Nonalcoholic fatty liver disease (NAFLD) has emerged as the most common cause of chronic liver disease in western countries (1). NAFLD is frequently associated with obesity, diabetes, metabolic syndrome, and increased cardiovascular risk. Moreover, patients with the aggressive form of NAFLD, nonalcoholic steatohepatitis or NASH, may be at higher risk of atherosclerosis than patients with simple steatosis due to increased oxidative stress and systemic inflammation (2–4). Mean platelet volume (MPV) is a marker of platelet activation and a validated predictor of cardiovascular risk (5). Larger platelets are enzymatically more active than small platelets, produce more thromboxane A2, and have an increased propensity to thrombosis (6).
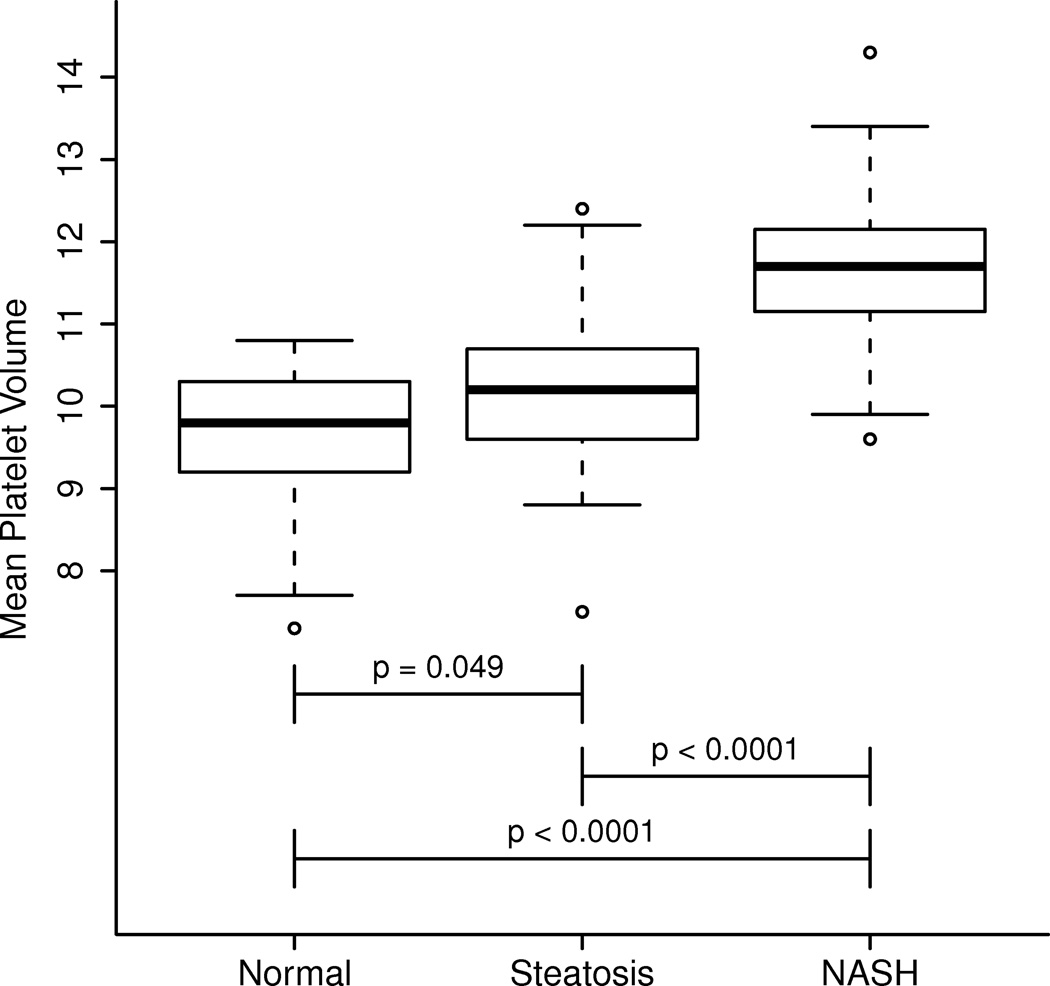
The aim of this study was two-fold: first to assess MPV levels in patients with biopsy proven NAFLD, and second to determine the relation between histological features of NASH and MPV. Our cohort consisted of 100 consecutive patients undergoing liver biopsy for clinical suspicion of NAFLD. Patients were divided into 3 groups: NASH (n=52), simple steatosis (n=25), and normal biopsy (n=21). We measured MPV in blood samples collected at the time of liver biopsy. The mean age was 49.8(± 10.6) years and the mean body mass index was 31.4 (± 4.8) kg/m2. The majority of patients were Caucasians (86%) and 48% were female. There was a stepwise significant increase in MPV levels from patients with normal biopsies to patients with simple steatosis to patients with NASH (9.5 fL, 10.2 fL, and 11.3 fL, respectively. P < 0.005) (figure 1). Moreover, there was a significant correlation between MPV levels and the individual histological features of NASH on liver biopsy including inflammation (rho = 0.64), steatosis (rho = 0.65), ballooning (rho = 0.60) and fibrosis (rho= 0.61), p<0.001 for all.
Figure 1.
We conclude that in adult patients with biopsy proven NAFLD, the histologic severity of liver injury and inflammation is strongly associated with higher MPV levels and therefore potentially increased cardiovascular risk. The study has some limitations including the cross-sectional design, the small sample size, and the relatively young patient population. Thus, a correlation between increasing MPV levels or NAFLD severity and previously documented cardiovascular events was not established. Larger studies are needed to externally validate our findings.
Acknowledgments
This work was supported by NIH DK076852 to AEF
Abbreviations
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- MPV
mean platelet volume
Footnotes
No conflicts of interest exist for any of the authors of this manuscript.
References
- 1.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 2.Alkhouri N, Tamimi TA, Yerian L, Lopez R, Zein NN, Feldstein AE. The Inflamed Liver and Atherosclerosis: A Link Between Histologic Severity of Nonalcoholic Fatty Liver Disease and Increased Cardiovascular Risk. Dig Dis Sci. 2009 doi: 10.1007/s10620-009-1075-y. [DOI] [PubMed] [Google Scholar]
- 3.Sung KC, Ryan MC, Wilson AM. The severity of nonalcoholic fatty liver disease is associated with increased cardiovascular risk in a large cohort of non-obese Asian subjects. Atherosclerosis. 2009;203:581–586. doi: 10.1016/j.atherosclerosis.2008.07.024. [DOI] [PubMed] [Google Scholar]
- 4.Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–1350. doi: 10.1056/NEJMra0912063. [DOI] [PubMed] [Google Scholar]
- 5.Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, Konkle B, Mohler ER, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:148–156. doi: 10.1111/j.1538-7836.2009.03584.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van der Loo B, Martin JF. A role for changes in platelet production in the cause of acute coronary syndromes. Arterioscler Thromb Vasc Biol. 1999;19:672–679. doi: 10.1161/01.atv.19.3.672. [DOI] [PubMed] [Google Scholar]