Abstract
Objective
This study analyzed the symptom frequencies of 17-item Hamilton Depression Rating Scale (HDRS-17) to understand the characteristics of each item and to propose the possible symptoms clusters.
Methods
From psychiatric clinics of 18 Hospitals in Korea, 1,183 patients, diagnosed with major depressive disorder (psychotic or non-psychotic), dysthymia or depressive disorder not otherwise specified. according to DSM-IV criteria, participated in this study from January 2006 to August 2008. The frequencies of each item of HDRS-17 were analyzed according to sex and severity. In addition, we compared this study with a previous study performed in England by Hamilton and with two studies performed in Korea by Kim et al.
Results
The frequencies of HDRS-17 items varied widely in this study, ranging from 95.8% in work and activities to 37.4% in loss of weight. But, depressed mood, psychic anxiety and work and activities items exhibited constant and higher frequency or rank regardless of study, the severity of depression or sex. Insomnia early, somatic gastrointestinal, genital symptoms and insight showed relatively constant but lower frequency or rank in disregard of studies or the clinical variables. Other symptoms had variable frequencies or ranks according to the variable clinical situations (culture, time, sex, severity of depression).
Conclusion
We propose three clusters of symptoms in depressive disorders: core symptoms cluster, an associated symptoms, and a situation-specific symptoms. We can use these possible symptom clusters of depression in simplifying diagnosis of depression, increasing diagnostic specificity in special situation and indexing disease severity.
Keywords: Symptom frequency, Variation, HDRS-17, Core symptoms cluster, Associate symptoms cluster, Situation-specific symptoms cluster
INTRODUCTION
The typical symptoms of depressive disorder consist of depressed mood, loss of interest or pleasure, changes in appetite and weight, changes in sleep and activity, lack of energy, feelings of guilt, problems thinking and making decisions, and recurrent thoughts of death or suicide.1 Of these symptoms, depressed mood, feelings of guilt and suicidal ideation are known as the depressive triad2 and can be easily recognized in depression, whereas other symptoms are sometimes mistakenly considered as symptoms of medical illnesses other than depression. This makes depressive disorder difficult to diagnose by non-professional or non-psychiatry medical professional.3
In reality, depressive patients do not exhibit precisely typical depressive symptoms such as depressive mood, feelings of guilt, and suicidal ideation.3 Rather, demographic characteristics, such as sociocultural background, sex, age, education level, financial situation, and clinical variables (e.g., symptom severity) may influence the presentation of depressive emotion.4-21
Considering these characteristics of the psychopathology of the depression, the diagnostic criteria and instruments used for depression require adjustment to each patient's clinical situation or variables. However, the diagnostic criteria and scales currently used appear to neglect these aspects as they only list the symptoms or items of the scale and consider them without adjustment or weighting according to significance in the whole context of a depressive disorder or according to specific situations.
General symptoms of depression that are not influenced by clinical or cultural variables, those symptoms can be used as universal criteria. Symptoms of depression that are sensitive to specific clinical variables and well-defined specific situations can be used as specifying criteria. For example, Kiev divided depressive symptoms into primary symptoms, which are not influenced by cultural situations and include terminal insomnia, depressed mood, diurnal variation of mood, and loss of interests, and secondary symptoms, which are easily influenced by cultural situations and comprise retardation, feelings of guilt, and suicidal ideation.22
It is impossible to consider all the clinical situations and demographic characteristics of patients when diagnosing depression. However, several clinical and demographic variables, such as culture or race, sex, and severity of depression, are frequently considered. In addition, they provide information that can be useful for evaluating the symptoms that are more influenced by such clinical or demographic variables.
This study analyzed the frequency of symptoms on the 17-item Hamilton Depression Rating Scale (HDRS-17),2 Korean version (K-HDRS),23 using multicenter Korean cohorts collected nationwide, and compared the findings with a previous study from England3 and two studies from Korea,24,25 to understand the characteristic frequency variations in the frequency of each item according to cultural parameters, sex, severity of depression, and chronological aspects, and to identify the possible symptom clusters. We hypothesized that although the frequency of symptoms varies, there may be characteristic patterns in this variation. Furthermore, the 17 items of the HDRS can be divided into three groups according to patterns in the symptom frequency. The first group includes core (general) symptoms with a constant and higher frequency; the second comprises associated symptoms with a constant but lower frequency; the third includes situation-specific symptoms with a variable frequency that is associated with a well-defined specific clinical situation.
METHODS
This study used the cross-sectional baseline data from the Clinical Research Center for Depression Study (CRESCEND study; homepage: www.smileagain.or.kr), which was supported by the Ministry of Health and Welfare of Korea. The CRESCEND study was a naturalistic, observational, multicenter, nationwide, and prospective cohort study. The participants were in-and outpatients that visited the psychiatric departments of 16 university hospitals and two general hospitals, distributed throughout South Korea from January 2006 to August 2008.
The inclusion criteria used were:
Age over 7 years.
Diagnosis of Major Depressive Disorder (MDD), dysthymia or depressive disorder Not Otherwise Specified. using DSM-IV-based structured clinical interview26 and presence of first instance of the disease or relapsed disease.
Provision of signed informed consent by patients, based on an explanation of this study.
The exclusion criteria used were:
Diagnosis of schizophrenia, organic mental disorder, or seizure disorder.
Diagnosis of eating disorder, brief psychotic disorder, or schizoaffective disorder.
Presence of clinically significant nephrological, hepatological, cardiovascular, respiratory, cerebrovascular, or endocrinological disease and difficulty in maintaining psychiatric evaluation and treatment. The consent form and research protocol were approved by the individual university and/or hospital institutional review boards. All participants reviewed the consent form and gave written informed consent to participate the study, in the presence of research staff.
Demographic data were collected and neurological and laboratory tests were performed at baseline. Patients that had organic or physical problems were excluded from the study. The HDRS-17, the Clinical Global Impression Scale-Severity (CGI-S),27 and the Social and Occupational Functioning Assessment Scale (SOFAS)28 were administered to evaluate the state of depression. The 17-item version of the HDRS, which was used in this study, was recently translated into a K-HDRS,23 the reliability and validity of which have been confirmed. The DSM-IV-based structured clinical interview and the rateradministered assessment were conducted by the same rater. The raters of each individual hospital were trained twice a year via formal consensus meeting for the use of rater-administered assessment instruments. The consensus meeting consisted of observing an experienced supervisory psychiatrist administer the evaluations and an actual administration via videotapes featuring standard MDD patients with or without psychotic features.
Statistical analyses were performed using the SPSS software (version 12.0K). The χ2-test was used to examine the differences in HDRS-17 symptom frequency between groups. All results were considered to be significant at the 5% level.
RESULTS
Demographic characteristics of subjects
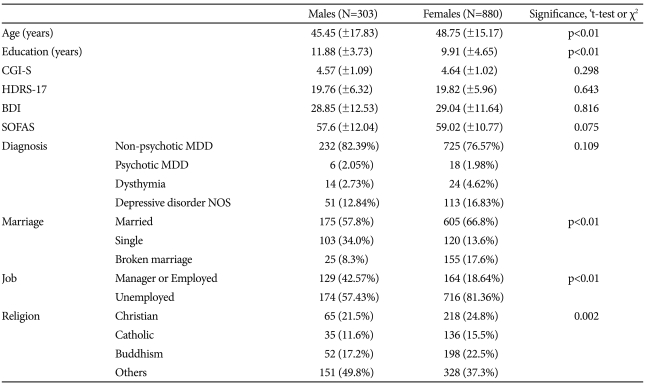
Table 1 presents the demographic characteristics of subjects. The total number of patients enrolled was 1,183 (males, 303; females, 880). Forty-three patients (3.0%) were younger than 18 years of age. The age of the youngest patient was 11 years old. The mean age was 45.5 years for males and 48.8 years for females. The mean duration of education was 11.9 years for males and 9.9 years for females. The mean CGI-S score was 4.57 for males and 4.64 for females. The mean HDRS-17 total score was 19.76 for males and 19.82 for females. The severity of depression in both male and female patients met the diagnostic requirements of MDD.
Table 1.
Demographic characteristics of subjects
CGI-S: Clinical Global Impression scale-Severity, HDRS-17: 17-item Hamilton Depression Rating Scale, BDI: Beck Depression Inventory, SOFAS: Social and Occupational Functioning Assessment Scale, MDD: major depressive disorder, NOS: Not Otherwise Specified. Broken marriage: include widowed, separated, divorced
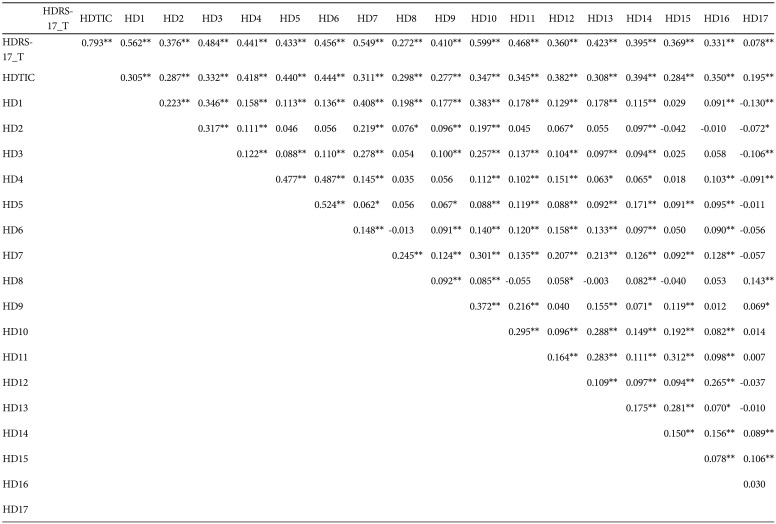
Correlation between HDRS-17 totals score and the presence/absence (yes/no) of each item
Table 2 shows the correlation between the HDRS-17 total score and the dichotomous (yes/no) criterion of each item. The presence of each item and the total count of existing items were both significantly correlated with the HDRS-17 total score. Thus, the dichotomous (yes/no) criterion of each item, which had a score of 1 as the cutoff point can explain the clinical state of patients, to a certain degree and with some limitations. Almost all items were positively correlated with each other. However, item 17 (insight) was negatively correlated with item 1 (depressed mood), item 2 (feelings of guilt), item 3 (suicide) and item 4 (insomnia early). This suggests that these four items may provide patients with insight into the presence of depression.
Table 2.
Correlation between the HDRS-17 total score and total count of present items and the presence/absence (yes/no) of each item
*p<0.05, **p<0.001 by pearson correlation test. HDRS-17_T: 17-item Hamilton Depression Rating Scale total score, HDITC: Hamilton Depression Rating Scale Total Item Count Existing, 1. Depressed mood, 2. Feelings of guilt, 3. Suicide, 4. Insomnia early, 5. Insomnia middle, 6. Insomnia late, 7. Work and activities, 8. Retardation, 9. Agitation, 10. Psychic anxiety, 11. Somatic anxiety, 12. Somatic gastrointestinal, 13. Somatic general, 14. Genital symptoms, 15. Hypochondriasis, 16. Loss of weight, 17. Insight
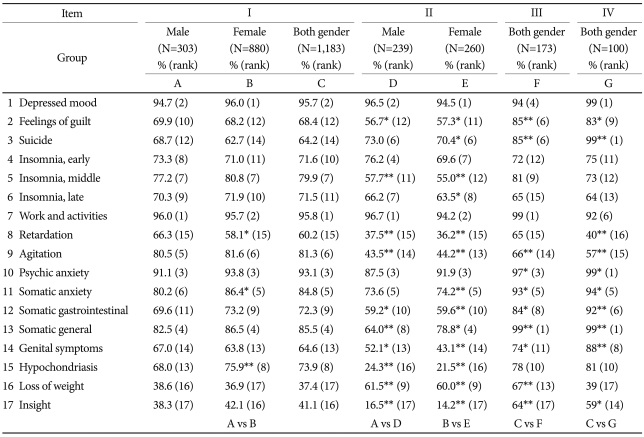
Frequency and rank of HDRS-17 items according to sex
Table 3 presents the frequency and rank of HDRS-17 items. The frequency of HDRS-17 items was more than 90% for three items (7, 1, and 10), 80-89% for three items (13, 11, and 9), in 70-79% for five items (5, 15, 12, 4, and 6), 60-69% for four items (2, 14, 3, and 8), and less than 50% for two items (16 and 17). The five most frequent symptoms, in descending order, were item 7 (work and activities), item 1 (depressed mood), item 10 (psychic anxiety), item 13 (somatic general), and item 9 (agitation) in males; and item 1 (depressed mood), item 7 (work and activities), item 10 (psychic anxiety), and item 13 (somatic general) in females. The five least common symptoms in ascending order were item 17 (insight), item 16 (loss of weight), item 8 (retardation), item 14 (genital symptoms), and item 15 (hypochondriasis) in males; and item 16 (loss of weight), item 17 (sight), item 8 (retardation), item 3 (suicide), and item 14 (genital symptoms) in females. There were significant differences in the frequency of three items (8, 11, and 15) between males and females. The frequency of psychomotor retardation was significantly higher in males than in females (66.3% vs. 58.1%), whereas somatic anxiety (86.4% vs. 80.2%) and hypochondriasis (75.9% vs. 68.0%) were significantly more frequent in females than in males. The comparison of rank of items between sexes revealed an absence of more than two rank differences for all but two items (4 and 15); the rank of insomnia early was three ranks higher in males and the rank of hypochondriasis was three ranks higher in females.
Table 3.
Comparison of symptom frequency (at least mild degree) between this study and the previous studies
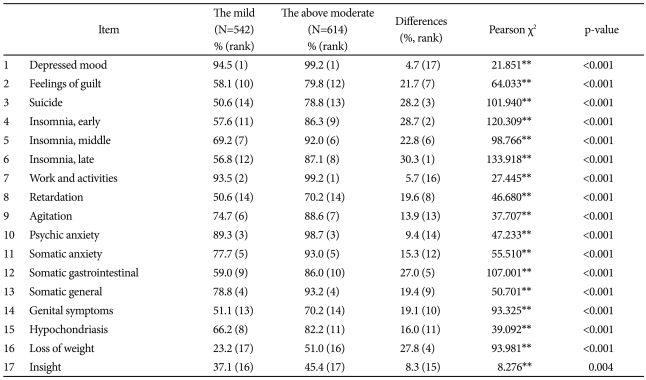
Comparison of symptom frequency according to symptom severity
To evaluate the relationship between the severity of depressive symptoms and the frequency of depressive symptoms, the sample was divided into two groups: the below moderate depression group (7< HDRS-17 score <20) and the above moderate depression group (HDRS-17 score ≥20). There were significant differences in symptom frequency between the two groups regarding all items of the HDRS-17 (Table 4). Percentage differences of symptom frequency were also observed between the below moderate group and the above moderate group: these differences were <10% for four items (1, 7, 10, and 17), 10-20% for six items (8, 9, 11, 13, 14, and 15), and >20% for seven items (2, 3, 4, 5, 6, 12, and 16). The rank of items was almost similar between the two groups with the exception of item 6 (insomnia late: 12th vs. 8th) and item 15 (hypochondriasis: 8th vs. 11th). Although insomnia late and hypochondriasis were both more frequent in the above moderate group, insomnia late was ranked higher in the above moderate group whereas hypochondriasis was ranked higher in the below moderate group. Synthetically, only insomnia late showed a wide variance in terms of both frequency and rank.
Table 4.
Comparison of symptom frequency (at least mild) between the above moderate severity depression group (HDRS-17≥20) and the mild depression groups (7<HDRS-17<20)
*p<0.05, **p<0.001 by χ2 test. HDRS: Hamilton Depression Rating Scale
DISCUSSION
The HDRS has been used as a standard for measuring depression for almost 50 years. However it is not a diagnostic instrument for depressive disorders. Current categorical classification of depressive disorders is based on criteria set of defining symptoms. Therefore, it is important to identify the characteristic manifestations of these symptoms.
This study evaluated the current HDRS characteristics of depressive disorders in Korea. We compared this study with a previous study performed in England by Hamilton3 and with two studies performed in Korea by Kim et al.24,25 (Table 3). In comparison with the Hamilton's study,3 we found that three items i.e., item 1 (depressed mood), item 7 (work and activities), and item 10 (psychic anxiety) were the most frequent symptoms in both studies. However, item 5 (insomnia middle), item 9 (agitation), item 15 (hypochondriasis), and item 16 (loss of weight) exhibited significant variance in the two studies, in terms of both frequency and rank. The comparison of symptom frequency between this study and the two studies performed by Kim revealed that three items (1, 7, and 10) had a frequency of >90% in all three studies. In contrast, item 2 (feelings of guilt), item 3 (suicide), item 9 (agitation) and item 13 (somatic general) showed significant variance between this study and the previous studies in terms of frequency and rank.
The results of this study and their comparison with the results of the Hamilton and Kim studies can be summarized as follows: 1) the presence of wide variance in the frequency of symptoms was observed in this study as well as in the previous studies; 2) a constant frequency or rank for some symptoms was observed regardless of study, sex or the severity of depression; and 3) variance in the frequency or rank of some symptoms was observed regardless of study, sex or the severity of depression.
The frequency of HDRS-17 items varied widely in this study, ranging from 95.8% for work and activities to 37.4% for loss of weight. Variance in symptom frequency was noticed both in Hamilton's study and Kim's two studies.
However, despite such variance in symptom frequency within groups, some symptoms showed constant frequency or rank regardless of study, the severity of depression or sex. Depressed mood, psychic anxiety and work and activities are among these symptoms, which also exhibited the highest frequency among the 17 items. Insomnia early, somatic gastrointestinal, genital symptoms and insight can be included in the group with constant but low frequency or rank.
Some items had variable frequency according to culture, times, severity of depression, or sex. Regarding cultural aspects, insomnia middle, agitation, hypochodriasis and loss of weight showed relatively wide variance. Regarding times, feelings of guilt, suicide, agitation, and somatic general showed wide variance. Regarding sex, retardation, somatic anxiety and hypochondriasis showed wide variance in this study. Regarding severity of depression, insomnia late seemed to have a wide frequency variance.
Based on these observations, the authors propose three clusters of symptoms in depressive disorders: core symptoms cluster, an associated symptoms cluster and a situation-specific symptoms cluster. The core symptoms cluster is present in most depressive disorders constantly and frequently and is not greatly affected by times, place, culture, sex or severity. The associated symptoms cluster is present constantly but less frequently and is not affected by clinical variance. In contrast, situation-specific symptoms cluster has variable frequency and is greatly affected by clinical situation. Depressed mood, work and activities, and psychic anxiety seem to belong to the core symptoms cluster; insomnia early, somatic gastrointestinal, genital symptoms and insight seem to be part of the associated symptom cluster; and insomnia middle, agitation, hypochodriasis and loss of weight can be classified into culture-specific symptoms cluster. Hypochondriasis, retardation and somatic anxiety can be grouped as sex-specific symptoms cluster. Feelings of guilt, suicide, agitation and somatic general can be classified as a time (or civilization)-specific symptoms cluster. Finally, insomnia late seems to be a severity-specific symptoms cluster.
We suggest that depressed mood, work and activities and psychic anxiety form a core symptoms cluster. This can be contrasted with two fundamental (or core) symptoms of the DSM-IV-TR diagnostic criteria for depressive episode. Depressed mood is commonly defined as a core symptom both in DSM-IV-TR and in this study. Here, the work and activities symptoms were regarded as corresponding to markedly diminished interest or pleasure in DSM-IV-TR. The only difference between this study and DSM-I-TR was psychic anxiety. The item of agitation in DSM-IV-TR diagnostic criteria for depressive episode can be seen as equivalent to psychic anxiety in this study. However, this symptom is handled only as an associated symptom and is just a part of compound psychomotor disturbance criterion of DSM-IV-TR diagnostic criteria for depressive episode. Depression has variable characteristic features; The anxiety component may be among these. In this respect, DSM-IV-TR categorical diagnostic criteria have been criticized for their apparent limitation in terms of reflecting the true clinical symptomatic nature of depression such as psychic anxiety component revealed in this study.29
The six most frequent symptoms in this study, work and activities, depressed mood, psychic anxiety, somatic general, somatic anxiety, and agitation are included in the core defining symptoms of major depressive disorder as well as and anxiety disorders in DSM-IV-TR. This seems to reflect the high prevalence of comorbidity between depressive disorders and anxiety disorders. The National Comorbidity Study in USA revealed that the lifetime prevalence of two or more psychiatric disorders was 21%, and that 61.8% of cases major depressive disorder had a previous history of other psychiatric diagnosis whereas 58% had a history of anxiety disorder.30
This study has some limitations. First, only cases with depression severity above the mild degree were considered in the calculation of the symptom frequency. This can distort the significance of symptoms in depression. Second, the Hamilton study was not contemporary to this study. Therefore, it was difficult to compare cultural differences between the studies. Third, the influence of diverse demographic characteristics on the expression of the symptomatology of depression was not addressed sufficiently.
Despite these limitations, this study is the first nationwide, multicenter, clinical population study of depression symptomatology in Korea. The results of this study led to the recognition of the importance of symptom frequency in the diagnosis of depression and the influence of sex, cultural parameters, times and symptom severity on the diagnosis of depression. In clinical practice, we can simplify the diagnosis of depression using only the core symptoms cluster without using all nine diagnostic categories of DSM-IV-TR. We can use symptoms classified as belonging to situation-specific symptoms cluster to increase the diagnostic specificity according to sex, culture and times (or degree of civilization). In addition, severity-specific symptoms, such as insomnia late can be used as an index of severe depression. Finally, future development or revision of depression rating scales should be channeled to give greater significance to symptoms that are more frequent such as depressed mood, work and activities, and psychic anxiety and to consider the situation-specific symptoms in specific settings.
Conclusions
This study evaluated the HDRS characteristics of depressive disorders in Korea. These results were then compared with those of previous studies performed by Hamilton in England3 and by Kim et al.24,25 in Korea. The frequency of HDRS-17 items varied widely in this study, ranging from 95.8% for work and activities. to 37.4% for loss of weight items. However, depressed mood, psychic anxiety and work and activities items exhibited constant and higher frequency or rank regardless of study, the severity of depression, or sex. Insomnia early, somatic gastrointestinal, genital symptoms and insight items displayed constant but lower frequency or rank regardless of the clinical variables. Moreover, we found that some situation-specific symptoms exhibited variable frequency or rank according to the variable clinical situations. We can use these possible symptom clusters of depression to simplify the diagnosis of depression, to increase diagnostic specificity in special situations and to index disease severity.
Acknowledgments
This research was supported by a grant of the Korea Health 21 R&D, Ministry of Health and Welfare, Republic of Korea (A050047). The Ministry of Health and Welfare had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
References
- 1.Sadock BJ, Kaplan HI, Sadock VA. Mood Disorder. In: Sadock BJ, Sadock VA, editors. Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 10th Edition. Philadelphia: Wolter Kluwer/Lippincott Williams & Wilkins; 2007. pp. 527–528. [Google Scholar]
- 2.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton M. Frequency of symptoms in melancholia (depressive illness) Br J Psychiatry. 1989;154:201–206. doi: 10.1192/bjp.154.2.201. [DOI] [PubMed] [Google Scholar]
- 4.Kraepelin E. New York: Arno Press; 1976. Manic-Depressive Insanity and Paranoia. [Google Scholar]
- 5.Carothers JC. The African Mind in Health and Disease; A Study in Ethnopsychiatry. Geneva: World Health Organization; 1953. [Google Scholar]
- 6.Venkoba Rao A. Depression: a psychiatric analysis of thirty cases. Indian J Psychiatry. 1966;8:143–154. [Google Scholar]
- 7.Kim KI, Li DG, Kim DH. Transcultural study of depressive symptom: a comparison among Chinese, Korean-Chinese in Yanbien and Korean in Seoul. J Korean Neuropsychiatr Assoc. 1995;34:1039–1049. [Google Scholar]
- 8.Kim KI. Clinical study of primary depressive symptom. Part III: a cross cultural comparison. J Korean Neuropsychiatr Assoc. 1977;16:53–60. [Google Scholar]
- 9.Gavin AR, Walton E, Chae DH, Alegria M, Jackson JS, Takeuchi D. The associations between socio-economic status and major depressive disorder among Blacks, Latinos, Asians and non-Hispanic Whites: findings from the Collaborative Psychiatric Epidemiology Studies. Psychol Med. 2010;40:51–61. doi: 10.1017/S0033291709006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang SM, Hahm BJ, Lee JY, Shin MS, Jeon HJ, Hong JP, et al. Cross-national difference in the prevalence of depression caused by the diagnostic threshold. J Affect Disord. 2008;106:159–167. doi: 10.1016/j.jad.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 11.Min SK, Suh SY, Song KJ. Symptoms to use for diagnostic criteria of hwa-byung, an anger syndrome. Psychiatry Investig. 2009;6:7–12. doi: 10.4306/pi.2009.6.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim JY, Choi SM, Seo GH, Cho SJ, Kim JG, Cho MJ. Cultural difference in expressing depressive symptoms in Koreans. Korean J Psychopathol. 2000;9:78–87. [Google Scholar]
- 13.Chang SM, Sohn JH, Lee JY, Choi JH, Cho SJ, Jeon HJ, et al. Characteristics of diagnostic criteria for depression in Korea. J Korean Neuropsychiatr Assoc. 2007;46:447–452. [Google Scholar]
- 14.Jang SN, Kawachi I, Chang J, Boo K, Shin HG, Lee H, et al. Marital status, gender and depression: analysis of the baseline survey of the Korean Longitudinal Study of Ageing (KLoSA) Soc Sci Med. 2009;69:1608–1615. doi: 10.1016/j.socscimed.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Sugihara Y, Sugisawa H, Shibata H, Harada K. Productive roles, gender, and depressive symptoms: evidence from a national longitudinal study of late-middle-aged Japanese. J Gerontol B Psychol Sci Soc Sci. 2008;63:P227–P234. doi: 10.1093/geronb/63.4.p227. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell AJ, Subramaniam H. Prognosis of depression in old age compared to middle age: a systematic review of comparative studies. Am J Psychiatry. 2005;162:1588–1601. doi: 10.1176/appi.ajp.162.9.1588. [DOI] [PubMed] [Google Scholar]
- 17.Hybels CF, Blazer DG, Pieper CF, Landerman LR, Steffens DC. Profiles of depressive symptoms in older adults diagnosed with major depression: latent cluster analysis. Am J Geriatr Psychiatry. 2009;17:387–396. doi: 10.1097/JGP.0b013e31819431ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong SW, Lee DS, Jae YM, Jang SH, Choi JH, Jang YK, et al. Comparison of depression symptoms of major depressive disorder between elderly and non-elderly group in Busan city in South Korea. J Korean Soc Biol Ther Psychiatry. 2008;14:58–64. [Google Scholar]
- 19.Kim BS, Jang HS, Lee JY, Suh GH, Hong JP, Hahm BJ, et al. Clinical manifestation of depression symptoms in Korean elderly. J Korean Geriatr Psychiatry. 2003;7:163–177. [Google Scholar]
- 20.Jang SN, Cho SI, Chang J, Boo K, Shin HG, Lee H, et al. Employment status and depressive symptoms in Koreans: results from a baseline survey of the Korean Longitudinal Study of Aging. J Gerontol B Psychol Sci Soc Sci. 2009;64:677–683. doi: 10.1093/geronb/gbp014. [DOI] [PubMed] [Google Scholar]
- 21.Gaudiano BA, Young D, Chelminski I, Zimmerman M. Depressive symptom profiles and severity patterns in outpatients with psychotic vs nonpsychotic major depression. Compr Psychiatry. 2008;49:421–429. doi: 10.1016/j.comppsych.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kiev A. New York: Free Press; 1972. Transcultural Psychiatry. [Google Scholar]
- 23.Yi JS, Bae SO, Ahn YM, Park DB, Noh KS, Shin HK, et al. Validity and reliability of the Korean version of the Hamilton Depression Rating Scale (K-HDRS) J Korean Neuropsychiatr Assoc. 2005;44:456–465. [Google Scholar]
- 24.Kim KI. Clinical study of primary depressive symptom. Part II: symptom pattern of the Korean depressive. J Korean Neuropsychiatr Assoc. 1977;16:46–52. [Google Scholar]
- 25.Kim KI, Cho YG. Clinical study of primary depressive symptom. part VII: chronological comparison of depressive symptom between 1974-1976 and 1992-1993. Ment Health Res. 1993;12:110–117. [Google Scholar]
- 26.First MB, Spitzer RL, Gibbon M, Williams JB. User's Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders Research Version SCID-I. New York: New York State Psychiatric Institute, Biometrics Research; 1996. [Google Scholar]
- 27.Guy W. Rockville: National Institute of Mental Health; 1976. ECDEU Assessment Manual for Psychopharmacology, Revised. [Google Scholar]
- 28.American Psychiatric Association. Fourth Edition. Washington, DC: American Psychiatric Press; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 29.Lopez MF, Compton WM, Grant BF, Breiling JP. Dimensional approaches in diagnostic classification: a critical appraisal. Int J Methods Psychiatr Res. 2007;16(Suppl 1):S6–S7. doi: 10.1002/mpr.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz M, Blazer DG. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry Suppl. 1996;(30):17–30. [PubMed] [Google Scholar]