Abstract
Urinary tract infection (UTI) is the most common bacterial infection in women in general and in postmenopausal women in particular. Two groups of elderly women with recurrent UTI should be differentiated regarding age and general status: healthy, young postmenopausal women aged 50 to 70 years who are neither institutionalized or catheterized and elderly institutionalized women with or without a catheter. Bacteriuria occurs more often in elderly functionally impaired women, but in general it is asymptomatic. However, the risk factors associated with recurrent UTI in elderly women are not widely described. In a multivariate analysis it was found that urinary incontinence, a history of UTI before menopause, and nonsecretor status were strongly associated with recurrent UTI in young postmenopausal women. Another study described the incidence and risk factors of acute cystitis among nondiabetic and diabetic postmenopausal women. Independent predictors of infection included insulin-treated patients and a lifetime history of urinary infection. Borderline associations included a history of vaginal estrogen cream use in the past month, kidney stones, and asymptomatic bacteriuria at baseline. Another important factor in postmenopausal women is the potential role that estrogen deficiency plays in the development of bacteriuria. There are at least two studies showing a beneficial effect of estrogen in the management of recurrent bacteriuria in elderly women. One of these studies showed that vaginal estrogen cream reduced vaginal pH from 5.5±0.7 to 3.6±1.0, restored lactobacillus, and decreased new episodes of UTI. Another study reported similar results using an estriol vaginal ring. However, contradictory results are found in the literature. For example, additional studies found that the use of estriol-containing vaginal pessaries was less effective than oral nitrofurantoin macrocrystals in preventing UTI in postmenopausal women. Two other studies also did not find any benefit in the reduction of UTI by oral estrogen therapy. Unfortunately, the use of estrogen in preventing UTI in postmenopausal women remains questionable. New strategies have been researched for reducing the use of antibiotics in the prevention and treatment of UTI. Two of them are probiotics and cranberry juice or capsules. Although several studies regarding probiotics and cranberry juice or capsules have reported a reduction of episodes of UTI, there is no conclusive evidence that they are useful in the prevention of UTI in postmenopausal women. As for the optimal drug, dosage, and length of treatment for UTI in the elderly, there are no studies comparing these data with the treatment for young women.
Keywords: Bacteriuria elderly women, Postmenopausal women, Urinary tract infections
INTRODUCTION
Urinary tract infection (UTI) is the most common bacterial infection in young and elderly women. Despite the higher incidence of bacteriuria in elderly women, most UTI research has been conducted in young women. This chapter will discuss epidemiological studies regarding risk factors associated with bacteriuria in elderly women. Bacteriuria in the elderly is associated with high mortality rates; however, in most cases, bacteriuria is asymptomatic and not a causal factor of death.
Estrogen deficiency plays an important role in the development of bacteriuria. Several studies have been conducted showing the efficacy of estrogen (orally and vaginally) in the prevention of UTI. Yet, the literature is divided on this subject, and other studies have not shown any advantage in using estrogen.
This chapter will focus on the updated known data regarding the use of estrogen in the prevention of bacteriuria in elderly women. The alarming increase in multidrug-resistant uropathogens makes it imperative that alternative strategies are found. One strategy is the restoration of flora with lactobacilli using probiotics and another is the use of cranberry, a competitive compound that inhibits the attachment of bacteria to the uroepithelial mucosa and thereby reduces the frequency of UTI.
METHODOLOGY
A systematic literature search was performed of studies conducted over the past 15 years. A few recent studies have investigated the management of UTI in postmenopausal women. The data were collected from the most up-to-date published studies and guidelines, which were found by searching Medline, PubMed, and the Cochrane database with the following key words: 'bacteriuria in elderly women' and 'postmenopausal women and UTI'. A total of 190 papers were screened by title and abstract: 111 for the first keyword and 79 for the second. Only English publications addressing the keywords were screened.
The 25 references used in the text were assessed according to the level of scientific evidence involved. The studies were rated according to the level of evidence (LoE) and the grade of recommendations (GoR) by using ICUD standards [1,2].
DEMOGRAPHY
UTI is the most common bacterial infection in women. Three groups of women with recurrent UTI should be distinguished on the basis of age: premenopausal women, healthy postmenopausal women between the ages of 50 to 70 years who are neither institutionalized nor catheterized, and elderly institutionalized women, who are in many cases catheterized.
Bacteriuria occurs more often in functionally impaired women than in those who are not impaired; persistent bacteriuria is seen more often in nursing home residents, and transient bacteriuria is seen more often in young, healthy postmenopausal women. The majority of elderly women with bacteriuria are asymptomatic and should not be treated with antibiotics (LoE 1b) [3,4]. In young to middle-aged women, the prevalence of UTI is <5%, rising considerably with advancing age. Epidemiologic studies have shown that 15% to 20% of 65-70 year-old women have bacteriuria, compared with 20% to 50% of women >80 years old.
Despite the high incidence of bacteriuria in postmenopausal women (young and institutionalized), most UTI research has been conducted in younger women. Hence, the most common UTI risk factors among healthy younger women, such as frequent vaginal intercourse, spermicide use, diaphragm use, condom use, a previous UTI history, recent antibiotic use, and nonsecretor status, were not widely investigated in middle-aged and elderly women (LoE 2a) [5].
BACTERIURIA IN YOUNG VS. ELDERLY WOMEN
Foxman et al conducted a case-control study investigating the role of health behavior and sexual and medical history in UTI risk among otherwise healthy women aged 40 to 65 years [4]. They showed that sexual activity was not associated with acquiring UTI in this age group, whereas a history of UTI during the past year, urine loss, antibiotic use during the previous 2 weeks, and exposure to cold during the previous 2 weeks were positively associated with UTI. In addition, drinking cranberry juice and taking vitamin C were moderately protective (LoE 2b) [4].
RISK FACTORS
A case-control study compared 149 postmenopausal women with a history of recurrent UTI with 53 age-matched women with no history of UTI. They looked for risk factors in healthy noninstitutionalized and noncatheterized women. Three urological factors, namely, incontinence (41% of case patients vs. 9% control patients; p<0.001), presence of a cystocele (19% vs. 0%; p<0.001), and postvoiding residual volume (28% vs. 2%; p<0.000008) were strongly associated with recurrent UTI. Multivariate analysis showed that urinary incontinence (odds ratio [OR], 5.79; 95% confidence interval [CI], 2.05-16.42; p=0.0009), a history of UTI before menopause (OR, 4.85; 95% CI, 1.7-13.84; p<0.003), and nonsecretor status (OR, 2.9; 95% CI, 1.28-6.25; p=0.005) were most strongly associated with recurrent UTI in postmenopausal women (LoE 2a) [5].
Jackson et al described the incidence and risk factors for acute cystitis among nondiabetic and diabetic postmenopausal women and the possible effect of estrogens on those women (LoE 2a) [6]. During 1,773 person-years of follow-up, 138 symptomatic UTIs occurred (incidence, 0.07 person-year). Independent prediction of infection included insulin-dependent diabetes mellitus (hazard ratio 95% CI, 1.7-7.0) and a lifetime history of UTI (hazard ratio for six or more infections, 6.9; 95% CI, 3.5-13.6). However, a borderline association included a history of vaginal estrogen cream use in recent months (hazard ratio, 1.8; 95% CI, 1.0-3.4), and a history of kidney stones (hazard ratio, 1.95; 95% CI, 0.9-3.5). However, sexual activity, urinary incontinence, parity, postcoital urination, vaginal dryness, use of cranberry juice, vaginal bacterial flora, and postvoid residual bladder volume were not associated with the incidence of acute cystitis after multivariable adjustment.
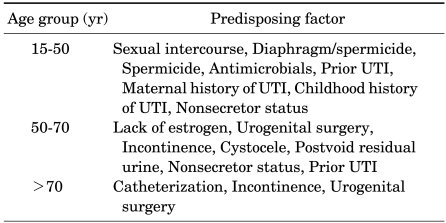
A study by Moore et al found that recent sexual intercourse, as described for younger women, was also strongly associated with incident UTI in other healthy postmenopausal women (LoE 2b) [7]. In the older, institutionalized women, urine catheterization and functional status deterioration appeared to be the most important risk factors associated with UTI (LoE 2a) [8]. The risk of UTI increases dramatically with catheterization. Table 1 describes the major factors predisposing adult women to UTI as related to age [9].
TABLE 1.
Major factors predisposing adult women to UTI as related to age [9]
UTI: urinary tract infection
BACTERIURIA AND MORTALITY
Bacteriuria has been discovered as a cause of increased mortality in elderly individuals. Studies of Greek, Finnish, and American patients showed decreased longevity associated with UTI (LoE 1b) [10-12]. The elderly patients with UTI were suffering from a variety of diseases other than UTI that might have increased their susceptibility to infections as well as their mortality.
Nordestam et al studied a population of elderly patients and compared their longevity in relation to bacteriuria (LoE 1b) [13]. There was no increase in mortality related to bacteriuria for otherwise healthy individuals. Bacteriuria per se did not appear to be a risk factor for mortality. In patients with concomitant disease, bacteriuria was associated with increased mortality, but it is not the cause.
THE ROLE OF ESTROGEN
Another important factor in postmenopausal women is the potential role that estrogen deficiency plays in the developmentof bacteriuria. Postmenopausal women frequently present with genitourinary symptoms; half have genitourinary disorders, and 29% have urinary incontinence (LoE 1b) [14]. Postmenopause is characterized by a significant reduction in ovary estrogen secretion, which is often associated with vaginal atrophy. Clinically, it manifests as a syndrome characterized by vaginal dryness, itching, dyspareunia, and urinary incontinence. This may sometimes imitate a UTI (LoE 2a) [15,16].
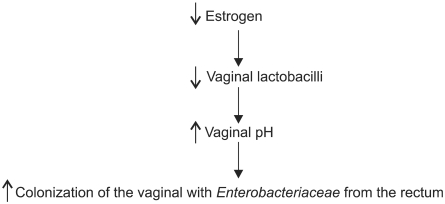
Estrogen stimulates the proliferation of lactobacillus in the vaginal epithelium, reduces pH, and avoids vaginal colonization of Enterobacteriaceae, which are the main pathogens of the urinary tract. Fig. 1 describes the relationship between estrogen and the vaginal flora and the pathophysiology of urinary tract infections in elderly women (LoE 1a) [17]. In addition, the absence of estrogen decreases the volume of the vaginal muscles, resulting in slackness of the ligaments holding the uteric pelvic floor and the bladder, resulting in the development of prolapse of the internal genitalia. Kicovic et al showed that vaginal cream decreased urogenital complaints associated with atrophic vaginitis (LoE 1b) [18].
FIG. 1.
Relationship between estrogen and the vaginal flora and pathophysiology of urinary tract infections in elderly women [17].
A previous randomized, double-blind, placebo-controlled study demonstrated that vaginal estriol treatment had a dramatic effect on recurrent UTIs in postmenopausal women. The results showed that the incidence of UTI in women who received vaginal estriol was reduced to 0.5 episodes per year compared with 5.9 episodes per year in women who received placebo. In addition, after 1 month of treatment, lactobacillus appeared in 60% of the estrogen-treated group but in none of the placebo group, and the vaginal pH decreased from 5.5±0.7 before treatment to 3.6±1.0 after treatment (LoE 1a) [19].
Several years later, similar results were obtained by Eriksen, using an estradiol-vaginal ring (LoE 1b) [20]. In that study, the women in the estradiol group had a significant reduction in the frequency of urogenital symptoms, such as vaginal dryness, dyspareunia, and urge and stress incontinence after 36 weeks of study. In addition, 45% of the women receiving estradiol were still free of UTI, in contrast with only 20% of the women treated with placebo.
However, contradicting results are found in the literature. For example, another study showed that the use of estriol-containing vaginal pessaries was less effective than the use of oral nitrofurantoin macrocrystals in the prevention of bacteriuria in postmenopausal women. This study also showed the failure of the estriol-containing vaginal pessaries to restore vaginal lactobacilli and to reduce vaginal pH in those women (LoE 1a) [21].
Brown et al assessed the effects of hormonal therapy on UTI frequency and examined potential risk factors (LoE 3) [22]. They used data from the Health and Estrogen/Progesterone Replacement Study, a randomized, blinded trial of the effect of hormone therapy on coronary heart disease events among 2,763 postmenopausal women aged 44 to 79 years with coronary diseases. UTI frequency was higher in the group receiving hormone treatment (0.625 mg conjugated estrogen plus 2.5 mg medroxyprogesterone acetate or placebo followed for a mean of 4.1 years), although the difference was not statistically significant. Statistically significant risk factors for UTI in the multivariate analysis included the following: women with diabetes mellitus in treatment (insulin OR, 1.81; 95% CI, 1.4-2.34), oral medication (OR, 1.44; 95% CI, 1.09-1.9), poor health (OR, 1.34; 95% CI, 1.14-1.57), vaginal itching (OR, 1.63; 95% CI, 1.07-2.5), and urge incontinence (OR, 1.51; 95% CI, 1.30-1.75). UTIs in the previous years were strongly associated with a simple UTI (OR, 7.00; 95% CI, 5.91-8.92) as well as with multiple UTIs (OR, 18.51; 95% CI, 14.27-24.02).
Jackson et al did not see that the use of oral or vaginal estrogen was a protective factor in order to avoid recurrent UTI (LoE 2a) [6].
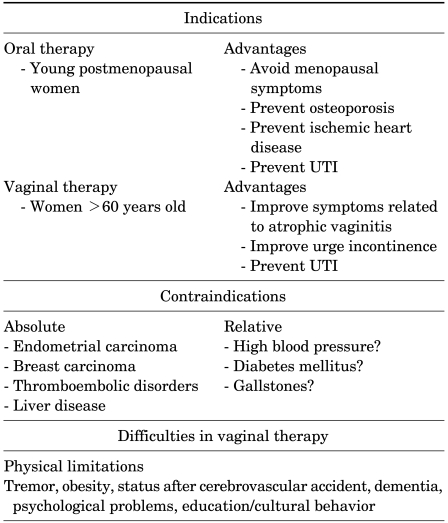
In conclusion, the efficacy of estrogen in the prevention of UTI in postmenopausal women with recurrent infections remains questionable. From a clinical perspective, the main currently recommended use of estrogen (probably vaginal and not oral) is in postmenopausal women, especially those infected with multidrug-resistant uropathogens, which limits the options and effectiveness of antimicrobial prophylaxis, and in women in whom the symptoms are related to atrophic vaginitis (5). Table 2 summarizes the indications and contraindications for estrogen therapy in UTI [3].
TABLE 2.
Indications and contraindications for estrogen therapy in UTI [3]
TREATMENT
Treatment of acute cystitis and pyelonephritis in otherwise healthy postmenopausal women is similar to that in premenopausal women; however, short-term therapy in postmenopausal women is not as well documented by controlled studies as in younger women. Raz and Rozenfeld published a study in postmenopausal women (mean age 65 years) with uncomplicated UTI in which ofloxacin, 200 mg once daily for 3 days (LoE 1b) [23], was significantly more effective in both short- and long-term follow-up than a 7 day course of cephalexin, 500 mg four times daily, even though all the uropathogens were susceptible to the two agents. In another double-blind study (LoE 1b), including a total of 183 postmenopausal women of at least 65 years of age with acute uncomplicated UTI, similar results were obtained with either a 3-day or a 7-day oral course of ciprofloxacin 250 mg two times daily (bacterial eradication 2 days after treatment 98% vs 93%, p=0.16), but the shorter course was better tolerated. The rate of bacterial eradication in this study was generally high, and the rate of bacterial resistance to ciprofloxacin low (GoR A) [24].
Asymptomatic bacteriuria in elderly women should not be treated with antibiotics (GoR A).
The optimal antimicrobials, dosages, and duration of treatment in elderly women appeared to be similar to those recommended for young postmenopausal women (GoR C). However, these results should not be extended to the frail elderly geriatric population with significant comorbidities, who frequently present with UTI caused by more resistant Gram-negative organisms and in whom treatment duration should be prolonged as in complicated UTI.
Estrogen (especially vaginal) could be administered for prevention of UTI; yet, the results are conflicting (GoR C). There are at least two clinical studies showing that vaginal estriol and estradiol-releasing vaginal rings restore vaginal flora, reduce pH, and reduce the number of symptomatic bacteriuria [19,20]. However, it appears that oral estrogen does not reduce the incidence of UTI in postmenopausal women (Hooton et al).
Alternative methods, like cranberry and probiotic lactobacilli, can contribute to preventing recurrent UTI in postmenopausal women, but more well-conducted studies are required to define their exact role and efficiency (GoR C). Once complicating factors, such as urinary obstruction, neurogenic bladder disturbances, etc, can be ruled out, an antimicrobial prophylaxis should be carried out as recommended for premenopausal women (GoR C).
NEW STRATEGIES
The alarming increase in multidrug-resistant uropathogens makes it imperative that alternative strategies are found. One strategy is the restoration of the normal flora with lactobacilli using probiotics. Another option is the use of a competitive compound that inhibits attachment of bacteria to the uroepithelium. Unfortunately, both methods have been evaluated without conclusive results, although there is some evidence that probiotics and cranberry are useful in preventing UTI.
Reid et al demonstrated the possibility of preventing uropathogen infection by using lactobacillus in vitro [25]. Several clinical studies showed that L. rhamnosus Gr-1 and L. fermentum-RC can colonize the vagina, a first step in preventing bacteriuria (LoE 2a). However, more studies, especially clinical studies, should be carried out to determine the role of probiotics in the prevention of UTI.
Another possibility is the use of cranberry. Cranberries contain a proanthocyanidin that can prevent the colonization of the E. coli uropathogen in the vaginal mucosa and reduce the frequency of bacteriuria (GoR C) [26]. McMurdo et al carried out a randomized controlled trial in elderly women to compare the efficacy in preventing UTI of cranberry capsules with trimethoprim (GoR C) [27]. The time to first recurrence of UTI was not significantly different between groups. In addition, trimethoprim had a very limited advantage over cranberry in the prevention of recurrent UTI in older women but had more adverse effects and withdrawals.
However, few clinical studies have been conducted, although in small and heterogenic populations, an advantage in the use of cranberry juice or other oral preparations in the prevention of bacteriuria has been shown. In the elderly population, there is only one clinical quasi-randomized study in elderly women with asymptomatic bacteriuria, which showed that bacteriuria and pyuria were significantly reduced in women taking cranberry juice in comparison with women who received placebo (GoR C) [28]. Because asymptomatic bacteriuria in the elderly is not treated, however, the clinical significance of this study remains inconclusive.
FURTHER RESEARCH
Further wide-scale randomized studies are essential to define and establish the exact role of estrogen therapy, probiotics, lactobacilli, and other possible and available methods to reduce the use of antibiotics.
CONCLUSIONS
Bacteriuria, particularly asymptomatic bacteriuria, is a very frequent finding in both healthy postmenopausal and institutionalized women. Urological factors, such as urinary incontinence, presence of any grade of cystocele and postvoiding residual volume, together with previous UTI and nonsecretor status, are associated with recurrent UTI in this population. Some studies showed a relationship between bacteriuria with diabetes or sexual intercourse. The role of vaginal or oral estrogen together with the use of probiotics and lactobacilli remains questionable.
Footnotes
This manuscript was published originally in: Naber KG, Schaeffer AJ, Heyns CF, Matsumoto T, Shoskes DA, Bjerklund Johansen TE (eds): Urogenital Infections. European Association of Urology - International Consultation on Urological Diseases, 1st edition 2010, Arnhem, The Netherlands, ISBN:978-90-79754-41-0.
The authors have nothing to disclose.
References
- 1.Abrams P, Khoury S, Grant A. Evidence--based medicine overview of the main steps for developing and grading guideline recommendations. Prog Urol. 2007;17:681–684. doi: 10.1016/s1166-7087(07)92383-0. [DOI] [PubMed] [Google Scholar]
- 2.Levels of evidence. Oxford Centre for Evidence-based medicine. [March 2009]. http://www.cebm.net.
- 3.Raz R. Hormone replacement therapy or prophylaxis in postmenopausal women with recurrent urinary tract infection. J Infect Dis. 2001;183(Suppl 1):S74–S76. doi: 10.1086/318842. [DOI] [PubMed] [Google Scholar]
- 4.Foxman B, Somsel P, Tallman P, Gillespie B, Raz R, Colodner R, et al. Urinary tract infection among women aged 40-65: behavioral and sexual risk factors. J Clin Epidemiol. 2001;54:710–718. doi: 10.1016/s0895-4356(00)00352-8. [DOI] [PubMed] [Google Scholar]
- 5.Raz R, Gennesin Y, Wasser J, Stoler Z, Rosenfeld S, Rottensterich E, et al. Recurrent urinary tract infections in postmenopausal women. Clin Infect Dis. 2000;30:152–156. doi: 10.1086/313596. [DOI] [PubMed] [Google Scholar]
- 6.Jackson SL, Boyko EJ, Scholes D, Abraham L, Gupta K, Fihn SD. Predictors of urinary tract infection after menopause: a prospective study. Am J Med. 2004;117:903–911. doi: 10.1016/j.amjmed.2004.07.045. [DOI] [PubMed] [Google Scholar]
- 7.Moore EE, Hawes SE, Scholes D, Boyko EJ, Hughes JP, Fihn SD. Sexual intercourse and risk of symptomatic urinary tract infection in post-menopausal women. J Gen Intern Med. 2008;23:595–599. doi: 10.1007/s11606-008-0535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolle LE. Asymptomatic bacteriuria in the elderly. Infect Dis Clin North Am. 1997;11:647–662. doi: 10.1016/s0891-5520(05)70378-0. [DOI] [PubMed] [Google Scholar]
- 9.Stamm WE, Raz R. Factors contributing to susceptibility of postmenopausal women to recurrent urinary tract infections. Clin Infect Dis. 1999;28:723–725. doi: 10.1086/515209. [DOI] [PubMed] [Google Scholar]
- 10.Dontas A, Kasviki-Charvati PC, Papanayiotou P, Marketos SG. Bacteriuria and survival in old age. N Engl J Med. 1981;304:939–943. doi: 10.1056/NEJM198104163041604. [DOI] [PubMed] [Google Scholar]
- 11.Nordenstam G, Brandberg A, Odén AS, Svanborg Edén C, Svanborg A. Bacteriuria and mortality in an elderly population. N Engl J Med. 1986;314:1152–1156. doi: 10.1056/NEJM198605013141804. [DOI] [PubMed] [Google Scholar]
- 12.Platt R, Polk BF, Murdock B, Rosner B. Mortality associated with nosocomial urinary tract infection. N Engl J Med. 1982;307:637–642. doi: 10.1056/NEJM198209093071101. [DOI] [PubMed] [Google Scholar]
- 13.Nordenstam G, Sundh V, Lincoln K, Svanborg A, Edén CS. Bacteriuria in representative population samples of persons aged 72-79 years. Am J Epidemiol. 1989;130:1176–1186. doi: 10.1093/oxfordjournals.aje.a115446. [DOI] [PubMed] [Google Scholar]
- 14.Iosif CS, Bekassy Z. Prevalence of genitor-urinary symptoms in the late menopause. Acta Obstet Gynecol Scand. 1984;63:257–260. doi: 10.3109/00016348409155509. [DOI] [PubMed] [Google Scholar]
- 15.Haspels AA, Luisi M, Kicovic PM. Endocrinological and clinical investigations in post-menopausal women following administration of vaginal cream containing oestriol. Maturitas. 1981;3:321–327. doi: 10.1016/0378-5122(81)90041-4. [DOI] [PubMed] [Google Scholar]
- 16.Thomas TM, Plymat KR, Blannin J, Meade TW. Prevalence of urinary incontinence. Br Med J. 1980;281:1243–1245. doi: 10.1136/bmj.281.6250.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raz R. Role of estriol therapy for women with recurrent urinary tract infections: advantages and disadvantages. Infectious Diseases in Clinical Practice. 1999;8:64–66. [Google Scholar]
- 18.Kicovic PM, Cortes-Prieto J, Milojević S, Haspels AA, Aljinovic A. The treatment of postmenopausal vaginal atrophy with ovestin vaginal cream or suppositories: clinical, endocrinological and safety aspects. Maturitas. 1980;2:275–282. doi: 10.1016/0378-5122(80)90029-8. [DOI] [PubMed] [Google Scholar]
- 19.Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993;329:753–756. doi: 10.1056/NEJM199309093291102. [DOI] [PubMed] [Google Scholar]
- 20.Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol. 1999;180:1072–1079. doi: 10.1016/s0002-9378(99)70597-1. [DOI] [PubMed] [Google Scholar]
- 21.Raz R, Colodner R, Rohana Y, Battino S, Rottensterich E, Wasser I, et al. Effectiveness of estriol-containing vaginal pessaries and nitrofurantoin macrocrystal therapy in the prevention of recurrent urinary tract infection in postmenopausal women. Clin Infect Dis. 2003;36:1362–1368. doi: 10.1086/374341. [DOI] [PubMed] [Google Scholar]
- 22.Brown JS, Vittinghoff E, Kanaya AM, Agarwal SK, Hulley S, Foxman B. Urinary tract infections in postmenopausal women: Effect of hormone therapy and risk factors. Obstet Gynecol. 2001;98:1045–1052. doi: 10.1016/s0029-7844(01)01630-1. [DOI] [PubMed] [Google Scholar]
- 23.Raz R, Rozenfeld S. 3-day course of ofloxacin versus cefalexin in the treatment of urinary tract infection in post-menopausal women. Antimicrob Agents Chemother. 1996;40:2200–2201. doi: 10.1128/aac.40.9.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vigel T, Verreault R, Gourdeau M, Morin M, Grenier-Gosselin L, Rochette L. Optimal duration of antibiotic therapy for uncomplicated urinary tract infection in older women: a double-blind randomized controlled trial. CMAJ. 2004;170:469–473. [PMC free article] [PubMed] [Google Scholar]
- 25.Reid G, Burton J. Use of lactobacillus to prevent infection by pathogenic bacteria. Microbes Infect. 2002;4:319–324. doi: 10.1016/s1286-4579(02)01544-7. [DOI] [PubMed] [Google Scholar]
- 26.Raz P. Urinary tract infection in elderly women. Int J Antimicrob Agents. 1998;10:177–179. doi: 10.1016/s0924-8579(98)00024-7. [DOI] [PubMed] [Google Scholar]
- 27.McMurdo ME, Argo I, Phillips G, Daly F, Davey P. Cranberry or trimethoprim for the prevention of recurrent urinary tract infections? A randomized controlled trial in older women. J Antimicrob Chemother. 2009;63:389–395. doi: 10.1093/jac/dkn489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avorn J, Monane M, Gurwitz JH, Glynn RJ, Choodnovskiy I, Lipsitz LA. Reduction of bacteriuria and pyuria after ingestion of cranberry juice. JAMA. 1994;271:751–754. doi: 10.1001/jama.1994.03510340041031. [DOI] [PubMed] [Google Scholar]