Abstract
SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis) is a relatively rare entity. The therapeutic approach of patients with SAPHO syndrome has included multiple drugs with varying success and incoherence responses. The therapy is still empirical today. SAPHO syndrome is commonly treated with non-steroidal anti-inflammatory drugs, bisphophonates and non-biologic disease modifying antirheumatic drugs. Recent reports showed successful treatment with tumour necrosis factor α (TNF α) antagonists, but there is still a dark side of SAPHO syndrome including a subgroup of patient’s refractory to all the treatments that have been empirically experienced. A clinical report of a patient with SAPHO syndrome with 12 years of evolution is described. All the therapeutic approaches, including anti TNF α therapy, have not prevented the clinical and radiographic progression of the disease. Given that the disease affects mostly younger patients, new therapeutic strategies are necessary in order to avoid potentially irreversible joint and bone lesions.
Background
SAPHO is a heterogenic syndrome that includes five different entities – synovitis, acne, pustulosis, hyperostosis and osteitis. Chamot et al classified it for the first time in 1987.1
The disease is characterised by periodic exacerbations and remissions and its severity can range widely. The most important feature of this syndrome is the association of multiple osteoarticular inflammation with specific dermatologic disorders. A possible link between these conditions and spondylarthropathies has also been underlined.2
To date, SAPHO syndrome in considered a rare disease, however its prevalence is probably underestimated. Its prevalence is considered not more than 1/10 000. SAPHO syndrome can be seen in all ages, but it is more frequent in children and young to middle-aged adults with a female predominance. Majority of reported cases come form Japan and Northern and Western Europe. Fewer cases were reported in the US and the UK.3 4
As its underlying aetiopathogenesis is still poorly understood, the treatment of SAPHO syndrome remains empirical.5 Non-steroidal anti-inflammatory drugs (NSAIDs) are the first choice for symptomatic relieve but have limited efficacy on the disease progression. Antibiotics and several immunosuppressants and immunomodulators (corticosteroids, sulfasalazine, methotrexate, ciclosporin, leflunomide) have been tried with varying degrees of success.6 Antitumour necrosis factor α (TNF-α) therapies could be considered in refractory SAPHO syndrome, with recent reports demonstrating treatment effectiveness in some patients.7
Case presentation
A 27-year-old male was referred to our clinic with pain at the level of the sternoclavicular joint bilaterally, associated with papular and pustular skin lesions scattered throughout the trunk and face.
The dermatosis had about 12 years of evolution, characterised by periods of exacerbation and remission. In teenage, he was diagnosed with acne fulminans on the face and trunk treated with antibiotic (doxycycline) and isotretinoin with a good dermatological evolution.
About 1 year after the onset of skin manifestations, he started with inflammatory pain complaints, in the anterior chest region (sternoclavicular), bilateral characterised as persistent and of moderate intensity. Throughout the duration of the disease he had always been treated with NSAIDs and analgesics in progressively higher doses.
On physical examination, he had scattered skin lesions in the dorsal trunk (figure 1). The joint examination revealed pain on sternoclavicular and costoclavicular joints palpation. There were no other significant alterations.
Figure 1.
Scattered acne skin lesions in the dorsal trunk.
Investigations
Blood tests showed no elevated inflammatory parameters, immunologic tests (antinuclear antibody, antidouble stranded DNA antibody, immunoglobulin levels and complement levels, human leucocyte antigen B27 and serologic tests (human immunodeficiency virus, venereal disease research laboratory and hepatitis B and C) were negative. The reactive arthritis related bacteria were tested (Chlamydia trachomatis, Salmonella spp., Shigella spp., Yersinia spp. and Campylobacter spp), with negative results.
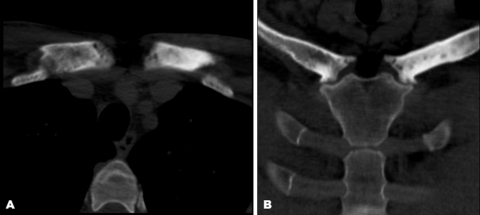
The chest radiography showed bilaterally severe destruction of the sternoclavicular joint (figure 2). Bone scintigraphy showed increased uptake on both sternocostoclavicular joints. A thoracic CT scan revealed sternocostoclavicular hyperostosis with subchondral erosions (figure 3A,B).
Figure 2.
Chest radiography showing bilaterally severe destruction of the sternoclavicular joint.
Figure 3.
(A, B) CT scans of the anterior chest wall showing sternocostoclavicular hyperostosis with subchondral erosions.
With these findings fulfulling the diagnostic criteria, SAPHO syndrome was diagnosed.
Treatment
The initial therapeutic approach included antibiotic (doxycycline) and NSAIDs with a significant improvement in the skin lesions but with persistence of pain complaints. Subsequently, treatment with oral prednisolone (0.5 mg/kg body weight/day) and alendronate (70 mg weekly) were added without success. Thus, the patient was started on methotrexate in increasing doses (until 20 mg weekly), keeping the need for prednisolone and NSAIDs for symptomatic relief. No osteoarticular improvement was verified.
After 6 months of therapeutic with corticosteroids and methotrexate, the patient began with pain complaints on the left arm.
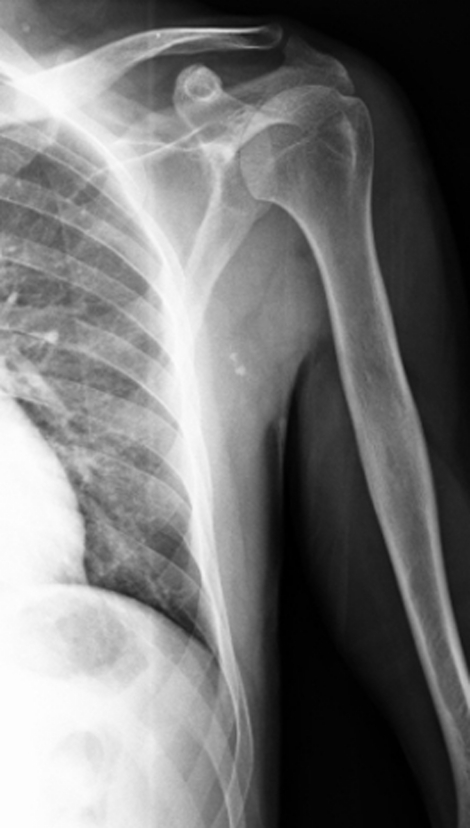
Left femur plain radiography showed osteosclerosis and hypertrophic osteitis (figure 4).
Figure 4.
Left femur plain radiography showing osteosclerosis and hypertrophic osteitis.
A CT scan of the left arm revealed typical SAPHO lesions of hypertrofic osteitis (figure 5).
Figure 5.
CT scan of the left arm showing typical synovitis, acne, pustulosis, hyperostosis and osteitis lesions of hypertrofic osteitis.
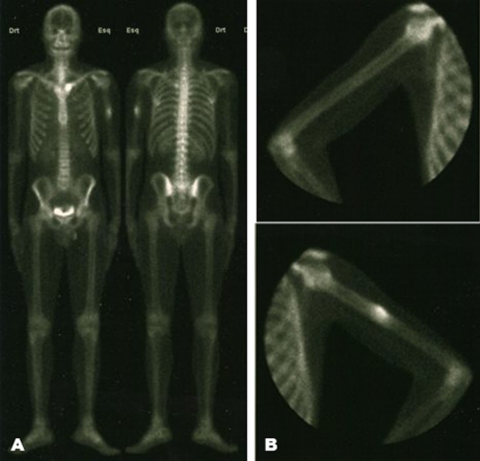
A second bone scintigraphy showed persistency of increased uptake on both sternocostoclavicular joints and associated osteosclerosis and hypertrophic osteitis on the left arm (figure 6A,B).
Figure 6.
(A, B) Bone scintigraphy showing intense hyperfixation on sternoclavicular joints and on the left humeral shaft.
Given the refractoriness of the disease, he was started on anti TNF α therapy – adalimumab 40 mg every 2 weeks, with slightly improvement of pain complaints but persistence of radiologic findings of osteitis.
Discussion
The SAPHO syndrome was first described as a single entity by Chamot, unifying in a single syndrome a variety of clinical and radiological manifestations, whose common denominators are osteoarticular and specific skin changes.1
Some diagnostic criteria were proposed for classification of this entity:
The existence of skin lesions or pustular acne in the presence of sterile synovitis, hyperostosis, osteitis;
Sterile synovitis, hyperostosis, osteitis involving the axial or peripheral skeleton (especially the anterior thoracic region, vertebrae or sacroiliac joints), with or without characteristic skin lesions;
Sterile synovitis, hyperostosis, osteitis involving the axial or peripheral skeleton (especially multiple metaphyses of long bones in children), with or without characteristic skin lesions.8
The skin and osteoarticular manifestations do not necessarily have to coexist for the diagnosis of SAPHO syndrome. In some cases may occur a time lag of several years between the onset of each of the clinical manifestations.
The osteoarticular changes include synovitis, hyperostosis and osteitis, and are most often found in the upper anterior thoracic region (sternoclavicular, costoclavicular, sternomanubrial). Osteoarticular lesions are manifested also in extra-thoracic sites (predominantly involving the sacroiliac joints) and may mimic other seronegative spondylarthropathies.9
Dermatological conditions can be split into two groups:
Severe acne (acne fulminans, acne conglobata and hidradenitis suppurativa)
Pustulosis (pustular psoriasis and palmoplantar pustulosis).9
In acne, the presence and activity of the anaerobic organism Propionibacterium acnes, has been advocated as a triggering factor and has been related to more severe skin lesions.10
Several studies have defended different infectious agents as potential causes of the clinical manifestations, regarding the favourable response to antibiotics observed in some cases. Similar to what happens in acne lesions, there is some evidence of P acnes having a primordial role in SAPHO pathogenesis, triggering an exacerbated systemic inflammatory response.2 11 In 1987, Trimble et al observed that intraarticular injection of inactivated P acnes in laboratory animals can cause joint lesions and bone erosions.12
Hurtado-Nédélec et al have published a study revealing that this bacterium appears to increase the production of IL-8 and TNF α by polymorphonuclear (PMN) in both healthy subjects and in patients with SAPHO syndrome, rheumatoid arthritis or psoriatic arthritis. A study in patients with SAPHO syndrome revealed that PMN had a significantly decreased response to P acnes, which could lead to a potential inherent mechanism of desensitisation.13
The role of autoimmunity in clinic perpetuation has gained importance over the past years. The simultaneous occurrence of various immune-mediated manifestations such as psoriasis vulgaris, pyoderma gangrenosum and inflammatory bowel disease support this theory.13
Despite the multiplicity of aetiopathogenic theories that have been proposed for the SAPHO syndrome, treatment of these patients remains empirical, without guidelines properly validated. Clinical results have been equally inconsistent.
There is agreement in therapy with analgesics and anti-inflammatory drugs for symptomatic relief. Some studies have shown bisphosphonates as a possible and promising therapeutic approach. Recently, taking into account the probable associated autoimmune component, immunomodulatory and immunosuppressive therapies have been tried with apparently symptomatic and radiological favourable results.6 7
The presented patient had a dermatological improvement with antibiotic and imunossupressive therapy. However, the radiological osteoarticular lesions located to the anterior thoracic region and to the left arm persisted despite the use of multiple therapeutic approaches, including anti-TNF α therapy.
The SAPHO syndrome is found predominantly in younger patients, with average ages of 30 and 50 years.3 The time of diagnosis between the onset of symptoms and diagnosis is approximately 9 years, according to a study involving 120 patients with SAPHO syndrome.14 Even though the long-term prognosis is favourable,15 it is expected that these patients present at the time of diagnosis, years of disease progression and hence potentially irreversible bone or joint lesions. In this context, the treatment should be as early, effectively and safely as possible, in order to prevent osteoarticular progression and to limit the adverse effects associated with pharmacological drugs. However, there is a dark side of the SAPHO syndrome, including patients refractory to all therapies currently experienced and described in the literature, which include NSAIDs, bisphophonates, glucocorticoids, non-biologic disease modifying antirheumatic drugs and TNF α antagonists.
We believe that the scientific advances in understanding the mechanisms of SAPHO syndrome and the development of new drugs, will drive us to potentially new immunosuppressive approaches directed to this specific subgroup of patients.
Learning points.
-
▶
SAPHO syndrome is a rare entity.
-
▶
The treatment is still empirical without validated guidelines and includes NSAIDs, bisphophonates, glucocorticoids and non-biologic disease modifying antirheumatic drugs.
-
▶
Some reports demonstrated improvement on skin and osteoarticular lesions with TNF α antagonists, such as adalimumab, infliximab and etanercept.
-
▶
There is a subgroup of patients with SAPHO syndrome refractory to all drugs empirically experienced and therefore it is an evidence that much more has to be done for this patients in the future.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Chamot AM, Benhamou CL, Kahn MF, et al. [Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases]. Rev Rhum Mal Osteoartic 1987;54:187–96 [PubMed] [Google Scholar]
- 2.Kahn MF, Khan MA. The SAPHO syndrome. Baillieres Clin Rheumatol 1994;8:333–62 [DOI] [PubMed] [Google Scholar]
- 3.Van Doornum S, Barraclough D, McColl G, et al. SAPHO: rare or just not recognized? Semin Arthritis Rheum 2000;30:70–7 [DOI] [PubMed] [Google Scholar]
- 4.Colina M, Govoni M, Orzincolo C, et al. Clinical and radiologic evolution of synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome: a single center study of a cohort of 71 subjects. Arthritis Rheum 2009;61:813–21 [DOI] [PubMed] [Google Scholar]
- 5.Magrey M, Khan MA. New insights into synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome. Curr Rheumatol Rep 2009;11:329–33 [DOI] [PubMed] [Google Scholar]
- 6.Olivieri I, Padula A, Palazzi C. Pharmacological management of SAPHO syndrome. Expert Opin Investig Drugs 2006;15:1229–33 [DOI] [PubMed] [Google Scholar]
- 7.Ben Abdelghani K, Dran DG, Gottenberg JE, et al. Tumor necrosis factor-alpha blockers in SAPHO syndrome. J Rheumatol 2010;37:1699–704 [DOI] [PubMed] [Google Scholar]
- 8.Benhamou CL, Chamot AM, Kahn MF. Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol 1988;6:109–12 [PubMed] [Google Scholar]
- 9.Robert B, Donald R. The SAPHO syndrome: an evolving concept for unifying several idiopathic disorders of bone and skin. Am J Roentgenol 1998;170:585. [DOI] [PubMed] [Google Scholar]
- 10.Webster GF. Inflammatory acne represents hypersensitivity to Propionibacterium acnes. Dermatology (Basel) 1998;196:80–1 [DOI] [PubMed] [Google Scholar]
- 11.Colina M, Lo Monaco A, Khodeir M, et al. Propionibacterium acnes and SAPHO syndrome: a case report and literature review. Clin Exp Rheumatol 2007;25:457–60 [PubMed] [Google Scholar]
- 12.Rozin AP, Nahir AM. Is SAPHO syndrome a target for antibiotic therapy? Clin Rheumatol 2007;26:817–20 [DOI] [PubMed] [Google Scholar]
- 13.Hurtado-Nedelec M, Chollet-Martin S, Nicaise-Roland P, et al. Characterization of the immune response in the synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome. Rheumatology (Oxford) 2008;47:1160–7 [DOI] [PubMed] [Google Scholar]
- 14.Hayem G, Bouchaud-Chabot A, Benali K, et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum 1999;29:159–71 [DOI] [PubMed] [Google Scholar]
- 15.Maugars Y, Berthelot JM, Ducloux JM, et al. SAPHO syndrome: a followup study of 19 cases with special emphasis on enthesis involvement. J Rheumatol 1995;22:2135–41 [PubMed] [Google Scholar]