.1016/j.brat.2006.11.011. [DOI] [PubMed] [Google Scholar]
- Kuha J. AIC and BIC: Comparisons of assumptions and performance. Sociological Methods & Research. 2004;33:188–229. [Google Scholar]
- Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Levinson CA, Rodebaugh TL. Validation of the Social Appearance Anxiety Scale: Factor, Convergent, and Divergent Validity. Assessment. 2011;18:350–357. doi: 10.1177/1073191111404808. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Luce KH, Crowther JH. The reliability of the Eating Disorder Examination- self-report questionnaire version (EDE-Q) International Journal of Eating Disorders. 1999;25:349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Martin KA, Rejeski WJ, Leary MR, McAuley E, Bane S. Is the Social Physique Anxiety Scale really multidimensional? Conceptual and statistical arguments for a unidimensional model. Journal of Sport & Exercise Psychology. 1997;19:359–367. [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Motl RW, Conroy DE, Horan PM. The Social Physique Anxiety Scale: An example of the potential consequence of negatively worded items in factorial validity studies. Journal of Applied Measurement. 2000;1:327–345. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5. Los Angeles, CA: Muthén & Muthén; 1998–2009. [Google Scholar]
- Mond J, Hay P, Rodgers B, Owen C, Beumont P. Beliefs of women concerning causes and risk factors for bulimia nervosa. Australian and New Zealand Journal of Psychiatry. 2004;38:463–469. doi: 10.1080/j.1440-1614.2004.01384.x. [DOI] [PubMed] [Google Scholar]
- Moscovitch DA. What is the core fear in social phobia?: A new model to facilitate individualized case conceptualization and treatment. Cognitive and Behavioral Practice. 2009;16:123–134. [Google Scholar]
- Oliver G, Wardle J. Perceived effects of stress on food choice. Physiology & Behavior. 1999;66:511–515. doi: 10.1016/s0031-9384(98)00322-9. [DOI] [PubMed] [Google Scholar]
- Pallister E, Waller G. Anxiety in the eating disorders: Understanding the overlap. Clinical Psychology Review. 2008;28:366–386. doi: 10.1016/j.cpr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35:741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Rieger E, Van Buren D, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley D. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. Clinical Psychology Review. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG. The reverse of social anxiety is not always the opposite: The reverse-scored items of the Social Interaction Anxiety Scale do not belong. Behavior Therapy. 2007;38:192–206. doi: 10.1016/j.beth.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Heimberg RG, Liebowitz MR, Schneier FR. The factor structure and screening utility of the Social Interaction Anxiety Scale. Psychological Assessment. 2006;18:231–237. doi: 10.1037/1040-3590.18.2.231. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu W, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2008;38:15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwalberg MD, Barlow DH, Alger SA, Howard LJ. Comparison of bulimics, obese binge eaters, social phobics, and individuals with panic disorder on comorbidity across DSM-III-R anxiety disorders. Journal of Abnormal Psychology. 1992;101:675–681. doi: 10.1037//0021-843x.101.4.675. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Steiger JH, Lind JC. Annual Spring Meeting of the Psychometric Society. Iowa City, Iowa; 1980. Statistically-based tests for the number of factors. [Google Scholar]
- Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of Psychosomatic Research. 2002;53:985–993. doi: 10.1016/s0022-3999(02)00488-9. [DOI] [PubMed] [Google Scholar]
- Stice E, Ng J, Shaw H. Risk factors and prodromal eating pathology. Journal of Child Psychology and Psychiatry. 2010;51:518–525. doi: 10.1111/j.1469-7610.2010.02212.x. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Utschig AC, Presnell K, Madeley M, Smits JJ. An investigation of the relationship between fear of negative evaluation and bulimic psychopathology. Eating Behaviors. 2010;11:231–238. doi: 10.1016/j.eatbeh.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Vander Wal JS, Thomas N. Predictors of body image dissatisfaction and disturbed eating attitudes and behaviors in African American and Hispanic girls. Eating Behaviors. 2004;5:291–301. doi: 10.1016/j.eatbeh.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Wal JS, Gibbons JL, Grazioso M. The sociocultural model of eating disorder development: Application to a Guatemalan sample. Eating Behaviors. 2008;9:277–284. doi: 10.1016/j.eatbeh.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Watson D, Friend R. Measurement of social-evaluative anxiety. Journal of Consulting and Clinical Psychology. 1969;33:448–457. doi: 10.1037/h0027806. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Rodebaugh TL. The Fear of Positive Evaluation Scale: Assessing a proposed cognitive component of social anxiety. Journal of Anxiety Disorders. 2008;22:44–55. doi: 10.1016/j.janxdis.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Wickramaratne PJ, Weissman MM. Using family studies to understand comorbidity. European Archives of Psychiatry and Clinical Neuroscience. 1993;243:150–157. doi: 10.1007/BF02190721. [DOI] [PubMed] [Google Scholar]
- Wilson TG. The Oxford handbook of eating disorders. New York, NY US: Oxford University Press; 2010. Cognitive behavioral therapy for eating disorders; pp. 331–347. [Google Scholar]
- Wonderlich-Tierney AL, Vander Wal JS. The effects of social support and coping on the relationship between social anxiety and eating disorders. Eating Behaviors. 2010;11:85–91. doi: 10.1016/j.eatbeh.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Zeller RA, Carmines EG. Measurement in the Social Sciences: The Link Between Theory and Data. New York: Cambridge University Press; 1980. [Google Scholar]