Abstract
BACKGROUND
Female sexual dysfunction is a focus of medical research but few studies describe the prevalence and covariates of recent sexual activity and satisfaction in older community-dwelling women.
METHODS
1303 older women from the Rancho Bernardo Study were mailed a questionnaire on general health, recent sexual activity, sexual satisfaction, and the Female Sexual Function Index (FSFI).
RESULTS
806 of 921 respondents (87.5%) age ≥40 years answered questions about recent sexual activity. Their median age was 67; mean years since menopause, 25; most were upper-middle class; 57% had attended at least one year of college; 90% reported good to excellent health. Half (49.8%) reported sexual activity within the past month with or without a partner, the majority of whom reported arousal (64.5%), lubrication (69%), and orgasm (67.1%) at least most of the time, although one-third reported low, very low, or no sexual desire. Although frequency of arousal, lubrication, and orgasm decrease with age, the youngest (<55 yrs) and oldest (>80 yrs) women reported a higher frequency of orgasm satisfaction. Emotional closeness during sex was associated with more frequent arousal, lubrication, and orgasm; estrogen therapy was not. Overall, two-thirds of sexually active women were moderately or very satisfied with their sex life, as were almost half of sexually inactive women.
CONCLUSION
Half these women were sexually active, with arousal, lubrication, and orgasm maintained into old age, despite low libido in one-third. Sexual satisfaction increased with age and did not require sexual activity.
Keywords: Age, female sexual function, libido, sexual activity, sexual satisfaction, women
INTRODUCTION
Alfred Kinsey and colleagues established the Institute for Sex Research and quantified male sexuality for the first time in their 1948 book [1]; five years later their book on female sexual behavior appeared [2]. In 1966 Masters and Johnson provided anatomic and physiologic data on human sexual response [3]. Although sexuality, particularly sexual dysfunction, is now a major focus of medical research, there are few studies of sexual activity and sexual satisfaction in community-dwelling older women.
It is known that sexual activity in older women is positively associated with having a partner [4–6], good health [6–8], and current estrogen use [9]. A few community-based [10] and population-based [4, 11, 12] studies have asked about satisfaction, desire, arousal, and orgasm in older women. The largest survey of female sexual activity leading to personal distress was mailed to a representative sample of 50,003 US women ages 18 to 101 in 2006; 63% responded [12]. In that study, low desire (libido) was the most common problem reported by all age groups; women aged 45–64 reported more sexually related distress than younger and older women.
We report here a study of sexual activity and satisfaction as reported by older community-dwelling women from the Rancho Bernardo Study cohort. We describe the (1) prevalence of current sexual activity; (2) characteristics associated with sexual activity including demographics, self-reported health, menopause history, and hormone use; (3) frequency of arousal, lubrication, orgasm, and pain during intercourse among sexually active women; and (4) sexual desire and sexual satisfaction in sexually active and sexually inactive older women.
METHODS
Study Population
The Rancho Bernardo Study (RBS) included 82% of community-dwelling adult residents of Rancho Bernardo, a suburb of San Diego, California. Since inception in 1972–4, Study participants have been followed annually by mail for vital status and morbidity, and every other year for specific conditions or behaviors potentially related to healthy aging. The Study was approved by the Institutional Review Board of the University of California, San Diego. Mailed questionnaires reminded participants that responses were voluntary and they did not need to answer any questions that they preferred not to answer.
MEASURES
In October 2002, 1303 surviving Rancho Bernardo Study community-dwelling women were mailed a questionnaire about physical and emotional health, menopause, hysterectomy status, current estrogen use, the presence or absence of an intimate partner, and the presence or absence of recent (past month) sexual activity with or without a partner. Standard 5-point scales with the responses “excellent,” “very good,” “good,” “fair or “poor” were used to assess self-rated physical and emotional health. The Female Sexual Function Index (FSFI) [13] was mailed in the same envelope, which included the participant RBS identifier but no personal identifiers.
The FSFI, a multidimensional scale for assessing sexual dysfunction in women, includes 19 questions developed by Rosen and colleagues [13]; FSFI has demonstrated reliability and validity in women with or without sexual dysfunction, has good test-retest reliability for each of its individual domains (r = .79 – .86) and overall (Cronbach’s alpha ≥.82). FSFI estimates the extent of difficulty in six domains of sexual function: desire, arousal lubrication, orgasm, pain, and satisfaction.
We inserted one additional question: “Over the past 4 weeks, have you engaged in any sexual activity or intercourse?” for a total of 20 questions (Appendix 1, question 3). The first two questions were answered independent of partner status or recent sexual activity and relate to sexual desire. The next eleven questions were answered only by women who had engaged in sexual activity in the past four weeks, with or without a partner, and relate to arousal, lubrication, and orgasm. The next four questions concerned emotional closeness with a partner and pain associated with vaginal penetration. The 19th question addressed satisfaction with overall sexual life in all respondents who had a partner whether or not they were currently sexually active. The last question addressed overall sexual satisfaction with or without a partner.
The FSFI questionnaire specifies that sexual activity could include caressing, foreplay, masturbation, and intercourse. Intercourse was defined as penile penetration (entry) of the vagina. The questionnaire specifically stated, “You do not need to have a partner to answer this questionnaire.”
Statistical Analysis
Data from 806 of the 921 women (87.5%) aged ≥40 who returned the questionnaire and answered the question about recent sexual activity with or without a partner in the past four weeks are the basis of this report. Baseline characteristics are summarized for the entire study cohort and compared between women who were sexually active and those who were not. Results are presented as means and standard deviations of continuous variables with t-test used to evaluate significant differences. Categorical variables are shown as percentages, and associations are tested with chi-square tests. Age is analyzed by quartile based on the 806 respondents, with 201 or 202 women in each quartile: quartiles are age <55.13; 55.14–68.02; 68.03–79.91; and ≥79.92. Data are analyzed using SAS (version 9.2; SAS Institute, Cary, NC) and SPSS (version 17.0; SPSS Inc., Chicago, IL).
RESULTS
Table 1 shows the characteristics of the 806 women overall and separately by the presence or absence of recent sexual activity. The median age was 67 (range 40 – 99) years; 63% (503) were postmenopausal, 20% (158) reported still having menses, and 17% (143) had insufficient data to classify. The mean number of years postmenopause was 24.6 years; mean age at menopause based on last menses was 47.7 years; 22.4 % of all women reported a bilateral oophorectomy. Overall 30.3% reported using estrogen therapy at the time of the survey. More than half of the women had at least begun a college education, and more than 90% of the heads of household were white-collar workers. The majority of women reported at least good physical and emotional health.
Table 1.
Characteristics of 2002 Mailer Respondents who answered question about sexual activity with or without a partner (FSFI_3)
| Characteristics | Total Respondents (n=806) | Sexual activity in last 4 wks | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No (n=405) | Yes (n=401) | |||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | p-value | |
| Age at Mailer | 806 | 66.9 | 15.3 | 405 | 74.9 | 13.0 | 401 | 58.7 | 13.0 | <.0001 |
| Yrs post-menopausal | 503 | 24.6 | 13.0 | 301 | 28.4 | 12.9 | 202 | 18.9 | 11.1 | <.0001 |
| BMI ** | 383 | 25.9 | 4.6 | 232 | 26.0 | 4.7 | 151 | 25.8 | 4.5 | n.s. |
| n | % | n | % | n | % | |||||
|
|
|
|
||||||||
| Over age 65 | 442 | 54.8 | 314 | 77.5 | 128 | 31.9 | <.0001 | |||
| Marital Status ** | ||||||||||
| living w/ spouse/partner | 232 | 60.1 | 112 | 47.4 | 120 | 79.5 | <.0001 | |||
| widowed | 109 | 28.2 | 92 | 39.1 | 17 | 11.2 | ||||
| other | 45 | 11.7 | 31 | 13.2 | 14 | 9.3 | ||||
| Some college | 413 | 57.0 | 218 | 63.7 | 195 | 51.0 | <.001 | |||
| Occupation | ||||||||||
| executives/professionals | 663 | 91.3 | 305 | 89.2 | 358 | 93.2 | n.s. | |||
| skilled/semi-skilled | 45 | 6.2 | 26 | 7.6 | 19 | 5.0 | ||||
| other | 18 | 2.5 | 11 | 3.2 | 7 | 1.8 | ||||
| Bilateral oopherectomy | 173 | 22.4 | 92 | 23.9 | 81 | 21.0 | n.s. | |||
| Ever HRT | 469 | 58.9 | 241 | 60.7 | 228 | 57.1 | n.s. | |||
| Current HRT | 238 | 30.3 | 90 | 22.8 | 148 | 37.8 | <.0001 | |||
| Self-Reported Physical | ||||||||||
| Health | ||||||||||
| excellent | 131 | 16.6 | 42 | 10.7 | 89 | 22.3 | <.0001 | |||
| very good | 321 | 40.6 | 142 | 36.1 | 179 | 45.0 | ||||
| good | 251 | 31.7 | 148 | 37.7 | 103 | 25.9 | ||||
| fair/poor | 88 | 11.1 | 61 | 15.5 | 27 | 6.8 | ||||
| Self-Reported Emotional | ||||||||||
| Health | ||||||||||
| excellent | 155 | 19.6 | 58 | 14.6 | 97 | 24.4 | <.0001 | |||
| very good | 314 | 39.6 | 150 | 38.2 | 164 | 41.2 | ||||
| good | 242 | 30.6 | 132 | 33.5 | 110 | 27.6 | ||||
| fair/poor | 81 | 10.2 | 54 | 13.7 | 27 | 6.8 | ||||
| Satisfaction w/ sex life | ||||||||||
| very satisfied | 203 | 34.2 | 72 | 34.3 | 131 | 34.2 | <.0001 | |||
| moderately satisfied | 158 | 26.6 | 30 | 14.3 | 128 | 33.3 | ||||
| equal satisf/dissatisfied | 93 | 15.7 | 40 | 19.0 | 53 | 13.8 | ||||
| moderately dissatisfied | 72 | 12.1 | 30 | 14.3 | 42 | 10.9 | ||||
| very dissatisfied | 68 | 11.4 | 38 | 18.1 | 30 | 7.8 | ||||
obtained from a sub-sample of women who attended a clinic visit in 1999–2002
Sexual Activity
Sexual activity in the past four weeks was reported by half the respondents (n = 401 with vs. 405 without sexual activity), 321(80%) of whom reported having a partner. Sexually active women were on average 16 years younger than sexually inactive women group (58.7 vs. 74.9 years, respectively, p <.0001) (Table 1). Overall 79.5% of sexually active women were living with a spouse or other partner, as were 47.4% of sexually inactive women. Recent sexual activity did not vary by occupation of head of household, but was less often reported by women with some college education than without. Ninety-three percent of sexually active women reported good, very good, or excellent physical and emotional health. Sexually active women were more likely than sexually inactive women to report current hormone use (p < .0001). Bilateral oophorectomy was not associated with sexual activity. In analyses stratified by quartiles of age, the likelihood of being sexually active declined with increasing age: 83% of the youngest women, 64% of the second quartile, 40% of the third quartile, and 13% of the fourth quartile reported recent sexual activity.
Sexual Desire and Sexual Satisfaction in Sexually Active and Sexually Inactive Women
All women with or without recent sexual activity were questioned about their interest in sex. Forty percent (39.87%) of all women stated that they never or almost never felt sexual desire; one-third of sexually active women reported low, very low, or no sexual desire. Only 3% said they felt sexual desire almost always or always--41% were in the youngest age group; 30% were using postmenopausal estrogen. Sexual desire was positively associated with current hormone use, sexual activity, and frequency of arousal, lubrication, and orgasm.
Most sexually active women were moderately satisfied (24%) or very satisfied (54%) with the amount of emotional closeness during sex with their partner. Emotional closeness was not related to age, current hormone use, or participant’s education level. Satisfaction with the amount of emotional closeness during sexual activity with a partner was associated with more frequent arousal, lubrication, and orgasm.
All women with or without recent sexual activity were questioned about their sexual satisfaction with a partner. About 64% of all women in this cohort were moderately satisfied (24%) or very satisfied (40%) with their sexual relationship with their partner. Reporting “very satisfied” was noted less frequently in the youngest women (33.5%).
Regardless of partner status or sexual activity, overall 61% reported that they were moderately satisfied (26.6%) or very satisfied (34.2%) with their overall sexual life. Nearly half of sexually inactive women (48.6%) reported they were at least moderately satisfied (Table 1). For all women, the frequency of being very satisfied with sexual life increased in a graded stepwise fashion with increasing quartile of age ( 25.3% for the youngest women, 30.1%, 44.1 %, and 46.7% for the oldest women (p<.001).
Arousal, Lubrication, Orgasm, Pain in Sexually Active Women
Among sexually active women, 64.5% reported being aroused most times, almost always, or always; 69% reported being lubricated most times, almost always, or always; 67.1 % achieved orgasm most times, almost always, or always; and 86.4% reported discomfort or pain during vaginal penetration only a few times, almost never, or never.
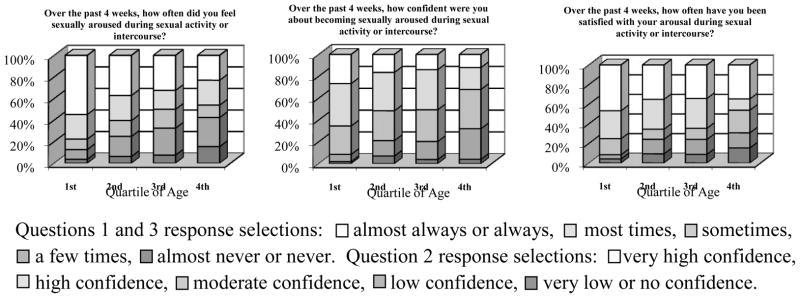
When analyzed by quartiles of age, the youngest women reported the highest frequency of arousal (54.8%), however, 23.1 % of the oldest women (age 80+) reported arousal almost always or always; a similar pattern for satisfaction with arousal was reported (Figure 1). Level of sexual arousal and confidence about sexual arousal followed a similar distribution. There was no significant association between arousal and current hormone use.
Figure 1.
Sexual Arousal Responses in Sexually Active Older Women (Responses to questions pertaining to arousal by quartile of age in sexually active women; first quartile < 55.12 years, second quartile 55.14 – 68.02 years, third quartile 68.03 – 79.91 years, fourth quartile > 79.92 years.)
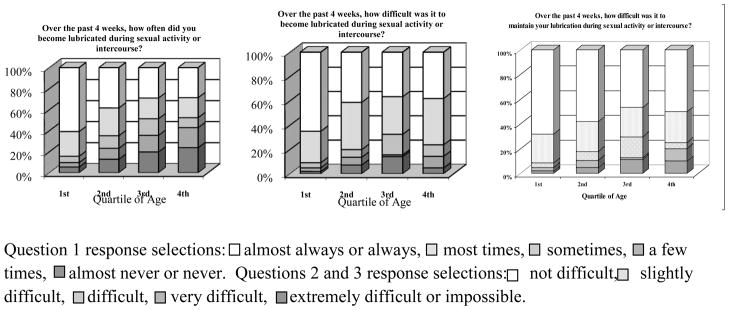
Frequency of lubrication during sexual activity decreased with age; 60.8% of the youngest women reported lubrication almost always or always compared to 28.6% of women age 80 or older; a similar trend was reported with frequency of and difficulty maintaining lubrication (Figure 2). There was no significant association between current hormone therapy use and lubrication.
Figure 2.
Lubrication Responses in Sexually Active Older Women (Responses to questions pertaining to lubrication by quartile of age in sexually active women; first quartile < 55.12 years, second quartile 55.14 – 68.02 years, third quartile 68.03 – 79.91 years, fourth quartile > 79.92 years.)
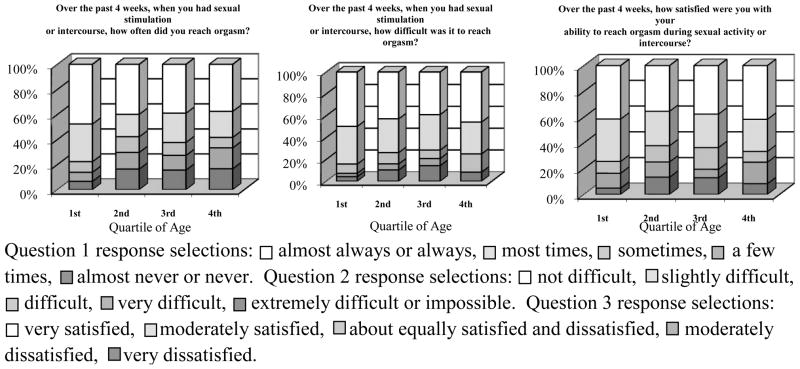
The youngest women had the highest frequency of orgasm (47.6%); however, 37.5% of the oldest women reported reaching orgasm almost always or always (Figure 3). Lack of difficulty reaching orgasm followed a similar distribution and trend. The highest orgasm satisfaction was reported in both the youngest and oldest women; almost 42% of women in the youngest age quartile were very satisfied with their ability to reach orgasm, 35.4% in the second quartile, 37.7% in the third quartile, and 41.7% in the oldest quartile (Figure 3). There was no significant association between orgasm and current hormone use.
Figure 3.
Orgasm Responses in Sexually Active Older Women (Responses to questions pertaining to orgasm by quartile of age in sexually active women; first quartile < 55.12 years, second quartile 55.14 – 68.02 years, third quartile 68.03 – 79.91 years, fourth quartile > 79.92 years.)
Less than 5% of sexually active women reported a very high or high levelof discomfort or pain during or following sexual activity. Among the oldest women, 71.4% reported their level or degree of discomfort or pain as low, very low, or none during or following vaginal penetration. There was no significant association between current HRT use and pain with vaginal penetration.
DISCUSSION
Half of these community-dwelling women aged 40 to 100 years reported sexual activity within the last four weeks. In other studies, recent sexual activity was questioned differently and in different age groups, making direct comparisons difficult. Despite differences in study design and population characteristics, a significant proportion of older women report sexual activity [4, 5, 7, 12, 14, 15].
Confirming other published studies, sexual activity decreased with age [7, 8, 10, 15, 16] and was positively associated with presence of a partner [4, 6, 9, 15].Good physical and emotional health was associated with sexual activity, consistent with other studies [4, 6, 9, 14, 15, 17]. Poor emotional or physical health or the presence of chronic illness was associated with sexual inactivity[7, 18–21]. While we report an inverse relationship between some college education and sexual activity, results from other studies linking sexual activity with college education are mixed [4, 5, 22, 23].
Because the Female Sexual Function Index was designed to quantify sexual dysfunction [13], most early reports in the literature described the sexual domains in terms of dysfunction; less data exist in unselected community-based samples. In the Rancho Bernardo cohort, frequent arousal, lubrication, and orgasm were reported by about two-thirds of sexually active women. Although the highest frequency of arousal and lubrication was reported by the youngest women, at least one in five women age ≥80 years reported arousal, lubrication, and orgasm almost always or always.
Low sexual desire was reported by about one-third of sexually active women in Rancho Bernardo, similar to the prevalence reported elsewhere [11, 12, 24]. A diagnosis of Hypoactive Sexual Desire Disorder (HSDD) requires symptoms resulting in personal distress; we did not ask about personal distress and cannot report the prevalence of HSDD. The youngest Rancho Bernardo women reported lower sexual satisfaction with higher sexual desire and this could represent a higher percentage of younger women who meet the criteria for HSDD. Low sexual desire increases with age, but distress about low sexual desire decreases with age [12].
Previously, low sexual desire has been correlated with low levels of arousal, orgasm, and pleasure [11, 25, 26], though sexual desire and arousal have also been suggested to occur independently [27]. In the present study, despite a correlation between sexual desire and other sexual function domains, only one of five sexually active women across all age groups reported high sexual desire. Nearly half of women aged 80 or older reported arousal, lubrication, and orgasm most of the time, but rarely reported sexual desire. In contrast to the traditional linear model in which desire precedes sex [3, 28], these results support a nonlinear model of sexuality in older women [29, 30] because sexual desire did not precede sexual arousal in most women, suggesting women engage in sexual activity for multiple reasons, which may include nurture, affirmation, or sustenance of a relationship.
Current hormone therapy was associated with sexual activity and desire but not with arousal, lubrication, orgasm, or satisfaction. Current estrogen therapy may affect sexual health indirectly by relieving menopausal symptoms or by improving how women perceive their emotional and/or physical health. No clinical trials have shown a causal association between estrogen therapy and the sexual function domains reported here [31]. Because oral estrogen therapy increases sex hormone binding globulin levels, and thereby reduces bioavailable estradiol levels, oral estrogen therapy may not provide physiologic free estradiol levels. In contrast, one study reports sexual desire increases with testosterone treatment [32]. Some clinical trial evidence shows use of transdermal testosterone along with estrogen may increase the frequency of satisfying sexual activity in naturally postmenopausal women with HSDD [33], but testosterone therapy is not approved by the U.S. FDA. Recent UK treatment guidelines recommend a multidisciplinary approach to female sexual problems and include the use of testosterone in selected patients [34].
While older age has been described as a significant predictor of low sexual satisfaction [35], the percentage of RBS sexually satisfied women actually increased with age quartile, with close to half (47.5%) of the women over 80 reporting sexual satisfaction almost always or always. Not only were the oldest women in this cohort the most satisfied overall, those who were recently sexually active experienced orgasm satisfaction rates similar to those of the youngest quartile. Sexual relationship satisfaction was also reported by the majority of women with or without recent sexual activity. Two-thirds of the sexually active women were moderately or very satisfied with their sex life, as were almost half of sexually inactive women. In this study, sexual activity was not always necessary for sexual satisfaction. Those who were not sexually active may have achieved sexual satisfaction through touching, caressing, or other intimacies that have developed over the course of a long relationship.
Generalizability in this study is limited by the socioeconomic homogeneity of the cohort. The response rate was good for this type of questionnaire, but response bias may exist because only those with the best emotional or physical health may have been sexually active or have taken time to complete the long questionnaire. The sexual activity questionnaire itself may have prompted sexual activity. Our 2002 questionnaire did not ask about the partner’s use of medication for erectile dysfunction; increasing use of such medication may have altered the sexual activity available to women. Given that sexual satisfaction does not always require sexual activity, a greater emphasis on specific sources of satisfaction may be useful in the evaluation of sexual domains [36]. Emotional and physical closeness to the partner may be more important than experiencing orgasm [37]. A more positive approach to female sexual health focusing on sexual satisfaction may be more beneficial to women than a focus limited to female sexual activity or dysfunction [36].
Acknowledgments
Funding: The Rancho Bernardo Study was funded by the National Institutes of Health/National Institute on Aging grants AG07181 and AG028507 and the National Institute of Diabetes and Digestive and Kidney Diseases, grant DK31801.
Appendix 1 Modified Female Sexual Function Index
How often did you feel sexual desire or interest?
How would you rate your level (degree) of sexual desire or interest?
-
Over the past 4 weeks, have you engaged in any sexual activity or intercourse?
Respondents who answered no were instructed to skip to #19.
How often did you feel sexually aroused during sexual activity or intercourse
How would you rate your level of sexual arousal during sexual activity or intercourse?
How confident were you about becoming sexually aroused during sexual activity or intercourse?
How often have you been satisfied with your arousal during sexual activity or intercourse?
How often did you become lubricated during sexual activity or intercourse?
How difficult was it to become lubricated during sexual activity or intercourse?
How often did you maintain your lubrication until completion of sexual activity or intercourse?
How difficult was it to maintain your lubrication until completion of sexual activity or intercourse?
When you had sexual stimulation or intercourse, how often did you reach orgasm?
When you had sexual stimulation or intercourse, how difficult was it for you to reach orgasm?
-
How satisfied were you with your ability to reach orgasm during sexual activity or intercourse?
Respondents who do not have a partner were instructed to skip to question #20.
How satisfied have you been with the amount of emotional closeness during sexual activity between you and your partner?
How would you rate your level (degree) of discomfort or pain during or following vaginal penetration?
How often did you experience discomfort or pain during vaginal penetration?
How often did you experience discomfort or pain following vaginal penetration?
How satisfied have you been with your sexual relationship with your partner?
How satisfied have you been with your overall sexual life?
Most responses used a five point Likert scale. Frequency responses – Almost always or always: 5 points, Most times (more than half of the time): 4 points, Sometimes (about half of the time): 3 points, A few times (less than half of the time): 2 points, Almost never or never: 1 point. Level responses – Very high: 5 points, High: 4 points, Moderate: 3 points, Low: 2 points, Very low or none at all: 1 point.
Footnotes
All authors have no conflicts of interest to report.
All authors had access to the data and a role in writing the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kinsey APWB, Martin CE. Sexual Behavior in the Human Male. Philadelphia: W.B. Saunders Co; 1948. [Google Scholar]
- 2.Kinsey APWB, Martin CE, Gebhard PH. Staff of the Institute of Sex Research Sexual Behavior in the Human Female. Philadelphia: W.B. Saunders Co; 1953. [Google Scholar]
- 3.Masters WHJV. Human Sexual Response. Toronto, New York: Bantam Books; 1966. [Google Scholar]
- 4.Addis IB, Van Den Eeden SK, Wassel-Fyr CL, et al. Sexual activity and function in middle-aged and older women. Obstet Gynecol. 2006;107(4):755–64. doi: 10.1097/01.AOG.0000202398.27428.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avis NE, Brockwell S, Randolph JF, Jr, et al. Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women's Health Across the Nation. Menopause. 2009;16(3):442–52. doi: 10.1097/gme.0b013e3181948dd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beutel ME, Stobel-Richter Y, Brahler E. Sexual desire and sexual activity of men and women across their lifespans: results from a representative German community survey. BJU Int. 2008;101(1):76–82. doi: 10.1111/j.1464-410X.2007.07204.x. [DOI] [PubMed] [Google Scholar]
- 7.Lindau ST, Schumm LP, Laumann EO, Levinson W, O'Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357(8):762–74. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolosi A, Laumann EO, Glasser DB, et al. Sexual behavior and sexual dysfunctions after age 40: the global study of sexual attitudes and behaviors. Urology. 2004;64(5):991–7. doi: 10.1016/j.urology.2004.06.055. [DOI] [PubMed] [Google Scholar]
- 9.Davison SL, Bell RJ, LaChina M, Holden SL, Davis SR. Sexual function in well women: stratification by sexual satisfaction, hormone use, and menopause status. J Sex Med. 2008;5(5):1214–22. doi: 10.1111/j.1743-6109.2008.00780.x. [DOI] [PubMed] [Google Scholar]
- 10.Hayes RD, Dennerstein L, Bennett CM, Koochaki PE, Leiblum SR, Graziottin A. Relationship between hypoactive sexual desire disorder and aging. Fertil Steril. 2007;87(1):107–12. doi: 10.1016/j.fertnstert.2006.05.071. [DOI] [PubMed] [Google Scholar]
- 11.Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive sexual desire disorder in postmenopausal women: US results from the Women's International Study of Health and Sexuality (WISHeS) Menopause. 2006;13(1):46–56. doi: 10.1097/01.gme.0000172596.76272.06. [DOI] [PubMed] [Google Scholar]
- 12.Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112(5):970–8. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 13.Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 14.Laumann EO, Paik A, Glasser DB, et al. A cross-national study of subjective sexual well-being among older women and men: findings from the Global Study of Sexual Attitudes and Behaviors. Arch Sex Behav. 2006;35(2):145–61. doi: 10.1007/s10508-005-9005-3. [DOI] [PubMed] [Google Scholar]
- 15.Huang AJ, Subak LL, Thom DH, et al. Sexual function and aging in racially and ethnically diverse women. J Am Geriatr Soc. 2009;57(8):1362–8. doi: 10.1111/j.1532-5415.2009.02353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howard JR, O'Neill S, Travers C. Factors affecting sexuality in older Australian women: sexual interest, sexual arousal, relationships and sexual distress in older Australian women. Climacteric. 2006;9(5):355–67. doi: 10.1080/13697130600961870. [DOI] [PubMed] [Google Scholar]
- 17.Marsiglio W, Donnelly D. Sexual relations in later life: a national study of married persons. J Gerontol. 1991;46(6):S338–44. doi: 10.1093/geronj/46.6.s338. [DOI] [PubMed] [Google Scholar]
- 18.Nussbaum MRH, Carol, Lenahan, Patricia Chronic Illness and Sexual Functioning. American Family Physician. 2003;62(2):7. [PubMed] [Google Scholar]
- 19.Cyranowski JM, Bromberger J, Youk A, Matthews K, Kravitz HM, Powell LH. Lifetime depression history and sexual function in women at midlife. Arch Sex Behav. 2004;33(6):539–48. doi: 10.1023/B:ASEB.0000044738.84813.3b. [DOI] [PubMed] [Google Scholar]
- 20.Gallicchio L, Schilling C, Tomic D, Miller SR, Zacur H, Flaws JA. Correlates of sexual functioning among mid-life women. Climacteric. 2007;10(2):132–42. doi: 10.1080/13697130601167956. [DOI] [PubMed] [Google Scholar]
- 21.Kaya C, Yilmaz G, Nurkalem Z, Ilktac A, Karaman MI. Sexual function in women with coronary artery disease: a preliminary study. Int J Impot Res. 2007;19(3):326–9. doi: 10.1038/sj.ijir.3901530. [DOI] [PubMed] [Google Scholar]
- 22.Robinson JG, Molzahn AE. Sexuality and quality of life. J Gerontol Nurs. 2007;33(3):19–27. doi: 10.3928/00989134-20070301-05. quiz 38–9. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez M, Viafara G, Caba F, Molina T, Ortiz C. Libido and orgasm in middle-aged woman. Maturitas. 2006;53(1):1–10. doi: 10.1016/j.maturitas.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Rosen RC, Shifren JL, Monz BU, Odom DM, Russo PA, Johannes CB. Correlates of sexually related personal distress in women with low sexual desire. J Sex Med. 2009;6(6):1549–60. doi: 10.1111/j.1743-6109.2009.01252.x. [DOI] [PubMed] [Google Scholar]
- 25.Hartmann U, Philippsohn S, Heiser K, Ruffer-Hesse C. Low sexual desire in midlife and older women: personality factors, psychosocial development, present sexuality. Menopause. 2004;11(6 Pt 2):726–40. doi: 10.1097/01.gme.0000143705.42486.33. [DOI] [PubMed] [Google Scholar]
- 26.Davis SR, Davison SL, Donath S, Bell RJ. Circulating androgen levels and self-reported sexual function in women. JAMA. 2005;294(1):91–6. doi: 10.1001/jama.294.1.91. [DOI] [PubMed] [Google Scholar]
- 27.Graziottin A. Libido: the biologic scenario. Maturitas. 2000;34 (Suppl 1):S9–16. doi: 10.1016/s0378-5122(99)00072-9. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan HS. The new sex therapy. New York: Brunner/Mazel; 1974. [Google Scholar]
- 29.Basson R. The female sexual response: a different model. J Sex Marital Ther. 2000;26(1):51–65. doi: 10.1080/009262300278641. [DOI] [PubMed] [Google Scholar]
- 30.Hayes RD. Circular and linear modeling of female sexual desire and arousal. J Sex Res. 48(2–3):130–41. doi: 10.1080/00224499.2010.548611. [DOI] [PubMed] [Google Scholar]
- 31.Wierman ME, Nappi RE, Avis N, et al. Endocrine aspects of women's sexual function. J Sex Med. 7(1 Pt 2):561–85. doi: 10.1111/j.1743-6109.2009.01629.x. [DOI] [PubMed] [Google Scholar]
- 32.Davison SL, Davis SR. Androgenic hormones and aging - The link with female sexual function. Horm Behav. 59(5):745–53. doi: 10.1016/j.yhbeh.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 33.Shifren JL, Davis SR, Moreau M, et al. Testosterone patch for the treatment of hypoactive sexual desire disorder in naturally menopausal women: results from the INTIMATE NM1 Study. Menopause. 2006;13(5):770–9. doi: 10.1097/01.gme.0000243567.32828.99. [DOI] [PubMed] [Google Scholar]
- 34.Wylie K, Rees M, Hackett G, et al. Androgens, health and sexuality in women and men. Hum Fertil (Camb) 13(4):277–97. doi: 10.3109/14647273.2010.530966. [DOI] [PubMed] [Google Scholar]
- 35.Tomic D, Gallicchio L, Whiteman MK, Lewis LM, Langenberg P, Flaws JA. Factors associated with determinants of sexual functioning in midlife women. Maturitas. 2006;53(2):144–57. doi: 10.1016/j.maturitas.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 36.Hutcherson HKS, Krychman M, Schwartz P, Leiblum S, Rosen R, Althof S. A Positive Approach to Female Sexual Health: A Summary Report. The Female Patient. 2009;Supplement(2009 April) [Google Scholar]
- 37.Busing S, Hoppe C, Liedtke R. Sexual satisfaction of women--development and results of a questionnaire. Psychother Psychosom Med Psychol. 2001;51(2):68–75. doi: 10.1055/s-2001-10757. [DOI] [PubMed] [Google Scholar]