Abstract
Muscle power declines earlier and more precipitously with advancing age compared to muscle strength. Peak muscle power has also emerged as an important predictor of functional limitations in older adults. Our current working hypothesis is focused on examining lower extremity muscle power as a more discriminant variable for understanding the relationships between impairments, functional limitations and resultant disability with aging.
Keywords: Aging, muscle power, exercise physiology, physical function, mobility-disability
Introduction
The prevention or postponement of mobility limitations for the aging population is of major public health importance. Mobility, the ability to move without assistance, is critical for maintaining independent functioning. Limitations in mobility, typically defined as difficulty in performing physical tasks such as walking one-quarter mile, climbing a flight of stairs or rising from a chair, are indicative of a marked decline in functional health(35). With persons aged 60 years or older representing the fastest growing segment of the worldwide population, there will continue to be a corresponding increase in the prevalence of mobility limitations. Improved knowledge of the specific physiologic mechanisms that mediate impairments in physical functioning will be crucial for developing effective therapeutic interventions for preserving mobility and independence among older people.
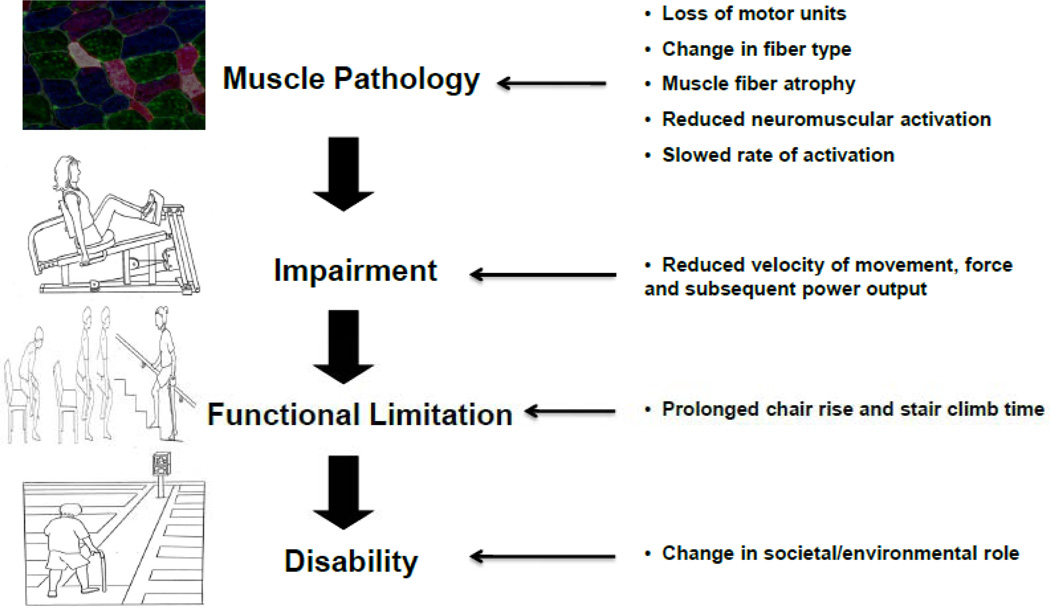
According to the disablement model, impairment refers to a loss or abnormality at the tissue, organ and body system level(35). At an individual level, impairments can progress to functional limitations and to subsequent disability. Although a large number of studies have established the role of muscle strength (the ability to generate maximal muscle force) as a proximal determinant of functional limitations in older adults, skeletal muscle power (the product of the force and velocity of muscle contraction) has been shown to decline earlier and more rapidly than muscle strength with advancing age(1). The underlying physiological mechanisms that contribute to this reduction in muscle power output among older adults include: a quantitative decline in muscle mass (sarcopenia), changes in muscle composition, muscle quality (reduced muscle strength per unit muscle mass), individual muscle fiber contractile properties and alterations in neuromuscular function(1, 24).
Our current working hypothesis is focused on examining lower extremity muscle power as a more critical variable in understanding the relationship between impairments, functional limitations, and resultant disability (Figure 1). This review article will summarize studies from our research group that have identified peak muscle power as a more influential predictor of functional performance in older adults compared to muscle strength. We will also describe recent evidence from our work investigating the underlying physiological determinants of skeletal muscle power impairments among elders with overt mobility limitations. Finally, we will describe novel therapeutic interventions targeted at restoring muscle power in older individuals.
Figure 1.
Power driven pathway to age-associated disability. [Adapted from (35). Copyright © 1994 Elsevier. Used with permission.]
Assessment of Lower Extremity Muscle Power in Older Adults
When muscle power is assessed across a range of external resistances (40%–90% of one repetition maximum (1RM)), peak muscle power is typically yielded at approximately 70% of the 1RM while maximal contraction velocity typically occurs at the lowest external resistance (40% of 1RM)(11, 15, 18). Dynamic muscle strength typically represents the greatest load lifted during a 1RM testing protocol. Muscle strength can also be reliably assessed using isokinetic or isometric dynamometry. Since the 1990’s, peak skeletal muscle power has been examined as an outcome variable distinct from muscle strength. Additional methods that have been developed to assess lower extremity muscle power in older individuals include vertical jump on a force platform, unloaded leg extensor power evaluation and isokinetic dynamometry. Evaluation of muscle power output using lower extremity pneumatic resistance training equipment has recently emerged as an accurate and valid muscle power assessment modality, particularly as this methodology can reliably capture the force and velocity components of muscle power output(18, 30). A recent systematic evaluation of this methodology demonstrated that peak power assessment with a multiple attempt protocol using pneumatic resistance equipment yields significantly higher performance and better reliability than protocols involving a single attempt at varying external resistances on pneumatic equipment in older adults (11). This multiple attempt protocol maximizes the achievement of maximal contraction velocity and subsequent maximal muscle power output and is feasible for the assessment of lower extremity muscle power in frail older populations.
Lower Extremity Muscle Power and Functional Performance
The seminal investigation by Bassey and coworkers (2) examined the contribution of muscle power to various functional tasks in frail institutionalized elders and demonstrated that leg extensor peak power was predictive of chair rise performance, stair climbing and gait speed. Foldvariet al. (19) further explored the relationships between muscle power, muscle strength and other physiologic factors relevant to functional independence among 80 elderly community-dwelling women with self-reported disability. Peak muscle power (r = 0.47) was superior to muscle strength (r = 0.43) and aerobic capacity (r = 0.40) in determining functional status and independently predicted functional dependency even after accounting for additional neuropsychological and health status indicators.
In a similar population of elderly women with self-reported limitations in function, Suzuki et al. ((34) compared the respective associations of muscle power and strength on performance based functional tasks such as the length of time necessary to rise from a chair ten times or to ascend a flight of stairs as fast as possible. Compared to muscle strength, muscle power of the ankle flexors was a stronger predictor of chair rise (r = 0.58 vs. 0.32) and stair climb performance (r = 0.49 vs. 0.37). Furthermore, muscle power remained an independent predictor of functional performance in multivariate analyses after accounting for muscle strength and additional self-report measures of health status and physical functioning.
It is important to note that inherent limitations may be associated with the ascertainment of self-reported functional status and level of mobility-disability, as older adults may underestimate or overestimate their functional capabilities. To overcome this bias, standardized and objective tests of physical performance such as the Short Physical Performance Battery test (SPPB) have been developed(22). The SPPB has been validated in large-scale epidemiologic studies and offers additional advantages over self-report measures of functional status in terms of applicability and reproducibility. The SPPB characterizes lower extremity function using timed measures of standing balance (side-by-side stand, tandem and semi-tandem positions), gait speed (timed 8-ft walk) and lower extremity strength (timed test of five chair rises). Scores obtained on a 12 point summary scale indicate a gradient of functional decline that has been shown to be highly predictive of subsequent mobility-related disability, institutionalization, and mortality (22). In the majority of recent trials that have enrolled mobility-limited older adult, participants were classified as “mobility-limited” if a SPPB summary performance of ≤ 9 was obtained (4, 6, 7, 14, 15, 26)
Many of the more recent studies examining the relationship between muscle poweron functional performance in older adults have employed the SPPB as study eligibility criteria or as a study outcome measure. (4, 7, 14, 15, 29). Bean et al. (5) examined the relative contribution of muscle power and strength on various measures of physical performance among community-dwelling older men and women with objective mobility-limitations. Compared to muscle strength, leg power consistently explained a greater proportion of the variance (2–8%) on all measures of physical performance (stair climb and chair stand performance, gait speed and the SPPB) assessed in these mobility-limited participants. Bean et al. (9) replicated these observations in a large cohort of 1032 older adults from the InCHIANTI study and demonstrated that impairments in muscle power were more influential proximal determinants of mobility performance than impairments in muscle strength. Older adults with low muscle power output had a 2–3 fold greater risk of significant mobility impairments compared to individuals with low muscle strength.
The independent influence of the velocity component of muscle power and functional performance has been established by several important studies. Compared to muscle strength, contraction velocity of leg extensors has been shown to be a stronger predictor of performance on lower intensity functional tasks such as habitual walking speed (r2 = 0.18 vs. 0.06)(33). Cuoco and colleagues (15) investigated the relationship between peak muscle power generated at high (40% 1RM) and low (70% 1RM) contraction velocitieson functional performance inolder men and women with mobility-limitations. Power output at 40% 1RM explained more of the variability in habitual gait velocity than did peak power at 70% 1RM (59% vs. 51%) and consistently accounted for higher respective percentages of the variance in other functional tasks such as chair rise performance (28% vs. 24%) and stair climb performance (43% vs. 42%). More recently, Mayson and coworkers (26) further illustrated the importance of muscle contraction velocity on balance performance. Among community dwelling older adults with mobility limitations, higher leg press contraction velocity (generated at 40% 1RM) was associated with better performance on several composite measures of balance that are predictive of falling. In the same study population, contraction velocity was shown to be independently predictive of mobility (7). Higher contraction velocity was also associated with higher SPPB status and superior in predicting mobility performance compared to traditional rehabilitive impairments such as aerobic capacity and obesity. This investigation also highlighted the emergence of limb contraction velocity as an important rehabilitive impairment and specific target for therapeutic intervention.
Physiological Determinants of Muscle Power and Mobility Limitations with Advancing Age
As muscle power is the product of force and contraction velocity, factors that lead to a reduction in either of these parameters, or both, will contribute to reduced muscle power output. Decrements in muscle power production with advancing age can be attributed to well-described changes in muscle quantity and quality. Such factors include a quantitative loss of muscle mass and alterations in the properties of individual muscle fibers, in particular, the selective reduction in the number and size of type II muscle fibers with advancing age which have the ability to generate four times the power output of type I fibers (24). Additionally, muscle power loss in older adults is influenced by increases in muscle fat infiltration, changes in neuromuscular function, muscle architecture, alterations in hormonal status, protein synthesis and inflammatory mediators (1, 24). However, among older adults with mobility limitations, a paucity of information exists on the specific underlying physiological mechanisms that contribute to the loss of muscle power. In order to address this important gap in knowledge, our research group has conducted several recent investigations to quantify the major physiological determinants of muscle power production with advancing age in healthy and mobility-limited elders.
Changes in Muscle Mass and Quality
Reid et al. (31) performed a comprehensive cross-sectional assessment of the major physiological mechanisms contributing to muscle power deficits within three distinct populations: healthy middle-aged adults (~ 47 yrs), healthy older adults (~ 74 yrs) and older adults with mobility limitations (~ 78 yrs). In using this experimental design, the authors attempted to examine differences in muscle power generation within a specific age range to potentially capture key factors that contribute to muscle power deficits and mobility limitations in older adults. Mobility-limited elders had significant reductions in lower extremity muscle power compared to healthy middle-aged (− 95%) and healthy older participants (− 65%). Corresponding differences in muscle mass were also quantified using computed tomography, with mobility-limited elders possessing significantly lower muscle mass compared to healthy middle-aged subjects (− 25%) and healthy older participants (− 13%). The magnitude of the discrepancy between the reduction in muscle power and muscle size indicates that other factors, distinct from muscle atrophy, are major contributors to the reductions in muscle power output among mobility-limited participants.
To date, no studies have examined the longitudinal changes in muscle mass among mobility-limited older adults. However, in relatively healthy older subjects, previous studies have reported a significant reduction of 14.7% in thigh muscle cross sectional area (CSA) after a 12 year follow-up period (mean initial age: 65 yrs) and a 5.6% reduction after an 9 year follow-up period (mean initial age: 71 yrs) (20). Goodpaster et al.(21) examined the longitudinal changes (~3 yrs) in muscle mass among 1880 relatively healthy older adults in the Health, Aging and Body Composition Study (mean initial age: 73.5 yrs; range: 70–79 yrs). In this cohort, annualized rates of muscle mass decline were approximately 2% per year. This investigation also noted that the decline in muscle performance (muscle strength) was on average 3-fold higher than the loss of muscle mass over this period, suggesting a decline in muscle quality. Reid et al.(31) also quantified indices of muscle quality (muscle strength and power normalized to muscle CSA) and reported significant differences in specific leg extensor muscle power among the mobility-limited participants while no differences were evident for measures of specific muscle strength across the three study groups evaluated. The similarities in specific strength in this investigation suggested that the preservation of muscle strength with aging has greater dependence on the maintenance of muscle mass, whereas the impairments in muscle power among elders with mobility limitations may develop independently of muscle atrophy with advancing age.
Skeletal Muscle Contractile Properties
The examination of single muscle fiber properties can directly quantify the contractile elements of muscle cells, without the potential confounding effects of factors such as neural influences or muscle architecture. Several studies have shown that single muscle fiber contractile function may be preserved in older adults despite the presence of significant reductions in whole muscle size and composition(20). However, these previous studies have been limited by small sample sizes and have typically included relatively healthy and physically active older subjects. We recently evaluated intrinsic single fiber properties in 34 mobility-limited elders with significant deficits in leg extensor muscle power, mid-thigh muscle size and composition (31). It was evident that the surviving muscle fibers in the mobility-limited elders partially compensated for the major age-related losses at the whole muscle level through maintenance and preservation of single muscle fiber size and contractile function. These findings are consistent with previous studies suggesting that surviving fibers compensate to partially correct deficits at the whole muscle level in an attempt to maintain optimal force-generating capacity (20).
Neuromuscular Activation
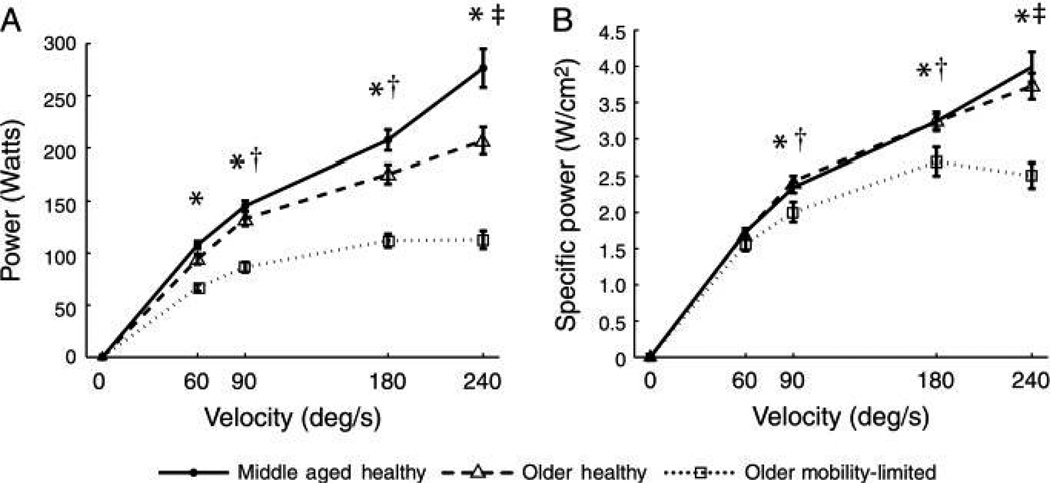
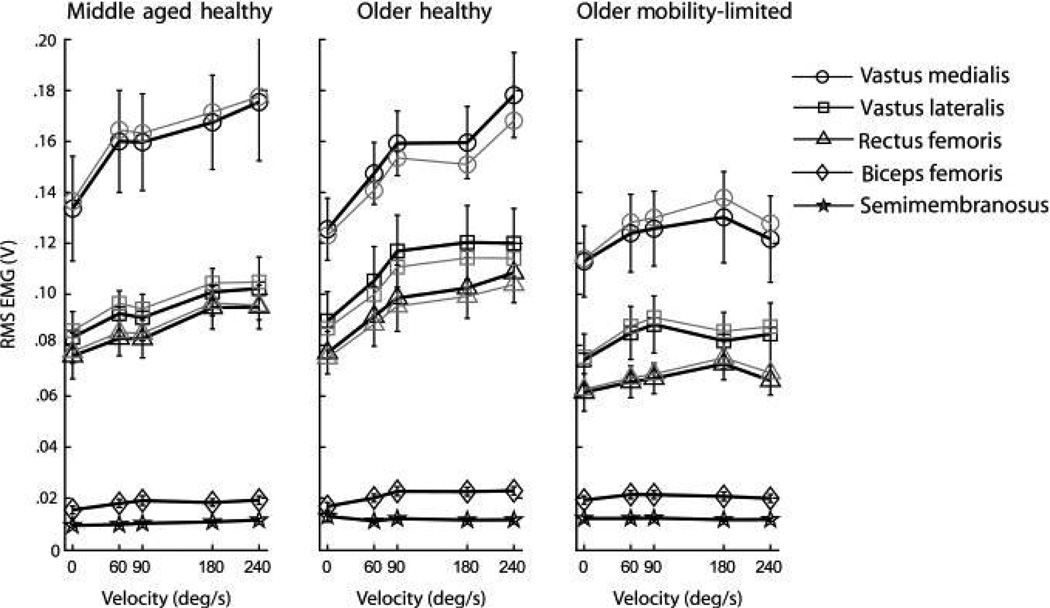
Neuromuscular activation impairments may impact movement velocity and muscle coordination leading to a reduction or a longer time to reach peak force, and thus a decline in muscle power generation. In two recent investigations, we have operationally defined neuromuscular activation as the process by which the nervous system produces muscular force through recruitment and rate coding of motor units (13, 14). Clark et al.(13) delineated the relationship between the neuromuscular system and muscle power generation within older adults with mobility limitations, healthy middle-aged adults and healthy older adults. Using surface electromyography (EMG) on the quadriceps and hamstrings musculature during maximal isokinetic dynamometry testing, mobility-limited elders demonstrated significant impairments in torque, power and agonist muscle activation, with the greatest deficits elicited at the fastest movement velocities (Figure 2 and 3). In addition to deficits in neuromuscular activity, Clark and colleagues (14)also demonstrated reductions in the rate of neuromuscular activity and impaired acceleration during dynamic leg extensions in mobility limited elders. Pre-movement time (i.e. duration between EMG onset and movement onset) and the rate of EMG rise (duration and relative amplitude of muscle activation) were markedly impaired in mobility-limited older adults during maximal power testing compared to healthy middle-aged adults and healthy older adults. This investigation also reported a significant positive association between SPPB score and rate of EMG rise (r = 0.56) among the older participants. Taken together, these studies suggest that impairments in the neuromuscular system may be a major physiologic mechanism contributing to muscle power deficits and mobility limitations with advancing age.
Figure 2.
Absolute power (Watts, A) and specific power (normalized to anterior mid-thigh muscle cross sectional area) (Watts per cm2, B) plotted against movement velocity in middle-aged healthy (mean ± SD age: 47.2 ± 5 yrs), older healthy (74 ± 4 yrs) and older mobility-limited participants (78.1 ± 5 yrs). Testing was conducted using a Cybex-II dynamometer. Five consecutive maximal isokinetic (constant velocity) knee extensions were performed at 60, 90, 180, and 240 degrees second, with participants instructed to kick out as fast and hard as possible. Each testing condition was separated by at least 1 minute of rest. A significant group × velocity interaction was indicated for both power variables with all groups significantly different. Post hoc testing revealed: *older mobility-limited was less than middle-aged healthy adults and older healthy adults; †power has increased from the previous (slower) velocity in middle-aged healthy and older healthy but not in older mobility- limited; and ‡power has increased from the previous (slower) velocity in middle-aged healthy but not in older healthy or older mobility-limited. Older mobility-limited showed no difference is absolute or specific power between contraction velocities (60–90, or between 90, 180 and 240 degrees per second) indicating a plateau in the ability to produce power at faster speeds. (Reprinted from (13).Copyright © 2010 Oxford University Press. Used with permission.)
Figure 3.
Absolute activation (thick black lines) and activation corrected for subcutaneous adipose* (thin gray lines provided for agonist muscles only) plotted against movement velocity. Activation was assessed from quadriceps and hamstrings muscles using surface electromyography (EMG). Agonist activation amplitude for each muscle was higher in middle-aged healthy adults and older healthy adults compared with older adults with mobility limitation. Furthermore, both middle-aged healthy and older healthy demonstrated significant positive associations between activation amplitude and velocity, whereas older mobility-limited did not. *EMG data were corrected because of the recognized signal attenuation caused by subcutaneous adipose tissue. (Reprinted from (13).Copyright © 2010 Oxford University Press. Used with permission.)
Resistance Training Interventions to Restore Muscle Power in Older Adults
Early studies evaluating whether resistance training interventions could increase lower extremity muscle power in older individuals reported minimal improvements. This was primarily because the traditional resistance training interventions employed were performed at relatively slow velocities, thus lacking the training specificity to improve peak muscle power within these populations. However, recent randomized trials designed to maximize muscle power output have generally demonstrated that high velocity power training is feasible, well tolerated, and can effectively improve lower extremity muscle power in healthy older men and women, older women with self-reported disability (18, 25), older adults with mobility limitations (30) and in older women aged over 80 years(12). This distinct type of resistance training ischaracterized by participantsperforming the concentric phase of eachrepetition as fast as possible.
Earleset al. (17) reported a 50–141% increase in leg power following 12 weeks of high velocity resistance training in combination with moderate intensity non-resistance exercise compared to a structured walking program in older men and women. Fielding et al.(18) examined high velocity lower extremity resistance training compared to traditional slow velocity resistance training in older women with self-reported disability. After 16 weeks of training, they observed an 84% greater increase in leg press power in the high velocity training group compared to the low velocity group.
The comparative effects of 12 weeks of high velocity resistance training and traditional strength training on lower extremity muscle power were evaluated in 45 older adults with self-reported mobility limitations(25). Improvements in knee and leg extensor muscle power after high velocity power training were approximately twofold greater compared to gains in muscle power as a result of strength training. Among older adults with mobility-limitations, a 12-week high-velocity resistance training intervention increased lower extremity muscle power (~25%), although these gains were comparable to improvements resulting from traditional slow velocity strength training in this population (~21%)(30). However, in this study, high velocity training was associated with significantly greater improvements in specific leg extensor muscle power (46%) compared to the induced gains from traditional strength training (20%).
While all of the aforementioned studies employed high velocity resistance training coupled with a relatively high external resistances (~70% of 1RM), only one study to date has examined high velocity training at varying external resistances. de Voset al. (16) examined changes in leg power in response to 12 weeks of high velocity resistance training in healthy older adults randomized to one of three different external resistances: 20% 1 RM; 50% 1 RM; or 80% 1 RM. Peak power output improved similarly (14–15%) across all training intensities suggesting that power output can be increased with high velocity training at low and high external resistances. In addition, this study demonstrated a dose-response relationship between the respective training intensities and concomitant improvements in muscle strength (20%) and muscle endurance (185%) elicited when using the highest loading intensity (80% 1RM). Simultaneous improvements in strength and endurance aspects of muscle performance, in addition to muscle power improvements, are likely to play an important role in preserving functional performance in older adults. More recently, 12 weeks of explosive heavy resistance training,with a loading intensity of 75–80% 1RM,demonstrated substantial improvements in muscle power (28%) and marked gains in rapid muscle force generating characteristics in healthy older woman aged 80-89 years(12).
Impact of Muscle Power Training on Physical Function
A number of randomized trials have evaluated the effect of power training interventions on changes in physical functioning in older adults (Table). The majority of these studies compared the effects of high velocity resistance training to conventional strength training or control interventions on functional outcomes.
Table.
Summary of Randomized Trials Investigating the Effects of Power Training on Physical Functioning.
| Study | Participants* | Power Training Intervention | Intervention Frequency & Duration |
Muscle Power Increase |
Significant Improvement in Physical Functioning |
|---|---|---|---|---|---|
| High Velocity Resistance Training | |||||
| Sayers et al. (32) | 15 women with self- reported disability, 73 yrs |
Bilateral leg press, knee extension resistance training performed at 70% 1RM. 3 sets × 8 repetitions (concentric phase at maximal velocity) |
3 × wk, 16 wks | Leg press: 97% | Balance: 5% Stair climb time: 13% |
| Henwood etal. (23) |
19 males and females, 71 yrs |
6 multi-joint upper & lower body resistance training at 40%-75% 1RM. 3 sets × 8 repetitions (concentric phase at maximal velocity) |
2 × wk, 24 wks | Leg extension: 62% Leg press: 58% |
Stair climb time: 6.5% 6 m fast walk time: 15% 5-Chair stand time: 13% Functional reach test (cm): 9% |
| Miszko et al. (27) |
11 older adults with low physical functioning and reduced muscle power, 72 yrs |
6 multi-joint upper & lower body resistance training at 50%–70% 1RM for first 8 weeks (slow contraction velocities), changed to 40% 1RM for remaining 8 weeks. 3 sets × 6–8 repetitions (concentric phase at maximal velocity) |
3 × wk, 16 wks | Peak anaerobic power (Wingate Test): 8% |
Performance on CS-PFP test and sub domains scores: CS-FFP Total: 15% Balance and coordination: 21%, Endurance:17% |
| Bottaro et al. (10) | 11 healthy males, 67 yrs |
6 multi-joint upper & lower body resistance training at 40%–60% 1RM. 3 sets × 8–10 repetitions (concentric phase at maximal velocity) |
2 × wk, 10 wks | Leg press: 31% Chest press: 37% |
8-Feet up-and-go: 15% 30-sec chair stand (reps): 43% Arm curl test: 50% |
| Orr et al.(28) | 112 healthy, high- functioning males and females, 69 yrs |
5 multi-joint upper & lower body resistance training randomized to 3 intensities: 20% (LOW) 50% (MED), 80% (HIGH) of 1RM. 3 sets × 8 repetitions (concentric phase at maximal velocity) |
2 × wk, 8–12 wks | Leg press, leg extension: LOW: 9%, 14% MED:14%, 18% HIGH: 12%, 14% |
Balance Performance: LOW: 10.8% MED: 2.1% HIGH: 3% |
| Earles et al. (17) | 21 healthy males and females, 77 yrs |
Hip and knee extensor, plantar & hip flexor resistance training performed between 50– 70% 1RM. 3 sets × 10 repetitions at usual, ramped or maximal velocities. An additional 45mins of walking/moderate activity (step- ups, chair rises) was also included |
3 × wk, 12 wks | Leg press: 22% | 6-minute walk distance: 20 meters SPPB score:0.7 unit |
| Interventions without Resistance Training Equipment | |||||
| Bean et al. (3) | 23 males and females with mobility limitations, 71 yrs (SPPB score: 9.7, range: 1–11) |
Weighted stair climbing: subjects ascended & descended a flight of stairs (10 steps) while wearing a weighted vest. 3 sets × 4 flights. Vest weight was adjusted to add progressive resistance throughout intervention |
3 × wk, 12 wks | Leg press: 17% Stair climb power: 12% |
SPPB score: 1.1 units Stair climb time: 11% |
| Bean et al. (4) |
10 females with mild to moderate mobility limitations, 77 yrs (SPPB score: 7.7, range: 4–10) |
Weighted vest training (InVest) with exercises designed specific to mobility tasks including chair stands, toe raises, pelvic raises, step ups, chest press. 3 sets × 10 repetitions. (concentric phase of repetition performed at maximal velocity). Vest weight was adjusted to add progressive resistance throughout intervention |
3 × wk, 12 wks | Leg press: 12–36% | SPPB score: 2.7 units 5-Chair stand time: 44% Gait speed: 0.07 m/sec Unilateral stance time: 50% |
| Bean et al. (8) | 72 males and females with mobility limitations, 75 yrs (SPPB score: 8.8, range: 4–9) |
InVest exercise training | 3 × wk, 16 wks | Leg press: 10% | SPPB score: 1.75 units LLFDI: 2.6 units |
= characteristics of participants randomized to power training intervention arm only; CS-FPP: Continuous Scale Physical Functional Performance; SPPB: Short Physical Performance Battery Test; LLFDI: Late Life Function and Disability Instrument.
Sayers et al. (32)evaluated 16 weeks of high velocity power training in older women with self-reported disability and noted modest improvements in dynamic balanceand stair climbing performance after large improvements in muscle power. However, equivalent improvements in functional performance were observed in the group randomized to traditional resistance training. Similarly, Henwoodet al. (23)also compared high velocity varied resistance training to strength training on functional performance in healthy older adults. They demonstrated similar improvements in muscle power with both training protocols after a 24-week intervention period. These gains were also accompanied by better performance on several functional measures, including stair climb and chair rise time, although the magnitude of these improvements were not different between intervention groups.
Two power training intervention studies have demonstrated that high velocity resistance training is associated with greater improvements in functional performance compared to conventional strength training. Among older adults with low muscle power, 16 weeks of high velocity power training elicited significant improvements in a battery of whole body functional performance tasks(27). These gains were significantly greater than those elicited after a corresponding program of traditional strength training (27). Similarly, Bottaroet al.(10)also reported that 10 weeks of high velocity resistance training significantly improved several functional performance measures after modest improvements in leg muscle power in sedentary older males. An intervention of traditional resistance training had no effect of the functional parameters assessed in this study.
Orr et al. (28) reported improvements in measures of dynamic balance in high functioning older men and women randomized to 8–12 weeks of high velocity resistance training and compared to an inactive control group. Power training performed at low intensity (20% of 1RM) was associated with the greatest improvements in balance performance compared to training performed at 50% and 80% of the 1RM. A 12-week program of high velocity resistance training resulted in a 22% increase in leg power with a corresponding increase of 20 meters in total distance walked during the six-minute walk test and a 0.7 unit increase in SPPB score in healthy older adults (17). These improvements in function were greater than those elicited from a self-paced walking program. A 20 meter improvement in 6 minute walk time and a respective 0.5 and 1.0 unit increase in SPPB score correspond to clinically meaningful and substantial improvements in physical performance measures among older adults (29).
Several studies have evaluated different types of exercise interventions that did not depend on specific resistance training equipment or isokinetic dynamometry but emphasized explosive power. These have included modified weighted stair climbing and weighted vest exercise. Bean et al. (3) compared 12 weeks of a weighted stair climbing program to a walking program in older adults with baseline mobility limitations. They reported that the stair climbing intervention increased leg power by 17% with a corresponding 12% increase in stair climbing power. Significant improvements in stair climb time and SPPB scores were observed, although these gains were not statistically greater compared to those observed following a walking intervention. In older women with mobility limitations, the same investigators also examined the effects of a program of weighted vest exercise performed at a high velocity (InVEST) compared to a program of upper and lower body chair-based exercises performed at slow velocity (4). Lower extremity power and chair rise time increased to a greater extent after InVEST compared to the slow velocity program. InVEST training was also associated with a substantial increases in SPPB score and gait speed (29). More recently, Bean and colleagues (8) compared the effects of a 16 week program of InVEST training versus a progressive resistance training program advocated by the National Institute on Aging among mobility-impaired older adults. InVEST training elicited significantly greater gains in limb muscle power compared to the conventional program. Substantial improvements in SPPB score and self reported function were also induced after InVEST, although these improvements were not significantly greater than the traditional resistance training program. In a secondary analysis of this study, Bean et al. (6) used multivariate regression models to delineate how the changes in leg power were significantly and independently associated with the clinically meaningful differences observed in SPPB and gait speed.
In summary, several carefully conducted randomized trials have demonstrated that high velocity resistance training is more effective for improving muscle power compared to traditional slow velocity training. In general, this type of power training is safe and well tolerated even in mobility-limited older adults and person aged > 80 years. However, the efficacy and feasibility of high velocity power training in older adults with chronic conditions such as osteoarthritis and osteoporosis have yet to be fully determined. There is now clear evidence that short term interventions of high velocity resistance training and other more practical power training modalities using weighted vests can induce substantial improvements in physical functioning and restore mobility in frail older adults. Studies with larger sample sizes are needed to clearly establish whether high velocity power training is more effective for enhancing functional outcomes in older adults. Additional studies are also needed to elucidate the longer term benefits of power training in older adults, specifically for maintaining active life expectancy, preventing falls and maintaining mobility into old age.
Conclusion
Muscle power is a more discriminant predictor of functional performance in older adults than muscle strength. A distinct biological basis for the precipitous decline in muscle power with aging has yet to be determined. However, additional research should attempt to elucidate the interrelationships between impairments in muscle power, the neuromuscular system, muscle contraction velocity, and the onset of mobility limitations with advancing age. Exercise interventions targeted at improving lower extremity muscle power have been well-tolerated, safe and effective, even among frail older adults. Improvements in muscle power are greater with resistance training interventions that emphasize high versus low contraction velocity. In addition, there is emerging evidence that higher velocity lower intensity resistance training, and several types of exercise programs performed at high velocity, can improve physical functioning in older adults to a greater extent than traditional slow velocity resistance training.
Acknowledgments
The authors recognize the contributions of many other researchers that could not be cited due to the reference limitations. This research was supported by the National Institute on Aging grant number AG18844 and based upon work supported by the U.S. Department of Agriculture, under agreement No. 58-1950-7-707. Any opinions, findings, conclusion, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the view of the U.S. Department of Agriculture. This research was also supported by the Boston Claude D. Pepper Older Americans Independence Center (1P30AG031679) and the Boston Rehabilitation Outcomes Center, funded by NIH Infrastructure Grant (1R24HD065688-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors of this manuscript report no conflicts of interest.
References
- 1.Aagaard P, Suetta C, Caserotti P, Magnusson SP, Kjaer M. Role of the nervous system in sarcopenia and muscle atrophy with aging: strength training as a countermeasure. Scand J Med Sci Sports. 2010;20(1):49–64. doi: 10.1111/j.1600-0838.2009.01084.x. [DOI] [PubMed] [Google Scholar]
- 2.Bassey EJ, Fiatarone MA, O'Neill EF, Kelly M, Evans WJ, Lipsitz LA. Leg extensor power and functional performance in very old men and women. Clin Sci (Lond) 1992;82(3):321–327. doi: 10.1042/cs0820321. [DOI] [PubMed] [Google Scholar]
- 3.Bean J, Herman S, Kiely DK, Callahan D, Mizer K, Frontera WR, Fielding RA. Weighted stair climbing in mobility-limited older people: a pilot study. J Am Geriatr Soc. 2002;50(4):663–670. doi: 10.1046/j.1532-5415.2002.50160.x. [DOI] [PubMed] [Google Scholar]
- 4.Bean JF, Herman S, Kiely DK, Frey IC, Leveille SG, Fielding RA, Frontera WR. Increased Velocity Exercise Specific to Task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community-dwelling older women. J Am Geriatr Soc. 2004;52(5):799–804. doi: 10.1111/j.1532-5415.2004.52222.x. [DOI] [PubMed] [Google Scholar]
- 5.Bean JF, Kiely DK, Herman S, Leveille SG, Mizer K, Frontera WR, Fielding RA. The relationship between leg power and physical performance in mobility-limited older people. J Am Geriatr Soc. 2002;50(3):461–467. doi: 10.1046/j.1532-5415.2002.50111.x. [DOI] [PubMed] [Google Scholar]
- 6.Bean JF, Kiely DK, LaRose S, Goldstein R, Frontera WR, Leveille SG. Are changes in leg power responsible for clinically meaningful improvements in mobility in older adults? J Am Geriatr Soc. 2010;58(12):2363–2368. doi: 10.1111/j.1532-5415.2010.03155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bean JF, Kiely DK, LaRose S, Leveille SG. Which impairments are most associated with high mobility performance in older adults? Implications for a rehabilitation prescription. Arch Phys Med Rehabil. 2008;89(12):2278–2284. doi: 10.1016/j.apmr.2008.04.029. [DOI] [PubMed] [Google Scholar]
- 8.Bean JF, Kiely DK, LaRose S, O'Neill E, Goldstein R, Frontera WR. Increased velocity exercise specific to task training versus the National Institute on Aging's strength training program: changes in limb power and mobility. J Gerontol A Biol Sci Med Sci. 2009;64(9):983–991. doi: 10.1093/gerona/glp056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003;58(8):728–733. doi: 10.1093/gerona/58.8.m728. [DOI] [PubMed] [Google Scholar]
- 10.Bottaro M, Machado SN, Nogueira W, Scales R, Veloso J. Effect of high versus low-velocity resistance training on muscular fitness and functional performance in older men. Eur J Appl Physiol. 2007;99(3):257–264. doi: 10.1007/s00421-006-0343-1. [DOI] [PubMed] [Google Scholar]
- 11.Callahan D, Phillips E, Carabello R, Frontera WR, Fielding RA. Assessment of lower extremity muscle power in functionally-limited elders. Aging Clin Exp Res. 2007;19(3):194–199. doi: 10.1007/BF03324689. [DOI] [PubMed] [Google Scholar]
- 12.Caserotti P, Aagaard P, Larsen JB, Puggaard L. Explosive heavy-resistance training in old and very old adults: changes in rapid muscle force, strength and power. Scand J Med Sci Sports. 2008;18(6):773–782. doi: 10.1111/j.1600-0838.2007.00732.x. [DOI] [PubMed] [Google Scholar]
- 13.Clark DJ, Patten C, Reid KF, Carabello RJ, Phillips EM, Fielding RA. Impaired voluntary neuromuscular activation limits muscle power in mobility-limited older adults. J Gerontol A Biol Sci Med Sci. 2010;65(5):495–502. doi: 10.1093/gerona/glq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark DJ, Patten C, Reid KF, Carabello RJ, Phillips EM, Fielding RA. Muscle performance and physical function are associated with voluntary rate of neuromuscular activation in older adults. J Gerontol A Biol Sci Med Sci. 2011;66(1):115–121. doi: 10.1093/gerona/glq153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuoco A, Callahan DM, Sayers S, Frontera WR, Bean J, Fielding RA. Impact of muscle power and force on gait speed in disabled older men and women. J Gerontol A Biol Sci Med Sci. 2004;59(11):1200–1206. doi: 10.1093/gerona/59.11.1200. [DOI] [PubMed] [Google Scholar]
- 16.de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Orr R, Fiatarone Singh MA. Optimal load for increasing muscle power during explosive resistance training in older adults. J Gerontol A Biol Sci Med Sci. 2005;60(5):638–647. doi: 10.1093/gerona/60.5.638. [DOI] [PubMed] [Google Scholar]
- 17.Earles DR, Judge JO, Gunnarsson OT. Velocity training induces power-specific adaptations in highly functioning older adults. Arch Phys Med Rehabil. 2001;82(7):872–878. doi: 10.1053/apmr.2001.23838. [DOI] [PubMed] [Google Scholar]
- 18.Fielding RA, LeBrasseur NK, Cuoco A, Bean J, Mizer K, Fiatarone Singh MA. High-velocity resistance training increases skeletal muscle peak power in older women. J Am Geriatr Soc. 2002;50(4):655–662. doi: 10.1046/j.1532-5415.2002.50159.x. [DOI] [PubMed] [Google Scholar]
- 19.Foldvari M, Clark M, Laviolette LC, Bernstein MA, Kaliton D, Castaneda C, Pu CT, Hausdorff JM, Fielding RA, Singh MA. Association of muscle power with functional status in community-dwelling elderly women. J Gerontol A Biol Sci Med Sci. 2000;55(4):M192–M199. doi: 10.1093/gerona/55.4.m192. [DOI] [PubMed] [Google Scholar]
- 20.Frontera WR, Reid KF, Phillips EM, Krivickas LS, Hughes VA, Roubenoff R, Fielding RA. Muscle fiber size and function in elderly humans: a longitudinal study. J Appl Physiol. 2008;105(2):637–642. doi: 10.1152/japplphysiol.90332.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–1064. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- 22.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 23.Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008;63(1):83–91. doi: 10.1093/gerona/63.1.83. [DOI] [PubMed] [Google Scholar]
- 24.Lexell J. Human aging, muscle mass, and fiber type composition. J Gerontol A Biol Sci Med Sci. 1995;50 doi: 10.1093/gerona/50a.special_issue.11. Spec No:11-6. [DOI] [PubMed] [Google Scholar]
- 25.Marsh AP, Miller ME, Rejeski WJ, Hutton SL, Kritchevsky SB. Lower extremity muscle function after strength or power training in older adults. J Aging Phys Act. 2009;17(4):416–443. doi: 10.1123/japa.17.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mayson DJ, Kiely DK, LaRose SI, Bean JF. Leg strength or velocity of movement: which is more influential on the balance of mobility limited elders? Am J Phys Med Rehabil. 2008;87(12):969–976. doi: 10.1097/PHM.0b013e31818dfee5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miszko TA, Cress ME, Slade JM, Covey CJ, Agrawal SK, Doerr CE. Effect of strength and power training on physical function in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2003;58(2):171–175. doi: 10.1093/gerona/58.2.m171. [DOI] [PubMed] [Google Scholar]
- 28.Orr R, de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Fiatarone-Singh MA. Power training improves balance in healthy older adults. J Gerontol A Biol Sci Med Sci. 2006;61(1):78–85. doi: 10.1093/gerona/61.1.78. [DOI] [PubMed] [Google Scholar]
- 29.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 30.Reid KF, Callahan DM, Carabello RJ, Phillips EM, Frontera WR, Fielding RA. Lower extremity power training in elderly subjects with mobility limitations: a randomized controlled trial. Aging Clin Exp Res. 2008;20(4):337–343. doi: 10.1007/bf03324865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reid KF, Doros G, Clark DJ, Patten C, Carabello RJ, Cloutier GJ, Phillips EM, Krivickas L, Frontera WR, Fielding RA. Muscle power failure in mobility-limited older adults: preserved single fiber function despite lower whole muscle size, quality and neuromuscular activation. Eur Jou Appl Physiol. 2011 doi: 10.1007/s00421-011-2200-0. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sayers SP, Bean J, Cuoco A, LeBrasseur NK, Jette A, Fielding RA. Changes in function and disability after resistance training: does velocity matter?: a pilot study. Am J Phys Med Rehabil. 2003;82(8):605–613. doi: 10.1097/01.PHM.0000078225.71442.B6. [DOI] [PubMed] [Google Scholar]
- 33.Sayers SP, Guralnik JM, Thombs LA, Fielding RA. Effect of leg muscle contraction velocity on functional performance in older men and women. J Am Geriatr Soc. 2005;53(3):467–471. doi: 10.1111/j.1532-5415.2005.53166.x. [DOI] [PubMed] [Google Scholar]
- 34.Suzuki T, Bean JF, Fielding RA. Muscle power of the ankle flexors predicts functional performance in community-dwelling older women. J Am Geriatr Soc. 2001;49(9):1161–1167. doi: 10.1046/j.1532-5415.2001.49232.x. [DOI] [PubMed] [Google Scholar]
- 35.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]