Abstract
Anaphylaxis is an acute, potentially fatal systemic reaction with varied mechanisms and clinical presentations. Although prompt recognition and treatment of anaphylaxis are imperative, both patients and healthcare professionals often fail to recognize and diagnose early signs and symptoms of the condition. Clinical manifestations vary widely, however, the most common signs are cutaneous symptoms, including angioedema, urticaria, erythema and pruritus. Immediate intramuscular administration of epinephrine into the lateral thigh is first-line therapy, even if the diagnosis is uncertain. The mainstays of long-term management include specialist assessment, avoidance measures, and the provision of an epinephrine auto-injector and an individualized anaphylaxis action plan. This article provides an overview of the causes, clinical features, diagnosis and acute and long-term management of this serious allergic reaction.
Introduction
Anaphylaxis is defined as a serious allergic reaction that is rapid in onset and may cause death [1,2]. The prevalence of anaphylaxis is estimated to be as high as 2%, and appears to be rising, particularly in the younger age group [3-5].
The more rapidly anaphylaxis develops, the more likely the reaction is to be severe and life-threatening [4]. Therefore, prompt recognition and management of the condition are imperative. However, anaphylaxis is often under-recognized and treated inadequately. Diagnosis and management are challenging since reactions are often immediate and unexpected. Furthermore, there is no single test to diagnose anaphylaxis in routine clinical practice [3,6]. This article will provide an overview of the causes and clinical features of anaphylaxis as well as strategies for the accurate diagnosis and management of the condition.
Causes
Most episodes of anaphylaxis are triggered through an immunologic mechanism involving immunoglobulin E (IgE) which leads to mast cell and basophil activation and the subsequent release of inflammatory mediators such as histamine, leukotrienes, tryptase and prostaglandins. Although any substance has the potential to cause anaphylaxis, the most common causes of IgE-mediated anaphylaxis are: foods, particularly, peanuts, tree nuts, shellfish and fish, cow’s milk, eggs and wheat; medications (most commonly penicillin), and natural rubber latex. Exercise, aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), opiates, and radiocontrast agents can also cause anaphylaxis, but anaphylactic reactions to these agents often result from non-IgE-mediated mechanisms. In other cases, the cause of anaphylactic reactions is unknown (idiopathic anaphylaxis). In children, anaphylaxis is most often caused by foods, while venom- and drug-induced anaphylaxis is more common in adults [4,7-9]. Table 1 provides a more comprehensive list of the potential causes of anaphylaxis.
Table 1.
Causes of anaphylaxis.
| Common: • Foods: most commonly peanuts, tree nuts, egg, seafood and fish, cow’s milk, wheat • Medications: most commonly antibiotics • Insect stings (bees and wasps) • Natural rubber latex • Unidentified (no cause found; idiopathic anaphylaxis) |
|---|
|
Less common: • Exercise • Semen • Food additives: monosodium glutamate, metabisulfite • Hormonal changes: menstrual factors • Topical medications • Transfusions |
Co-morbidities and concurrent medications may also affect the severity of anaphylactic reactions and patient response to treatment. For example, patients with asthma and cardiovascular disease are more likely to experience a poor outcome from anaphylaxis. Concurrent administration of beta-blockers can interfere with the patient's ability to respond to epinephrine, the first-line of treatment for anaphylaxis (discussed later). Furthermore, the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) can impact a patient’s compensatory physiologic response to anaphylaxis, leading to more severe reactions [10].
Signs and symptoms
Since anaphylaxis is a generalized reaction, a wide variety of clinical signs and symptoms involving the skin, gastrointestinal and respiratory tracts, and cardiovascular system can be observed (see Table 2). The most common clinical manifestations are cutaneous symptoms, including urticaria and angioedema, erythema (flushing), and pruritus (itching) [11]. Patients also often describe an impending sense of death (angor animi). Death due to anaphylaxis usually occurs as a result of respiratory obstruction or cardiovascular collapse, or both. Evidence suggests that there is a direct correlation between the immediacy of symptom onset and the severity of the episode, with the more rapid the onset, the more severe the event [12]. It is important to note that the signs and symptoms of anaphylaxis are unpredictable and may vary from patient to patient and from one reaction to another. Therefore, the absence of one or more of the common symptoms listed in Table 2 does not rule out anaphylaxis, and should not delay immediate treatment.
Table 2.
|
Skin • Urticaria (hives) • Angioedema (swelling) • Erythema (flushing) • Pruritus (itching) |
Gastrointestinal: • Nausea • Vomiting • Abdominal pain • Diarrhea |
|
Respiratory: • Upper airway: – Nasal congestion – Sneezing – Hoarseness – Cough – Oropharyngeal or laryngeal edema |
Neurologic: • Light-headedness • Dizziness • Confusion |
| • Lower airway: dyspnea – Bronchospasms – Wheezing – Chest tightness |
Oral: • Itching • Tingling or swelling of the lips, tongue or palate |
|
Cardiovascular: • Hypotension • Dizziness • Syncope • Tachycardia |
Other: • Sense of impending doom • Anxiety |
The signs and symptoms of anaphylaxis typically develop within minutes after exposure to the offending antigen, but may occasionally occur as late as 1 hour post exposure. Symptoms usually follow a uniphasic course, with resolution of symptoms within hours of treatment. However, up to 20% of reactions follow a biphasic course characterized by an asymptomatic period of 1-8 hours followed by recurrent symptoms [13].
Diagnosis
The diagnosis of anaphylaxis is based primarily on clinical signs and symptoms, as well as a detailed description of the acute episode, including antecedent activities and events. Diagnostic criteria for anaphylaxis were published by a multidisciplinary group of experts in 2005 and 2006, and are shown in Table 3[1,2]. A diagnosis of anaphylaxis is highly likely when any one of the criteria listed in Table 3 is fulfilled. Since the evaluation and diagnosis of anaphylaxis is often complex, referral to an allergist with training and expertise in the identification and management of anaphylaxis should be considered.
Table 3.
| Anaphylaxis is highly likely when any 1 of the following 3 criteria is fulfilled following exposure to an allergen: | |
|---|---|
| 1 |
Acute onset of an illness (minutes to several hours) with involvement of the skin, mucosal tissue, or both (e.g., generalized hives, pruritus or flushing, swollen lips-tongue-uvula) and at least 1 of the following: a. Respiratory compromise (e.g. dyspnea, wheeze, bronchospasm, stridor, reduced PEF, hypoxemia) b. Reduced BP or associated symptoms of end-organ dysfunction (e.g. hypotonia [collapse], syncope, incontinence) |
| 2 |
2 or more of the following that occur rapidly after exposure to a likely allergen for that patient (minutes to several hours): a. Involvement of the skin-mucosal tissue (e.g., generalized hives, itch-flush, swollen lips-tongue-uvula) b. Respiratory compromise (e.g., dyspnea, wheeze, bronchospasm, stridor, reduced PEF, hypoxemia) c. Reduced BP or associated symptoms (e.g., hypotonia [collapse], syncope, incontinence) d. Persistent GI symptoms (e.g., painful abdominal cramps, vomiting) |
| 3 |
Reduced BP after exposure to a known allergen for that patient (minutes to several hours): a. Infants and children: low systolic BP (age specific) or > 30% decrease in systolic BP* b. Adults: systolic BP < 90 mmHg or > 30% decrease from that person’s baseline |
PEF = Peak expiratory flow; BP: blood pressure; GI: gastrointestinal
* Low systolic blood pressure for children is age specific and defined as: < 70 mmHg for age 1 month to 1 year; < 70mmHg + [2 x age] for age 1 to 10 years; < 90mmHg for age 11 to 17 years.
History
The history is the most important tool to establish the cause of anaphylaxis and should take precedence over diagnostic tests. It should elicit information about clinical manifestations (e.g., urticaria, angioedema, flushing, pruritus, airway obstruction, gastrointestinal symptoms, syncope, and hypotension); agents encountered before the reaction, such as foods, medications or insect bites/stings, as well as the patient’s activities preceding the event (e.g., exercise, sexual activity). The absence of cutaneous symptoms puts the diagnosis in question since the majority of anaphylactic episodes include cutaneous symptoms; however, their absence does not rule out anaphylaxis [4].
Additional diagnostic tests
The diagnosis of a specific cause of anaphylaxis may be supported by the results of skin tests and/or in vitro IgE tests [4]. These tests can determine the presence of specific IgE antibodies to foods, medications (e.g., penicillin), and stinging insects. However, for the majority of medications, standardized skin tests and/or in vitro tests are not available. In general, skin testing is more sensitive than in vitro testing and is the diagnostic procedure of choice for the evaluation of most IgE-mediated causes of anaphylaxis (if available for the relevant trigger or allergen). If skin testing is performed, it should be done under the supervision of a physician who is experienced in the procedure in a setting with appropriate rescue equipment and medication available [4].
The clinical diagnosis of anaphylaxis can sometimes be supported by the documentation of elevated concentrations of mast cell and basophil mediators such as plasma histamine or serum or plasma total tryptase. However, it is critical to obtain blood samples for these measurements as soon as possible after the onset of symptoms since elevations are transient.
Differential diagnosis
Other diagnoses that might present with signs and/or symptoms characteristic of anaphylaxis should be excluded. The most common conditions that mimic anaphylaxis include: vasodepressor (vasovagal/neurocardiogenic) reactions (which are characterized by hypotension, pallor, bradycardia, weakness, nausea and vomiting); acute respiratory decompensation from severe asthma attacks, foreign body aspiration and pulmonary embolism; vocal cord dysfunction; acute anxiety (e.g., panic attack or hyperventilation syndrome); myocardial dysfunction, acute poisoning; hypoglycemia; and seizure disorders [4,14].
Treatment
Acute management
The acute treatment of anaphylaxis begins with rapid assessment of the airway, breathing and circulation. Epinephrine is the drug of choice for anaphylaxis and should be given immediately to any patient with a suspected anaphylactic episode. Treatment should be provided even if the diagnosis is uncertain since there here are no contraindications to the use of epinephrine [6].
The recommended dosing of epinephrine for the acute treatment of anaphylaxis is 0.01 mg/kg up to a maximum of 0.5 mg administered intramuscularly every 5–20 min as necessary [6]. Intramuscular administration into the lateral thigh is recommended as it allows for more rapid absorption and higher plasma epinephrine levels compared to subcutaneous administration [10]. Glucagon should also be considered in patients using beta-blockers.
All patients receiving emergency epinephrine must be transported to hospital immediately (ideally by ambulance) for evaluation and observation. Patients should also be placed in a recumbent (supine) position with the lower extremities elevated, unless this is precluded by shortness of breath or vomiting [6,15,16].
As mentioned earlier, patients with asthma, particularly those with poorly controlled asthma, are at increased risk of a fatal reaction. In these patients, anaphylaxis may be mistaken for an asthma exacerbation and inappropriately treated solely with asthma inhalers. Therefore, if there are ongoing asthma symptoms in an individual with known anaphylaxis, epinephrine should be given [6].
Oxygen therapy should also be considered in any patient with symptoms of anaphylaxis, particularly for those with prolonged reactions. Intravenous fluids (crystalloid solutions or colloid volume expanders) should also be provided since massive fluid shifts can occur rapidly in anaphylaxis due to increased vascular permeability. Volume replacement is particularly important for patients whose hypotension persists despite epinephrine injections. Supportive therapy such as inhaled beta2-agonists (for patients experiencing bronchospasm) and antihistamines (for control of cutaneous symptoms) can also be helpful, but should never replace epinephrine as first-line therapy. Vasopressors, such as dopamine, can also be considered if epinephrine injections and volume expansion with intravenous fluids fail to alleviate hypotension. Glucocorticosteroids have a slow onset of action and, therefore, these agents have not been shown to be effective for the acute treatment of anaphylaxis. Theoretically, however, they may prevent biphasic or protracted reactions and, hence, are often given on an empirical basis. To date, there is no conclusive evidence that the administration of glucocorticosteroids prevents a biphasic response [4].
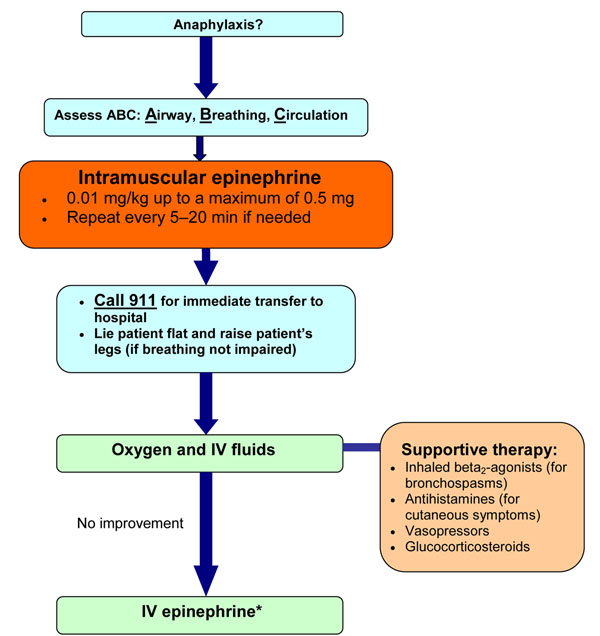
If intramuscular epinephrine and intravenous fluids fail to improve anaphylactic symptoms, intravenous infusions of epinephrine may be required; however, these infusions should be given by a physician who is trained and experienced in its use and has the capacity for continuous blood pressure and cardiac monitoring. Figure 1 provides a simplified algorithm for the acute management of anaphylaxis.
Figure 1.
Simplified algorithm for the acute management of anaphylaxis. IV: intravenous *Should be given by a physician trained in the use of IV epinephrine with capacity for continuous blood pressure and cardiac monitoring
Following acute treatment, patients should be observed for a period of time due to the risk of a biphasic response or possible recurrence of the reaction as epinephrine wears off. The observation period should be individualized based on the severity of the initial reaction and access to care. Experts have recommended observing patients for 4 to 6 hours following an anaphylactic reaction, with prolonged observation times for patients with severe or refractory symptoms [6].
Long-term management
The mainstays of long-term management for patients who have experienced an anaphylactic episode include: specialist assessment, a prescription for an epinephrine auto-injector, patient and caregiver education on avoidance measures, and the provision of an individualized anaphylaxis action plan.
Specialist assessment
After acute anaphylaxis, patients should be assessed for their future risk of anaphylaxis, ideally by an allergist. These specialists are experienced in identifying and confirming the cause of anaphylaxis, educating patients on appropriate avoidance strategies, drafting an anaphylaxis action plan, and advising whether immunotherapy is appropriate [4,6].
Prescription for an epinephrine auto-injector
A prescription for an epinephrine auto-injector should be provided to all patients who have experienced anaphylaxis previously, including those who have had any rapid-onset systemic allergic reaction (gastrointestinal, respiratory, cardiac); diffuse hives to any food or insect stings; or any rapid-onset (i.e., minutes to hours) reaction of any severity to the highest risk foods such as peanut, tree nuts, fish, and shellfish [6].
There are currently two epinephrine auto-injectors available in North America: EpiPen® and Twinject®. Both products come in two dosages (0.15 mg and 0.30 mg), which are prescribed according to weight. The 0.30 mg dosage should be used for those weighing 30 kg or more, and the 0.15 mg dosage for children weighing between 15–30 kg. Certain sources recommend switching to the 0.30 mg dose at 25 kg rather than 30 kg [16]. These devices should be stored properly (avoiding temperature extremes) and replaced before the expiration date. More information on these auto-injectors is available at http://www.epipen.ca and http://www.twinject.ca.
Upon prescription of an epinephrine auto-injector, healthcare providers must instruct the patient on how and when to use the device. Instructions on proper use should be reviewed verbally and accompanied by a DVD and/or written material, and should be reinforced annually.
Education on avoidance measures
Patients and their caregivers should be educated about agents or exposures that may place them at risk for future reactions, and should be counselled on avoidance measures that may be used to reduce the risk for such exposures. Avoidance strategies should be individualized, taking into consideration factors such as relevant triggers, age, activity, occupation, hobbies, residential conditions, access to medical care, and the patient’s level of personal anxiety. Individuals who have had anaphylactic reactions to foods should be instructed to read food labels carefully, watching for hidden ingredients such as “natural flavour” or “spices” that may indicate the presence of allergens (e.g., peanut, tree nuts, milk, egg, shellfish, fish, sesame, soy and wheat), as well as “may contain” warnings [4]. Recent evidence suggests that peanut allergic children can be desensitized to peanut by feeding them increasing amounts of peanut under close supervision [17]. Similar results have been noted for egg and milk allergy. Although these results are promising, further confirmatory studies in this area are needed before routinely recommending desensitization procedures to patients with these food allergies (for more information, see article on Food Allergy in this supplement).
Patients with anaphylaxis to medications should be informed about all cross-reacting medications that should be avoided. Should there be a future essential indication for use of the medication causing anaphylactic reactions, it may be helpful to educate patients about possible management options, such as medication pretreatment and use of low osmolarity agents in patients with a history of reactions to radiographic contrast media, or induction of drug tolerance procedures (also known as drug desensitization) [4]. Induction of drug tolerance procedures temporarily modify a patient’s immunologic or non-immunologic response to a drug through the administration of incremental doses of the drug. However, drug tolerance is usually maintained only as long as the drug is administered; therefore, the procedure needs to be repeated in the future if the patient requires the drug again after finishing a prior therapeutic course (for more information, see article on Drug Allergy in this supplement).
Patients who have had an anaphylactic reaction to an insect sting should be advised about avoidance measures to reduce the risk of future stings. Such measures include: being alert when eating outdoors (as wasps are attracted to food), wearing shoes and long pants when in fields, and having nests or hives near the patient’s home removed [14]. Patients who have previously experienced venom-induced anaphylaxis are often candidates for venom immunotherapy, which is successful in preventing anaphylaxis in up to 98% of patients (see article on Allergen Immunotherapy in this supplement).
Subjects at high risk of a reaction to latex include: healthcare workers, children with spina bifida and genitourinary abnormalities; and workers with occupational exposure to latex. Patients with spina bifida (regardless of a history of latex allergy) and patients with a positive history of latex allergy should have all medical-surgical-dental procedures performed in a latex-safe environment. This is an environment in which no natural rubber latex gloves are used in the room or surgical suite and in which there are limited latex-based accessories (catheters, adhesives, tourniquets, anesthesia equipment or devices) which come in contact with the patient [4].
Patients should also obtain and wear medical identification (such as a MedicAlert bracelet/necklace) that indicates that they have experienced anaphylaxis as well as the responsible agent. Patients should also be instructed to avoid drugs that might increase their susceptibility and/or complicate the management of an anaphylactic event, such as beta-blockers, ACE inhibitors, or ARBs [4].
Anaphylaxis action plan
A comprehensive, individualized anaphylaxis action plan should be prepared which defines roles and responsibilities and emergency protocols [6]. Important information that should be included in this plan is shown in Table 4[6,18]. Examples of such a plan, along with other relevant information and materials, can be downloaded at Anaphylaxis Canada (http://www.anaphylaxis.ca) or the Food Allergy and Anaphylaxis Network (http://www.foodallergy.org; a US-based association). Action plans should be reviewed annually and updated if necessary. A copy of the plan should be made available to all relevant persons, such as day-care providers, teachers, and employers. Recommendations for the management of anaphylaxis in schools and other community settings [15] are available through the Allergy Safe Communities website at http://www.allergysafecommunities.ca.
Table 4.
| Contact details • Names and contact details for emergencies, including family members, allergist/immunologist and family doctor • Contact details for local emergency or ambulance services |
|---|
|
Allergens/Triggers • Clear identification of allergens/triggers to be avoided – Include generic and proprietary names of drugs and possible cross-sensitivities, if relevant |
|
How to recognize the signs and symptoms of anaphylaxis • Mouth: itching, swelling of lips/tongue • Throat: itching, tightness, closure, hoarseness • Skin: itching, hives, eczema, swelling, flushing • Gut: vomiting, diarrhea, abdominal pain • Lung: shortness of breath, cough, wheeze • Heart: hypotension, dizziness, syncope, tachycardia • Neuro (or head): light-headedness • Other: feeling of impending doom, anxiety |
|
Medications prescribed and when they should be used • Epinephrine auto-injectors (first-line); should include detailed instructions (with photographs, if possible) on how to correctly administer the auto-injector device (for daycare, school and/or office staff) • Antihistamines (for cutaneous symptoms) • Inhaled beta2-agonists (for bronchospasm) |
| Where medication is stored at home, work or school |
Conclusions
Anaphylaxis is an acute, potentially fatal systemic reaction with varied mechanisms and clinical presentations. Prompt recognition and treatment of anaphylaxis are imperative; however, both patients and healthcare professionals often fail to recognize and diagnose anaphylaxis in its early stages. Diagnostic criteria which take into account the variable clinical manifestations of anaphylaxis are now available and can assist healthcare providers in the early recognition of the condition. Immediate intramuscular administration of epinephrine into the lateral thigh is first-line therapy for anaphylaxis. Acute management may also involve oxygen therapy, intravenous fluids, and adjunctive therapies such as antihistamines or inhaled beta2-agonists. The mainstays of long-term management include specialist assessment, a prescription for an epinephrine auto-injector, patient and caregiver education on avoidance measures, and the provision of an individualized anaphylaxis action plan.
Key take-home messages
• Anaphylaxis is defined as a serious allergic reaction that is rapid in onset and may cause death.
• Prompt recognition and treatment are critical in anaphylaxis.
• The diagnosis is based primarily on clinical signs and symptoms.
• The most common clinical manifestations are cutaneous symptoms, including urticaria and angioedema, erythema, and pruritus.
• Referral to an allergist or immunologist should be considered for all persons who have experienced a previous anaphylactic episode.
• Epinephrine is the drug of choice for anaphylaxis and should be given immediately, even if the diagnosis is uncertain; intramuscular administration into the lateral thigh is recommended.
• There are no contraindications to the use of epinephrine.
• The mainstays of long-term treatment include: specialist assessment, avoidance measures, and the provision of an epinephrine auto-injector and an individualized anaphylaxis action plan.
Competing interests
Dr. Harold Kim is the past president of the Canadian Network for Respiratory Care and co-chief editor of Allergy, Asthma &Clinical Immunology. He has received consulting fees and honoraria for continuing education from AstraZeneca, GlaxoSmithKline, Graceway Pharmaceuticals, King Pharma, Merck Frosst, Novartis, and Nycomed.
Dr. David Fischer is a member of the Board of Directors of the Canadian Society of Allergy & Clinical Immunology. He has received consulting fees and honoraria for continuing education from AstraZeneca, GlaxoSmithKline, Graceway Pharmaceuticals, King Pharma, Merck Frosst, Novartis, Paladin Labs and Nycomed.
Contributor Information
Harold Kim, Email: hlkimkw@gmail.com.
David Fischer, Email: dkfischer@rogers.com.
Acknowledgements
This article has been published as part of Allergy, Asthma & Clinical Immunology Volume 7 Supplement 1, 2011: Practical guide for allergy and immunology in Canada. The full contents of the supplement are available online at http://www.aacijournal.com/supplements/7/S1
References
- Sampson HA, Munoz-Furlong A, Bock SA, Schmitt C, Bass R, Chowdhury BA, Decker WW, Furlong TJ, Galli SJ, Golden DB, Gruchalla RS, Harlor AD Jr, Hepner DL, Howarth M, Kaplan AP, Levy JH, Lewis LM, Lieberman PL, Metcalfe DD, Murphy R, Pollart SM, Pumphrey RS, Rosenwasser LJ, Simons FE, Wood JP, Camargo CA Jr. Symposium on the definition and management of anaphylaxis: summary report. J Allergy Clin Immunol. 2005;115:584–91. doi: 10.1016/j.jaci.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, Brown SG, Camargo CA Jr, Cydulka R, Galli SJ, Gidudu J, Gruchalla RS, Harlor AD Jr, Hepner DL, Lewis LM, Lieberman PL, Metcalfe DD, O'Connor R, Muraro A, Rudman A, Schmitt C, Scherrer D, Simons FE, Thomas S, Wood JP, Decker WW. Second symposium on the definition and management of anaphylaxis: summary report – Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117:391–7. doi: 10.1016/j.jaci.2005.12.1303. [DOI] [PubMed] [Google Scholar]
- Lieberman PL, Camargo CA, Bohlke K, Jick H, Miller RL, Sheikh A, Simons FE. Epidemiology of anaphylaxis: findings of the ACAAI Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006;97:596–602. doi: 10.1016/S1081-1206(10)61086-1. [DOI] [PubMed] [Google Scholar]
- Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, Bernstein JA, Burks AW, Feldweg AM, Fink JN, Greenberger PA, Golden DB, James JM, Kemp SF, Ledford DK, Lieberman P, Sheffer AL, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, Lang D, Nicklas RA, Oppenheimer J, Portnoy JM, Randolph C, Schuller DE, Spector SL, Tilles S, Wallace D. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol. 2010;126:477–80. doi: 10.1016/j.jaci.2010.06.022. [DOI] [PubMed] [Google Scholar]
- Shen Y, Li L, Grant J, Zhao Z, Zhang X, Zhou L, Fowler D. Anaphylactic deaths in Maryland (US) and Shanghai: a review of forensic autopsy cases from 2004 to 2006. Forensic Sci Int. 2009;186:1–5. doi: 10.1016/j.forsciint.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Waserman S, Chad Z, Francoeur MJ, Small P, Stark D, Vander Leek TK, Kaplan A, Kastner M. Management of anaphylaxis in primary care: Canadian expert consensus recommendations. Allergy. 2010;65:1082–92. doi: 10.1111/j.1398-9995.2010.02418.x. [DOI] [PubMed] [Google Scholar]
- Braganza SC, Acworth JP, McKinnon DR, Peake JE, Brown AF. Paediatric emergency department anaphylaxis: different patterns from adults. Arch Dis Child. 2006;91:159–63. doi: 10.1136/adc.2004.069914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SGA. Clinical features and severity grading of anaphylaxis. J Allergy Clin Immunol. 2004;114:371–76. doi: 10.1016/j.jaci.2004.04.029. [DOI] [PubMed] [Google Scholar]
- Brown AF, McKinnon D, Chu K. Emergency department anaphylaxis: a review of 142 patients in a single year. J Allergy Clin Immunol. 2001;108:861–66. doi: 10.1067/mai.2001.119028. [DOI] [PubMed] [Google Scholar]
- Simon FE. Anaphylaxis, killer allergy: long-term management in the community. J Allergy Clin Immunol. 2006;117:367–77. doi: 10.1016/j.jaci.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Webb LM, Lieberman P. Anaphylaxis: a review of 601 cases. Ann Allergy Asthma Immunol. 2006;97:39–43. doi: 10.1016/S1081-1206(10)61367-1. [DOI] [PubMed] [Google Scholar]
- Terr AI. Anaphylaxis. Clin Rev Allergy. 1985;3:3–23. doi: 10.1007/BF02993040. [DOI] [PubMed] [Google Scholar]
- Stark BJ, Sullivan TJ. Biphasic and protracted anaphylaxis. J Allergy Clin Immunol. 1986;78:76–83. doi: 10.1016/0091-6749(86)90117-X. [DOI] [PubMed] [Google Scholar]
- Ellis AK, Day JH. Diagnosis and management of anaphylaxis. CMAJ. 2003;169:307–11. [PMC free article] [PubMed] [Google Scholar]
- Canadian Society of Allergy and Clinical Immunology. Anaphylaxis in schools & other settings. 2. CSACI; 2009. [Google Scholar]
- Sicherer SH, Simons FE. Section on Allergy and Immunology American Academy of Pediatrics. Self-injectable epinephrine for first-aid management of anaphylaxis. Pediatrics. 2007;119:638–46. doi: 10.1542/peds.2006-3689. [DOI] [PubMed] [Google Scholar]
- Burks A. Peanut allergy. Lancet. 2008;371:1538–46. doi: 10.1016/S0140-6736(08)60659-5. [DOI] [PubMed] [Google Scholar]
- Muraro A, Roberts G, Clark A, Eigenmann PA, Halken S, Lack G, Moneret-Vautrin A, Niggemann B, Rancé F. EAACI Task Force on Anaphylaxis in Children. The management of anaphylaxis in childhood: position paper of the European academy of allergology and clinical immunology. Allergy. 2007;62:857–71. doi: 10.1111/j.1398-9995.2007.01421.x. [DOI] [PubMed] [Google Scholar]