Abstract
Background
The purpose of this study was to evaluate the correlation between contrast sensitivity and calculated higher-order aberrations based on individual natural pupil diameter after cataract surgery.
Methods
This prospective study included 120 eyes from 92 patients who were randomized to receive one of four lenses, including three aspheric lenses (Acrysof SN60WF, Tecnis ZA9000, and Hoya Py60AD) and one spherical lens (Acrysof SN60AT). Contrast sensitivity, higher-order aberrations of the whole eye, and pupil diameter under photopic and mesopic conditions were measured 1 month postoperatively. Higher-order aberrations were decomposed into Zernike coefficients, calculated according to individual pupil diameter. The correlation between higher-order aberrations and contrast sensitivity was evaluated.
Results
There were no significant differences in contrast sensitivity function between the four types of lenses under photopic conditions. However, the contrast sensitivity function and area under log contrast sensitivity function in the aspheric lenses were significantly better than in the spherical lens under mesopic conditions. Under mesopic conditions, spherical aberration in eyes with aspheric lenses was significantly lower than in eyes with spherical lenses (P < 0.05). Under photopic conditions, coma aberration had a significant negative correlation with contrast sensitivity at 12 cycles/degree. Under mesopic conditions, spherical aberration had a significant negative correlation with contrast sensitivity at 3, 6, and 12 cycles/degree with glare, and with contrast sensitivity at 6 and 18 cycles/degree without glare.
Conclusion
In terms of influence on visual function, coma aberration may be more significant under photopic conditions and spherical aberration under mesopic conditions.
Keywords: mesopic conditions, spherical aberration, wavefront, photopic and mesopic conditions
Introduction
Advances in intraocular lens (IOL) and phacoemulsification technology have enabled cataract surgery to achieve better postoperative visual quality, as well as safe removal of opaque lenses, a precise refractive outcome, and restoration of excellent visual acuity.1–3 In addition, the methodology for evaluating optical and visual function has developed as laser corneal refractive surgery has advanced,4–7 and has been applied to normal eyes8 and in ocular pathologies, such as cataract9 and dry eye.10,11 In other words, wavefront analysis which quantifies low-order and high-order aberrations can explain the decrease in visual function, measured by contrast sensitivity testing, which could not be detected by conventional visual acuity testing. Use of these measurements has opened up a whole new possibility for evaluating postoperative results and to predict, customize, and correct ocular aberrations and residual refractive error after cataract surgery using aspheric and light-adjustable IOLs.12–17
Aspheric IOLs are available today, and a number of peer-reviewed articles show their benefits in different ways and under different conditions,18–20 despite intraindividual variations in corneal spherical aberration.21 Many reports have demonstrated a decrease in spherical aberration for fixed pupil diameters of 3–6 mm. These studies compared spherical aberration after instillation of cycloplegic agents and visual function between aspheric IOLs and spherical IOLs. In a previous study, we found that spherical aberration has an important effect on postoperative visual function, even when the spherical aberration is calculated based on the natural pupil diameter in individual patients.20 The purpose of this study was to determine in detail the correlation between contrast sensitivity and the calculated wavefront aberration based on individual natural pupil diameter and to elucidate optimized amounts of wavefront aberrations after cataract surgery.
Methods and materials
One hundred and twenty consecutive eyes from 92 cataract patients (36 males, 56 females, average age 68.6 ± 9.1 years) who underwent cataract extraction and implantation of acrylic IOLs at Keio University Hospital between October 2007 and December 2009 were included in this prospective study. Patients with significant senile cataract and postoperative visual acuity better than 20/20 were eligible for inclusion in the study. Exclusion criteria were previous or coexistent ocular pathology and complications during cataract surgery or postoperatively. Written informed consent was obtained from all participants. This study was performed in accordance with the tenets of the Declaration of Helsinki.
Patients were randomized to receive one of the following IOLs, including three types of aspheric lenses (Acrysof IQ SN60WF [Alcon, Fort Worth, TX, 30 eyes; WF group], Tecnis ZA9003 [AMO, Santa Ana, CA, 30 eyes; Tecnis group], PY60AD [Hoya, Tokyo, Japan, 30 eyes; Hoya group]) and one type of spherical lens SN60AT [Alcon, 30 eyes; AT group]. Patient demographics are shown in Table 1. The average IOL powers (range) were 19.6 ± 4.5 D (6.0 to 24.0 D) in eyes with Acrysof IQ SN60WF, 20.3 ± 3.5 D (11.0 to 25.5 D) in eyes with Tecnis ZA9003, 18.8 ± 4.1 D (10.0 to 24.0 D) in eyes with PY60AD, and 19.3 ± 3.8 D (12.0 to 24.5 D) in eyes with SN60AT (Table 1). There was no significant difference in the average IOL powers, age, and postoperative refraction, astigmatism, and pupil diameters under photopic and mesopic conditions between the three types of aspheric and one type of spherical IOLs (Kruskal–Wallis test, P > 0.05).
Table 1.
Demographics of the four groups
| WF group | Tecnis group | Hoya group | AT group | |
|---|---|---|---|---|
| IOL | SN60WF | ZA9003 | PY60AD | SN60AT |
| Intended SA correction for 6 mm diameter (μm) | 0.20 | 0.27 | 0.18 | – |
| Eyes (n) | 30 | 30 | 30 | 30 |
| Age (years) | 68.7 ± 9.9 | 68.6 ± 3.8 | 68.5 ± 9.0 | 68.1 ± 8.7 |
| Gender | ||||
| Male/Female | 14/16 | 16/14 | 15/15 | 12/18 |
| IOL power (D) | 19.6 ± 4.5 | 20.3 ± 3.5 | 18.8 ± 4.1 | 19.3 ± 3.8 |
| Range | 6–24 | 11–25.5 | 10–24 | 12–24.5 |
| Postoperative refraction | ||||
| SE (D) | −1.2 ± 1.3 | −0.7 ± 1.1 | −0.7 ± 1.4 | −0.8 ± 1.2 |
| Astigmatism (D) | −1.0 ± 0.5 | −1.2 ± 1.0 | −0.9 ± 0.5 | −1.1 ± 0.6 |
| Pupil diameter (mm) | ||||
| Photopic | 3.03 ± 0.63 | 2.75 ± 0.62 | 2.81 ± 0.55 | 2.87 ± 0.38 |
| Mesopic | 4.08 ± 0.70 | 4.22 ± 0.89 | 3.93 ± 0.58 | 4.26 ± 0.59 |
Abbreviations: IOL, intraocular lens; D, diopter; SE, spherical equivalent.
Surgical techniques
All surgeries were performed by one of two experienced surgeons (TY and KN). After topical or sub-Tenon’s anesthesia with 2% lidocaine, a 2.2 mm (Acrysof IQ SN60WF, SN60AT, and PY60AD) or 2.75 mm (Tecnis) corneoscleral incision made at the 12 o’clock position. Sodium hyaluronate viscoelastic (1%, OpeganHi, Santen, Osaka, Japan) was used to reform and stabilize the anterior chamber and protect the endothelial cells. A 5.0–5.5 mm continuous curvilinear capsulorrhexis was created with a 27-gauge needle and the nucleus was removed by a standard phacoemulsification technique using the Infiniti (Alcon Surgical, Fort Worth, TX) or CV24000 (Nidek, Gamagori, Japan) phaco device. The IOLs were injected into the capsular bag in all eyes using an injector system. Tecnis ZA9003 IOLs were implanted using the AMO Unfolder Emerald Series. The Acrysof IQ and SN60AT IOLs were implanted using the Monarch injector system. The Hoya PY60AD IOLs were implanted using the Hoya preload system. The viscoelastic agent was completely removed at the end of the procedure. Postoperative medications included levofloxacin (Cravit, Santen, Osaka, Japan), 0.1% diclofenac sodium (Diclod, Wakamoto, Tokyo, Japan), and 0.01% betamethasone sodium phosphate (Sanbetazon, Santen, Osaka, Japan), prescribed three times a day for 1 month.
Measurements
Corrected distance visual acuity, contrast sensitivity, higher-order aberrations, and pupil diameter under photopic and mesopic conditions were measured 1 month after cataract surgery. Contrast sensitivity testing was measured at six spatial frequencies of 1.5, 3, 6, 12, and 18 cycles per degree (cpd) 1 month after surgery using the Optec 6500 vision testing system (Stereo Optical Co Inc, Chicago, IL) with best spectacle correction under photopic conditions (85 candela/m2) and mesopic conditions (3 candela/m2) with or without glare. The wavefront analysis was conducted under mesopic conditions (0.35 candela/m2) without administering cycloplegic agent 1 month after surgery using ARK-10000 (OPD-Scan, Nidek, Gamagori, Japan). ARK-10000 is based on the dynamic skiascopy principle, ie, an infrared light slit and photodetectors are placed on a rotating wheel along the same rotational position across the pupil.22,23 By rotating the wheel, the instrument measures the time for light to peak at each photodiode, and by comparing the results with the theoretical reference time, the optical pathway difference and related wavefront error are calculated. This procedure yields 1440 data points within 0.4 seconds. The wavefront data was obtained after 1-minute dark adaptation. A single measurement of pupil and wavefront aberration was taken for each eye when the image quality and data obtained were of satisfactory, good quality. If well focused or properly aligned images of the eye could not be obtained, the measurement was repeated until images of suitable quality were acquired.
The pupil diameter was measured using FP-10000 (TMI, Saitama, Japan) under photopic (150 candela/m2) and mesopic (0.35 candela/m2) conditions without pharmacologic treatment. FP-10000 is a handheld digital infrared pupillometer. Pupil diameter under mesopic conditions was measured after 1 minute of dark adaptation at 0.35 candela/m2. Depth of focus was measured by an accommodometer (D’Acomo, WOC, Kyoto, Japan) without covering the fellow eye. A spheric lens of +2 or +3 dioptor was added to the full distance correction, and patients were required to look at the cross target. The target was slowly brought closer until the patient reported blurring of the cross image. The measurement was repeated three times, and the average distance in dioptor was recorded as the near point of accommodation. The depth of focus was defined as the difference in dioptor between the near and far points.
Analysis
The area under log contrast sensitivity function (AULCSF) was determined according to the method of Applegate et al.24 The log of the contrast sensitivity was plotted as a function of the log spatial frequency, and third-order polynomials were fitted to the data. The fitted function was integrated between 0.176 (corresponding to 1.5 cpd) and 1.08 (corresponding to 18 cpd), and the resulting value was defined as the AULCSF.24
The wavefront maps were analyzed up to the eighth-order Zernike coefficients using the individual pupil diameter under photopic and mesopic conditions. The root mean square of the third-order, fourth-order, and total higher-order aberrations were calculated. S3 and S4 represent the root mean square of the third-order and fourth-order Zernike coefficients, respectively. Total higher-order aberration represents the root mean square from third-order to eighth-order Zernike coefficients.
Statistical analysis
A P value less than 0.05 was considered statistically significant. The Mann–Whitney U test was used to evaluate differences in pupil diameter and wavefront aberrations between aspheric and spheric IOL groups, and the Kruskal–Wallis test was used to evaluate differences between the four groups. A Pearson correlation analysis was used to evaluate correlations between contrast sensitivity, AULCSF, and wavefront aberrations under photopic and mesopic conditions. All statistical analyses were performed using SSRI (SSRI Co Ltd, Tokyo, Japan) computer software.
Results
The preoperative and postoperative logarithms of minimal angle resolution (logMAR) were 0.28 ± 0.43 and −0.07 ± 0.07, respectively. The logMAR significantly improved after surgery (P < 0.001). No eyes had any postoperative complications. Postoperative slit-lamp examination in mydriasis showed well-centered IOLs in the capsular bag in all eyes. There was no evidence of posterior capsule opacification or anterior capsule shrinkage at the time of testing.
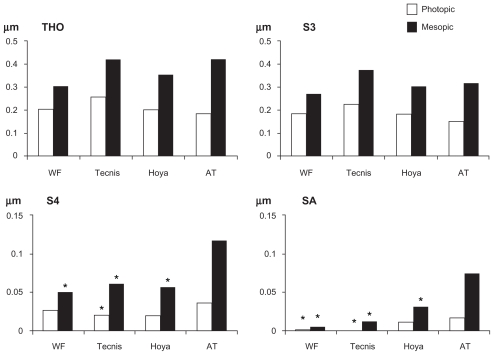
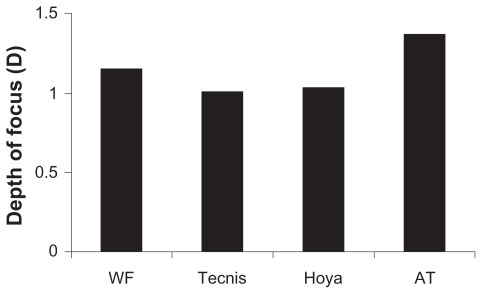
Figure 1 shows the ocular wavefront aberrations according to individual pupil diameter under photopic and mesopic conditions. Under photopic conditions, S4 and spheric aberration in the Tecnis group were significantly lower than in the AT group. Spheric aberration in the WF group was significantly lower than in the AT group. There were no significant differences in total higher-order aberration and S3 between the four groups. Under mesopic conditions, although there were no significant differences in total higher-order aberration and S3 between the four groups, S4 and spheric aberration in the three aspheric IOL groups was significantly lower than in the AT group. There were no significant differences in depth of focus between the groups (Figure 2).
Figure 1.
Higher order aberrations in each group.
Note: *P < 0.05 compared with AT group.
Figure 2.
Depth of focus in each group.
Table 2 shows the results of contrast sensitivity and AULCSF. As shown in Table 2, there were no significant differences in contrast sensitivity and AULCSF between the four groups under photopic and mesopic conditions without glare (P > 0.05). Only under mesopic conditions with glare, AULCSF and contrast sensitivity at 6 cpd in the aspheric IOL groups was significantly better when compared with the AT group (P = 0.04 for the WF group, P = 0.02 for the Tecnis group, and P = 0.01 for the Hoya group).
Table 2.
Contrast sensitivity and AULCSF in each group
| WF group | Tecnis group | Hoya group | AT group | |
|---|---|---|---|---|
| Photopic, without glare | ||||
| 1.5 cpd* | 1.46 ± 0.22 | 1.40 ± 0.15 | 1.49 ± 0.19 | 1.47 ± 0.19 |
| 3 cpd* | 1.68 ± 0.21 | 1.72 ± 0.23 | 1.76 ± 0.20 | 1.75 ± 0.18 |
| 6 cpd* | 1.73 ± 0.24 | 1.73 ± 0.24 | 1.77 ± 0.21 | 1.75 ± 0.24 |
| 12 cpd* | 1.29 ± 0.40 | 1.24 ± 0.42 | 1.21 ± 0.45 | 1.13 ± 0.34 |
| 18 cpd* | 0.80 ± 0.47 | 0.78 ± 0.44 | 0.74 ± 0.47 | 0.65 ± 0.49 |
| AULCSF* | 1.65 ± 0.23 | 1.64 ± 0.26 | 1.65 ± 0.23 | 1.64 ± 0.27 |
| Photopic, with glare | ||||
| 1.5 cpd* | 1.46 ± 0.20 | 1.46 ± 0.19 | 1.45 ± 0.21 | 1.48 ± 0.24 |
| 3 cpd* | 1.69 ± 0.20 | 1.70 ± 0.20 | 1.71 ± 0.22 | 1.73 ± 0.23 |
| 6 cpd* | 1.70 ± 0.20 | 1.73 ± 0.18 | 1.77 ± 0.21 | 1.74 ± 0.26 |
| 12 cpd* | 1.27 ± 0.33 | 1.29 ± 0.44 | 1.21 ± 0.52 | 1.21 ± 0.46 |
| 18 cpd* | 0.66 ± 0.50 | 0.75 ± 0.53 | 0.63 ± 0.50 | 0.63 ± 0.50 |
| AULCSF* | 1.64 ± 0.21 | 1.66 ± 0.24 | 1.64 ± 0.23 | 1.65 ± 0.27 |
| Mesopic, without glare | ||||
| 1.5 cpd* | 1.57 ± 0.22 | 1.56 ± 0.24 | 1.56 ± 0.22 | 1.55 ± 0.19 |
| 3 cpd* | 1.68 ± 0.20 | 1.73 ± 0.23 | 1.74 ± 0.17 | 1.66 ± 0.19 |
| 6 cpd* | 1.57 ± 0.21 | 1.61 ± 0.26 | 1.60 ± 0.23 | 1.48 ± 0.36 |
| 12 cpd* | 0.56 ± 0.63 | 0.78 ± 0.58 | 0.81 ± 0.57 | 0.63 ± 0.57 |
| 18 cpd* | 0.28 ± 0.49 | 0.26 ± 0.36 | 0.34 ± 0.43 | 0.18 ± 0.28 |
| AULCSF* | 1.45 ± 0.31 | 1.49 ± 0.29 | 1.51 ± 0.25 | 1.38 ± 0.27 |
| Mesopic, with glare | ||||
| 1.5 cpd* | 1.41 ± 0.23 | 1.44 ± 0.23 | 1.43 ± 0.19 | 1.36 ± 0.26 |
| 3 cpd* | 1.59 ± 0.25 | 1.57 ± 0.23 | 1.58 ± 0.25 | 1.53 ± 0.24 |
| 6 cpd** | 1.44 ± 0.33 | 1.46 ± 0.22 | 1.57 ± 0.25 | 1.17 ± 0.62 |
| 12 cpd* | 0.45 ± 0.56 | 0.51 ± 0.61 | 0.47 ± 0.60 | 0.39 ± 0.51 |
| 18 cpd* | 0.20 ± 0.39 | 0.21 ± 0.36 | 0.20 ± 0.25 | 0.08 ± 0.20 |
| AULCSF* | 1.30 ± 0.28 | 1.32 ± 0.25 | 1.34 ± 0.25 | 1.16 ± 0.36 |
Notes: Mann–Whitney U test P < 0.05 compared with AT group; Kruskal–Wallis test *P > 0.05, **P = 0.0385.
Abbreviations: AULCSF, area under the log contrast sensitivity function; cpd, cycle per degree.
Table 3 shows the correlation between contrast sensitivity and ocular wavefront aberration. Under photopic conditions with and without glare, total higher-order aberration and S3 had significant negative correlations with contrast sensitivity at 12 cpd. Under photopic conditions without glare, spheric aberration had significant negative correlations with contrast sensitivity at 3 cpd and 6 cpd.
Table 3.
Correlation coefficients and P value of Pearson’s correlation analysis between higher-order aberrations, pupil diameter, contrast sensitivity function, and AULCSF in all eyes (n = 120)
| THO | S3 | S4 | SA | P.D. | |
|---|---|---|---|---|---|
| Photopic, without glare | |||||
| 1.5 cpd | −0.21 (0.02) | −0.20 (0.03) | −0.14 (0.14) | −0.11 (0.22) | −0.12 (0.20) |
| 3 cpd | −0.13 (0.18) | −0.10 (0.18) | 0.02 (0.79) | −0.19 (0.04) | −0.06 (0.48) |
| 6 cpd | −0.13 (0.15) | −0.12 (0.18) | 0.005 (0.95) | −0.20 (0.02) | −0.06 (0.51) |
| 12 cpd | −0.27 (< 0.01) | −0.23 (0.01) | −0.16 (0.07) | −0.18 (0.06) | −0.03 (0.76) |
| 18 cpd | −0.14 (0.11) | −0.12 (0.20) | −0.10 (0.29) | −0.12 (0.17) | 0.10 (0.25) |
| Photopic, with glare | |||||
| 1.5 cpd | −0.08 (0.43) | −0.06 (0.58) | −0.11 (0.21) | −0.08 (0.34) | −0.02 (0.80) |
| 3 cpd | −0.17 (0.07) | −0.14 (0.12) | −0.15 (0.11) | −0.14 (0.12) | −0.07 (0.41) |
| 6 cpd | −0.14 (0.12) | −0.13 (0.16) | −0.11 (0.24) | −0.13 (0.17) | 0.04 (0.67) |
| 12 cpd | −0.22 (0.01) | −0.18 (0.04) | −0.10 (0.28) | −0.11 (0.23) | 0 (0.97) |
| 18 cpd | −0.12 (0.16) | −0.10 (0.25) | −0.05 (0.58) | −0.15 (0.11) | 0.01 (0.91) |
| Mesopic, without glare | |||||
| 1.5 cpd | −0.02 (0.79) | −0.01 (0.90) | −0.04 (0.68) | −0.14 (0.11) | −0.03 (0.70) |
| 3 cpd | −0.10 (0.28) | −0.08 (0.35) | −0.10 (0.25) | −0.23 (< 0.01) | −0.07 (0.40) |
| 6 cpd | −0.16 (0.07) | −0.12 (0.18) | −0.27 (< 0.01) | −0.37 (< 0.01) | −0.07 (0.45) |
| 12 cpd | −0.07 (0.43) | −0.05 (0.58) | −0.04 (0.65) | −0.20 (0.02) | 0 (0.92) |
| 18 cpd | −0.09 (0.32) | −0.04 (0.69) | −0.10 (0.28) | −0.08 (0.37) | −0.02 (0.78) |
| Mesopic, with glare | |||||
| 1.5 cpd | −0.04 (0.62) | 0 (0.95) | 0.05 (0.60) | 0 (0.90) | 0.11 (0.21) |
| 3 cpd | −0.10 (0.24) | −0.07 (0.40) | 0.04 (0.70) | −0.06 (0.47) | 0.09 (0.33) |
| 6 cpd | −0.15 (0.08) | −0.14 (0.12) | −0.24 (< 0.01) | −0.25 (< 0.01) | −0.02 (0.78) |
| 12 cpd | −0.05 (0.54) | −0.03 (0.74) | 0.03 (0.76) | −0.10 (0.26) | 0.09 (0.27) |
| 18 cpd | −0.02 (0.85) | 0 (0.99) | −0.02 (0.84) | −0.18 (0.04) | 0.03 (0.70) |
Note: numbers in bold are statistically significant at P < 0.05.
Abbreviations: PD, pupil diameter; cpd, cycle per degree; THO, total higher order aberration; S3, RMS of third-order aberration; S4, RMS of fourth-order aberration; SA, spherical aberration; RMS, root mean square.
Under mesopic conditions, spheric aberration had a significant negative correlation with contrast sensitivity at 3, 6, and 12 cpd with glare, and with contrast sensitivity at 6 and 18 cpd without glare, although total higher-order aberration and S3 had no significant correlation with contrast sensitivity.
Discussion
We evaluated the relationship between postoperative ocular wavefront aberration and contrast sensitivity in eyes with three different types of aspheric IOLs and one type of spheric IOL under photopic and mesopic conditions. We demonstrated that, when ocular wavefront aberrations were calculated in accordance with individual pupil diameter, coma-like aberration (S3) had a negative correlation with contrast sensitivity at specific frequencies only under photopic conditions, whereas spherical aberration had a negative correlation with contrast sensitivity under mesopic conditions.
In this study, there were no significant differences in contrast sensitivity between the aspheric IOLs and the spherical IOL under photopic conditions. The effectiveness of aspheric IOLs in improving visual function has been well established by previous studies.25–35 We postulate that the results of this study might be due to the weak effect of the asphericity of the IOLs within individual pupil diameter under photopic conditions. In this case series, the average pupil diameters were around 3 mm under photopic conditions and 4 mm under mesopic conditions in the four groups. In a previous study in which we demonstrated that the amounts of spherical aberration correction in aspheric IOLs were dependent on the analysis diameter and varied with IOL types, the amounts of correction of spherical aberration were nearly 0 μm at a 3 mm pupil diameter and 0.05–0.1 μm at a 4 mm pupil diameter for all types of aspheric IOLs.36 That is, the ability of aspheric IOLs to decrease spherical aberration is limited at pupil diameters of 3–4 mm. For this reason, it might be reasonable to expect that there would be no differences in visual function between the aspheric and spherical IOLs, although there was a significant negative correlation between spheric aberration and contrast sensitivity.
Interestingly, in the current study, spheric aberration had a negative correlation with contrast sensitivity at 3 cpd and 6 cpd under photopic and mesopic conditions, whereas comalike aberration (S3) had a negative correlation with contrast sensitivity at 1.5 cpd and 12 cpd under photopic conditions. In other words, different types of aberration might have effects on contrast sensitivity at different spatial frequencies. Cuthbertson et al reported that an aspheric IOL performed better than a spherical IOL with significant differences at 3 cpd and 6 cpd.29 The results obtained here are almost consistent with findings in the previous study. Further studies will reveal valuable information to explain the deterioration of contrast sensitivity function at specific frequencies due to the increase of specific types of higher-order aberration.
Depth of focus tended to be smaller in eyes with aspheric IOLs than those with the spheric IOL. However, there were no significant differences. Oshika et al reported that comatic-like aberration of the cornea, along with corneal multifocality, contributed to the apparent accommodation in pseudophakic eyes.37 In their report, coma-like aberration of the subjects ranged from 0 μm to 0.8 μm, which was relatively large. Tabernero et al used a “virtual surgery” approach to predict the optical performance of IOLs, and reported that the average depths of focus were similar for aspheric and spheric IOLs.38
A weakness of our study is that it was not performed with an intraindividual clinical study design. Contrast sensitivity is affected by individual differences, partly due to optical quality, such as wavefront aberration, and partly due to neural processing. Comparison of contrast sensitivity between the four types of IOLs might be influenced by individual differences in neural processing. Another limitation of this study was the age distribution of the subjects. We included subjects aged 49–85 years (mean 68.7 ± 8.7 years) and did not include younger subjects, because the subjects were selected from those who underwent cataract surgery, and thus, younger subjects were seldom included. In general, contrast sensitivity function has been reported to be age-related. 39–42 The limited age distribution in this study might make it possible to avoid the effects of subject age on visual function. Further evaluation is needed to confirm these results in younger normal subjects.
To our knowledge, this is the first study to find that coma aberration may be more significant under photopic conditions and spherical aberration under mesopic conditions when higher-order aberrations are calculated according to individual pupil diameter. Previous studies comparing visual function between aspheric and spherical IOLs demonstrated that aspheric IOLs provide better optical quality. However, the optimal wavefront aberration remains unknown because the interaction between complicated Zernike coefficients can both improve and reduce visual performance,43 although many reports have demonstrated that the contrast sensitivity function is compromised by an increase in higher-order aberrations in normal eyes8 following keratorefractive surgery6 and implantation of IOLs.20,44 Negative spherical aberration around 0.05 μm might provide better optical quality, as reported by Wang et al in their theoretical studies.45,46
In conclusion, there were significant negative correlations between wavefront aberration and contrast sensitivity function when wavefront aberration was calculated based on individual pupil diameter, which also indicated that calculated wavefront aberration based on individual pupil diameter reflected visual function well.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Liu Y, Zeng M, Liu X, et al. Torsional mode versus conventional ultrasound mode phacoemulsification: randomized comparative clinical study. J Cataract Refract Surg. 2007;33:287–292. doi: 10.1016/j.jcrs.2006.10.044. [DOI] [PubMed] [Google Scholar]
- 2.Verhulst E, Vrijghem JC. Accuracy of intraocular lens power calculations using the Zeiss IOL master. A prospective study. Bull Soc Belge Ophtalmol. 2001;281:61–65. French. [PubMed] [Google Scholar]
- 3.Rajan MS, Keilhorn I, Bell JA. Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye. 2002;16:552–556. doi: 10.1038/sj.eye.6700157. [DOI] [PubMed] [Google Scholar]
- 4.Applegate RA, Hilmantel G, Howland HC, Tu EY, Starck T, Zayac EJ. Corneal first surface optical aberrations and visual performance. J Refract Surg. 2000;16:507–514. doi: 10.3928/1081-597X-20000901-04. [DOI] [PubMed] [Google Scholar]
- 5.Padmanabhan P, Mrochen M, Basuthkar S, Viswanathan D, Joseph R. Wavefront-guided versus wavefront-optimized laser in situ keratomileusis: contralateral comparative study. J Cataract Refract Surg. 2008;34:389–397. doi: 10.1016/j.jcrs.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Oshika T, Tokunaga T, Samejima T, Miyata K, Kawana K, Kaji Y. Influence of pupil diameter on the relation between ocular higher-order aberration and contrast sensitivity after laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2006;47:1334–1338. doi: 10.1167/iovs.05-1154. [DOI] [PubMed] [Google Scholar]
- 7.Marcos S. Aberrations and visual performance following standard laser vision correction. J Refract Surg. 2001;17:S596–S601. doi: 10.3928/1081-597X-20010901-19. [DOI] [PubMed] [Google Scholar]
- 8.Oshika T, Okamoto C, Samejima T, Tokunaga T, Miyata K. Contrast sensitivity function and ocular higher-order wavefront aberrations in normal human eyes. Ophthalmology. 2006;113:1807–1812. doi: 10.1016/j.ophtha.2006.03.061. [DOI] [PubMed] [Google Scholar]
- 9.Packer M, Fine IH, Hoffman RS. Wavefront technology in cataract surgery. Curr Opin Ophthalmol. 2004;15:56–60. doi: 10.1097/00055735-200402000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Montes-Mico R, Alio JL, Charman WN. Dynamic changes in the tear film in dry eyes. Invest Ophthalmol Vis Sci. 2005;46:1615–1619. doi: 10.1167/iovs.05-0017. [DOI] [PubMed] [Google Scholar]
- 11.Koh S, Maeda N, Hirohara Y, et al. Serial measurements of higher-order aberrations after blinking in patients with dry eye. Invest Ophthalmol Vis Sci. 2008;49:133–138. doi: 10.1167/iovs.07-0762. [DOI] [PubMed] [Google Scholar]
- 12.Beiko GH. Personalized correction of spherical aberration in cataract surgery. J Cataract Refract Surg. 2007;33:1455–1460. doi: 10.1016/j.jcrs.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 13.Altmann GE. Wavefront-customized intraocular lenses. Curr Opin Ophthalmol. 2004;15:358–364. doi: 10.1097/00055735-200408000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Von Mohrenfels CW, Salgado J, Khoramnia R, Maier M, Lohmann CP. Clinical results with the light adjustable intraocular lens after cataract surgery. J Refract Surg. 2010;26:314–320. doi: 10.3928/1081597X-20090617-12. [DOI] [PubMed] [Google Scholar]
- 15.Chayet A, Sandstedt CA, Chang SH, Rhee P, Tsuchiyama B, Schwartz D. Correction of residual hyperopia after cataract surgery using the light adjustable intraocular lens technology. Am J Ophthalmol. 2009;147:392–397. e1. doi: 10.1016/j.ajo.2008.08.039. [DOI] [PubMed] [Google Scholar]
- 16.Chayet A, Sandstedt C, Chang S, et al. Correction of myopia after cataract surgery with a light-adjustable lens. Ophthalmology. 2009;116:1432–1435. doi: 10.1016/j.ophtha.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 17.Werner L, Mamalis N. Wavefront corrections of intraocular lenses. Ophthalmol Clin North Am. 2004;17:233–245. doi: 10.1016/j.ohc.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Kasper T, Buhren J, Kohnen T. Intraindividual comparison of higher-order aberrations after implantation of aspherical and spherical intraocular lenses as a function of pupil diameter. J Cataract Refract Surg. 2006;32:78–84. doi: 10.1016/j.jcrs.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Kohnen T, Klaproth OK, Buhren J. Effect of intraocular lens asphericity on quality of vision after cataract removal: an intraindividual comparison. Ophthalmology. 2009;116:1697–1706. doi: 10.1016/j.ophtha.2009.03.052. [DOI] [PubMed] [Google Scholar]
- 20.Yamaguchi T, Dogru M, Yamaguchi K, et al. Effect of spherical aberration on visual function under photopic and mesopic conditions after cataract surgery. J Cataract Refract Surg. 2009;35:57–63. doi: 10.1016/j.jcrs.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 21.Beiko GH, Haigis W, Steinmueller A. Distribution of corneal spherical aberration in a comprehensive ophthalmology practice and whether keratometry can predict aberration values. J Cataract Refract Surg. 2007;33:848–858. doi: 10.1016/j.jcrs.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 22.Buscemi P. Clinical applications of the OPD-scan wavefront aberrometer/ corneal topographer. J Refract Surg. 2002;18:S385–S388. doi: 10.3928/1081-597X-20020502-23. [DOI] [PubMed] [Google Scholar]
- 23.MacRae S, Fujieda M. Slit skiascopic-guided ablation using the Nidek laser. J Refract Surg. 2000;16:S576–S580. doi: 10.3928/1081-597X-20000901-18. [DOI] [PubMed] [Google Scholar]
- 24.Applegate RA, Howland HC, Sharp RP, Cottingham AJ, Yee RW. Corneal aberrations and visual performance after radial keratotomy. J Refract Surg. 1998;14:397–407. doi: 10.3928/1081-597X-19980701-05. [DOI] [PubMed] [Google Scholar]
- 25.Bellucci R, Scialdone A, Buratto L, et al. Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60 AT intraocular lenses: a multicenter randomized study. J Cataract Refract Surg. 2005;31:712–717. doi: 10.1016/j.jcrs.2004.08.049. [DOI] [PubMed] [Google Scholar]
- 26.Mester U, Dillinger P, Anterist N. Impact of a modified optic design on visual function: clinical comparative study. J Cataract Refract Surg. 2003;29:652–660. doi: 10.1016/s0886-3350(02)01983-1. [DOI] [PubMed] [Google Scholar]
- 27.Rocha KM, Soriano ES, Chalita MR, et al. Wavefront analysis and contrast sensitivity of aspheric and spherical intraocular lenses: a randomized prospective study. Am J Ophthalmol. 2006;142:750–756. doi: 10.1016/j.ajo.2006.06.031. [DOI] [PubMed] [Google Scholar]
- 28.Sandoval HP, Fernandez de Castro LE, Vroman DT, Solomon KD. Comparison of visual outcomes, photopic contrast sensitivity, wavefront analysis, and patient satisfaction following cataract extraction and IOL implantation: aspheric vs spherical acrylic lenses. Eye (Lond) 2008;22:1469–1475. doi: 10.1038/sj.eye.6702925. [DOI] [PubMed] [Google Scholar]
- 29.Cuthbertson FM, Dhingra S, Benjamin L. Objective and subjective outcomes in comparing three different aspheric intraocular lens implants with their spherical counterparts. Eye (Lond) 2009;23:877–883. doi: 10.1038/eye.2008.122. [DOI] [PubMed] [Google Scholar]
- 30.Pandita D, Raj SM, Vasavada VA, Vasavada VA, Kazi NS, Vasavada AR. Contrast sensitivity and glare disability after implantation of AcrySof IQ Natural aspherical intraocular lens: Prospective randomized masked clinical trial. J Cataract Refract Surg. 2007;33:603–610. doi: 10.1016/j.jcrs.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 31.Denoyer A, Le Lez ML, Majzoub S, Pisella PJ. Quality of vision after cataract surgery after Tecnis Z9000 intraocular lens implantation: effect of contrast sensitivity and wavefront aberration improvements on the quality of daily vision. J Cataract Refract Surg. 2007;33:210–216. doi: 10.1016/j.jcrs.2006.10.035. [DOI] [PubMed] [Google Scholar]
- 32.Caporossi A, Martone G, Casprini F, Rapisarda L. Prospective randomized study of clinical performance of 3 aspheric and 2 spherical intraocular lenses in 250 eyes. J Refract Surg. 2007;23:639–648. doi: 10.3928/1081-597X-20070901-02. [DOI] [PubMed] [Google Scholar]
- 33.Tzelikis PF, Akaishi L, Trindade FC, Boteon JE. Spherical aberration and contrast sensitivity in eyes implanted with aspheric and spherical intraocular lenses: a comparative study. Am J Ophthalmol. 2008;145:827–833. doi: 10.1016/j.ajo.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 34.Kurz S, Krummenauer F, Thieme H, Dick HB. Contrast sensitivity after implantation of a spherical versus an aspherical intraocular lens in biaxial microincision cataract surgery. J Cataract Refract Surg. 2007;33:393–400. doi: 10.1016/j.jcrs.2006.10.066. [DOI] [PubMed] [Google Scholar]
- 35.Kasper T, Buhren J, Kohnen T. Visual performance of aspherical and spherical intraocular lenses: Intraindividual comparison of visual acuity, contrast sensitivity, and higher-order aberrations. J Cataract Refract Surg. 2006;32:2022–2029. doi: 10.1016/j.jcrs.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 36.Yamaguchi T, Negishi K, Ono T, et al. Feasibility of spherical aberration correction with aspheric intraocular lenses in cataract surgery based on individual pupil diameter. J Cataract Refract Surg. 2009;35:1725–1733. doi: 10.1016/j.jcrs.2009.05.031. [DOI] [PubMed] [Google Scholar]
- 37.Oshika T, Mimura T, Tanaka S, et al. Apparent accommodation and corneal wavefront aberration in pseudophakic eyes. Invest Ophthalmol Vis Sci. 2002;43:2882–2886. [PubMed] [Google Scholar]
- 38.Tabernero J, Piers P, Benito A, Redondo M, Artal P. Predicting the optical performance of eyes implanted with IOLs to correct spherical aberration. Invest Ophthalmol Vis Sci. 2006;47:4651–4658. doi: 10.1167/iovs.06-0444. [DOI] [PubMed] [Google Scholar]
- 39.Owsley C, Sekuler R, Boldt C. Aging and low-contrast vision: face perception. Invest Ophthalmol Vis Sci. 1981;21:362–365. [PubMed] [Google Scholar]
- 40.Nameda N, Kawara T, Ohzu H. Human visual spatio-temporal frequency performance as a function of age. Optom Vis Sci. 1989;66:760–765. doi: 10.1097/00006324-198911000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Owsley C, Sekuler R, Siemsen D. Contrast sensitivity throughout adulthood. Vision Res. 1983;23:689–699. doi: 10.1016/0042-6989(83)90210-9. [DOI] [PubMed] [Google Scholar]
- 42.Nomura H, Ando F, Niino N, Shimokata H, Miyake Y. Age-related change in contrast sensitivity among Japanese adults. Jpn J Ophthalmol. 2003;47:299–303. doi: 10.1016/s0021-5155(03)00011-x. [DOI] [PubMed] [Google Scholar]
- 43.Applegate RA, Marsack JD, Ramos R, Sarver EJ. Interaction between aberrations to improve or reduce visual performance. J Cataract Refract Surg. 2003;29:1487–1495. doi: 10.1016/s0886-3350(03)00334-1. [DOI] [PubMed] [Google Scholar]
- 44.Yamaguchi T, Negishi K, Kato N, Arai H, Toda I, Tsubota K. Factors affecting contrast sensitivity with the Artisan phakic intraocular lens for high myopia. J Refract Surg. 2009;25:25–32. doi: 10.3928/1081597X-20090101-05. [DOI] [PubMed] [Google Scholar]
- 45.Wang L, Koch DD. Custom optimization of intraocular lens asphericity. J Cataract Refract Surg. 2007;33:1713–1720. doi: 10.1016/j.jcrs.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 46.Koch DD, Wang L. Custom optimization of intraocular lens asphericity. Trans Am Ophthalmol Soc. 2007;105:36–41. [PMC free article] [PubMed] [Google Scholar]