Abstract
In the model medical curriculum HannibaL at Hannover Medical School (MHH, Hannover, Germany), communication skills in taking case histories and disclosing diagnoses (breaking bad news) are assessed through an objective structured clinical examination (OSCE). This is part of the examinations which at the MHH represent the equivalent to the First Part of the Medical Examinations. The second year doctor-patient communication course preparing for these examinations was evaluated during the 2009/10 academic year.
Using questionnaires specific to the learning objectives, learning needs were assessed, pre-post comparisons of self-assessed competencies were performed and key teaching methods were evaluated (5-point Likert scales, “5”=fully agree). At T0 (start of the course) 267 students participated (response rate: 93.7%), of which 180 filled out the T1 questionnaire during the last session of the course (67.4%). Within-subject analyses of variance and paired t-tests were conducted.
The highest learning needs were found for the “to show how”-items regarding history taking and disclosing diagnoses (M=4.4). The T1-T0 comparisons showed the greatest improvements for history taking (“to know how”: mean difference = +1.7, “to show how”: +1.8, p<.0001 as with all tests) and the “to know how”-item regarding the disclosure of diagnoses (+1.6), followed by the “to show how”-items on disclosing a diagnosis (+1.4), shared decision making (+1.2), self-assessing one’s own strengths/weaknesses (+1.0) and confidently approaching new patients (+0.7). Students with T0 values of 1 or 2 on the respective scales improved on average by 2.2 points across all items, students with the value of 3 by 1.1, and from 4 or 5 by 0.1. Methodically, the use of simulated patients was rated the most helpful (M=4.8, 87% with the scale value 5).
This doctor-patient communication course is associated with substantial improvements regarding all key learning objectives. Regarding methods, the deployed simulated patients (2-4 per 10-student-course group in 3 of the 7 course sessions, respectively) were rated the most helpful. The present evaluation calls for both further development of the doctor-patient communication curriculum at the MHH and joint activities across medical schools, which are discussed at the end of the paper.
Keywords: Doctor-Patient Communication, Undergraduate Medical Education, Medical History Taking, Diagnosis Disclosure, Health Communication
Abstract
Im MHH-Modellstudiengang HannibaL werden Gesprächsführungskompetenzen für Anamneseerhebung und Diagnosemitteilung durch eine Objective Structured Clinical Examination (OSCE) geprüft, die Teil der dem Ersten Abschnitt der Ärztlichen Prüfung äquivalenten Prüfungen sind. Das vorbereitende Gesprächsführungspraktikum im 2. Studienjahr wurde 2009/10 evaluiert.
Mittels lernzielspezifischer Fragebogen wurden der Lernbedarf erhoben, Vorher-Nachher-Vergleiche der selbsteingeschätzten Kompetenzen durchgeführt und zentrale Lehrmethoden bewertet (5-Punkt-Likertskalen, „5“=hohe Ausprägung). Zu T0 (Beginn des Praktikums) nahmen 267 Studierende teil (Teilnahmerate: 93,7%), von denen 180 den T1-Fragebogen beim letzten Praktikumstermin ausfüllten (67,4%). Es wurden Varianzanalysen mit Messwiederholungsfaktor und T-Tests für verbundene Stichproben durchgeführt.
Die höchsten Lernbedarfe zeigten sich bei den „to show how“-Items zu Anamneseerhebung und Diagnosemitteilung (M=4,4). Die T1-T0-Vergleiche zeigten die größten Verbesserungen bei den anamnesespezifischen Items („to know how“: Mittelwertsdifferenz=+1,7, „to show how“:+1,8, p<.0001 wie bei allen Tests) und beim „to know how“-Item zur Diagnosemitteilung (+1,6), gefolgt von der Umsetzung einer Diagnosemitteilung (+1,4), partizipativer Entscheidungsfindung (+1,2), der Einschätzung eigener Stärken/Schwächen (+1,0) und dem sicheren Zugehen auf neue Patienten (+0,7). Studierende mit T0-Werten von „1“ oder „2“ auf den jeweiligen Skalen verbesserten sich über alle Items im Mittel um 2,2 Punkte, solche mit „3“ um 1,1, und mit „4“ oder „5“ um 0,1. Methodisch wurde der Einsatz der Simulationspatienten am hilfreichsten bewertet (M=4,8; 87% mit dem Wert „5“).
Das Gesprächsführungspraktikum ist bezüglich aller zentralen Lernziele mit deutlichen Lernfortschritten assoziiert. Methodisch wird vor allem der Einsatz von Simulationspatienten (pro Praktikumsgruppe mit 10 Studierenden zu 3 von 7 Terminen mit jeweils 2-4 Simulationspatienten) am besten bewertet. Die Evaluation spricht für einen weiteren Ausbau des Gesprächsführungscurriculums an der MHH und von hochschul-/fakultätsübergreifenden Aktivitäten, die abschließend diskutiert werden.
Introduction
Both the new version of the German Medical Licensure Act [1], which specifies the teaching of practical experiences in dealing with patients as a new objective in §1, and the National Competence-Based Learning Objectives for Undergraduate Medical Education (NKLM) [2] have contributed to a central curricular role of social and communicative skills in medical schools. The model medical curriculum HannibaL (Hanoverian integrated, job-oriented and adaptive curriculum) at Hannover Medical School (MHH) centres practical skills in dealing with patients and their diseases. All newly enrolled students at the MHH are taught according to this curriculum since the winter term of 2005/06.
HannibaL also includes a 28-hour course on doctor-patient communication skills. It is offered by the Medical Psychology Unit and the Medical Sociology Unit in cooperation with the Institute of General Practice, the Clinic for Psychosomatics and Psychotherapy and the Clinical Psychology Working Group of the Clinic of Psychiatry, Social Psychiatry and Psychotherapy. Its learning objectives consist of basic skills in taking patient histories, disclosing diagnoses (breaking bad news), and the use of shared decision-making (SDM) in these contexts. These skills are assessed at two of six stations of an objective structured clinical examination (OSCE). This is part of MHH’s internal examinations, which in HannibaL represent the equivalent to the mid-course First Part of the Medical Examinations. The other four OSCE stations test examination techniques which are taught in other parts of the module “Diagnostic Methods”**, to which the communication course belongs. At the same time, in 2010 simulated patients (SP) were used for the third time not only in the OSCE but also in the course itself. Beyond the central evaluation of the total module, it was therefore important to specifically evaluate the course regarding its learning objectives.
Course Concept and Content
The course includes seven sessions lasting four hours each. The students of each year are divided into 28 groups of ten to allow repeated role play within the group and with the SP. Since its first appearance in the literature [3], the use of SP has become the international standard for the practical study of communication skills in medical studies [4], [5] and is now also popular in Germany [5], [6], [7]. Feedback from the SP is seen an important part of the learning process [4], [8]. The SP used here were primarily recruited amongst members of the German Diabetes Association (Hanover Region), and amongst cardiac patient groups and instructed patients of the Institute of General Practice. A smaller number were drawn from a larger pool of amateur actors which was first set up in 2007 through the mediation of the Amateur Theatre Association of Lower Saxony (in the OSCE amateur actors form the majority of the SP, with each SP used only either in the course or the OSCE). In total, about 80 SP aged 23-77 (61.3% women) are currently available. They are paid adequately for their services.
Table 1 (Tab. 1) gives an overview over the seven course sessions. In the first two sessions the basics of doctor-patient communication are taught based on the axioms of Watzlawick [9] and the models by Schulz von Thun [10]. Practical exercises (such as role plays) are used to facilitate active listening, nonverbal communication and initiating communication.
Table 1. Overview of course content and methods (academic year 2009/10).
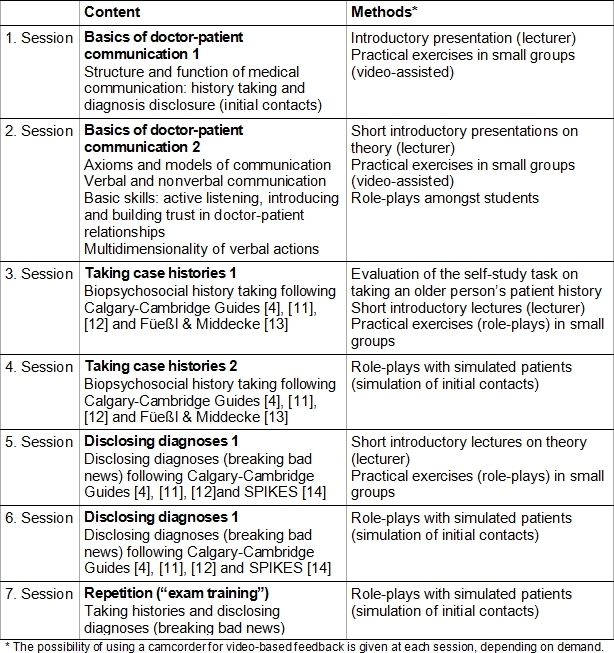
In preparation for the third session, students are instructed to take a biopsychosocial case history with an elderly person (self-study exercise). An appraisal of this takes place in the group at the beginning of the third session, which focuses on the structure and conduct of patient histories in terms of content and practice. Usually, an initial contact in a medical practice is defined as the setting for role plays. For the preparation and appraisal of the role plays, the students use an observation sheet developed by the APG-Teaching Team, which combines the key criteria of the Calgary-Cambridge Guides [11], [4], [12] and Füeßl and Middeke [13]. In the fourth unit two SP are invited for each group of ten, which, through rotation and by splitting of groups, allows for up to eight role plays per course group. To train biopsychosocial history taking, the SP either describe own disease experiences (excluding currently existing symptoms and emergency situations) or use predefined cases.
The focus of the fifth session is the disclosure of diagnoses in a comprehensible and patient-oriented manner based on the Calgary-Cambridge Guides [11], [4], [12] and SPIKES [14]. Through role play students practice breaking bad news as a medical task. Again, a specific observation sheet is used, and – in the sixth session – SP facilitate practising. The role plays are based on predefined cases, with their contents adjusted to the SP. They either relate to diabetes mellitus type 2, hypertension, coronary heart disease, disc herniation, chronic bronchitis/COPD, benign prostatic hyperplasia, or breast cancer. These diseases (which relate to a preparatory course at the beginning of HannibaL and other modules) constitute possible themes for the OSCE-station on diagnosis disclosure. In addition to a short patient history, diagnostic findings and the diagnosis itself they contain selected treatment options which offer students the opportunity to practice SDM [15]. Of course, based on a self-administered profile sheet and briefings before ach course sessions the SP have a say on disease patterns they are able and willing to act out. The final session again involves SP and provides opportunities for repetition and exam preparation. Here, the SP are prepared to simulate both contexts (history having and diagnosis disclosure).
The course is accompanied by a biweekly lecture (eight sessions of one hour each) to deepen theoretical backgrounds (relating to [16] besides the aforementioned references) and to teach clinical knowledge, partly through patient presentations. Video-assisted learning is part of the course, both through the use of instructional videos for analysis and discussion as well as for recording and appraisal of the students' practical exercises. Written material is usually provided to the students via MHH’s e-learning platform ILIAS.
This article reports the internal evaluation results of the course during the 2009/10 academic year. Relating to its key learning objectives, it focuses on the learning needs of the students and their competencies at the beginning of the course (T0) as well as their learning progress by the end of the course (T1). The central question is whether the students rate their competencies at T1 as higher than at T0. In addition, key methods such as the use of SP are evaluated. All data are based on self-reports.
Methods
Questionnaires
The questionnaires were specifically developed for the learning objectives and oriented towards the competencies tested at the two OSCE stations (history taking and diagnosis disclosure). The T0-questionnaire includes seven items for self-assessment: In accordance with [17] items on knowledge (“to know how”) and confidence in one’s own abilities (“to show how”) regarding history taking and diagnosis disclosure, one “to show how”-item each on self-confidence regarding patient contact and consulting treatment options (SDM), and one regarding self-awareness of one’s own strengths and weaknesses in communication (see Table 2 (Tab. 2)). The same sheet also contains a column on the respective learning needs. Finally, it contains a free text field to describe existing experience with patients in the medical field (over and above the nursing internship). Data on age and gender are also collected through the questionnaire.
Table 2. Questionnaires (left: T0, right: T1).
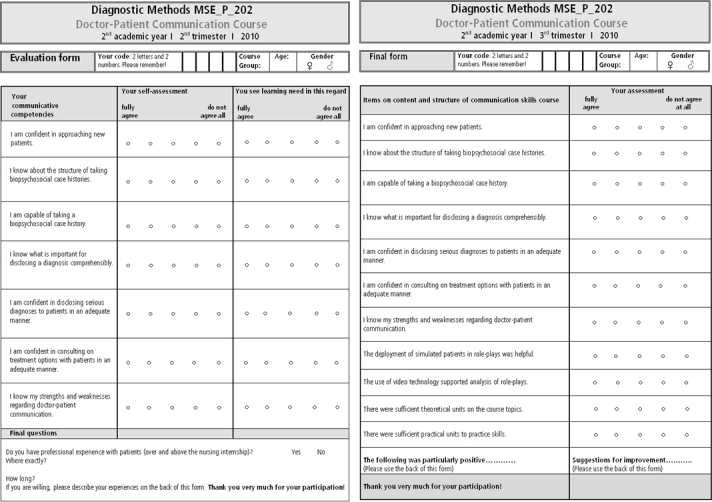
The second questionnaire (T1) takes up the seven competency items for the pre-post comparison and also includes items to evaluate the use of the SP, video support and quantity of theory and practice. For all items, a 5-point Likert scale ranging from 1 (do not agree at all) to 5 (fully agree) was used. In addition, the T1-questionnaire provided students with a free text field giving them the opportunity to list, from their point of view, both positive aspects and suggestions for improvement.
Sample and procedure
In total 285 students participated in the course in the 2009/10 academic year. The T0-questionnaire was issued at the first course session and completed by 267 students (response rate: 93.7%). Of these, 180 students completed the T1 questionnaire at the end of the course (equivalent to 63.2% of the course participants and 67.4% of the T0-sample). The survey was conducted anonymously using personal codes. Reasons for non-response at T0 are assumed to be organisational in nature, for example due to people changing to the MHH from other universities at beginning of the summer term (i.e. between the second and third course session) which were admitted to the course. Regarding T1-nonresponse it should be noted that one missed session was permitted per student and that due to the density of examinations towards the end of the summer term, some of the students used the final session as "their" missed session (see the dropout analysis below regarding possible attrition biases).
Data analysis
Following a description of the sample by gender, age and experience with patients, and a T1-dropout analysis, differences in the learning needs at T0, the competency assessments at T0 and the evaluation of methods at T1 were tested using within-subject analyses of variance. The seven or four items, respectively, defined the repeated measure factor. In all three analyses, the sphericity assumption was tested using Mauchly’s sphericity test. This test was always significant (p<.0001) and thus the assumption violated (i.e. in each case unequal variances of the differences of all measurement pairs were shown). As epsilon was >.75 in all analyses (learning needs: .87; competency assessments: .91; evaluation of methods: .89), the Huynh-Feldt correction was applied, and the corresponding degrees of freedom and p-values are reported. However, divergent conclusions arose neither from the comparison to the model under the assumption of sphericity nor to the multivariate approach. The learning progress regarding each competency (pre-post analysis from T0 to T1) was tested using t-tests for paired samples (all analyses: SPSS/PASW Statistics Version 18).
Results
Sample description and dropout analysis
Table 3 (Tab. 3) describes the T0-sample by gender, age and experience with patients. More than two thirds of students are women (68.8%). They have a larger age variability than male students (standard deviation = 3.6, vs. 2.4), while on average they do not differ significantly. In total nearly half of the students have experience in dealing with patients over and beyond the nursing internship (49.8%, with a higher proportion among men than women – 56.4% vs. 45.7% –, without this difference being significant).
Table 3. Sample description (N=267) by gender, age and experience with patients*.
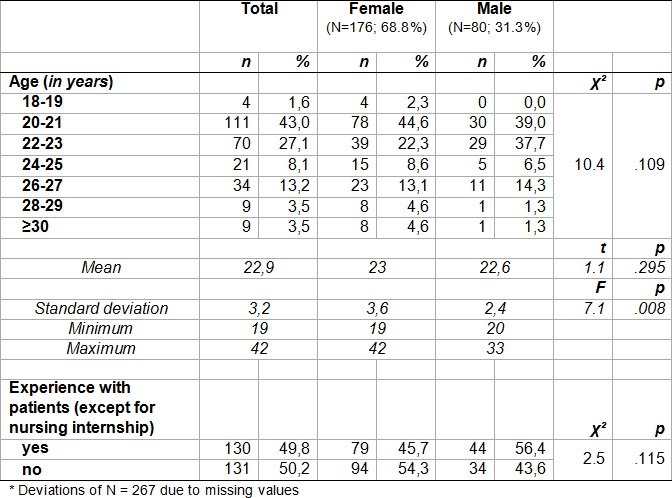
The longitudinal dropout analysis rendered the following results. Of those students with data available at both points in time, 67% were women, with this proportion being higher in the group with no T1-data (72.7%), although this was not statistically significant (Chi²=0.81, p=.368). The age difference between the two groups was also not significant (M=22.8 vs. 22.9, F(1.257)=0.02, p=.899), as was experience with patients (46.9% vs. 55.8%, Chi²=1.85, p=.174). Regarding learning needs, a significant difference emerged in terms of a higher value in the group with data at T0 and T1 regarding one’s own strengths and weaknesses in communication (M=4.1 vs. 3.8, F(1.260)=3.99, p=.047). The self-assessments of the students’ own skills at T0 showed differences in the confidence in the ability to take a patient’s history (M=2.5 in the group with data for T0 and T1 vs. 2.2, F(1.264)=6.19, p=.013), in knowing how disclose a diagnosis in a comprehensible fashion (3.1 vs. 2.7, F(1,266)=11:43, p=.001), and in the confidence in regard to actually disclosing a serious diagnosis (2.7 vs. 2.4, F(1.266)=4.63, p=.032).
Subjective Learning Needs at T0
As Figure 1 (Fig. 1) shows, on average students report considerable learning needs with regard to the course’s learning objectives. At the same time there were significant differences (F(5.247) 23.4, p<.0001). The highest demand can be found for the “to show how”-items regarding history taking and disclosing diagnoses (both M=4.4 [median=5, not shown here]), followed by the SDM-item (median=5) and the two corresponding knowledge items (median=4). Values for the confidence in approaching new patients and the assessment of the students’ own strengths and weaknesses regarding medical communication are at a similar level but slightly lower (M=4.0 and 3.9, median=4).
Figure 1. Perceived learning needs at T0.
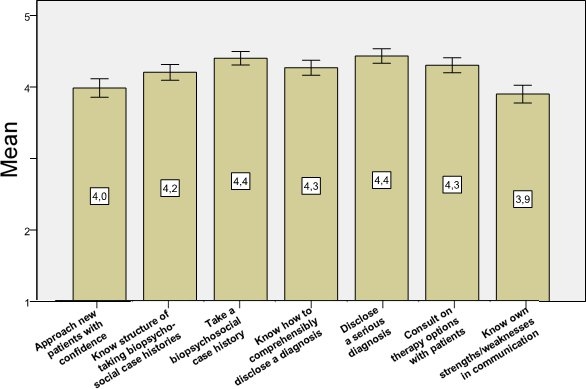
(1 = fully disagree, 5 = fully agree; mean values with 95% confidence intervals)
Self-assessed competencies at T0 and T1 and learning progress (comparison T1-T0)
As Figure 2 (Fig. 2) shows, at T0 the lowest average competency self-assessment emerged for the “to show how”-items regarding history taking and diagnosis disclosure (M=2.2 and 2.4 [median=2, not shown here]), followed by the corresponding knowledge items (median=2 and 3, respectively) and the SDM-item (median=3). Results for confidence in approaching new patients and one’s own strengths and weaknesses are somewhat higher (M =3.4 or 3.1, median=3). Thus, the self-assessments of competencies show an inverse pattern compared to the learning needs (see above). The differences are statistically significant (F(5.429)=48.6, p<.0001).
Figure 2. Self-assessments of competencies at T0 and T1 and learning progress (comparison T1-T0) .
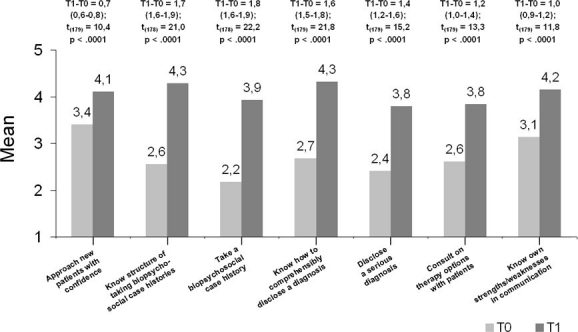
(1 = fully disagree, 5 = fully agree; mean differences with 95% confidence intervals; t-tests for dependent samples, N = 180, deviating degrees of freedom due to missing values)
The T1-T0 comparisons show that significant progress was made regarding all seven learning objectives. The biggest differences were found for the item on history taking (“to know how”: mean difference=1.7, “to show how”: 1.8, p<.0001 for all tests) and the “to know how”-item on disclosure of diagnoses (1.6). These are followed by the self-assessment of the competency to actually break bad news on a diagnosis (1.4), SDM (1.2), knowing one’s own strengths and weaknesses (1.0) and confidently approaching new patients (0.7). At the same time an analysis stratified according to baseline levels showed that students who on the respective scales had rated themselves with the values 1 or 2 on average improved by 2.2 points across all items, those who had rated themselves with 3 improved by 1.1 points, and those with 4 or 5 by 0.1 (not shown).
Evaluation of methods (at T1)
As Figure 3 (Fig. 3) shows, students rated the use of the SP as most helpful (M=4.8), with 87% selecting “fully agree”. The theoretical and practical parts of the sessions were rated equally, though slightly lower than the SP (M=4.2 and 4.0). In comparison, the use of video technology to record role plays was rated positive by fewer students (M=3.5). The differences were statistically significant (F(2.673)=64.9, p<.0001). All medians of the items (except regarding the SP) were 4, respectively.
Figure 3. Evaluation of various teaching methods (at T1).
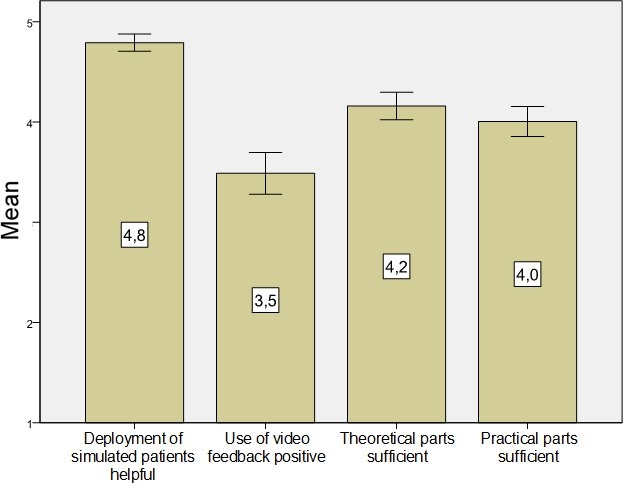
(1 = fully disagree, 5 = fully agree; mean values with 95% confidence intervals)
Discussion
In sum, based on students’ self-assessments the doctor-patient communication course in the second year of HannibaL is associated with significant learning progress regarding all its key learning objectives. This is especially true for taking patient histories and disclosing diagnoses (breaking bad news) as its central themes, both in terms of “to know how”- and “to show how”-levels of competency. Taking biopsychosocial case histories showed the strongest learning progress, followed by patient-oriented disclosure of diagnoses, SDM, knowing one’s own strengths and weaknesses in communication and the self-confidence in approaching new patients. The latter two had initially shown the lowest learning needs and the best self-assessments. Furthermore, students who had initially rated themselves rather poorly (1 or 2 on 5-point scales) on average improved by 2.2 points across all learning objectives, those with intermediate initial self-assessments by 1.1 points, and those with good or optimal T0-values by 0.1 points. Regarding the evaluation of the methods used, the use of SP was rated most positively, followed by the quantity of theory and practice and the use of video feedback.
Before discussing these results in terms of their possible implications for teaching social communication skills in medical school, some particularly methodological limitations of the study should be mentioned. In the first place, it represents a pre-post comparison, and thus only a quasi-experimental design [18]. It was not possible to conduct a (randomised) comparison of the course as the intervention with a control group (e.g. one with “traditional” training in communication skills), which would certainly have been helpful in appraising the results. This, however, is not uncommon in this domain [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29] and the pre-post comparison nonetheless allows a judgement of the competence gain. At the same time one might ask which external factors from the students’ environment could have improved these specific communication skills. Nevertheless, an earlier study with a control group, which found declines for some parameters in an intervention group with OSCE-training compared to a control group from a previous semester [30], shows that causal interpretations of the course effects in the present study should be treated cautiously.
Secondly, the mapping of the learning progress is based solely on the students’ self-assessments. An objectifying collection of data through performance assessments in the course was not desirable from a didactic point of view, and linking the results to the OSCE-marks was not straightforward for organisational reasons (however, the latter is intended for future academic years by the authors). Strictly speaking, learning objective self-assessments did not operationalise competencies or skills (which would have required observation sheets, SP surveys or theoretical tests [31]) but related self-efficacy expectancies (SEE). SEE are generally defined as the confidence in being able to perform target-oriented behaviour personally [32]. The more self-efficacious a person sees him- or herself the more likely he or she will be capable of performing the behaviour (i.e., showing the skill) in the future. Therefore the above mentioned limitation in this case is at least partly compensated by the fact that strong SEE are also an important intermediary between exercise-induced abilities in medical students and performance in exams such as an OSCE [33]. Thus, it can be assumed that the increased SEE actually have contributed to improved performance, which also could have been shown had pertinent measurements been available (see also [34]).
Thirdly, a self-developed questionnaire was used to model the specific learning objectives of the course as closely as possible. So on the one hand, comparability to other studies is limited and alternatively, it would have been possible to adapt the scales of Parle et al. [35] like, e.g., Ammentorp et al. did [36] (albeit, this would have implied a transfer from continuing training to undergraduate training). On the other hand, further analyses and experience with the present scales will have to show whether the numerically rather low learning progresses amongst students with high competency self-assessments at T0 represent ceiling effects or whether modified response scales might be able to show more significant changes in this subgroup as well.
Finally, no T1-questionnaire was received from 32.6% of the T0-participants. Here, as mentioned before it should be kept in mind that one missed session was permitted and due to the exam density at the end of the summer term, some students chose the final session as their missed session. It could be assumed that participation in T1 was selective in the sense that particularly students with positive self-assessments would have chosen to miss out on the final training session. However, the dropout analysis suggests that this effect was rather weak. Although all three significant (of seven total) comparisons in T0-competencies between T1-participants and non-participants showed higher values in the T1-participants, the level of these differences (0.3 to 0.4 scale points) is not likely an indication for strong “expert knowledge” on the side of the T1-participants. At the same time, even amongst the T1-participants those with relatively good self-assessments showed learning process, so that – given all T0- participants had participated in T1 – overall gains on average would at least not have reduced by negative changes. Since simultaneously gender, age and experience were not significantly associated with dropout, it does not seem to have seriously affected the study’s internal validity. Nonetheless, in the future organisational measures will be desirable in order to increase participation rates in T1, for example by providing an online version of the T1-questionnaire.
Overall, the results of the study indicate that the course contributes significantly to the teaching of social-communicative skills to MHH students. It takes up learning needs stated by the students. The learning progress as represented in the self-assessments points towards both the appropriateness of the content and methods of the course for the students and their acceptance of these. This is, not least of all, relevant in regards to the placement of the course in the second academic year, as some of the students in the introductory plenary sessions of the course expressed concern regarding insufficient medical knowledge for taking case histories and – in particular – disclosing diagnoses. Since this concern was not mentioned in the free text fields of the final questionnaire, it is likely that the course’s focus on communication skills was sufficiently successful. Although the OSCE as part of the final module exams certainly will also have had a motivating effect, from our point of view it was possible to impart the necessary orientation to the overall concept and its objectives to the students through the methodical and didactic structures of the course, which allowed consecutive and standardised teaching and learning.
The particularly positive evaluation of the SP as a didactic and methodical “medium” is consistent with the results of numerous other studies (for a summary see [4], [6], [7]) and with data from the T1 free text fields which were used by 53% of students and where 44 of 139 positive responses related to the SP. This encourages consolidation and improvement of this infrastructure, which has been used in preparing students for the OSCE since 2008, e.g. through further training in the feedback skills of the SP [37] and further development of role standards and other quality assurance measures [38]. The absence of criticism in the free text field of the T1-questionnaire regarding the interactive nature of role playing, which includes high levels of experiential learning and performing in front of fellow students [39], also speaks for the course concept. By splitting course groups into small groups in the sessions including SP as well and the explicit training of constructive feedback, students were introduced to performing in front of a group right from the outset of the course.
The significantly poorer (though still positive) evaluation of the amounts of theoretical and practical parts in the sessions are also reflected in the free text field data where from a total of 73 proposals for improvement 43 mention the need for more practice and less theory. Perhaps this balance is not optimal to date, especially with regard to the learning goals of communicating (among others) serious diagnoses, and as this is only specifically addressed as a topic from the fifth course session onwards. This has already led conceptual changes as part of the quality assurance and continuous development of the course concept following the 2009/10 academic year. These changes aim for the consistent teaching of the basics of medical communication using the topics of taking medical histories (1st course session) and breaking bad news (2nd session) so as to focus on the topics right from the outset.
Finally the rather moderately positive assessment of the use of video feedback points to another need for improvement in the course concept. Although this method has proven valuable in teaching communication skills [4], [24], it significantly increases the amount of time needed due to the presentation and discussion of the recordings. In this context, it is our experience that students tend to favour increasing the amount of role play against video analysis. It is a task for the development of the course concept to integrate this method more consistently and achieve a better balance between in-depth analysis and the number of simulations. In addition, infrastructure such as observation rooms with appropriate equipment (and mirrored glass walls such as in the Study Hospital Munster®) would be beneficial.
A further evaluation of the free text fields pointed towards “atmospheric” reasons for the success of the course. The professional, educational and personal competence of the tutors was positively mentioned in 51 cases. 14 mentions described the group size of 10 students as optimal. In addition, the opportunity for experiential learning in a way that respects individuality and the low threshold for more introverted students to get involved were perceived positively. More partner interviews and small group work within the groups of 10 were called for in nine cases.
Analyses stratified by gender and experience were not reported because they revealed only marginal differences. For example, the pre-post comparisons only showed a gender difference regarding confidence in approaching new patients, with men at T0 having slightly higher self-assessments (M=3.8 vs. 3.2) and women reporting slightly higher significant learning progress (0.8 vs. 0.5; p=.032). All other tests were not significant, as with the evaluation of methods. The mean differences of all learning needs, with a maximum of 0.4 points, were lower than the learning progress. All told, the differences indicate slightly more positive self-assessments of male students, which is consistent with more pronounced medical ideals in female medical students [40]. Nonetheless, gender-specific aspects in the present cohort of students appear of marginal relevance regarding the acquisition of communicative skills.
Overall, the positive evaluation of the communication course in our view represents a further empirical argument for a longitudinal social communication and doctor-patient communication curriculum at the MHH, which integrates and further develops existing curricula in a learning spiral [41]. In the long term, this could include evaluations which study the effects of such a curriculum on the subsequent performance of students and postgraduate doctors during the Practical Year or in professional practice (particularly as such effects are not without preconditions [42]).
In addition, we agree with the recommendations to strengthen cross-university and cross-faculty activities, not least of all in terms of valid and reliable examination methods [43]. This is supported by the expected efficiency gains. These are not least of all important because the implementation of teaching concepts such as the one evaluated here (practice-oriented teaching and learning in small groups of students and using SP) requires significant personnel, organisational and financial resources.
It is plausible that such efforts are particularly sustainable if longitudinal curricula covering all academic years become the standard in this area of competence. Ideally such (interdisciplinary is possible) activities are based on a consensus framework. A blueprint for such a model could be the British consensus paper [44]. It begins by defining respect as the basis of effective clinical communication and by discussing theory and evidence, the role of clinical communication, specific topics such as behaviour modification, media and communication beyond the patient lists virtually all relevant key issues. We hope that this evaluation study of one curricular block at the MHH will add to this overall process.
Notes
*APG-Teaching Team MHH (Doctor-Patient Communication Teaching Team MHH): Karin Lange (Coordinator), Ulrich Brinkmeier, Gundula Ernst, Angelika Kursch, Thomas von Lengerke, Thomas Schneller (Medical Psychology Unit); Siegfried Geyer (Coordinator), Anja Löbel, Friederike Otto, Stefanie Sperlich (Medical Sociology Unit); Eva Hummers-Pradier, Carsten Kruschinski, Heidrun Lingner, Christiane Müller, Erika Penner (Institute for General Practice); Uwe Hartmann, Susanne Philippsohn, Lotta Winter (Clinical Psychology Working Group at the Clinic for Psychiatry, Social Psychiatry and Psychotherapy); Burkard Jäger, Maike Möllenkamp, Angela Trieschmann (Clinic for Psychosomatics and Psychotherapy)
**Coordinator of the Longitudinal Internal Medicine Curriculum : Prof. Dr. Hermann Haller, M.D. (who has also lead the development of HannibaL as MHH’s Dean of Medicine and Postgraduate and Complementary Studies); Coordinator of the Module „Diagnostic Methods“: Dr. Saskia Merkel, M.D..
Acknowledgement
We would like to thank the students of the model medical curriculum HannibaL who started studying in 2008 for their participation in the study, and thus their willingness to complete yet another questionnaire in addition to the surveys conducted by the Evaluation Office at Hannover Medical School’s Academic Dean’s Office.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bundesministerium der Justiz. Approbationsordnung für Ärzte vom 27. Juni 2002. Berlin: Bundesministerium der Justiz; 2010. Available from: http://www.gesetze-im-internet.de/_appro_2002/BJNR240500002.html. [Google Scholar]
- 2.Hahn EG, Fischer MR. Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM) für Deutschland: Zusammenarbeit der Gesellschaft für Medizinische Ausbildung (GMA) und des Medizinischen Fakultätentages (MFT) GMS Z Med Ausbild. 2009;26(3):Doc35. doi: 10.3205/zma000627. Available from: http://dx.doi.org/10.3205/zma000627. [DOI] [Google Scholar]
- 3.Barrows HS. Simulated patients in medical training. Can Med Assoc J. 1968;98(14):674–676. [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz S, Silverman J, Draper J. Teaching and learning communicating skills in medicine. 2nd edition. Oxford: Radcliffe; 2004. [Google Scholar]
- 5.Fröhmel A, Burger W, Ortwein H. Einbindung von Simulationspatienten in das Studium der Humanmedizin in Deutschland. Dtsch Med Wochenschr. 2007;132(11):549–554. doi: 10.1055/s-2007-970375. Available from: http://dx.doi.org/10.1055/s-2007-970375. [DOI] [PubMed] [Google Scholar]
- 6.Rockenbauch K, Fabry G, Petersen C, Daig I, Philipp S. Der Einsatz von Schauspielpatienten in der Medizinischen Psychologie – allgemeiner Überblick und konkrete Umsetzungsbeispiele. Z Med Psychol. 2008;17(4):185–192. [Google Scholar]
- 7.Simmenroth-Nayda A, Chenot JF, Fischer Th, Scherer M, Stanske B, Kochen MM. Mit Laienschauspielern das ärztliche Gespräch trainieren. Dtsch Arztebl. 2007;104(13):A847–A852. [Google Scholar]
- 8.Bokken L, Rethans J-J, Jöbsis Q, Duvivier R, Scherpbier A, van der Vleuten C. Instructiveness of real patients and simulated patients in undergraduate medical education: a randomized experiment. Acad Med. 2010;85(1):148–154. doi: 10.1097/ACM.0b013e3181c48130. Available from: http://dx.doi.org/10.1097/ACM.0b013e3181c48130. [DOI] [PubMed] [Google Scholar]
- 9.Watzlawick P, Beavin JH, Jackson DD. Menschliche Kommunikation: Formen, Störungen, Paradoxien. Bern: Huber; 1969. [Google Scholar]
- 10.Schulz von Thun F. Miteinander reden. Reinbek: Rowohlt; 2008. [Google Scholar]
- 11.Kurtz S, Silverman J, Benson J, Draper J. Marrying content and process in clinical method teaching: enhancing the Calgary-Cambridge Guides. Acad Med. 2003;78(8):802–809. doi: 10.1097/00001888-200308000-00011. Available from: http://dx.doi.org/10.1097/00001888-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Silverman J, Kurtz S, Draper J. Skills for communicating with patients. 2nd edition. Oxford: Radcliffe; 2005. [Google Scholar]
- 13.Füeßl HS, Middeke M. Anamnese und klinische Untersuchung. 4. Auflage. Stuttgart: Thieme; 2010. [Google Scholar]
- 14.Baile W, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES–A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. doi: 10.1634/theoncologist.5-4-302. Available from: http://dx.doi.org/10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 15.Scheibler F, Janssen C, Pfaff H. Shared decision making: ein Überblicksartikel über die internationale Forschungsliteratur. Soz Praventivmed. 2003;48(1):11–23. doi: 10.1007/s000380300002. Available from: http://dx.doi.org/10.1007/s000380300002. [DOI] [PubMed] [Google Scholar]
- 16.Buser K, Schneller T, Wildgrube K. KLB Medizinische Psychologie - Medizinische Soziologie. 6. Auflage. München: Elsevier/Urban & Fischer; 2007. [Google Scholar]
- 17.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):63–67. doi: 10.1097/00001888-199009000-00045. Available from: http://dx.doi.org/10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 18.Mohr LB. Impact analysis for program evaluation. Chicago, Il: Dorsey Press; 1988. [Google Scholar]
- 19.Bahrs O. Kommunikationsförderung in der Vor-Klinik – Kursus der Medizinischen Psychologie und Medizinischen Soziologie. Z Med Psychol. 2010;19(2):97–101. [Google Scholar]
- 20.Brenk-Franz K, Kubieziel H, Schulz S, Gensichen J. Simulationspatienten in der allgemeinmedizinischen Lehre: Das Jenaer Programm – eine Pilotstudie. Z Allg Med. 2010;86(4):152–158. [Google Scholar]
- 21.Fischbeck S, Mauch M, Leschnik E, Laubach W. Entwicklung und Evaluation einer OSCE für die Überprüfung kommunikativer ärztlicher Kompetenz im Kursus der Medizinischen Psychologie und Medizinischen Soziologie. Z Med Psychol. 2010;19(2):94–96. [Google Scholar]
- 22.Fischer T, Chenot J-F, Kleiber C, Kochen MM, Simmenroth-Nayda A, Staats H, Hermann-Lingen C. Kurs „ärztliche Basisfähigkeiten“ – Evaluation eines primärärztlichen orientierten Unterrichtskonzeptes im Rahmen der neuen Approbationsordnung. GMS Z Med Ausbild. 2005;22(3):Doc59. Available from: http://www.egms.de/de/journals/zma/2005-22/zma000059.shtml. [Google Scholar]
- 23.Koerfer A, Köhle K, Obliers R, Sonntag B, Thomas W, Albus C. Training und Prüfung kommunikativer Kompetenz. Aus- und Fortbildungskonzepte zur ärztlichen Gesprächsführung. Gesprächsforschung. 2008;9:34–78. Available from: http://www.gespraechsforschung-ozs.de/heft2008/ag-koerfer.pdf. [Google Scholar]
- 24.Kopecky-Wenzel M, Maier EM, Muntau AC, Reinhardt D, Frank R. Überbringen schlechter Nachrichten – videogestützte Trainingseinheit für Medizinstudenten. Z Kinder Jugendpsychiatr Psychother. 2009;37(2):139–144. doi: 10.1024/1422-4917.37.2.139. Available from: http://dx.doi.org/10.1024/1422-4917.37.2.139. [DOI] [PubMed] [Google Scholar]
- 25.Mitzkat A, Schulz C, Kasenda B, Langer T, Schnell MW. „ARZT IM GANZEN SPREKTRUM“: Die INTEGRIERTEN CURRICULA der Medizinerausbildung an der Universität Witten/Herdecke – Rückblick auf sechs Jahre Lehre im Hinblick auf Praxisorientiertung und theoretische Vorgaben. GMS Z Med Ausbild. 2006;23(4):Doc66. Available from: http://www.egms.de/static/de/journals/zma/2006-23/zma000285.shtml. [Google Scholar]
- 26.Petersen C, Busche W, Bergelt C, Huse-Kleinstoll G. Kommunikationstraining als Teil des Medizinstudiums: Ein Modellversuch. GMS Z Med Ausbild. 2005;22(1):Doc08. Available from: http://www.egms.de/static/de/journals/zma/2005-22/zma000008.shtml. [Google Scholar]
- 27.Philipp S, Merten K. Erfahrungen mit Standardisierten Patienten im neuen Lehrkonzept zur Vermittlung kommunikativer Kompetenzen im Fach Medizinische Psychologie – das Jenaer Modell. Z Med Psychol. 2006;15(1):11–19. [Google Scholar]
- 28.Pucher-Matzner I, Gleiss A, Schmidts M, Frischenschlager O. Die Checkliste PD „Professionelles ärztliches Kommunikationsverhalten“ in Unterricht und Evaluation kommunikativer Fertigkeiten im Medizinstudium. GMS Z Med Ausbild. 2006;23(4):Doc68. Available from: http://www.egms.de/static/de/journals/zma/2006-23/zma000287.shtml. [Google Scholar]
- 29.Wiesmann U, Niehörster G, Hannich H-J. Medizinpsychologische Lehre innovativ gestalten: Förderung von Kommunikations- und Forschungskompetenzen in der vorklinischen Ausbildung. Z Med Psychol. 2009;18(2):88–96. [Google Scholar]
- 30.Kopp V, Schewe S. Kann durch Training Anamnese und klinische Untersuchung vermittelt werden? GMS Z Med Ausbild. 2005;22(1):Doc15. Available from: http://www.egms.de/static/de/journals/zma/2005-22/zma000015.shtml. [Google Scholar]
- 31.Duffy FD, Gordon GH, Whelan G, Cole-Kelly K, Frankel R All Participants in the American Academy on Physician and Patient’s Conference on Education and Evaluation of Competence in Communication and Interpersonal Skills. Assessing competence in communication and interpersonal skills: the Kalamazoo II Report. Acad Med. 2004;79(6):495–507. doi: 10.1097/00001888-200406000-00002. Available from: http://dx.doi.org/10.1097/00001888-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997. [Google Scholar]
- 33.Mavis B. Self-efficacy and OSCE performance among second year medical students. Adv Health Sci Educ. 2001;6(2):93–102. doi: 10.1023/A:1011404132508. Available from: http://dx.doi.org/10.1023/A:1011404132508. [DOI] [PubMed] [Google Scholar]
- 34.Schultz JH, Schönemann J, Lauber H, Nikendei C, Herzog W, Jünger J. Einsatz von Simulationspatienten im Kommunikations- und Interaktionstraining für Medizinerinnen und Mediziner (Medi-KIT): Bedarfsanalyse – Training – Perspektiven. Gruppendynamik Organisationsberatung. 2007;38(1):7–23. doi: 10.1007/s11612-007-0002-y. Available from: http://dx.doi.org/10.1007/s11612-007-0002-y. [DOI] [Google Scholar]
- 35.Parle M, Maguire P, Heaven C. The development of a training model to improve health professionals’ skills, self-efficacy and outcome expectancies when communicating with cancer patients. Soc Sci Med. 1997;44(2):231–240. doi: 10.1016/S0277-9536(96)00148-7. Available from: http://dx.doi.org/10.1016/S0277-9536(96)00148-7. [DOI] [PubMed] [Google Scholar]
- 36.Ammentorp J, Sabroe S, Kofoed P-E, Mainz J. The effect of training in communication skills on medical doctors’ and nurses’ self-efficacy: a randomized controlled trial. Patient Educ Couns. 2007;66(3):270–277. doi: 10.1016/j.pec.2006.12.012. Available from: http://dx.doi.org/10.1016/j.pec.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Bokken L, Linssen T, Scherpbier A, van der Vleuten C, Rethans JJ. Feedback by simulated patients in undergraduate medical education: a systematic review of the literature. Med Educ. 2009;43(3):202–210. doi: 10.1111/j.1365-2923.2008.03268.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2008.03268.x. [DOI] [PubMed] [Google Scholar]
- 38.Cleland JA, Abe K, Rethans J-J. The use of simulated patients in medical education: AMEE Guide No 42. Med Teach. 2009;31(6):477–486. doi: 10.1080/01421590903002821. Available from: http://dx.doi.org/10.1080/01421590903002821. [DOI] [PubMed] [Google Scholar]
- 39.Dieckmann P, Rall M, Eich C, Schnabel K, Jünger J, Nikendei C. Rollenspiel als wesentliches Element bei Simulationsverfahren in der Medizin. Z Evid Fortbild Qual Gesundhwes. 2008;102(10):642–647. doi: 10.1016/j.zefq.2008.11.020. Available from: http://dx.doi.org/10.1016/j.zefq.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 40.Schrauth M, Kowalski A, Weyrich P, Begenau J, Werner A, Zipfel S, Nikendel C. Selbstbild, Arztbild und Arztideal: Ein Vergleich Medizinstudierender 1981 und 2006. Psychother Psych Med. 2009;59(12):446–453. doi: 10.1055/s-0029-1202343. Available from: http://dx.doi.org/10.1055/s-0029-1202343. [DOI] [PubMed] [Google Scholar]
- 41.Bachmann C, Hölzer H, Dieterich A, Fabry G, Langewitz W, Lauber H, Ortwein H, Pruskil S, Schubert S, Sennekamp M, Simmenroth-Nayda A, Silbernagel W, Scheffer S, Kiessling C. Longitudinales, bologna-kompatibles Modell-Curriculum „Kommunikative und soziale Kompetenzen“: Ergebnisse eines interdisziplinären Workshops deutschsprachiger medizinischer Fakultäten. GMS Z Med Ausbild. 2009;26(4):Doc38. doi: 10.3205/zma000631. Available from: http://dx.doi.org/10.3205/zma000631. [DOI] [Google Scholar]
- 42.Stimmel B, Cohen D, Fallar R, Smith L. The use of standardised patients to assess clinical competence: does practice make perfect? Med Educ. 2006;40(5):444–449. doi: 10.1111/j.1365-2929.2006.02446.x. Available from: http://dx.doi.org/10.1111/j.1365-2929.2006.02446.x. [DOI] [PubMed] [Google Scholar]
- 43.Kiessling C, Dieterich A, Fabry G, Hölzer H, Langewitz W, Mühlinghaus I, Pruskil S, Scheffer S, Schubert S. Basler Consensus Statement „Kommunikative und soziale Kompetenzen im Medizinstudium“: Ein Positionspapier des GMA-Ausschusses Kommunikative und soziale Kompetenzen. GMS Z Med Ausbild. 2008;25(2):Doc83. Available from: http://www.egms.de/static/de/journals/zma/2008-25/zma000567.shtml. [Google Scholar]
- 44.von Fragstein M, Silverman J, Cushing A, Quilligan S, Salisbury H, Wiskin C UK Council for Clinical Communication Skills Teeaching in Undergraduate Medical Education. UK consensus statement on the content of communication curricula in undergraduate medical education. Med Educ. 2008;42(11):1100–1107. doi: 10.1111/j.1365-2923.2008.03137.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2008.03137.x. [DOI] [PubMed] [Google Scholar]