To the Editor
The optimal strategy for glycemic control in elderly adults with diabetes is uncertain because of competing risks from non-diabetic conditions and higher risk of adverse drug effects. The lack of specificity in current treatment guidelines for elderly patients reflects the weak evidence base for decision-making. To quantify the implications of potential changes in treatment guidelines, we characterize current drug usage by diabetic elders in the US and quantify the number who might benefit from reduced anti-diabetic drug exposure if the target HbA1c were increased in the elderly.
METHODS
We analyzed data from the National Health and Nutrition Examination Survey (NHANES) 2003-2008, a series of cross-sectional surveys of the civilian, non-institutionalized population of the US. We identified 876 adults 65 years and older with diagnosed diabetes. After excluding individuals with missing HbA1c or serum creatinine, 756 diabetic elders were included in the analysis, representing 6.4 million individuals when applied to the 2000 US Census population. Medication use by HbA1C level was described. Analyses were performed using Stata Version 11 (StataCorp, College Station, TX) survey modules to obtain unbiased estimates from the complex NHANES sampling design.
RESULTS
Mean (±SE) age was 73.1 (±0.3) and mean(±SE) body mass index was 30.6 (±0.32) kg/m2; 45.8% were men; 12.3% were non-Hispanic black, 4.9% were Mexican American, and 14.4% were current smokers. More than half (66.4%) had diabetes for 10 years or more; 75.0% had diagnosed hypertension, 62.4% had diagnosed high cholesterol; 46.7% had cardiovascular disease; 25.3% had a history of cancer; and 22.0% had retinopathy. Mean (±SE) HbA1c was 6.8% (±0.06): 63.4%, 23.9%, and 12.8% of diabetic elders had HbA1c under 7%, 7 –7.9%, and 8% or higher, respectively (see Figure). More than 80% of elders were treated with anti-diabetic medications: 39.4% with sulfonylureas, 36.8% with metformin, 18.7% with thiazolidinediones (TZDs), and 17.3% with insulin. Most elders also used multiple non-diabetes prescription medications (52.3% used 4 or more; 31.0% used six or more) for a mean (±SE) of 5.4 (±0.2) for total number of prescription medications. Two percent of diabetic elders used metformin despite contraindications (renal dysfunction or age ≥ 80) (corresponding to 168,000 individuals) and 3.4% used a TZD despite a history of heart failure (corresponding to 286,000 individuals).
Figure.
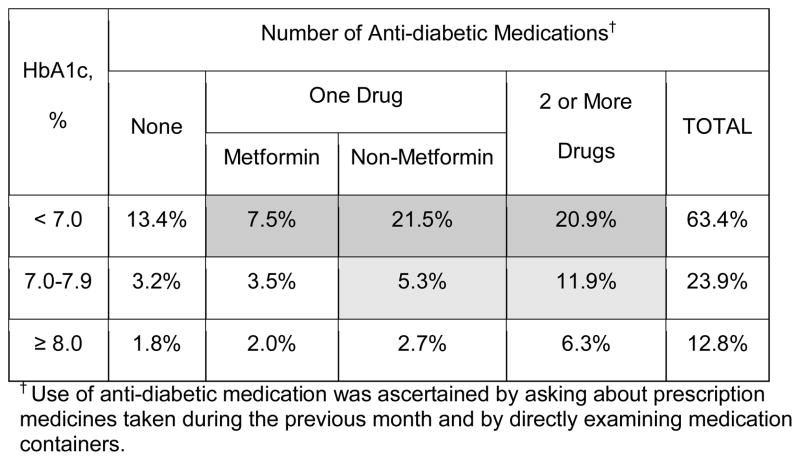
The distribution of elderly adults with diagnosed diabetes in the US, by number and type of anti-diabetic medication and by HbA1c level. The percentages add to 100% in HbA1c column, corresponding to a total of 6.4 million diabetic elders. These percentages are broken down further across the rows of the table. All data are from NHANES 2003–2008 and are weighted to the US population according to the 2000 Census.
The Figure displays medication use by HbA1c level. 49.9% all elders (corresponding to the darker gray area) were on medications with an HbA1c less than 7%; in fact, 20.9% of all elders were on multiple medications in order to achieve this HbA1c level. If the glycemic target for diabetic elders were raised from 7% to 8%, then 49.9% (dark gray area in the Figure) of diabetic elders (3.2 million adults) might be able to discontinue or reduce their anti-diabetic medication regimen.
In addition to this group, 17.2% of diabetic elders (corresponding to the light gray area) who had HbA1c between 7 and 7.9% were taking medications other than metformin or taking more than one drug. These patients may also modify their anti-diabetic medications regimen. These patients would correspond to an additional 1.1 million elders.
DISCUSSION
About 81% of diabetic elders in the US use one or more anti-diabetic medication; about 60% of diabetic elders are taking anti-diabetic medications besides metformin; and about 5% are using an anti-diabetic drug despite an apparent contraindication to its use. In addition, most diabetic elders are taking 5 or more prescription medications in total.
The present level of prescribing for elderly diabetics is very likely a reflection of physicians pursuing the standard glycemic control HbA1c target of <7.0%. Although tighter glycemic control reduces microvascular risk1, hypoglycemia, polypharmacy, and other adverse drug effects pose special concerns for diabetic elders. Severe hypoglycemic episodes may contribute to dementia2; polypharmacy may increase the risk of injurious falls3,4. Moreover, In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, the all-cause mortality in intensive versus standard glycemia group was not different among those participants age 65 or older5. A higher glycemic goal may be appropriate for elderly individuals, particularly those with severe or frequent hypoglycemia.
The 2011 American Diabetes Association Standards of Medical Care for Diabetes6 recommends HbA1c < 7% for most individuals with diabetes, but qualifies the recommendation for older adults: “For patients with advanced diabetes complications, life-limiting comorbid illness, or substantial cognitive or functional impairment, it is reasonable to set less-intensive glycemic target goals.” Similarly, the 2003 American Geriatrics Society’s Guidelines for Improving the Care of the Older Person with Diabetes Mellitus7 recommends “For frail older adults, persons with life expectancy of less than 5 years, and others in whom the risks of intensive glycemic control appear to outweigh the benefits, a less stringent target such as 8% is appropriate.”
The 2011 VA-DoD Diabetes Guidelines Working Group8 recommends HbA1c targets based on shared decision making between clinicians and patients that focuses on life expectancy. Specific recommendations for HbA1c target ranges from < 7% to < 9% are offered based on age or the presence/severity of major comorbidities and microvascular complications. Although this individualized approach to diabetes care is clinically reasonable, there is no direct trial in an elderly population to support a target of 7% as opposed to 8% and no direct trial evidence supporting an individualized approach.
If the general HbA1c goal in diabetic elders were raised from 7% to 8%, more than 3 million diabetic adults in the US, might be able to simplify their diabetes care. Whether a higher HbA1c target is indeed appropriate will require a randomized controlled trial focused on diabetic elders.
Acknowledgments
P.L. received research grant support from Sanofi-Aventis and Novartis, is a consultant for Sanofi-Aventis and Eli Lilly, a member of scientific advisory boards for Sanofi-Aventis and Novo Nordisk, and on the speaker’s bureau of Amylin Pharmaceuticals and Novo Nordisk.
SPONSOR’S ROLE: None.
Footnotes
AUTHOR CONTRIBUTIONS
H-C Yeh researched the data, contributed to discussion and wrote the manuscript. E.S. Huang, P Levin, and F.L. Brancati contributed to discussion and reviewed/edited manuscript. S-H Liu researched the data and reviewed/edited manuscript.
Conflict of Interest
Drs. Yeh and Brancati are supported by NIDDK Diabetes Research and Training Center (P60 DK079637). Dr. Brancati is supported by a grant from the National Institutes of Health, NIDDK, Bethesda, MD (K24 DK62222). Dr. Huang is supported by the NIDDK Diabetes Research and Training Center at the University of Chicago (P60DK020595).
References
- 1.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes (UKPDS 38) BMJ. 1998;317:703–713. [PMC free article] [PubMed] [Google Scholar]
- 2.Whitmer RA, Karter AJ, Yaffe K, et al. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA. 2009 Apr 15;301:1565–72. doi: 10.1001/jama.2009.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 4.Huang ES, Karter AJ, Danielson KK, et al. The association between the number of prescription medications and incident falls in a multi-ethnic population of adult type-2 diabetes patients: the diabetes and aging study. J Gen Intern Med. 2010;25:141–146. doi: 10.1007/s11606-009-1179-2. Epub 2009 Dec 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calles-Escandón J, Lovato LC, Simons-Morton DG, et al. Effect of intensive compared with standard glycemia treatment strategies on mortality by baseline subgroup characteristics: The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care. 2010;33:721–727. doi: 10.2337/dc09-1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Standards of medical care in diabetes–2011. Diabetes Care. 2011;34 (Suppl 1):S42. doi: 10.2337/dc11-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown AF, Mangione CM, Saliba D, et al. Guidelines for improving the care of the older individual with diabetes mellitus. J Am Geriatr Soc. 2003;51 (Suppl):S265–S280. doi: 10.1046/j.1532-5415.51.5s.1.x. [DOI] [PubMed] [Google Scholar]
- 8.Pogach L, Conlin PR, Hobbs C, et al. for the VA-DoD Diabetes Guideline Working Group. What clinicians need to know about absolute risk of benefits and harms of A1c laboratory accuracy. Federal Practitioner. 2011;39:39–44. [Google Scholar]