Abstract
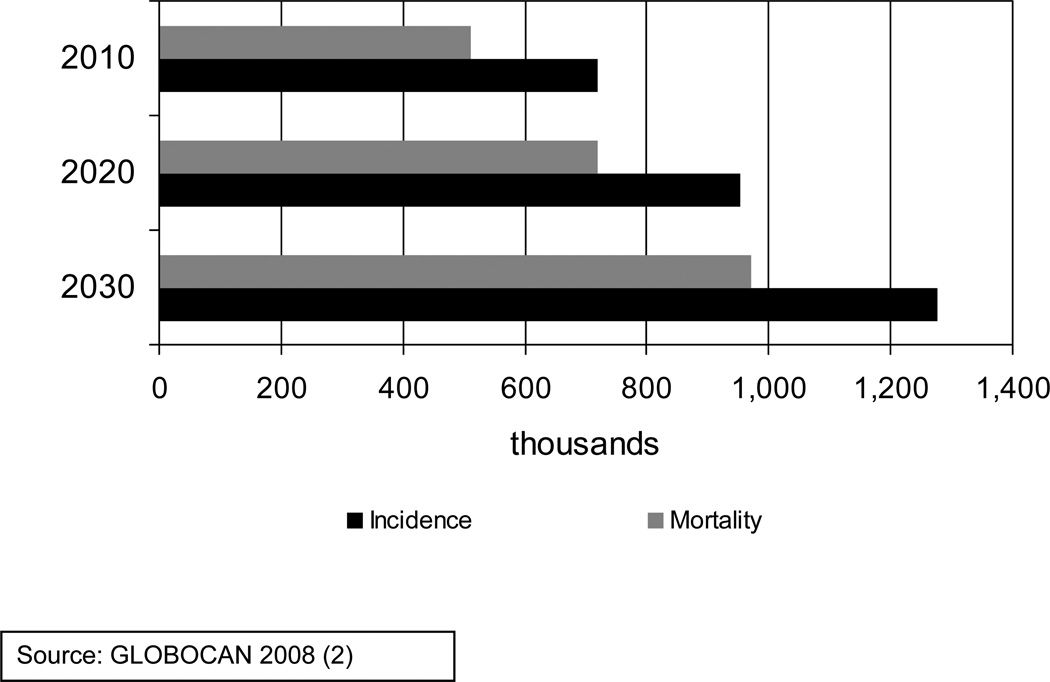
In Africa there were an estimated 681,000 new cancer cases and 512,000 deaths in 2008. Projections to 2030 show a startling rise, with corresponding figures of 1.27 million cases and 0.97 million deaths resulting from population growth and aging alone. The figures make no assumptions about incidence rates which may increase due to the further introduction of tobacco and a more westernized lifestyle. The current situation in many parts of Africa with respect to health care systems suggests that improved cancer treatment would be an insufficient response to this increasing burden. Much could be achieved through cancer prevention by applying current knowledge about major risk factors and the natural history of the disease. For example, vaccination against hepatitis B virus and human papilloma viruses would prevent the occurrence of two of the most common cancers in Africa, liver and cervix respectively, in the long-term. Strong measures to prevent the widespread introduction of tobacco must be a priority. Early detection and treatment of cervical and breast cancers using approaches applicable now in Africa would provide immediate value, as would the management of human immunodeficiency virus (HIV) infection in respect to HIV-associated malignancies. In parallel, further research is needed into the causes of cancer and the barriers to implementation of promising prevention strategies. Underpinning all is the need for African governments to look forward and prioritise cancer through national cancer control plans, to invest in public health infrastructure and to ensure the adequate training and support for people in cancer prevention and control. Given this core commitment from within Africa, international partners can provide complementary support in a cooperation that permits action now to mitigate the impending tragedy of cancer on the continent of Africa.
Keywords: cancer, Africa, aetiology, prevention
“We should put out the fire while it is still small” – a Kalenjin proverb, Kenya
Cancer occurrence in Africa
Cancer is one of the world’s major killers, being responsible for about 12.6% of all deaths globally in 2004 and killing more people than AIDS, tuberculosis and malaria combined.1 The most recent estimates of global cancer burden, in 2008, revealed a total of 12.7 million new cancer cases worldwide, with 7.6 million deaths.2 Projections based on these data reveal around a 70% increase in the number of new cases and deaths per year for the twenty years to 2030 due only to demographic changes. The majority of this increase will come in the developing countries with about 65% of the annual burden to be found there in just twenty years time.2
Africa is the continent least prepared to face this unprecedented growth in cancer burden (incidence and mortality). In 2008, there were an estimated 681,000 new cancer cases and 512,000 deaths. In 2030, the corresponding figures are projected to be 1.27 million cases and 0.97 million deaths, even assuming no increase in underlying incidence rates (Figure 1).2 These figures are driven by the projected increase in the African population from 1.02 billion in 2010 to 1.56 billion in 2030, with around 85% of this total residing in sub-Saharan Africa.3 The conservative assumption about stable underlying incidence rates is unlikely to hold given changing exposures to known risk factors e.g. tobacco, diet, obesity and physical inactivity, chronic infections and altered reproductive patterns. In Uganda significant increases in incidence of cancers of the prostate, breast, the cervix and of lymphoma/leukaemia were reported from 1991–2006.4 The most common cancers in Africa are summarized in Table 1. This reveals a predominance of cancers which are difficult to treat e.g. liver, stomach and oesophagus, even in countries with state-of-the-art diagnosis and therapy.
Figure 1.
African Cancer Burden 2010 to 2030
Table 1.
The most common cancers in Africa (estimated numbers of incident cases in males and females in 2008) (2)
| Cancer site | Estimated number of new cases |
Identified risk factors with high public health relevance to Africa |
High priority actions |
|---|---|---|---|
| Breast | 92 600 | Hormonal and reproductive factors, obesity, physical inactivity, alcohol | Early detection and treatment; breast cancer awareness; physical activity; avoidance of obesity |
| Cervix | 80 400 | High-risk mucosal HPV, tobacco | HPV vaccination; screening and treatment |
| Liver | 51 500 | HBV, HCV, aflatoxins | HBV vaccination; clean needles; screening of blood for transfusion; avoidance of unnecessary injections; aflatoxin control |
| Prostate | 39 500 | ||
| Non-Hodgkin lymphoma including Burkitt lymphoma | 37 200 | EBV, malaria, HIV (indirect), HCV | Anti-retrovirals; chemotherapy protocols adapted to low-resource settings |
| Colon and rectum | 34 900 | Obesity, physical inactivity, alcohol, tobacco | Tobacco control; physical activity |
| Kaposi sarcoma | 34 500* | HIV (indirect), KSHV | Anti-retrovirals |
| Oesophagus | 27 800 | Tobacco, alcohol | Tobacco control; alcohol control |
| Lung | 26 700 | Tobacco | Tobacco control |
| Stomach | 22 600 | Helicobacter pylori | |
| Bladder | 22 000 | Schistosoma, tobacco, | Tobacco control; anti-schistosomal drugs, |
sub-Saharan Africa only
The above figures are devastating, highlighting the emergence of cancer as a major public health problem in Africa. This challenge has been placed in context by the recent United Nations Resolution on non-communicable diseases,5 emphasising the priority required in relation to cancer and other chronic disorders. However, the global benefits of this initiative will not be maximized if the focus addressing non-communicable diseases is limited to tobacco-, alcohol-, physical inactivity- and obesity-related illness because currently four of the five most common cancers in Africa (see Table 1) are not significantly associated with these risk factors. Therefore a more flexible, tailored approach is needed in Africa, recognising in particular the important contribution of chronic infections.
One ray of hope is that there is some time to react. However, this demands urgent, concerted action from African governments, planners, leaders, health workers and scientists, with the help of the World Health Organization (WHO) and its Regional Office for Africa,6 non-governmental organizations, the public and private sectors, and international organizations. The response requires implementation of effective and affordable cancer control programmes integrated into clinical and public health systems. Establishing adequate health care infrastructure and public health services is a long process requiring strong government support; it is a stark reality that there has been little such investment in recent decades in many sub-Saharan African countries. The response also requires research into the causes and prevention of cancer in Africa, a focused, coordinated programme targeted at priority areas.
What are the reasons behind the dramatic situation in Africa? First, marked population growth and aging have been mentioned above in relation to increasing incidence. Second, low socio-economic status and deficient health care infrastructure, resulting in inadequate access to preventive and clinical services are important. Third, there are specific exposure patterns that explain the resulting cancer burden, and these are discussed briefly below.
Cancer risk factors
Strikingly some 25 to 30% of all cancers occurring in Africa are linked to infectious agents including viruses, bacteria and parasites (see Table 1).7,8 In fact two of the top three causes of cancer death (cervix and liver) and half of the ten most common cancers are associated with infections (Table 1 and ref 2). This places Africa in a rather positive position in the longer-term because the two major risk factors for cancer of the liver and cervix are known and there are effective vaccines. Thus if these two preventive measures are implemented, combined with a concerted effort to avoid the import of lifestyle, environmental and occupational risks from the more developed countries, a significant impact on cancer incidence and mortality could be achieved.9
Cancer of the cervix is the most common cause of cancer death in Africa (10.4% of all cancer deaths) and represents one in five of all cancer deaths in African women.2 Infection with human papilloma virus (HPV) is recognized as a necessary cause of cervical cancer, with HPV 16 and 18 being the most important oncogenic subtypes. The prevalence of HPV infection is higher in sub-Saharan Africa than any other area of the world.10
Liver cancer (predominantly hepatocellular carcinoma (HCC)) is the second leading cause of cancer death in Africa, equal to breast cancer, which each explains 9.8% of the total. 2 Major risk factors in Africa are chronic infection with hepatitis B virus (HBV), more prevalent in sub-Saharan Africa, and hepatitis C (HCV) virus, which is more prevalent in northern Africa.8 Another important contributor is dietary exposure to aflatoxins, fungal toxins produced under conditions of high humidity and temperature for crop storage.11 These potent hepatocarcinogens contaminate the dietary staples, maize and peanuts, and combined with chronic HBV infection lead to a particularly high risk of liver cancer.11
Non-Hodgkin lymphoma is the fourth most common cause of cancer death in Africa, representing 6% of the total. Again infectious agents have been implicated in the aetiology, including Epstein Barr virus (EBV), human immunodeficiency virus (HIV)8 and more recently HCV,12 although the picture is far less clear than for the infections associated with cervical and liver cancer. With respect to Burkitt’s lymphoma in children, research in Malawi further supported the role of EBV and malaria in the development of the disease, as well as a possible role for HIV.13
Kaposi sarcoma (KS) is another of the common types of cancer found in sub-Saharan Africa and is increasing in incidence4 with an estimated 34,500 new cases each year (Table 1). Highest rates are in eastern Africa followed by southern Africa.2 KS is associated with infection by KS-associated herpes virus (human herpes virus type 8 (HHV-8) in immune suppressed individuals such as seen with HIV infection.
Finally in terms of infections and cancer in Africa, one should note the roles of Helicobacter pylori in stomach cancer and Schistosoma haematobium in bladder cancer, the latter being particularly associated with squamous cell carcinoma in parts of northern Africa.14
Of the other common cancers in Africa it is worth noting that breast cancer is now the most common cancer in both sexes combined and is responsible for one in four of all cancers in African women, and just under one in five cancer deaths.2 It is also a cancer that is likely to have an increase in underlying incidence due to the change in pattern of risk factors in Africa, most notably earlier age at menarche, later childbirth, fewer children, reduced duration of breastfeeding and an increasing risk of obesity and physical inactivity, at least in urban areas.
An increase in lung and other tobacco-related cancers (oesophagus bladder, head and neck etc) is also expected as a result of a progressive shift of tobacco consumption from the developed world (legal restrictions, education, and awareness) to the more vulnerable low-resource countries. An increasing prevalence of obesity (especially among women), a more sedentary lifestyle, dietary changes, altered reproductive patterns as well as adoption of other western lifestyle changes would further modify the cancer risk in Africa, not only in terms of breast cancer as mentioned above, but also colorectal and other cancers. Finally the current existence and possible importation of further occupational exposures should not be overlooked.9
Surveillance, prevention and treatment
A majority of African countries have not traditionally considered cancer as a high priority in their health planning, compared to other competing concerns such as malaria and AIDS. This lack of awareness and prioritization is coupled, as mentioned above, to the chronic lack of basic infrastructure for diagnosis, treatment and prevention. For instance, some 15 African nations lack pathology and radiotherapy services. A recent study by Sankaranarayanan and colleagues15 showed that survival from colorectal, breast and cervix cancer is markedly lower in Africa compared to other regions of the world, even the other low resource countries. In The Gambia, the 5-year survival did not exceed 22% for these malignancies, while it ranged from 40 to 80% in China and Singapore. Thus the inequalities in access to cancer diagnosis, screening, treatment and care are added in Africa to the increasing occurrence of the disease. It is here that efforts such as those of the International Atomic Energy Authority (IAEA) with its Programme of Action for Cancer Therapy (PACT) and the International Network for Cancer Treatment and Research (INCTR) are so relevant. A cogent case has recently been made by the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries for progress in the areas of cancer treatment and care in low and middle-resource countries.16
Knowledge of cancer among Africans is also limited. For example, the Union for International Cancer Control (UICC) reported that more than a quarter of Africans surveyed believed that cancer had no cure once diagnosed and only 36% referred to cancer as an important health issue.17 Most often cancer is fatal due to the late stage of clinical presentation, something in turn a consequence of inadequate information and awareness. The barriers to cancer control therefore need to be understood in the specific context of Africa. A recent example from Ethiopia provided an illustration of the beliefs and practices of women with breast cancer and began to describe ways in which this knowledge may be implemented to affect the current late diagnosis and high mortality rates.18
A part of the above low prioritization of cancer has been the lack of information on cancer incidence and mortality in most African countries. When available, this information is often incomplete and the quality of data is variable. Population-based cancer registries cover only 8% of the African population, while this figure is about 99% for the USA and 40% for Europe. Furthermore, only 1% of the African population is covered by high quality cancer registries included in the last volume of “Cancer Incidence in Five Continents”.19 More accurate figures on the scale of the cancer burden and its projection are key requirements for an effective cancer control strategy and their provision would be a tremendous support to African governments in planning for protection of their people in this generation and the next.
Priorities and actions
The globalization of cancer requires a response from the international community. The response to a call for action in “The World Cancer Declaration”20 reflects an appetite for change. Combating cancer in Africa requires a comprehensive and multifaceted approach, using all the skills, commitment and cooperation available. With limited resources, the identification of priorities is a prerequisite for the establishment of efficient clinical and public health approaches. African governments need awareness of the current and impending situation, and to establish cost-effective and sustained national cancer control programmes, including prevention, early diagnosis and treatment. In this regard, the supporting role of the international community and related specialized organizations is crucial, but external support can only serve as a catalyst to a sustained commitment to public health and health care infrastructures from within.
Given the major cancers listed in Table 1, there is much that could be done in the way of control on the basis of current knowledge (see Table 2). In relation to infection-associated cancers, screening for pre-cancerous lesions of the cervix by visual inspection or, once affordable, identifying high-risk women by HPV DNA testing is an effective measure to control cervical cancer.21,22 This, coupled with HPV vaccination, would significantly reduce the incidence and mortality due to this tumour in Africa. In the case of both HPV DNA testing and vaccination, urgent efforts are required to make these approaches affordable in the regions they are needed most. Rwanda recently became the first African country to introduce a national vaccination programme for HPV, although sustainable funding remains a challenge to be faced.23
Table 2.
Ten priorities and actions for cancer research and control in Africa
| Ten Priorities and Actions for Cancer Research and Control in Africa |
|
Vaccinating against HBV will contribute to lowering the incidence and mortality due to HCC.24,25 In 2005, only 39% of the eligible African population was in receipt of HBV vaccine.26 With the commitment and engagement of GAVI, UNICEF and WHO, the current coverage reached 65 % for 2008.26 Despite this progress, more emphasis from African governments is required to further extend HBV immunization. In addition, low technology approaches to reduce exposure to aflatoxins, ubiquitous dietary contaminants, could also serve to reduce the HCC burden.27 The success of work with subsistence farmers to reduce carcinogen contamination of staple foods is promising and has benefits beyond the impact on cancer.11,26,28 The screening of blood for transfusion, the use of clean needles and avoidance of unnecessary injections in order to combat transmission of HCV would be a further positive impact on HCC occurrence.
The availability of anti-retroviral drugs for HIV-infected patients will help reduce the cancer-related burden for this infection. Indeed, a significant decrease in the incidence of some AIDS-defining malignancies, e.g. Kaposi sarcoma (KS) and non-Hodgkin's lymphomas, following the introduction of HAART have been reported.29 However, the use of highly active combination antiretroviral therapy (cART) leads to an increase of non-AIDS-defining malignancies, such as cervical cancer and HCC.29 The schistosoma-associated bladder cancer incidence and morbidity could be potentially reduced by controlling the parasitic infestation (education to avoid water infested by Schistosoma eggs, control of snails and improved water sanitation), and by making available effective anti-schistosomal drugs.8
A critical area of intervention in which political leadership offers great potential is the fight against tobacco. Tobacco consumption is responsible for about 30% of cancers worldwide. However, among the low-resource countries, those in Africa have experienced the highest increase in tobacco consumption, and therefore face future increases in lung and other tobacco-related cancers.30 Increasing taxes and enforcing strict pricing policies in order to reduce tobacco consumption as well as restricting cigarette smoking in public areas and providing educational information offer potentially simple and efficient measures to combat this impending epidemic. In this regard, the role of the African Tobacco Control Consortium will be instrumental. The African Union could play a role at a high political level to stimulate and encourage the implementation of a cancer control programme in each African member state. These efforts can draw on support from the WHO Tobacco Free Initiative and also the political force and obligations of the WHO Framework Convention for Tobacco Control, the first treaty negotiated under the auspices of the WHO.
Cumulative evidence clearly indicates that obesity and physical inactivity are risk factors for development of cancers including breast, endometrium, oesophagus (adenocarcinoma), kidney and colon.31 With urbanization and a more westernized lifestyle these risk factors are spreading, with many low resource countries in Africa and elsewhere now experiencing the so-called importation of obesity.32 Therefore preventive measures should be integrated in a national plan for control of non-communicable diseases, as recommended by the WHO Global strategy on diet, physical activity and health.33
It would be an error to think that all the causes of cancer in Africa are known and the remaining task is restricted to the implementation of prevention. For example, in terms of incidence rates oesophageal cancer is the third most common malignancy in men in sub-Saharan Africa, but cancer registry data reveal remarkable geographic variation between Eastern Africa, where it is the most frequent cancer in men and Western Africa where it is not even among the top ten.2 What is the cause? For cancers that are increasing in incidence the picture is similarly unclear; for prostate, for example, causes are unknown. The first step to prevention is the identification of causation. For this reason, in the cancer agenda for Africa, research into cancer aetiology must retain prominence.
Many of the high resource countries are increasingly focusing their research efforts on development of cancer treatments tailored to the individual – the field of personalized medicine. But what of Africa? Should African countries place priority on these areas when so much that is preventable is not prevented and when many basic treatments and palliative care measures are still unavailable? While integrating new avenues in cancer treatment and diagnosis is important,16 modern approaches in descriptive, analytical and molecular epidemiology should be also prioritized in Africa to provide the evidence-base for the establishment of relevant and effective public health policies to prevent cancer. To focus on the former and neglect the latter would, we suggest, be a grave mistake. The success of the HIV control and research programme in Uganda and in other parts in the continent demonstrates what could be delivered in terms of a scientific contribution to prevention if conditions are right.34
Another important priority area is education and training. There is a general, but desperately urgent requirement for expansion of technical and university training to meet the chronic shortage of human resources in the health sector in Africa. In terms of causes and prevention of cancer, interdisciplinary approaches linking the basic sciences to both the clinical treatment and management of cancer but also to epidemiology and public health should be a priority. Cancer research is a principal element in a cancer control strategy, including research into how to implement known preventions in the African context, an oft-neglected area of cancer research generally.
Technology transfer and training should be integral to collaboration. It should also be informed by excellence and quality. African participation in the scientific endeavour must be in a partnership of equals, not simply as a source of interesting populations or biological samples. Areas of training relevant to cancer research and control in Africa include cancer registration, the causes and molecular pathogenesis of cancer, development of preventions (primary prevention, early detection and screening), implementation of prevention strategies, health services research, and the factors (social, cultural, biological) determining the late presentation of most cancers. The African Organization for Research and Training in Cancer (AORTIC), which creates links between African health scientists, teachers and the international community, has a tremendous opportunity to promote this agenda.
Conclusions
There is no longer any doubt about the striking reality of cancer in Africa. In the near future, it is estimated that more than two in every three cancer deaths will occur in less developed countries,2 and that African countries will pay a high price because they are ill-prepared to face this impending tragedy. There is much that could be done (see Table 2 for a summary) and an effective collaboration with international institutions and agencies, is a key step for success. Africa’s problem is the world’s problem. It is said in Africa that “If the house of your neighbour is burning, give him help, as the fire is not far from you”. A strong commitment should come from the high resource countries through recognition of cancer in Africa as a global issue. It is also said in Africa that “If someone is washing your back, you should wash your front”. Thus, Africa also needs the commitment of its own governments and political leaders, its own health professionals, its own people to prioritize the development of efficient national cancer control programmes. This commitment must rally all social strata and resources in a concerted action, drawing on appropriate international support. With an eye to the future, a prominent place must be retained for training young scientists and qualified health professionals, as these are the ones who will take up the challenges of tomorrow and whose children will in time reap the benefits of their efforts.
Acknowledgements
The authors would like to thank Jacques Ferlay, Silvia Franceschi, Rengwaswamy Sankaranarayanan, Vincent Cogliano, Kurt Straif and Eduardo Seleiro for their insightful comments.
Grant Sponsor: Dr Wild acknowledges support from the NIEHS, USA; grant no. ES06052.
Abbreviations
- KS
Kaposi sarcoma
- WHO
World Health Organization
- HPV
human papilloma virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- EBV
Epstein Barr virus
- HIV
human immunodeficiency virus
- HHV-8
human herpes virus type 8
- IAEA
International Atomic Energy Authority
- PACT
Programme of Action for Cancer Therapy
- INCTR
International Network for Cancer Treatment and Research
- UICC
Union for International Cancer Control
- GAVI
Global Alliance for Vaccines and Immunisation
- cART
active combination antiretroviral therapy
- AORTIC
African Organization for Research and Training in Cancer
Footnotes
Drs Wild and Sylla were responsible for the planning and writing of this article.
The two authors have no conflicts of interest to declare.
No ethics committee approval was required for this article.
Reference List
- 1.World Health Organization. The global burden of disease: 2004 update - Annex A: Deaths and DALYs 2004 Annex tables. WHO; 2008. eds. [Google Scholar]
- 2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 3.United Nations. World Population Prospects, the 2010 Revision. http://esa.un.org/unpd/wpp/unpp/panel_population.htm.
- 4.Parkin DM, Nambooze S, Wabwire-Mangen F, Wabinga HR. Changing cancer incidence in Kampala, Uganda, 1991–2006. Int J Cancer. 2010;126:1187–1195. doi: 10.1002/ijc.24838. [DOI] [PubMed] [Google Scholar]
- 5.United Nations General Assembly - Resolutions, 64th Session, 2010. http://www.un.org/ga/64/resolutions.shtml.
- 6.WHO. Cancer Prevention and Control: a Strategy for the WHO African Region. Yaounde, Republic of Cameroon; 2008. Report No: AFR/RC58/9. [Google Scholar]
- 7.Parkin DM, Sitas F, Chirenje M, Stein L, Abratt R, Wabinga H. Part I: Cancer in Indigenous Africans--burden, distribution, and trends. Lancet Oncol. 2008;9:683–692. doi: 10.1016/S1470-2045(08)70175-X. [DOI] [PubMed] [Google Scholar]
- 8.Sitas F, Parkin DM, Chirenje M, Stein L, Abratt R, Wabinga H. Part II: Cancer in Indigenous Africans--causes and control. Lancet Oncol. 2008;9:786–795. doi: 10.1016/S1470-2045(08)70198-0. [DOI] [PubMed] [Google Scholar]
- 9.Ly A. Cancer et environment en Afrique. Oncologie. 2007;9:370–379. [Google Scholar]
- 10.Bruni L, Diaz M, Castellsague X, Ferrer E, Bosch FX, de Sanjosé S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202:1789–1799. doi: 10.1086/657321. [DOI] [PubMed] [Google Scholar]
- 11.Wild CP, Gong YY. Mycotoxins and human disease: a largely ignored global health issue. Carcinogenesis. 2010;31:71–82. doi: 10.1093/carcin/bgp264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El-Ghissassi F, Ibrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V. A review of human carcinogens--Part B: biological agents. Lancet Oncol. 2009;10:321–322. doi: 10.1016/s1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- 13.Mutalima N, Molyneux E, Jaffe H, Kamiza S, Borgstein E, Mkandawire N, Liomba G, Batumba M, Lagos D, Gratrix F, Boshoff C, Casabonne D, et al. Associations between Burkitt lymphoma among children in Malawi and infection with HIV, EBV and malaria: results from a case-control study. PLoS One. 2008;3:e2505. doi: 10.1371/journal.pone.0002505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030–3044. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- 15.Sankaranarayanan R, Swaminathan R, Brenner H, Chen K, Chia KS, Chen JG, Law SC, Ahn YO, Xiang YB, Yeole BB, Shin HR, Shanta V, et al. Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol. 2010;11:165–173. doi: 10.1016/S1470-2045(09)70335-3. [DOI] [PubMed] [Google Scholar]
- 16.Farmer P, Frenk J, Knaul FM, Shulman LN, Alleyne G, Armstrong L, Atun R, Blayney D, Chen L, Feachem R, Gospodarowicz M, Gralow J, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet. 2010;376:1186–1193. doi: 10.1016/S0140-6736(10)61152-X. [DOI] [PubMed] [Google Scholar]
- 17.Union for International Cancer Control. UICC Special reports. 2010 http://old.uicc.org/index.php?option=com_content&task=view&id=16583.
- 18.Dye TD, Bogale S, Hobden C, Tilahun Y, Hechter V, Deressa T, Bize M, Reeler A. A mixed-method assessment of beliefs and practice around breast cancer in Ethiopia: Implications for public health programming and cancer control. Global Public Health. 2010;22:1–13. doi: 10.1080/17441692.2010.510479. [DOI] [PubMed] [Google Scholar]
- 19.Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, Boyle P, editors. Cancer Incidence in Five Continents. Vol. IX. Lyon, France: IARC Scientific Publications No. 160; 2008. [Google Scholar]
- 20.UICC Declaration. http://www.uicc.org/declaration.
- 21.Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, Hingmire S, Malvi SG, Thorat R, Kothari A, Chinoy R, Kelkar R, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360:1385–1394. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- 22.Denny L, Kuhn L, Hu CC, Tsai WY, Wright TC., Jr Human papillomavirus-based cervical cancer prevention: long-term results of a randomized screening trial. J Natl Cancer Inst. 2010;102:1557–1567. doi: 10.1093/jnci/djq342. [DOI] [PubMed] [Google Scholar]
- 23.Anon. Financing HPV vaccination in developing countries. Lancet. 2011;377:1544. doi: 10.1016/S0140-6736(11)60622-3. [DOI] [PubMed] [Google Scholar]
- 24.Chang MH, You SL, Chen CJ, Liu CJ, Lee CM, Lin SM, Chu HC, Wu TC, Yang SS, Kuo HS, Chen DS. Decreased incidence of hepatocellular carcinoma in hepatitis B vaccinees: a 20-year follow-up study. J Natl Cancer Inst. 2009;101:1348–1355. doi: 10.1093/jnci/djp288. [DOI] [PubMed] [Google Scholar]
- 25.Viviani S, Carrieri P, Bah E, Hall AJ, Kirk GD, Mendy M, Montesano R, Plymoth A, Sam O, Van der SM, Whittle H, Hainaut P. 20 years into the Gambia Hepatitis Intervention Study: assessment of initial hypotheses and prospects for evaluation of protective effectiveness against liver cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:3216–3223. doi: 10.1158/1055-9965.EPI-08-0303. [DOI] [PubMed] [Google Scholar]
- 26.WHO/UNICEF coverage estimates 1980–2008. http://www.who.int/immunization_monitoring/en/
- 27.Turner PC, Sylla A, Gong YY, Diallo MS, Sutcliffe AE, Hall AJ, Wild CP. Reduction in exposure to carcinogenic aflatoxins by postharvest intervention measures in West Africa: a community-based intervention study. Lancet. 2005;365:1950–1956. doi: 10.1016/S0140-6736(05)66661-5. [DOI] [PubMed] [Google Scholar]
- 28.van der Westhuizen L, Shephard GS, Burger HM, Rheeder JP, Gelderblom WC, Wild CP, Gong YY. Fumonisin B1 as a urinary biomarker of exposure in a maize intervention study among South African subsistence farmers. Cancer Epidemiol Biomarkers Prev. 2011;20:483–489. doi: 10.1158/1055-9965.EPI-10-1002. [DOI] [PubMed] [Google Scholar]
- 29.Bower M, Palmieri C, Dhillon T. AIDS-related malignancies: changing epidemiology and the impact of highly active antiretroviral therapy. Curr Opin Infect Dis. 2006;19:14–19. doi: 10.1097/01.qco.0000200295.30285.13. [DOI] [PubMed] [Google Scholar]
- 30.The Tobacco Atlas, Third edition. The American Cancer Society and World Lung Foundation; 2009. http://www.tobaccoatlas.org/tobaccoatlas/press_4-14-10.html. [Google Scholar]
- 31.World Cancer Report. Lyon, France: International Agency for Research on Cancer; 2008. http://www.iarc.fr/en/publications/pdfs-online/wcr/2008/wcr_2008.pdf. [Google Scholar]
- 32.Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: A problem of the rich or the poor? BMC Public Health. 2009;9:465. doi: 10.1186/1471-2458-9-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO; 2004. WHO global strategy on diet, physical activity and health. [DOI] [PubMed] [Google Scholar]
- 34.Gotch F, Gilmour J. Science, medicine and research in the developing world: a perspective. Nat Immunol. 2007;8:1273–1276. doi: 10.1038/ni1531. [DOI] [PubMed] [Google Scholar]