Abstract
African Americans have been consistently shown to have less deep (slow wave sleep; SWS) and more light (Stages 1 and 2) sleep than Caucasian Americans. This paper explored whether discrimination, a stressor that uniquely impacts certain ethnic groups, contributes to differences in sleep architecture. The sleep of 164 African and Caucasian Americans was examined with laboratory based polysomnography (PSG). Experiences of perceived discrimination (The Scale of Ethnic Experience) and sociodemographic factors were also assessed. After adjusting for age, body mass index (BMI), socioeconomic status (SES) and smoking status, African Americans slept approximately 4.5% more total sleep time (TST) in Stage 2 sleep and 4.7% less TST in SWS than Caucasian Americans (ps< .05). Perceived discrimination was a partial mediator of ethnic differences in sleep architecture. Individuals who reported experiencing more discrimination slept more time in Stage 2 and less time in SWS (ps< .05). Results suggest that the impact of stress related to ethnic group membership plays a part in explaining differences in sleep architecture.
Keywords: African American, discrimination, sleep architecture, stress
Sleep is a critical component of physical and psychological functioning and is linked to a range of adult health issues (Ferrie et al. 2007; Gangwisch et al. 2007; Ikehara et al. 2009), learning and memory processes (Diekelmann et al. 2009), mood (Tsuno et al. 2005) as well as neuroendocrine and immune system function (Meerlo et al. 2008; Van Cauter et al. 2008). Understanding factors that promote and detract from optimal sleep is critical when investigating human health outcomes.
Consistent differences in sleep architecture between African and Caucasian Americans have been reported, such that African Americans sleep a smaller proportion of time in deep sleep (slow wave sleep; SWS) and more time in light sleep (Stages 1 and 2) each night (Mezick et al. 2008; Redline et al. 2004; Profant et al. 2002; Thomas et al. 2006; Hall et al. 2009; Ruiter et al. 2011; Beatty et al. 2011). A recent meta-analysis also suggests that African Americans sleep for less total time, take longer to fall asleep and have less efficient sleep than their Caucasian counterparts (Ruiter et al. 2011). Results of the meta-analysis suggest that differences in sleep continuity and duration were moderated by biopsychosocial factors such as adiposity, employment status, mental illness and medication use; however, explanatory variables did not account for racial differences in sleep architecture (Ruiter et al. 2011).
Stress exerts a prominent influence on sleep physiology (Kim and Dimsdale, 2007); while it remains unclear what is driving ethnic differences in sleep architecture, an appealing, but unresolved hypothesis is that sleep differences may be reflective of unique aspects of stress related to ethnicity. One candidate mediator of this association is perceived discrimination, a variable linked to a variety of health outcomes (Williams and Mohammed, 2009; Williams et al. 1997; Pascoe and Smart Richman, 2009). Previous work has demonstrated that perceived discrimination mediated ethnic differences in Stage 4 sleep (Thomas et al. 2006); however, the finding has yet to be replicated in an independent sample.
Objectives
The current study characterized differences in sleep architecture between African and Caucasian Americans. All participants underwent laboratory-based polysomnography (PSG) and provided information about perceived discrimination, socioeconomic status and health practices. The primary objective was to replicate previous findings showing that ethnic discrimination mediates racial differences in sleep architecture in an independent sample of participants. Further, the current study controlled for socioeconomic status, a variable linked to sleep variables but not considered in the previous investigation. Based on previous work, we hypothesized that discrimination would mediate ethnic differences in SWS.
Methods
Subjects were recruited from the local San Diego, California area to participate in a larger study investigating differences in vascular health between African and Caucasian Americans. Recruitment occurred through local papers, online advertisements, community flyers, participation in health fairs and word-of-mouth. Exclusion criteria included: diagnosis of and/or ongoing treatment for any clinical illness other than hypertension (e.g., asthma, diabetes), blood pressure (BP) ≥170/105 mm Hg, current substance abuse, previous diagnosis of a sleep disorder, or a history of psychosis. Participants were also excluded if they were pregnant or were taking any prescription medication (including hormonal contraception or hormone replacement therapy) and subjects were asked to refrain from taking any over the counter medications for 24 hours prior to admission. Three patients being treated for hypertension were accepted into the study after being tapered off their antihypertensive medications by the study physician and maintaining BP < 170/105 mm Hg for 3 weeks. All participants in the study reported working ≥20 hours/week. The project was approved by the Institutional Review Board of the University of California San Diego (UCSD).
Procedure
Once written informed consent was obtained, participants met with a study physician to undergo a physical exam and answer questions about their medical history. If study criteria were met, sleep monitoring was conducted with standard polysomnography (PSG) which occurred over two consecutive nights at the UCSD General Clinical Research Center Gillin Laboratory of Sleep and Chronobiology (GCRC-GLSC). On each night, PSG set-up began at 21:00 hrs and lights off occurred between 22:00 and 24:00 hrs. Each morning, participants were wakened at 06:00 hrs and PSG recording equipment was removed. The first night of monitoring served as an acclimation night and data from the second night of sleep recording are the focus of this study. Psychosocial questionnaires were given to participants upon admission and were collected prior to discharge.
Measures
Sociodemographic Information and Health Practices
Information about gender, racial identity (Caucasian American coded as −1 and African American coded as 1), age, years of education, occupation and health practices were collected via self-report. BMI was calculated from height and weight measurements (to the nearest 0.1 kg and 0.1 cm) taken during the physical exam and was defined as the ratio of body weight in kilograms divided by square height in meters (kg/m2). Participants were classified as smokers if they reported smoking cigarettes daily (No coded as 0 and Yes as 1).
Discrimination
Discrimination was assessed using The Scale of Ethnic Experience (Malcarne et al. 2006), a 32-item, self-report questionnaire developed to measure the cognitive experience of ethnicity across several dimensions. The scale yields a perceived discrimination scale, which assesses the extent to which an individual believes that members of his or her ethnic group have been discriminated against in society. Higher scores are indicative of greater endorsement of perceived discrimination. The questionnaire was developed using a college sample from diverse ethnic backgrounds. Initial studies showed the perceived discrimination scale to have good internal consistency in African American participants (Cronbach’s α= 0.86). In our sample, Cronbach’s α for the perceived discrimination scale was 0.88. Concurrent validity of the questionnaire was established through significant associations in the expected direction with existing group-specific instruments (Malcarne et al. 2006).
Socioeconomic Status
Current SES was assessed with the clinician-rated, Hollingshead 2-Factor Index of Social Position. This scale assesses highest level of formal education attained and current occupation. The two factors are summed, weighted and combined into a continuous measure of social index. Scores range from 11 to 77, with lower social index scores indicating higher SES (Hollingshead. 1957).
Sleep Monitoring
Sleep data acquisition was performed using the Embla A10 polysomnography system (Embla Systems Inc., Broomfield, CO USA). We assessed: Electroencephalography (C4/C3), electrooculography, chin electromyography, leg electromyography, airflow with an oronasal thermal sensor, airflow with an air pressure transducer, snore events with a piezo snore sensor, respiratory effort with piezo thoracic and abdominal belts, oxygen saturation with a pulse oximetersensor, and body position with a position indicator.
Records were hand scored by experienced polysomnographic technicians using the criteria of Rechtschaffen and Kales (1968) and Somnologica software (Embla, Broomfield, CO). Records were scored for TST, sleep onset latency (SOL), sleep efficiency (SE), percentage wake after sleep onset (WASO), percentage of Stage 1, Stage 2, SWS (composed of Stages 3 and 4 sleep) and REM sleep. TST was considered the total time asleep (in minutes) minus any waking time and was the sum of all time spent in Stages 1 and 2, SWS and REM. SOL was defined as the time from lights out to the first epoch of Stage 2 sleep. SE was calculated as (TST × 100/time in bed). The percentages of Stage 1, Stage 2, SWS and REM were calculated as the percentage TST spent in each stage. Percent WASO was defined as (minutes awake after sleep onset/TST).
Statistical Analysis
Data were analyzed using SPSS 17.0 (SPSS Inc., Chicago, IL). Simple mediation analyses were performed using the INDIRECT SPSS macro (version 4) (Preacher and Hayes. 2004). Before conducting analyses, skewed sleep data (Stage 1, SOL, SE and WASO) were log-normalized to approximate a normal distribution.
Ethnic differences on continuous outcome measures were assessed using ANOVA; Chi-Squared tests were used to assess differences on categorical outcome measures. We conducted bivariate correlations to assess associations between variables in the study. ANCOVA analyses were used to assess if ethnic differences in sleep architecture variables remained once covariates that differed across ethnicity (age, BMI, SES and smoking status) were considered.
We next tested whether perceived discrimination mediated ethnic differences in sleep architecture in those variables that (1) were significantly different between ethnicities after covariates were considered and (2) were associated with perceived discrimination. We controlled for known covariates of sleep architecture (age, BMI, SES and smoking status) in all analyses.
Mediation effects were examined using a bootstrapped (5000 times) multivariate test of mediation (Preacher and Hayes, 2004; Preacher and Hayes, 2008). This strategy compares the indirect effects of an independent variable (IV; ethnicity) on a dependent variable (DV; sleep stage) though a mediator (perceived discrimination) while taking covariates into consideration. Using this regression-based mediation strategy, regression coefficients are calculated for the effect of the IV on the mediating variable (path a), the mediating variable on the DV (path b), and the IV on the DV without the inclusion of mediators (path c), and finally, the IV on the DV after the mediator is considered (path c′). The product-of-coefficients (paths a*b) are calculated using a bootstrapping procedure to yield a point estimate for the indirect (mediating) effect.
Bootstrapping is a nonparametric statistical technique that can be used to derive an estimate of a statistic’s sampling distribution (Mooney et al. 1993). Bootstrapping involves randomly sampling subsets of data and calculating a desired statistic. This process is repeated thousands of times yielding a sampling distribution for that statistic. The desired statistic (in this case a point estimate for the indirect effect) and accompanying confidence intervals are then derived from the sampling distribution. The resulting confidence interval of the point estimate provides a test of significance that evaluates whether the theorized mediator statistically accounts for a significant part of IV’s prediction of DV (Preacher and Hayes, 2004; Efron et al. 1993).
Results
Ethnic Differences
Information about demographics and sleep variables is presented in Table 1. The final sample consisted of 164 participants; approximately 44.5% were women, 39.6% self identified as African American. Participants were between the age of 19 and 53 years. The mean years of education completed in the sample was 14.8 (SD = 2.2) years. African American participants were significantly older and had higher BMI’s than Caucasian American participants. African American participants were also more likely to smoke, had higher Hollingshead total scores (reflective of lower SES) and endorsed more perceived discrimination.
Table 1.
Sample Demographics and Characteristics
| Variable | African American (n = 65) | Caucasian American (n = 99) |
|---|---|---|
| Women | 31 (47.7) | 42 (42.4) |
| Smoking* | 13 (20.0) | 7 (7.1) |
| Age ** | 38.2 ± .99 | 33.4 ± 1.10 |
| BMI** | 28.04 ± .51 | 24.67 ± .40 |
| Perceived Discrimination** | 3.49 ± .09 | 2.54 ± .09 |
| Hollingshead ** | 45.0 ± 1.60 | 37.9 ± 1.54 |
| Time in bed (min) | 428.1 ± 5.38 | 426.2 ± 4.78 |
| TST (min) | 385.54 ± 6.12 | 397.93 ± 4.92 |
| Sleep Efficiency* | 90.01 ± .82 | 93.34± .49 |
| Sleep Latency (min)* | 17.01 ± 2.47 | 8.70 ± 9.78 |
| WASO (%)* | 6.93 ± .77 | 5.18 ± .53 |
| Stage 1* | 6.92 ± .63 | 5.02 ± .34 |
| Stage 2** | 54.46 ± 1.09 | 49.29 ± .83 |
| SWS** | 16.10 ± 1.15 | 23.73 ± 1.00 |
| REM | 22.52 ± .77 | 21.96 ± .57 |
Note. Gender and smoking data are n (%). All others are M ± SEM.
Untransformed estimated marginal means and standard errors are presented for the variables sleep latency, Stage 1 sleep and WASO; however p values reflect ANOVAs conducted with transformed variables as the outcome measure.
BMI = body mass index; TST = Total Sleep Time; WASO = wake after sleep onset; REM = rapid eye movement; M = mean; SEM = standard error of the mean.
p < .05,
p < .01
Average time in bed was 427.00 min (SE=3.58) and average TST was 393.02 min (SE=3.85). African American participants evidenced relatively adverse sleep profiles (took longer to fall asleep, had less efficient sleep, spent more time awake after sleep onset, spent more time in Stages 1 and 2 sleep and less time in SWS) compared to Caucasian American participants.
Associations Between Sleep Architecture, Perceived Discrimination and Covariates
Age, BMI, SES, smoking status and discrimination were all associated with relatively adverse sleep. Increasing age and BMI were both associated with less efficient sleep, more time awake after sleep onset, more time slept in Stage 1 and 2 sleep and less time slept in SWS. Participants who smoked had less TST, with increased time slept in Stage 1 and 2 sleep and less time slept in SWS. Lower SES was related to less efficient sleep, more time awake after sleep onset and increased time slept in Stage 1 sleep. Finally, perceived discrimination was associated with increased time slept in Stage 2 sleep and decreased time slept in SWS. Bivariate correlations relating covariates and perceived discrimination to sleep architecture are listed in Table 2.
Table 2.
Correlations Between Demographic Factors, Socioeconomic Status, Perceived Discrimination and Sleep Architecture
| Variable | Sleep Efficiency | WASO | TST | SOL | % REM | % Stage 1 sleep | % Stage 2 sleep | % SWS |
|---|---|---|---|---|---|---|---|---|
| Age | −.33** | .42** | −.07 | .01 | .31** | .40** | .21** | −.51** |
| BMI | −.27** | .25** | −.12 | .05 | .09 | .28** | .16* | −32** |
| Smoking | −.13 | .12 | −.19* | .07 | −.06 | .24** | .22** | −.25** |
| Hollingshead | −.16* | .17* | −.14 | .03 | .02 | .17* | .01 | −.10 |
| Perceived Discrimination | −.14 | .10 | .07 | .13 | .10 | .15 | .27** | −.35** |
BMI = body mass index; WASO = wake after sleep onset; TST = Total sleep time; SOL = Sleep onset latency; REM = rapid eye movement; SWS = slow wave sleep
p < .05,
p < .01
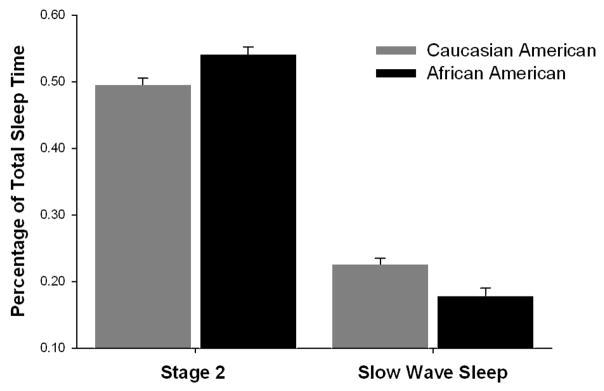
There were significant ethnic differences in age, BMI, SES and smoking status and each of these covariates was also associated with sleep architecture. We therefore conducted a series of ANCOVAs to investigate whether controlling for covariates accounted for ethnic differences in sleep architecture. After controlling for age, BMI, SES and smoking status, ethnicity was no longer significantly associated with SE, F(5,159) = 2.98, p=.09, WASO, F(5,159) = .20, p=.66, or Stage 1 sleep, F(5,159) = 0.66, p=.42. However, ethnic differences persisted in SOL, [F(5,159) = 6.69, p< 0.05, partial η2 = 0.04], Stage 2 sleep [F(5,159) = 8.54, p<.01, partial η2 = 0.05] and SWS [F(5,159) = 9.45, p<.01, partial η2 = 0.06]. After covariates were considered, AA’s spent approximately 4.5% more TST in Stage 2 sleep and 4.7% less TST in SWS than Caucasian Americans. The racial difference in SWS is equivalent to an approximately 20% reduction in SWS in AA’s when compared their Caucasian counterparts. See Figure 1.
Figure 1.
Estimated marginal means (standard error of the mean) of percentage of sleep stage controlling for age, BMI, SES and smoking status in African and Caucasian American participants.
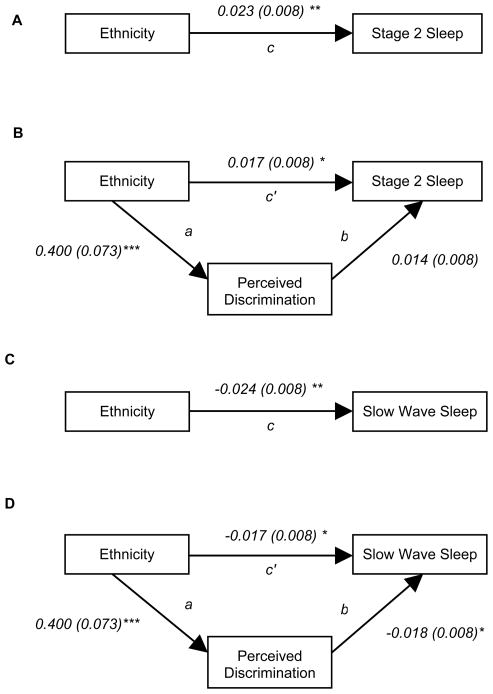
SOL was unrelated to discrimination and was not examined in subsequent analyses. The following paragraphs report the results of the mediation analyses testing whether perceived discrimination mediated the relationship between ethnicity, Stage 2 and SWS. Covariates (age, BMI, SES and smoking status) were controlled for in each step of the subsequent analyses. Regression coefficients were calculated and are reported in the path diagrams in Figure 2. Point estimates for the indirect (mediated) paths and corresponding confidence intervals were obtained using the bootstrapping method and are reported below.
Figure 2.
Perceived discrimination significantly mediated ethnic differences in Stage 2 Sleep and SWS (covariates age, BMI, SES and smoking were controlled for in the model). Path values are unstandardized regression coefficients with SE in parentheses. The point estimates represent the mediated (indirect) effects derived from the bootstrapped product of paths a and b. (A) Ethnicity significantly predicted time slept in Stage 2 sleep. (B) Perceived discrimination was a partial mediator of the effects of ethnicity on Stage 2 sleep (point estimate = 0.0055; BCa = 0.0002 – 0.0131). (C) Ethnicity significantly predicted time slept in SWS. (D). Perceived discrimination was a partial mediator of the effects of ethnicity on SWS (point estimate = −0.0071; BCa = −.0146 – −.0018).
*p < .05, ** p < .01, ***p < .001.
Perceived Discrimination as a Mediator of Ethnic Differences in Stage 2 Sleep
Perceived discrimination was a significant mediator of the relationship between ethnicity and Stage 2 sleep. In other words, the effect of ethnicity was significantly reduced (path c to path c′) after accounting for differences in perceived discrimination (point estimate = 0.0055; BCa = 0.0002 – 0.0131). However, perceived discrimination was only a partial (rather than full) mediator with the direct effect (path c′) remaining significant (t = 2.02, p =.05), indicating that additional variables mediate this relationship.
Perceived Discrimination as a Mediator of Ethnic Differences in SWS
Perceived discrimination was also a significant partial mediator of the relationship between ethnicity and SWS (point estimate = −0.0071; BCa = −.0146 – −.0018), with the direct effect (path c′) remaining significant (t = −2.00, p =.05).
Discussion
This study investigated the relationship between ethnicity, discrimination and multiple dimensions of sleep. Substantial ethnic differences were detected in PSG-assessed sleep architecture. Consistent with previous investigations, after controlling for differences in age, BMI, SES and smoking status, African American participants took longer to fall asleep, slept more time in Stage 2 and less time in SWS than Caucasian participants.
Perceived discrimination emerged as a partial mediator of ethnic differences in Stage 2 and SWS. A previous investigation on a different sample reported similar findings, but did not account for the potential influence of SES on the relationship between discrimination and sleep (Thomas et al. 2006). Our results suggest that perceived discrimination plays a role in the relationship between ethnicity and sleep above and beyond the influence of demographic characteristics.
Given the pervasive influence that sleep has on health, investigating factors, such as discrimination, that detract from optimal sleep is important. Specifically, SWS is associated with suppression of the sympathetic nervous system, lowered blood pressure and decreased heart rate (Van Cauter et al. 2008; Dijk, 2008). SWS suppression studies have demonstrated that short term SWS deprivation is associated with reduced insulin sensitivity and decreased blood pressure dipping (Dijk, 2008; Tasali et al. 2008; Sayk et al. 2010). It is unclear what the effects of chronic, reduced SWS are on health, but one can hypothesize that it may be linked to the development of adverse health profiles and is potentially a mechanism contributing to health disparities between African and Caucasian Americans.
The mechanisms underlying the relationship between discrimination and sleep are not entirely clear. Chronic stress associated with discrimination has been proposed as a mechanism though which discrimination may affect other health outcomes (Pascoe and Smart Richman, 2009; Williams et al. 2008). With regards to sleep, a variety of chronic and experimental stressors have been associated with reductions in SWS (Kim and Dimsdale, 2007). Chronic stress may lead to hypothalamic-pituitary-adrenal (HPA) axis dysfunction and sympathetic nervous system (SNS) hyperactivation, each of which have been shown to influence sleep architecture by decreasing time slept in SWS and increasing time slept in light sleep(Buckley and Schatzberg, 2005). Potentially, chronic stress in the form of perceived discrimination leads to the pattern of shifted sleep architecture (more time slept in light and less time slept in deep sleep) observed in our sample.
The findings from this study should be interpreted in light of potential limitations. Previous work has found that ethnic differences in sleep are more pronounced when sleep is assessed within the hospital setting versus at home (Stepnowsky et al. 2003). Thus, the SWS differences observed in our study may have been artificially exaggerated by the study protocol. The uniqueness of the sample under investigation is another potential limitation of the study. Participants were all healthy, of a restricted age range and residents of Southern California, it is unclear the extent to which these findings would generalize to a wider population. Additionally, the parent study was interested in health outcomes in working individuals, therefore participants in our sample all reported working greater than or equal to 20 hours per week. This limited the range of SES available in the sample and, as has been suggested in previous investigations of SES and sleep, it may have curtailed the detection of potential relationships (Hall et al. 2009). Further, we assessed SES using the Hollingshead 2-Factor Index of Social Position, which does not assess aspects of SES such as income, wealth, perceived social status, or adequacy of income, variables which may be significantly associated with sleep (Braveman et al. 2005). Finally, the study did not control for mental illness with the exception of excluding subjects with a history of psychosis or who were in ongoing treatment.
Despite limitations, our findings suggest that discrimination plays an important role in the relationship between ethnicity and sleep. Using polysomnographic measures of sleep architecture, we found that individuals who reported more perceived discrimination slept more time in Stage 2 and less time in SWS. Further, perceived discrimination served as a partial mediator of the ethnicity and sleep relationships even after covariates were considered.
In the future, other potential moderators and/or mediators of the discrimination and sleep association should be explored. For example, meta-analysis of the literature has shown that perceived discrimination is longitudinally predictive of negative mental health consequences (Pascoe and Smart Richman, 2009; Pavalko et al. 2003; Brown et al. 2000). In turn, poor mental health in the form of anxiety, depression and worry has been associated with worse sleep(Beatty et al. 2011; Kecklund and Åkerstedt, 2004; Hall et al. 2000; Åkerstedt et al. 2007). Considering the potential impact of ethnic disparities in mental illness on sleep architecture is an important next step in the literature (Ruiter et al. 2011). Investigation of the role of coping styles is an additional avenue for future work. The impact of discrimination on blood pressure has been dependent on coping style in several investigations (James et al. 1984; Krieger, 1990; Krieger and Sidney, 1996). Potentially, certain active coping strategies may be more advantageous in buffering the negative consequences of discrimination on sleep outcomes. In sum, future work should continue to unpack the race-sleep quality relationship, by examining especially those mediators that may be amenable to change.
Highlights.
There are ethnic differences in sleep architecture.
African Americans sleep more time in light and less deep sleep than Caucasian Americans.
Perceived discrimination was a partial mediator of ethnic differences in sleep architecture.
Increased discrimination was associated with more time in light and less time in deep sleep.
Acknowledgments
This work was supported by NIH grantsHL36005, HL44915 (J.E.D.), RR 00827 (University of California San Diego General Clinical Research Center Grant) and P60 MD00220 (San Diego EXPORT Center Grant).
Abbreviations
- SWS
slow wave sleep
- PSG
polysmnography
- BMI
body mass index
- SES
socioeconomic status
- TST
total sleep time
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Åkerstedt T, Kecklund G, Axelsson J. Impaired sleep after bedtime stress and worries. Biological Psychology. 2007;76:170–173. doi: 10.1016/j.biopsycho.2007.07.010. [DOI] [PubMed] [Google Scholar]
- Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, Mezick EJ, Strollo PJ, Matthews KA. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology. 2011;30:351–359. doi: 10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Brown TN, Williams DR, Jackson JS, Neighbors HW, Torres M, Sellers SL, Brown KT. “Being black and feeling blue”: the mental health consequences of racial discrimination. Race and Society. 2000;2:117–131. [Google Scholar]
- Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. Journal of Clinical Endocrinology & Metabolism. 2005;90:3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- Diekelmann S, Wilhelm I, Born J. The whats and whens of sleep-dependent memory consolidation. Sleep Medicine Reviews. 2009;13:309–321. doi: 10.1016/j.smrv.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Dijk DJ. Slow-wave sleep, diabetes, and the sympathetic nervous system. Proceedings of the National Academy of Sciences. 2008;105:1107–1108. doi: 10.1073/pnas.0711635105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ. An introduction to the bootstrap. CRC Press LLC; Boca Raton, FL: 1993. [Google Scholar]
- Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, Marmot MG. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–1666. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, Rundle AG, Zammit GK, Malaspina D. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30:1667–1673. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall M, Buysse DJ, Nowell PD, Nofzinger EA, Houck P, Reynolds CF, Kupfer DJ. Symptoms of stress and depression as correlates of sleep in primary insomnia. Psychosomatic Medicine. 2000;62:227–230. doi: 10.1097/00006842-200003000-00014. [DOI] [PubMed] [Google Scholar]
- Hall MH, Matthews KA, Kravitz HM, Gold EB, Buysse DJ, Bromberger JT, Owens JF, Sowers M. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Two Factor Index of Social Position. Yale University Press; New Haven, CT: 1957. [Google Scholar]
- Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A JACC Study Group. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:295–301. doi: 10.1093/sleep/32.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SA, LaCroix AZ, Kleinbaum DG, Strogatz DS. John Henryism and blood pressure differences among black men. II. The role of occupational stressors. Journal of Behavioral Medicine. 1984;7:259–275. doi: 10.1007/BF00845359. [DOI] [PubMed] [Google Scholar]
- Kecklund G, Åkerstedt T. Apprehension of the subsequent working day is associated with a low amount of slow wave sleep. Biological Psychology. 2004;66:169–176. doi: 10.1016/j.biopsycho.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Kim EJ, Dimsdale JE. The Effect of Psychosocial Stress on Sleep: A Review of Polysomnographic Evidence. Behavioral Sleep Medicine. 2007;5:256–278. doi: 10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Social Science and Medicine. 1990;30:1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. American Journal of Public Health. 1996;86:1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malcarne VL, Chavira DA, Fernandez S, Liu PJ. The scale of ethnic experience: development and psychometric properties. Journal of Personality Assessment. 2006;86:150– 161. doi: 10.1207/s15327752jpa8602_04. [DOI] [PubMed] [Google Scholar]
- Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews. 2008;12:197–210. doi: 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Mezick EJ, Matthews KA, Hall M, Strollo PJ, Jr, Buysse DJ, Kamarck TW, Owens JF, Reis SE. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosomatic Medicine. 2008;70:410–416. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney CZ, Duval RD, Duval R. Bootstrapping: a nonparametric approach to statistical inference. Sage Publications, Inc; Newbury Park, CA: 1993. [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavalko EK, Mossakowski KN, Hamilton VJ. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women’s physical and emotional health. Journal of Health and Social Behavior. 2003;44:18–33. [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Profant J, Ancoli-Israel S, Dimsdale JE. Are there ethnic differences in sleep architecture? American Journal of Human Biology. 2002;14:321–326. doi: 10.1002/ajhb.10032. [DOI] [PubMed] [Google Scholar]
- Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring for sleep stages of human subjects. Bethesda, Washington: DCUS Government Printing Office; 1968. [Google Scholar]
- Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Archives of Internal Medicine. 2004;164:406–418. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: A meta-analysis. Sleep Medicine. 2011;12:209–214. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- Sayk F, Teckentrup C, Becker C, Heutling D, Wellhoner P, Lehnert H, Dodt C. Effects of selective slow-wave sleep deprivation on nocturnal blood pressure dipping and daytime blood pressure regulation. American Journal of Physiology. 2010;298:191–197. doi: 10.1152/ajpregu.00368.2009. [DOI] [PubMed] [Google Scholar]
- Stepnowsky CJ, Jr, Moore PJ, Dimsdale JE. Effect of ethnicity on sleep: complexities for epidemiologic research. Sleep. 2003;26:329–332. doi: 10.1093/sleep/26.3.329. [DOI] [PubMed] [Google Scholar]
- Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proceedings of the National Academy of Sciences. 2008;105:1044–1049. doi: 10.1073/pnas.0706446105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health psychology. 2006;25:635–642. doi: 10.1037/0278-6133.25.5.635. [DOI] [PubMed] [Google Scholar]
- Tsuno N, Besset A, Ritchie K. Sleep and depression. Journal of Clinical Psychiatry. 2005;66:1254–1269. doi: 10.4088/jcp.v66n1008. [DOI] [PubMed] [Google Scholar]
- Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Medicine. 2008;9:23–28. doi: 10.1016/S1389-9457(08)70013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2008;98:S29–S37. doi: 10.2105/ajph.98.supplement_1.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2:335. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]