Abstract
Chlorthalidone (CTD) reduces 24-hour blood pressure more effectively than hydrochlorothiazide (HCTZ), but whether this influences electrocardiographic left ventricular hypertrophy (LVH) is uncertain. One source of comparative data is the Multiple Risk Factor Intervention Trial (MRFIT), which randomly assigned 8,012 hypertensive men to special intervention (SI) or usual care (UC). SI participants could use CTD or HCTZ initially; previous analyses have grouped clinics by their main diuretic used (C-clinics: CTD; H-clinics: HCTZ). After 48 months, SI participants receiving HCTZ were recommended to switch to CTD, in part, because higher mortality was observed for SI compared to UC participants in H-clinics, while the opposite was found in C-clinics. In this analysis, we examined change in continuous measures of electrocardiographic LVH using both an ecologic analysis by previously-reported C- or H-clinic groupings, and an individual participant analysis where use of CTD or HCTZ by SI participants was considered and updated annually. Through 48 months, differences between SI and UC in LVH were larger for C-clinics compared to H-clinics (Sokolow-Lyon: −93.9 vs −54.9 μV, P=0.049; Cornell voltage: −68.1 vs −35.9 μV, P=0.019; Cornell voltage product: −4.6 vs −2.2 μV/ms, P=0.071; left ventricular mass: −4.4 vs −2.8 gm, P=0.002). At the individual participant level, Sokolow-Lyon and left ventricular mass were significantly lower for SI men receiving CTD compared to HCTZ through 48 months and 84 months of follow-up. Our findings on LVH support the idea that greater blood pressure reduction with CTD than HCTZ may have led to differences in mortality observed in MRFIT.
Keywords: hydrochlorothiazide, chlorthalidone, left ventricular hypertrophy, hypertension, blood pressure, electrocardiography
Lowering of blood pressure with a diuretic-based regimen has decreased stroke, heart failure, and cardiovascular disease events in several outcome-based clinical trials.1 Most of these studies used the thiazide-like diuretic, chlorthalidone (CTD), yet 95% of thiazide prescriptions are for hydrochlorothiazide (HCTZ).2 There has been little direct comparison of the two agents on measures other than blood pressure reduction.1
One source of comparative data comes from the Multiple Risk Factor Intervention Trial (MRFIT), which used both CTD and HCTZ in a nonrandomized manner.3 Almost five years into the trial, a recommendation was made by the external data and safety monitoring committee (i.e., the MRFIT Policy Advisory Board) to switch all hypertensive participants in the special intervention (SI) group who were taking 50 or 100 mg/day of HCTZ, to 50 mg/day of CTD.4 This protocol change was prompted by an ecologic analysis revealing that coronary heart disease mortality rates for the SI group were significantly higher than for usual care (UC) participants in clinics where HCTZ was predominantly used (i.e., ‘H-clinics’).4,5 Conversely, mortality rates were lower for SI compared to UC participants in clinics with high utilization of CTD (i.e., ‘C-clinics’). After the protocol change, this unfavorable mortality pattern for SI compared to UC participants reversed during follow-up, giving relevance of the ecological association identified earlier.4 Although choice of diuretic was believed to have influenced the findings, conclusions about the specific impact of CTD or HCTZ in MRFIT remain speculative.
A small, prospective study suggested that CTD can sustain reductions in blood pressure throughout a 24-hour period more effectively than HCTZ, probably due to its longer half-life.6 These data led us to investigate the effects of CTD and HCTZ on electrocardiographic left ventricular hypertrophy (LVH) in MRFIT. Left ventricular hypertrophy is strongly influenced by blood pressure and is an established risk factor for coronary heart disease.7-9 Differences in LVH may yield further insight into the MRFIT findings.
METHODS
Study Cohort
The design and methods of MRFIT have been extensively reported.3 Briefly, MRFIT was a large randomized primary prevention trial designed to determine effects on coronary heart disease mortality of a multifaceted intervention targeting smoking cessation, reduction in serum cholesterol, and stepped-care treatment of hypertension. Men aged 35 to 57 years were invited to attend 3 screening examinations in 22 clinical centers located in 18 US cities. Participants were selected based on their having an above average risk of developing coronary heart disease, as determined from a risk score calculated as a function of serum cholesterol, diastolic blood pressure, and cigarette smoking. Participants who were free of coronary heart disease by history and examination, including a resting electrocardiogram, were eligible for randomization.
After providing consent, 12,866 men were randomly assigned to two groups, special intervention (SI) or usual care (UC). The SI program included counseling on smoking cessation, advice on dietary modifications to reduce cholesterol levels, and treatment for hypertension, while the UC group received treatment of their risk factors as considered on an individual basis by their usual sources of care within the community. Of those randomized, 8,012 (62%) were classified as hypertensive at baseline, defined as average diastolic blood pressure level of ≥ 90 mmHg or who had been receiving antihypertensive drugs on entry. These 8,012 men, also the focus of earlier reports, are included in this analysis.
Intervention
Hypertension treatment for SI participants used a stepped-care approach which included moderate salt reduction, weight loss, and antihypertensive drugs.10 Initial medication was an oral diuretic, either CTD or HCTZ, at a dose of 50 or 100 mg daily (the standard doses used at the time MRFIT was carried out). This was followed by stepwise addition of an antiadrenergic drug or a beta-blocker (Step 2), an arteriolar vasodilator (Step 3), and guanethidine (Step 4), designed to achieve and maintain a diastolic blood pressure goal of 80-89 mmHg. The choice of which diuretic to initiate in SI participants was left to the discretion of the individual physician. Within many clinics there was a tendency to use predominantly one diuretic or the other, which enabled clinics to be categorized in earlier ecologic analyses according to the diuretic predominantly used in that clinic (C-clinic: chlorthalidone; H-clinic: HCTZ).
Blood Pressure and Electrocardiographic Measurements
A random zero sphygmomanometer was used to measure clinic blood pressure in the seated position after five minutes rest, as detailed elsewhere.10 Two measurements were recorded at each of the second and third screening visits and annually thereafter throughout follow-up.
Procedures have been reported for recording resting electrocardiograms and for computerized measurements, including different measures of LVH.11-15 Briefly, standard 12-lead resting electrocardiograms were recorded at the second and third screening visits, and then annually for the duration of follow-up. Standard limb electrodes were placed on the torso to permit exercise as well as resting electrocardiograms at baseline (at the third of three screening visits before randomization).12 This lead configuration was maintained for recording resting electrocardiograms at annual visits following randomization. The electrocardiograms were recorded on magnetic tape cassettes with standard 3-channel electrocardiogram machines (Marquette series 3500; Marquette Inc, Milwaukee, WI). The analog cassettes were processed by computer algorithm at the Computer Electrocardiogram Center (Dalhousie University, Halifax), and were also visually coded at the Electrocardiogram Coding Center at the University of Minnesota.
The following continuous measurements were used to define LVH: Sokolow-Lyon voltage (μV) = ∣ SV1∣ + max ∣ RV5/V6 ∣;16 Cornell voltage (μV) = SV3 + RaVL;17 and Cornell voltage product (μV/ms) = Cornell voltage * QRS duration.17 The following computer measurements were used to calculate left ventricular mass (gm) for whites: 0.023 Cornell voltage + 0.010 Sokolow-Lyon + 1.32 weight + 10.6; and, for blacks: 0.0018 Cornell voltage + 0.51 JV5 + 1.45 weight + 17.4.18 In MRFIT, approximately 3% of hypertensive men reported their race something other than white or black and left ventricular mass for these men is determined using the formula for whites.
Statistical Analysis
We assessed the association between CTD and HCTZ use and LVH using two types of analyses: 1) an ecologic analysis, with the 22 MRFIT clinics classified (as in previous reports) as “C”-clinics, “H”-clinics, or “switching”-clinics;4,5 and, 2) an individual participant analysis, with use of CTD, HCTZ, or antihypertensive medication other than CTD or HCTZ considered time-dependent covariates and updated annually. Both analyses were restricted to men hypertensive at baseline. The ecologic analysis was carried out through 4 years of follow-up, the last measurement prior to the recommendation to switch all participants to 50 mg of CTD; it utilized information from both SI and UC participants who were hypertensive at entry into C- or H-clinics. The individual participant analysis was performed for the same 4-year period and also for the duration of the trial (84 months) taking into account individual changes in CTD and HCTZ prescriptions; it used information for all SI hypertensive men, including those in the “switching” clinics, but not men in the UC group. Both the ecologic and individual participant analyses were repeated excluding participants with major conduction defects as evidenced by QRS ≥ 120 ms.19
Ecologic Analysis
The ecologic analysis takes advantage of the randomization to SI and UC which was carried out within-clinic. As a consequence, SI and UC men within-clinic are similar on average with respect to baseline characteristics, both those measured and not measured. For the ecologic analysis, the estimand used to quantify differences between CTD and HCTZ for blood pressure and LVH is the difference in “intention to treat” estimands (SI-UC) for C-clinics versus H-clinics (i.e., a difference of differences). Two potential limitations of this estimand are that the grouping variable, CTD or HCTZ, determined post-randomization, may be a marker for a factor other than CTD or HCTZ that is related to LVH, as well as the possibility of misclassification within clinic grouping (e.g., not all SI participants in the C-clinics were treated for hypertension and some used HCTZ).20 To assess the likelihood that the clinic label of C- or H- was due to another factor related to LVH, we carried out an analysis for men who were normotensive at entry. Since fewer of these men were initiated on antihypertensive drugs during follow-up, we hypothesized that differences among C- and H-clinics would be minimal, and if so, would provide support for the inference that differences between clinics for the hypertensive men are due primarily to differences in use of CTD and HCTZ.
Treatment groups were compared for blood pressure and continuous measures of LVH using longitudinal regression analyses (SAS PROC MIXED, SAS Version 9.2). Within-clinic groupings, analyses were stratified by clinic, with baseline level of assessed outcome included as a covariate. To determine whether SI-UC differences in LVH varied among C- and H-clinics, an interaction term (treatment group x clinic grouping) was included in the regression models.
Individual Participant Analysis
For the individual participant analysis, the estimand of C-H differences in blood pressure and LVH is the difference during follow-up among the subset of hypertensive participants in the SI group who were prescribed these treatments. This estimator is subject to the usual type of confounding present in epidemiological analyses.
Longitudinal regression models were used to study the association of time-updated antihypertensive drugs use and LVH. Analyses were also carried out for change in the measures of LVH at 48-months (i.e., a single time point as in the ecologic analysis instead of all follow-up time points). SI participants were categorized as being prescribed CTD, HCTZ, an antihypertensive drug other than CTD or HCTZ, or on no antihypertensive medications, and differences between CTD and HCTZ were assessed. Two models were considered. One model included the following baseline covariates: age, race, serum cholesterol, smoking status, body mass index, systolic blood pressure, use of antihypertensive medication, serum potassium, fasting serum glucose, serum creatinine, uric acid, proteinuria (1+ or greater), number of alcoholic drinks per week, clinic, and baseline level of the electrocardiographic measure considered. A second model included a propensity score. The propensity score, which was the probability of using HCTZ instead of CTD at 48 months as a function of baseline predictors, was determined using logistic regression. The aforementioned baseline covariates were used as predictors. Regression models similar to those described above were also used to study the relationship of change in LVH with change in blood pressure for SI participants.
RESULTS
Study Cohort
Of the 8,012 hypertensive men enrolled in MRFIT, 2,112 (1,046 SI and 1,066 UC) were randomized by six clinics that predominantly used CTD (i.e., C-clinics); 3,399 (1,725 SI and 1,674 UC) were randomized by nine clinics that predominantly used HCTZ (i.e., H-clinics); and 2,501 (1,248 SI and 1,253 UC) were randomized by seven clinics that initially used CTD then switched to HCTZ during the first 4 years of the study (i.e., switching-clinics). As previously reported, the characteristics of SI and UC hypertensive men were well-balanced at baseline.3 This was also the case for the SI-UC comparison within the 3 groups of clinics (data not shown).
Table 1 summarizes the baseline characteristics for the hypertensive participants overall, and by clinic grouping. Baseline characteristics, including continuous measures of LVH, were similar for participants in C- and H-clinics. Participants in the switching clinics were less likely to be black and to smoke. Overall, average systolic and diastolic BP levels were 141.2 mmHg and 95.5 mmHg, respectively. Approximately 31% were taking antihypertensive medications at entry.
Table 1.
Baseline characteristics of MRFIT participants hypertensive at entry, by clinic grouping.
| Variable | C-clinics | H-clinics | Switching- clinics |
Total |
|---|---|---|---|---|
| Number of participants | 2112 | 3399 | 2501 | 8012 |
| Age (years)* | 46.8 (5.8) | 46.7 (5.9) | 46.6 (5.9) | 46.7 (5.9) |
| Black (%) | 10.0 | 10.7 | 5.5 | 8.9 |
| Smoker (%) | 58.6 | 56.1 | 50.9 | 55.1 |
| Serum cholesterol (mg/dl)* | 249.3 (36.6) | 249.7 (36.6) | 251.7 (34.4) | 250.2 (35.9) |
| Body mass index (kg/m2)* | 27.8 (3.4) | 28.0 (3.5) | 28.0 (3.5) | 28.0 (3.5) |
| Systolic blood pressure (mm Hg)* | 142.0 (13.1) | 141.5 (13.1) | 140.2 (12.5) | 141.2 (12.9) |
| Diastolic blood pressure (mm Hg)* | 95.8 (6.9) | 95.5 (6.7) | 95.3 (6.6) | 95.5 (6.7) |
| Potassium (mmol/L)* | 4.36 (0.46) | 4.37 (0.48) | 4.38 (0.44) | 4.37 (0.46) |
| On antihypertensive medication (%) | 31.3 | 31.0 | 30.9 | 31.1 |
| Left ventricular hypertrophy (%), by Minnesota code |
2.3 | 2.7 | 2.3 | 2.5 |
| Electrocardiographic Measurement | ||||
| Absolute maximum of R amplitude V5/6 (μV)* | 1702.0 (515.4) | 1677.8 (530.9) | 1726.1 (525.2) | 1699.4 (525.4) |
| Absolute S amplitude V1 (μV)* | 947.4 (461.5) | 979.3 (461.6) | 921.3 (445.4) | 952.7 (457.2) |
| R amplitude aVL (μV)* | 290.3 (251.3) | 271.0 (251.5) | 268.4 (240.8) | 275.3 (248.3) |
| Absolute S amplitude V3 (μV)* | 1031.3 (467.6) | 1065.2 (467.6) | 1019.6 (463.7) | 1042.0 (466.8) |
| QRS duration (ms) | 85.3 (9.4) | 84.7 (9.6) | 85.5 (9.3) | 85.1 (9.4) |
| Criteria for Electrocardiographic Left Ventricular Hypertrophy | ||||
| Sokolow-Lyon (SL) (μV)* | 2649.4 (789.4) | 2657.3 (788.3) | 2647.3 (768.4) | 2652.1 (782.3) |
| Cornell voltage (μV)* | 1322.1 (527.0) | 1336.2 (528.5) | 1288.1 (517.6) | 1317.4 (525.1) |
| Cornell voltage product (μV/ms)* | 113.9 (49.8) | 114.5 (50.7) | 111.3 (49.1) | 113.3 (50.0) |
| Left ventricular mass (gm)* | 178.0 (21.6) | 177.4 (22.6) | 178.9 (21.4) | 178.0 (21.9) |
mean (S.D.)
Formulas: Sokolow-Lyon voltage (μV) = ∣SV1∣ + max ∣RV5/V6∣
Cornell voltage (μV) = SV3 + RaVL
Cornell voltage product (μV/ms) = Cornell voltage * QRS duration
Left ventricular mass (white men): 0.023 Cornell voltage + 0.010 Sokolow-Lyon + 1.32 weight + 10.6
Left ventricular mass (black men): 0.0018 Cornell voltage + 0.51 JV5 + 1.45 weight + 17.4
Use of CTD, HCTZ and Other Antihypertensives in MRFIT
Figure 1 gives the percentage of SI participants prescribed CTD or HCTZ or other treatment (neither CTD nor HCTZ) by month of follow-up, irrespective of clinic grouping. Use of CTD declined during the first 4 years, from approximately 33.4% at 12 months to 26.6% at 48 months, while use of HCTZ increased from 27.4% at 12 months to a high of 42.5% at 48 months. Following the protocol change, which occurred after all participants had completed the 48 month visit, use of CTD increased (to 50.8% by 84 months) while use of HCTZ declined to 14.7% by 84 months.
Figure 1.
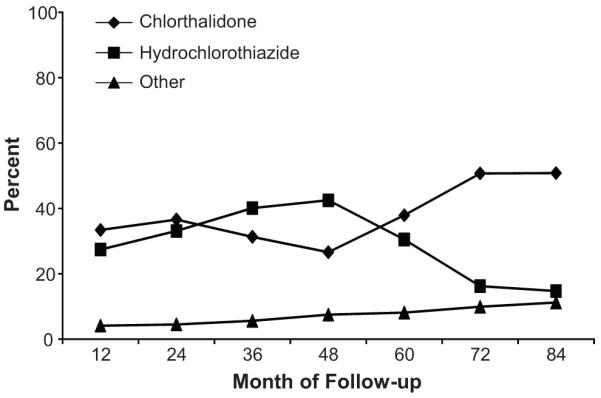
Percent of SI participants (hypertensive at baseline) who were prescribed CTD, HCTZ, or other antihypertensive drugs besides CTD and HCTZ, by month of follow-up.
At 48 months, of SI hypertensive participants, 80% in C-clinics, 75% in H-clinics, and 76% in switching clinics were prescribed antihypertensive medication. The distribution of CTD and HCTZ use according to clinic grouping is summarized in Figure 2. Among C-clinics, use of CTD ranged from 43-58% (average=48%), while among H-clinics, use of HCTZ ranged from 40-61% (average=49.5%). In the switching clinics, 49.7% of SI participants were prescribed HCTZ and 21.2% were prescribed CTD. After the protocol change (i.e., by the 72 month follow-up visit), these percentages were approximately reversed – among SI participants in the switching clinics, 51.4% were prescribed CTD and 16.8% were prescribed HCTZ (data not shown). Less than 10% of UC participants were prescribed CTD in each of the clinic groupings and about 35% were prescribed HCTZ at 48 months.
Figure 2.
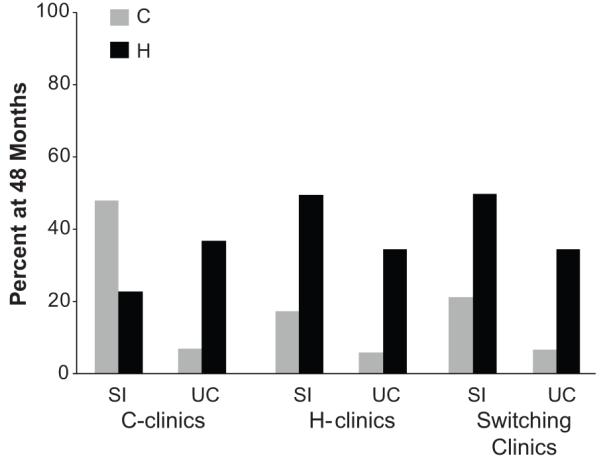
Percent of SI and UC participants prescribed CTD and HCTZ at 48 months according to clinic grouping: C-clinics, H-clinics, and switching-clinics.
Additional antihypertensive medication was added to the diuretic used to achieve BP goal. In C-clinics, 52.9% of SI participants at 48 months were prescribed a Step 2 drug, 13.2% were prescribed Step 3, and 0.6% were prescribed Step 4. In SI participants of H-clinics, the corresponding percentages were 42.4%, 12.0%, and 0.7%.
Blood Pressure and LVH Measures through 48 Months According to C- or H-Clinic
Changes in systolic and diastolic blood pressure were greater for SI compared to UC participants in both the C- and H-clinics. The SI-UC differences were greater within C-clinics compared to H-clinics for systolic (−10.4 vs −8.6 mm Hg; P=0.001 for clinic difference) and diastolic blood pressure (−6.5 vs −5.1 mmHg; P<0.001 for clinic difference) (Table 2). All continuous LVH measures were significantly lower in the SI compared to UC group, regardless of clinic designation. Mean differences between SI and UC in these measures were all uniformly of greater magnitude in the C- compared to the H-clinics (P-values for interaction between C- and H-clinics: Sokolow-Lyon, P=0.049; Cornell voltage, P=0.019; Cornell voltage product, P=0.071; left ventricular mass, P=0.002).
Table 2.
Mean blood pressure, potassium, and electrocardiographic changes from baseline through 48 months by treatment group for C- and H-clinics in MRFIT.
| C-clinics | H-clinics | ||||||
|---|---|---|---|---|---|---|---|
| Variable | SI | UC | SI-UC difference (S.E.) |
SI | UC | SI-UC difference (S.E.) |
P-Value for interaction* |
| Systolic blood pressure (mm Hg) |
−19.7 | −9.4 | −10.4 (0.4) | −18.1 | −9.5 | −8.6 (0.3) | .001 |
| Diastolic blood pressure (mm Hg) |
−11.5 | −5.0 | −6.5 (0.3) | −11.3 | −6.3 | −5.1 (0.2) | .000 |
| Potassium (mmol/L) | −0.42 | −0.08 | −0.33 (0.02) | −0.31 | −0.08 | −0.23 (0.01) | .000 |
| Electrocardiographic Measurement | |||||||
| R amplitude aVL (μV) | −13.3 | 7.1 | −20.4 (4.6) | 20.8 | 32.3 | −11.5 (4.4) | .218 |
| S Amplitude V3 (μV) | −136.1 | −88.7 | −47.4 (8.5) | −138.7 | −114.2 | −24.5 (7.1) | .066 |
| QRS duration (ms) | 0.7 | −0.3 | 1.0 (0.2) | 1.2 | 0.4 | 0.8 (0.2) | .552 |
| Criteria for Electrocardiographic Left Ventricular Hypertrophy | |||||||
| Sokolow-Lyon (μV) | −346.3 | −252.4 | −93.9 (15.1) | −297.1 | −242.2 | −54.9 (12.1) | .049 |
| Cornell voltage (μV) | −149.5 | −81.4 | −68.1 (9.6) | −117.9 | −82.0 | −35.9 (8.0) | .019 |
| Cornell voltage product (μV/ms) |
−11.9 | −7.4 | −4.6 (0.9) | −8.7 | −6.5 | −2.2 (0.8) | .071 |
| Left ventricular mass (gm) |
−8.4 | −4.1 | −4.4 (0.4) | −7.5 | −4.7 | −2.8 (0.3) | .002 |
The p-value for interaction assesses whether the SI-UC differences for C- and H- clinics differ significantly from one another.
SI = special intervention; UC = usual care
Analyses were also carried out for the men who were normotensive at entry to determine whether differences between C- and H-clinics were evident in this subgroup. Participants randomized to SI with repeated diastolic blood pressure ≥ 90 mmHg during follow-up were placed on antihypertensives. Overall, the percent of SI men who were normotensive at entry receiving antihypertensives at 48 months was much smaller (22.2%) than for men hypertensive at entry (76.5%). Likewise, while differences in use of CTD and HCTZ were evident among clinics (13.4% used CTD and 9.3% used HCTZ among C-clinics and 5.0% used CTD and 12.9% used HCTZ among H-clinics at 48 months), the percentages using these drugs were much smaller than for hypertensive men. Consequently, SI-UC differences in blood pressure change were smaller. Differences in systolic blood pressure for SI-UC averaged -2.6 mmHg (SE=0.46) for C-clinics and −3.0 mmHg (SE=0.34) for H-clinics (P=0.56 for difference), while SI-UC differences in diastolic blood pressure averaged −1.8 (SE=0.30) and −2.1 (SE=0.22) mmHg respectively, for C- and H-clinics (P=0.48 for difference). Differences in SI-UC in LVH did not vary significantly by C- or H-clinic grouping (Sokolow-Lyon, P=0.35; Cornell voltage, P=0.12; Cornell voltage product, P=0.26; left ventricular mass, P=0.49).
Only a small number of participants had a QRS duration ≥ 120 mm (11 participants at baseline and ≤12 at each annual visit). Exclusion of these participants did not impact the results.
Individual Participant Analysis with Time-Updated Use of CTD and HCTZ – All SI Hypertensives
Table 3 summarizes differences between CTD and HCTZ for the individual participant analysis of SI men; it is based on all annual follow-up measures of LVH through 48 and 84 months. For comparison, the estimand based on the clinic analysis shown in Table 2 is given in the last column. Similar to the clinic-level analysis, differences in blood pressure and in most measures of LVH significantly favored participants taking CTD. However, for Cornell voltage product, the CTD-HCTZ differences were significant in the opposite direction of the ecologic analysis, and no significant difference was observed for the Cornell voltage measure between CTD and HCTZ. In contrast to the clinic analyses, we also found that QRS duration (the multiplicand to convert Cornell voltage to Cornell voltage product) was greater for CTD compared to HCTZ. Unadjusted (no covariate adjustment) estimates of the CTD-HCTZ differences were similar to those in Table 3 (data not shown). Likewise, when the covariate adjustment was expanded to include use of Step 2, 3 and 4 drugs, the CTD-HCTZ differences in blood pressure and measures of LVH were similar.
Table 3.
Mean differences in blood pressure, potassium, and electrocardiographic LVH through 48 and 84 months for individual SI participants who were hypertensive at baseline, and comparison with differences between C- and H-clinic SI-UC differences through 48 months.
| Through 48 Months | Through 84 Months | SI-UC Difference for C- vs H-Clinics (Through 48 Months)† |
|||||
|---|---|---|---|---|---|---|---|
| Variable | C-H difference* |
95% CI | P- value |
C-H difference* |
95% CI | P- value |
|
| Systolic blood pressure (mm Hg) |
−1.6 | −2.1, −1.1 | < .001 | −1.7 | −2.1, −1.3 | < .001 | −1.8 |
| Diastolic blood pressure (mm Hg) |
−0.7 | −1.0, −0.4 | < .001 | −0.8 | −1.0, −0.5 | < .001 | −1.4 |
| Potassium (mmol/L) | −0.23 | −0.3, −0.2 | <.001 | −0.23 | −0.2, −0.2 | <.001 | −0.10 |
| Electrocardiographic Measurement | |||||||
| Absolute maximum of R amplitude V5,6 (μV) |
−23.8 | −37.3, −10.3 | < .001 | −7.9 | −17.5, 1.7 | .11 | −8.8 |
| Absolute S amplitude V1 (μV) |
−12.4 | −24.8, 0.1 | .05 | −16.0 | −25.3, −6.7 | < .001 | −31.6 |
| R amplitude aVL (μV) | 4.5 | −2.0, 11.0 | .17 | 3.4 | −1.3, 8.1 | .16 | −9.0 |
| Absolute S amplitude V3 (μV) |
0.6 | −10.5, 11.6 | .92 | −4.8 | −12.7, 3.0 | .23 | −22.9 |
| QRS duration (ms) | 0.9 | 0.6, 1.3 | < .001 | 0.8 | 0.6, 1.1 | < .001 | 0.2 |
| Criteria for Electrocardiographic Left Ventricular Hypertrophy | |||||||
| Cornell voltage (μV) | 4.4 | −8.1, 16.9 | .49 | −0.9 | −9.9, 8.1 | .84 | −32.1 |
| Sokolow-Lyon (μV) | −37.5 | −56.6, −18.5 | < .001 | −26.3 | −40.1, −12.4 | < .001 | −38.9 |
| Cornell voltage product (μV/ms) |
1.8 | 0.5, 3.0 | .007 | 1.3 | 0.3, 2.2 | .007 | −2.3 |
| Left ventricular mass (gm) | −0.5 | −1.0, −0.0 | .04 | −0.5 | −0.8, −0.2 | .004 | −1.6 |
Change in systolic and diastolic blood pressure adjusted for baseline blood pressure level and for age, race, and baseline serum cholesterol, HDL, LDL, triglycerides, antihypertensive use, glucose, creatinine, potassium, proteinuria, uric acid, drinks per week, body mass index, and smoking status. Change in electrocardiographic level adjusted for baseline electrocardiographic level and for age, race, and baseline systolic blood pressure, diastolic blood pressure, serum cholesterol, HDL, LDL, triglycerides, antihypertensive use, glucose, creatinine, potassium, proteinuria, uric acid, drinks per week, body mass index, and smoking status.
Adjusted for baseline level only
A propensity score analysis which compares CTD and HCTZ for each of the LVH measures at 48 months is summarized in the online supplement (please see http://hyper.ahajournals.org). The first step in this analysis was to determine factors associated with the use of HCTZ (vs CTD) among hypertensive men at 48 months (i.e., the propensity for using HCTZ). Older age and use of antihypertensive treatment at entry were significantly associated with less use of CTD than HCTZ. No other factor besides clinic was significantly associated with the use of HCTZ vs CTD. After adjustment of CTD vs HCTZ differences in blood pressure and LVH for propensity score, the results for LVH measures were similar to Table 3.
To explore the differences between clinic and individual participant analyses for Cornell voltage and product, we carried out a subgroup analysis according to use of antihypertensive treatment at entry, the most important predictor of using CTD in the propensity score analyses. For the individual participant analyses, interaction p-values were P=0.22 for Cornell voltage and P=0.29 for Cornell voltage product; for the clinic analyses, the interaction p-values were P=0.16 for Cornell voltage and P=0.20 for Cornell voltage product.
Blood pressure reductions in the SI group with hypertension at entry were associated with decreases in each of the LVH measures (P<0.001 for each measure). The association of blood pressure change with LVH change was similar for SI participants in C- and H-clinics and for UC participants.
DISCUSSION
The presence of LVH in MRFIT has been independently associated with an increased risk of cardiovascular death.13-15 Our primary analysis found that SI-UC differences in continuous measures of electrocardiographic LVH were of greater magnitude in C-clinics than in H-clinics, suggesting a differential benefit in favor of treatment with CTD compared to HCTZ. When examined at the individual participant level, those receiving CTD also had less LVH as assessed by Sokolow-Lyon and left ventricular mass criteria than those receiving HCTZ. These findings occurred when both CTD and HCTZ were widely used through 48 months, and persisted after participants were switched to CTD through long-term (84 months) follow-up. Our analyses offer new insight into the recent report from MRFIT concluding that CTD is more effective at reducing cardiovascular events than HCTZ.21
Our study results are consistent with earlier reports from MRFIT which have shown that overall LVH incidence was lower in the SI compared to the UC group and that reductions in blood pressure were associated with a reduced incidence of LVH.13 It is possible that the differences in LVH between CTD and HCTZ may have occurred as a consequence of improved blood pressure control in participants receiving CTD than HCTZ. The change in systolic blood pressure from baseline to 48 months between SI and UC groups was 1.7 mmHg greater in participants of C-clinics than H-clinics; these differences were also consistent with differences for CTD vs HCTZ observed at the individual participant level. Importantly, office blood pressure measurements were taken in MRFIT during daytime hours and may not have reflected potentially larger blood pressure differences between regimens occurring over an entire 24-hour period.
Several limitations typical of post-hoc analyses should be noted. Diuretic assignment in MRFIT was not randomized, leading to heterogeneity of diuretic use within the C- and H-clinics and the potential for misclassification within clinic grouping (i.e., not all SI participants in the C- clinics were treated for hypertension and some received HCTZ). However, unlike the individual participant analysis, confounding within the clinic designation is protected by overall randomization to SI or UC group. The results of the ecologic analysis are further strengthened by the absence of differences in LVH between SI and UC groups in the analysis of men normotensive at entry, which supports the notion that hypertensive men were affected differently by use of CTD vs HCTZ. Second, higher doses of both CTD and HCTZ were used in MRFIT than what are currently utilized. Given established potency differences between the two agents, it is not clear whether the lower doses of CTD and HCTZ in common use today would give similar results. Third, LVH was assessed using electrocardiography rather than by echocardiography or magnetic resonance imaging. While these newer methods of cardiac imaging may be more sensitive, electrocardiographically-determined LVH remains an established predictor of cardiovascular disease risk in both MRFIT and elsewhere.8,9,12-15
Lastly, the findings for Cornell voltage and product in the individual participant analysis were not consistent with those of the ecologic (clinic-level) analysis. We conducted sensitivity analyses of the individual components of the Cornell LVH measures and observed that the discrepancy may result, in part, from a significant increase in QRS duration found in individual participant analyses but not in clinic analyses. We also assessed whether the CTD and HCTZ differences varied by use of antihypertensive treatment at entry and the evidence for subgroup heterogeneity was weak.
Perspectives
Previous MRFIT reports have documented a lower incidence of LVH for SI compared to UC men, but these analyses did not assess possible differences related to use of CTD vs HCTZ. In ecologic analyses, we found that SI-UC differences in electrocardiographically-defined continuous measures of LVH were of greater magnitude in clinics with high utilization of CTD compared to those where HCTZ predominated. At the individual participant level for all SI hypertensives, both Sokolow-Lyon and left ventricular mass measures were also lower in users of CTD compared to HCTZ. Given the strong association between LVH and blood pressure, our findings suggest that differences in blood pressure lowering may explain the variation in mortality observed between CTD and HCTZ in MRFIT, and also underscore the need for a randomized clinical outcome trial comparing the two agents.
Supplementary Material
Acknowledgements
We express appreciation to the MRFIT study participants and the many investigators who contributed to the design and conduct of the study.
Sources of funding: The Multiple Risk Factor Intervention Trial was supported by a contract and grants from the National Heart, Lung, and Blood Institute. This funding included R01-HL68140.
Footnotes
Disclosures: All authors report no conflicts of interest in the publication of this manuscript.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ernst ME, Moser M. Use of diuretics in patients with hypertension. N Engl J Med. 2009;361:2153–2164. doi: 10.1056/NEJMra0907219. [DOI] [PubMed] [Google Scholar]
- 2.Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the veterans health administration. J Clin Hypertens (Greenwich) 2010;12:927–934. doi: 10.1111/j.1751-7176.2010.00373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Multiple Risk Factor Intervention Trial Research Group Multiple Risk Factor Intervention Trial. Risk factor changes and mortality results. JAMA. 1982;248:1465–1477. [PubMed] [Google Scholar]
- 4.Multiple Risk Factor Intervention Trial Research Group Mortality after 10 ½ years for hypertensive participants in the Multiple Risk Factor Intervention Trial. Circulation. 1990;82:1616–1628. doi: 10.1161/01.cir.82.5.1616. [DOI] [PubMed] [Google Scholar]
- 5.Bartsch G, Broste S, Grandits G, Grimm RH, Neaton JD, Svendsen KH. Hydrochlorothiazide, chlorthalidone and mortality in the Multiple Risk Factor Intervention Trial. Circulation. 1984;70(suppl II):1438. (abstract) [Google Scholar]
- 6.Ernst ME, Carter BL, Goerdt CJ, Steffensmeier JJ, Phillips BB, Zimmerman MB, Bergus GR. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47:352–358. doi: 10.1161/01.HYP.0000203309.07140.d3. [DOI] [PubMed] [Google Scholar]
- 7.Bacharova L, Estes H, Bang L, Rowlandson I, Schillaci G, Verdecchia P, Macfarlane PW. The first statement of the Working Group on Electrocardiographic Diagnosis of Left Ventricular Hypertrophy. J Electrocardiol. 2010;43:197–199. doi: 10.1016/j.jelectrocard.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh BP, Pham MX, Froelicher VF. Prognostic value of electrocardiographic criteria for left ventricular hypertrophy. Am Heart J. 2005;150:161–167. doi: 10.1016/j.ahj.2004.08.041. [DOI] [PubMed] [Google Scholar]
- 9.Jain A, Tandri H, Dalal D, Chahal H, Soliman EZ, Prineas RJ, Folsom AR, Lima JA, Bluemke DA. Diagnostic and prognostic utility of electrocardiography for left ventricular hypertrophy defined by magnetic resonance imaging in relationship to ethnicity: the Multi-Ethnic Study of Atherosclerosis (MESA) Am Heart J. 2010;159:652–658. doi: 10.1016/j.ahj.2009.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen JD, Grimm RH, Smith WM. Multiple Risk Factor Intervention Trial. VI. Intervention on blood pressure. Prev Med. 1981;10:501–518. doi: 10.1016/0091-7435(81)90062-1. [DOI] [PubMed] [Google Scholar]
- 11.Wolf H, MacInnis PJ, Stock S, Helppi RK, Rautaharju PM. The Dalhousie Program: a comprehensive analysis program for rest and exercise electrocardiograms. In: Zwietz C, Schneider B, editors. Computer Application on ECG and VCG Analysis. North-Holland Publishing; Amsterdam: 1973. pp. 231–288. [Google Scholar]
- 12.Multiple Risk Factor Intervention Trial Research Group Baseline rest electrocardiographic abnormalities, antihypertensive treatment and mortality in the Multiple Risk Factor Intervention Trial. Am J Cardiol. 1985;55:1–15. doi: 10.1016/0002-9149(85)90290-5. [DOI] [PubMed] [Google Scholar]
- 13.MacMahon S, Collins G, Rautaharju P, Cutler J, Neaton J, Prineas R, Crow R, Stamler J, for the Multiple Risk Factor Intervention Trial Research Group Electrocardiographic left ventricular hypertrophy and effects of antihypertensive drug therapy in hypertensive participants in the Multiple Risk Factor Intervention Trial. Am J Cardiol. 1989;63:202–210. doi: 10.1016/0002-9149(89)90286-5. [DOI] [PubMed] [Google Scholar]
- 14.Crow RS, Prineas RJ, Hannan PJ, Grandits G, Blackburn H. Prognostic associations of Minnesota code serial electrocardiographic change classification with coronary heart disease mortality in the Multiple Risk Factor Intervention Trial. Am J Cardiol. 1997;80:138–144. doi: 10.1016/s0002-9149(97)00307-x. [DOI] [PubMed] [Google Scholar]
- 15.Prineas RJ, Rautaharju PM, Grandits G, Crow R, for the MRFIT Research Group Independent risk for cardiovascular disease predicted by modified continuous score electrocardiographic criteria for 6-year incidence and regression of left ventricular hypertrophy among clinically disease free men: 16-year follow-up for the Multiple Risk Factor Intervention Trial. J Electrocardiol. 2001;34:91–101. doi: 10.1054/jelc.2001.23360. [DOI] [PubMed] [Google Scholar]
- 16.Sokolow M, Lyon T. Ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J. 1949;37:161–186. doi: 10.1016/0002-8703(49)90562-1. [DOI] [PubMed] [Google Scholar]
- 17.Molloy TJ, Okin PM, Devereux RB, Kligfield P. Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J Am Coll Cardiol. 1992;20:1180–1186. doi: 10.1016/0735-1097(92)90376-x. [DOI] [PubMed] [Google Scholar]
- 18.Rautaharju PM, Park LP, Gottdiener JS. Race- and sex-specific ECG models for left ventricular mass in older populations. Factors influencing overestimation of left ventricular hypertrophy prevalence by ECG criteria in African-Americans. J Electrocardiol. 2000;33:205–218. doi: 10.1054/jelc.2000.7667. [DOI] [PubMed] [Google Scholar]
- 19.Hancock EW, Deal BJ, Mirvis DM, Okin P, Kligfield P, Gettes LS. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram. Part V: electrocardiogram changes associated with cardiac chamber hypertrophy. A scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee; Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53:992–1002. doi: 10.1016/j.jacc.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 20.Morgenstern H. Uses of ecologic analysis in epidemiologic research. Am J Public Health. 1982;72:1336–1344. doi: 10.2105/ajph.72.12.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorsch MP, Gillespie BW, Erickson SR, Bleske BE, Weder AB. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57:689–694. doi: 10.1161/HYPERTENSIONAHA.110.161505. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


