Abstract
Purpose
To present outcomes of transurethral removal (TUR) of intravesical or intraurethral mesh after midurethral slings.
Materials and Methods
This was a retrospective chart review of 23 consecutive women: 20 with intravesical mesh and 3 with intraurethral mesh.
Results
To remove the mesh, transurethral resection with an electrode loop (TUR-E) was used in 16 women and transurethral resection with a holmium laser (TUR-H) was used in 7. The median follow-up was 2.1 months. Twenty-six percent of the women (6/23) had a mesh remnant: 6.2% (1/16) of the women treated with TUR-E and 71.4% (5/7) of the women treated with TUR-H. Of the 5 women treated with TUR-H, 3 underwent concomitant transvaginal removal. On the follow-up cystoscopic exam, a mesh remnant was observed in 3 women (1 treated with TUR-E and 2 treated with TUR-H). Vesico-vaginal fistulas were found in 2 women during and after TUR-E, respectively. Stress urinary incontinence recurred in 1 woman.
Conclusions
TUR-E has a high success rate but carries a risk of bladder perforation. Complete resection using TUR-H depends on the location of the mesh and the range of motion of the instrument.
Keywords: Complications, Management, Suburethral slings
INTRODUCTION
Tension-free vaginal tape (TVT) is now the treatment of choice for female stress urinary incontinence because of its ease of use, minimal invasiveness, and high success rate [1]. However, this technique can have several complications. Properly identifying and treating complications remains critical for the practicing physician. Intravesical and intraurethral mesh are troublesome complications clinically and legally. Mesh in the bladder or urethra following midurethral sling has been reported to occur in somewhere between less than 1% to 6% of patients and can result from intraoperative needle penetration or tape erosion [2-4]. Even though the trans-obturator tape (TOT) procedure has less risk of lower urinary tract injury, surgeons should handle with care to prevent this complication. Bladder injury that is recognized during the operation is not usually related to long-term sequelae [5,6]. However, when bladder injury is missed or the mesh erodes into the bladder or urethra, patients might suffer from painful urination, recurrent urinary tract infection, irritative or obstructive symptoms, and hematuria.
Since the first case of urethral mesh erosion was reported in 2001, several case series have provided various techniques to manage this difficult complication [7,8-10]. Intravesical or intraurethral mesh can be removed by open surgery (cystorrhapy or urethrolysis and urethroplasty) or endoscopic surgery. However, evidence is lacking on the efficacies of these techniques.
The objective of this study was to determine the efficacy and complication associated with transurethral removal (TUR) of the intravesical or intraurethral mesh following midurethral sling procedures.
MATERIALS AND METHODS
A retrospective chart review was performed for women who had undergone transurethral surgery for bladder or urethral mesh between January 2002 and December 2010. A total of 23 consecutive women were identified, and their demographics, midurethral sling procedures, and removal procedures were reviewed. The surgical outcomes and complications were evaluated. To remove the mesh, transurethral resection with an electrode loop (TUR-E) was used until March 2010, when a holmium laser became available in the study center. Thereafter, transurethral resection with a holmium laser (TUR-H) was performed. The usual surgical techniques of TUR-E and TUR-H are described below.
1. Transurethral resection with an electrode loop
TUR-E was performed for 15 women with intravesical mesh and 1 woman with intraurethral mesh. With the patient under spinal anesthesia in the lithotomy position, a urethro-cystoscopic exam was performed with a 25 Fr resectoscope and a 0, 30, and 70 degree telescope. When the stone was attached to the mesh, lithotripsy was performed with a lithoclast. The mesh was then resected with an electrode loop until it was not visible or the perivesical fat was reached. The resected mesh was removed by foreign body forceps. After confirming that no mesh remained in the bladder or urethra a 16 Fr Foley catheter was inserted and left in place for a median of 6 days (range, 3 to 29 days). The median operation time was 57 minutes (40 to 135 minutes), and the median hospital stay was 8 days (4 to 36 days). Pictures of the TUR-E are provided in Fig. 1.
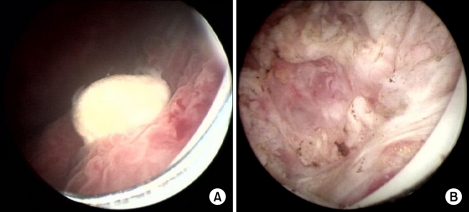
FIG. 1.
Pictures of the transurethral resection with an electrode loop for intravesical mesh. (A) Preoperative finding: stone encrustation. (B) Postoperative finding: no mesh remained and perivesical fat was seen.
Seven patients were treated with the TUR-H procedure with a rigid scope: 5 cases of intravesical mesh and 2 cases of intraurethral mesh. The surgery was similar to that for TUR-E except a holmium laser was used. When the stone was observed, lithotripsy was performed with the laser. The mesh was excised as near to the bladder or urethral mucosa as possible. When the laser could not cut deeply enough and strings or a portion of the mesh remained, the remnant was evaporated by the laser. The median energy used was 4.3 kJ (range, 0.7 to 14.9 kJ). After confirming that no mesh remained in the bladder or urethra, a 16 Fr Foley catheter was inserted and left in place for a median of 1 day (range, 1 to 2 days). The median operation time was 125 minutes (range, 30 to 180 minutes) and the median hospital stay was 4.5 days (range, 3 to 10 days). Pictures of the TUR-H are provided in Fig. 2.
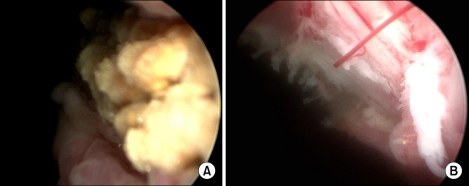
FIG. 2.
Pictures of the transurethral resection with a holmium laser for intravesical mesh. (A) Preoperative finding: stone encrustation. (B) Postoperative finding: no mesh remained.
Three women required concomitant transvaginal surgery for remnant mesh after TUR-H: 2 with intravesical mesh and 1 with intraurethral mesh. A midline vaginal incision was made and submucosal dissection was performed with mezenbaum scissors. After identifying the mesh, it was grasped with Kelly forceps and further dissection proceeded toward the exposed side while carefully maintaining traction on the mesh. After exposing the cut edge of the mesh through the vaginal incision, the whole exposed portion of the mesh was resected and removed. After removing the mesh, a cystoscopic exam excluded any mesh remnants. The wound was closed layer-by-layer with 3-0 Vicryl sutures. A Foley catheter was left in place for a median of 14 days (range, 6 to 21 days). The median operation time was 215 minutes (range, 180 to 220 minutes) and the median hospital stay was 8 days (range, 6 to 22 days). Pictures of the combined transvaginal and TUR-H procedures are provided in Fig. 3.
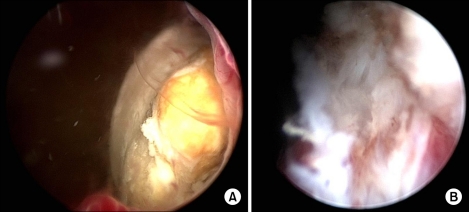
FIG. 3.
Pictures of the combined transvaginal and transurethral resection with a holmium laser for intraurethral mesh. (A) Preoperative finding: stone encrustation. (B) Postoperative finding: no mesh remained after transvaginal removal.
RESULTS
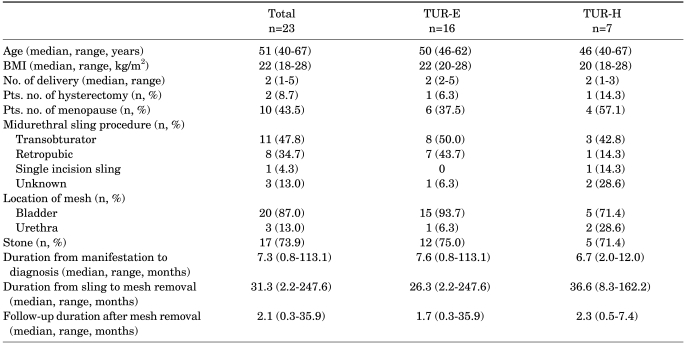
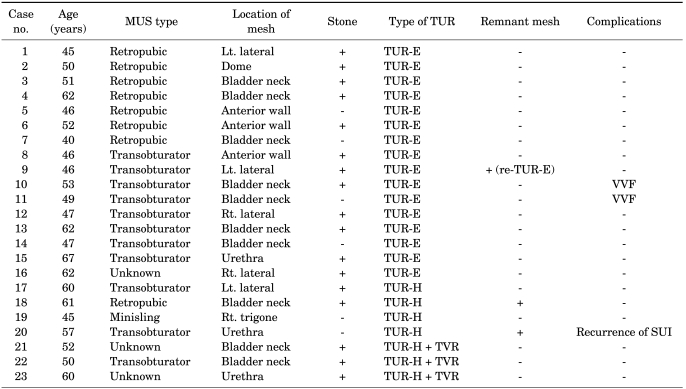
Patient demographics and the clinical characteristics of a total of 23 women are described in Table 1 according to the removal technique. Twenty women had intravesical mesh and 3 had intraurethral mesh. Sixteen women had the TUR-E procedure and 7 women had the TUR-H procedure. At the time of surgery, the median age was 51 years (range, 40 to 67 years). The median period between the midurethral sling and mesh removal was 31.3 months (range, 2.2 to 247.6 months), and the median follow-up period was 2.1 months (range, 0.3 to 35.9 months) after mesh removal. The previous midurethral sling procedures were 11 transobturator slings, 8 retropubic slings, 1 single incision sling, and 3 which were not identified. Seventeen women (73.9%) had calculi. Most women presented with multiple symptoms, including dysuria, hematuria, and irritative or obstructive urinary symptoms.
TABLE 1.
Patient demographics and clinical characteristics
TUR-E: transurethral resection with electrode loop, TUR-H: transurethral resection with holmium laser, BMI: body mass index
Table 2 summarizes the preoperative findings, surgical outcomes, and complications for all 23 cases. Overall, 6 women (26%) had a mesh remnant after transurethral surgery: 1 woman (6.2%) after TUR-E and 5 women (71.4%) after TUR-H. The woman who had a mesh remnant after TUR-E underwent repeat TUR-E for the remnant, and no mesh remained on the follow-up cystoscopic exam. Of the 5 women who had remnant mesh after TUR-H, 3 underwent concomitant transvaginal removal. On the postoperative cystoscopic exam, 2 women had remnant mesh after TUR-H. One woman had transvaginal removal with no mesh visible on the follow-up cystoscopic exam. In the other woman, a string of the mesh remained. She wanted to delay additional treatment for the remaining mesh because she had none of the preoperative symptoms.
TABLE 2.
Summary of the 23 cases
MUS: midurethral sling, TUR: transurethral removal, TUR-E: transurethral resection with electrode loop, TUR-H: transurethral resection with holmium laser, TVR: transvaginal removal, VVF: vesico-vaginal fistula, SUI: stress urinary incontinence
Two cases of vesico-vaginal fistulas occurred in women treated with TUR-E. One case was found during the TUR-E, and the fistula tract was immediately repaired transvaginally. A Foley catheter was placed for 29 days and no sequelae were observed during 9.5 months of follow-up. The other case was found 15 days after TUR-E. The woman experienced continuous urine leakage 7 days after the Foley catheter was removed. On the vaginal exam, an approximately 5 mm fistula tract was observed. Transvaginal fistulectomy was performed and a Foley catheter was placed for 21 days. No sequelae were observed during 35.5 months of follow-up. One case of stress incontinence (Stamey grade I) recurred in a woman who had remaining intraurethral mesh after TUR-H.
DISCUSSION
In this retrospective study, 26% of women (6/23) had a mesh remnant after transurethral removal of intravesical or intraurethral mesh. Mesh exposure in the bladder or urethra is an uncommon but troublesome complication of midurethral slings. Several authors have described their approaches to this difficult problem, with no consensus on the best approach [11-16]. Frenkl et al proposed a treatment algorithm after reviewing 22 cases of iatrogenic foreign bodies in the bladder and urethra following pelvic floor surgery [17]. They recommended cystorrhaphy or urethroplasty for mesh erosion of the lower urinary tract. They commented on the technical difficulties of endoscopic resection of the mesh due to the encrusted stone material and the difficulty in applying tension to the mesh during resection. However, there are more positive outcomes for endoscopic mesh removal. Standard transurethral resection had success rates of 90% to 100% in several case series with a small number of patients [7,17-19]. With the electrode loop, the mesh can be resected down to the submucosal portion. The electrode loop can also resect mesh in the bladder neck or urethra. Our series also showed a high success rate (93.7% [15/16]) after the TUR-E procedure. The location of the mesh did not affect the result. On the contrary, the holmium laser completely removed the mesh in only 28% of women (2/7). Some case reports have described the holmium laser as being effective for removing mesh [16,18,19]. However, this method leaves the possibility of remnant mesh exposure. Doumouchtsis et al reported that 4 of 6 women had recurrent erosion after transurethral resection using a holmium laser [20]. The holmium laser allows sharp incision of the mesh at the entrance and exit points. However, complete excision is difficult with a rigid cystoscope when the mesh is located in the bladder neck or urethra. Of the 3 successful cases of holmium laser excision reported by Giri et al, none were in the bladder neck or urethra, and a flexible instrument was used [16]. In the present study, the mesh was in the bladder neck or urethra in all 5 cases with mesh remaining after TUR-H, and we used a rigid scope. Therefore, we suggest that complete removal of the mesh using TUR-H depends on the location of the mesh and the range of motion of the instrument. Another reason for the low success rate after TUR-H might be less experience with the technique using holmium laser.
Two cases of vesico-vaginal fistulas were found during or after the TUR-E procedure. As mentioned above, one advantage of the electrode loop is that it can resect the mesh down to the submucosal portion. However, this resection carries a relatively high risk of bladder or urethral perforation. Because damaged urethral or bladder mucosa is atrophic, the risk of perforation may be increased. A factor requiring deep resection is the difficulty in allowing tension to the mesh. Two groups reported a combined endoscopic laparoscopic tape removal method [8,15]. In this method, a laparoscopic trocar was inserted suprapubically into the bladder under cystoscopic control. Under traction and fixation by suprapubically introduced forceps, the tape was cut and extracted transurethrally. A disadvantage of this technique is that it requires an additional bladder tract, which can increase the hospital stay and morbidity. To avoid bladder or urethral perforation, transurethral resection should be carried out carefully. Oh and Ryu recommended transvaginal finger-guided resection [21]. Nevertheless, transurethral resection using an electrode loop for intraurethral mesh might have a higher possibility of urethral perforation or incomplete resection. Also, with a holmium laser and rigid scope, it is difficult to remove the urethral mesh completely. Thus, we do not recommend transurethral surgery for urethral mesh.
All of the women had resolution of the preoperative lower urinary tract symptoms. The median duration from the manifestation of symptoms to diagnosis was more than 7 months. The possibility of unrecognized tape perforation or erosion and cystosopic exam should be considered in patients with lower urinary tract symptoms after a midurethral sling procedure. Stress urinary incontinence recurred in 1 woman who had a mesh remnant after TUR-H. She wanted to delay further treatment because the grade was minimal and her preoperative symptom was resolved. Given these results, transurethral resection wolud have a good functional outcome and low risk recurrence of stress incontinence.
This was a retrospective study and included a small number of cases. However, there are only limited data on the effectiveness of transurethral management for bladder or urethral mesh. Our results can provide information on the outcomes and complications of different transurethral removal techniques and can help physicians to choose the best treatment modality.
CONCLUSIONS
Transurethral surgery is associated with low morbidity and is familiar to urologists. To remove intravesical or intraurethral mesh after midurethral sling procedures, TUR-E has a high success rate, although it has a high risk of bladder perforation. In contrast, TUR-H has less risk of tissue damage, but complete resection seems to depend on the location of the mesh and the range of motion of the instrument. The evidence for TUR-H is not sufficient to conclude that this is an ineffective method for mesh removal; however, it should be performed in selected patients. Transurethral resection has good functional outcomes and a low risk of recurrence of stress incontinence.
Footnotes
The authors have nothing to disclose.
References
- 1.Lee YS, Lee HN, Lee KS. The evolution of surgical treatment for female stress urinary incontinence: era of mid-urethral slings. Korean J Urol. 2010;51:223–232. doi: 10.4111/kju.2010.51.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abouassaly R, Steinberg JR, Lemieux M, Marois C, Gilchrist LI, Bourque JL, et al. Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004;94:110–113. doi: 10.1111/j.1464-410X.2004.04910.x. [DOI] [PubMed] [Google Scholar]
- 3.Novara G, Galfano A, Boscolo-Berto R, Secco S, Cavalleri S, Ficarra V, et al. Complication rates of tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials comparing tension-free midurethral tapes to other surgical procedures and different devices. Eur Urol. 2008;53:288–308. doi: 10.1016/j.eururo.2007.10.073. [DOI] [PubMed] [Google Scholar]
- 4.Meschia M, Pifarotti P, Bernasconi F, Guercio E, Maffiolini M, Magatti F, et al. Tension-Free vaginal tape: analysis of outcomes and complications in 404 stress incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S24–S27. doi: 10.1007/s001920170008. [DOI] [PubMed] [Google Scholar]
- 5.McLennan MT, Melick CF. Bladder perforation during tension-free vaginal tape procedures: analysis of learning curve and risk factors. Obstet Gynecol. 2005;106:1000–1004. doi: 10.1097/01.AOG.0000185256.32405.76. [DOI] [PubMed] [Google Scholar]
- 6.Gold RS, Groutz A, Pauzner D, Lessing J, Gordon D. Bladder perforation during tension-free vaginal tape surgery: does it matter? J Reprod Med. 2007;52:616–618. [PubMed] [Google Scholar]
- 7.Koelbl H, Stoerer S, Seliger G, Wolters M. Transurethral penetration of a tension-free vaginal tape. BJOG. 2001;108:763–765. doi: 10.1111/j.1471-0528.2001.00188.x. [DOI] [PubMed] [Google Scholar]
- 8.Baracat F, Mitre AI, Kanashiro H, Montellato NI. Endoscopic treatment of vesical and urethral perforations after tension-free vaginal tape (TVT) procedure for female stress urinary incontinence. Clinics (Sao Paulo) 2005;60:397–400. doi: 10.1590/s1807-59322005000500008. [DOI] [PubMed] [Google Scholar]
- 9.Starkman JS, Wolter C, Gomelsky A, Scarpero HM, Dmochowski RR. Voiding dysfunction following removal of eroded synthetic mid urethral slings. J Urol. 2006;176:1040–1044. doi: 10.1016/j.juro.2006.04.103. [DOI] [PubMed] [Google Scholar]
- 10.Doumouchtsis SK, Lee FY, Bramwell D, Fynes MM. Evaluation of holmium laser for managing mesh/suture complications of continence surgery. BJU Int. 2011;108:1472–1478. doi: 10.1111/j.1464-410X.2010.10012.x. [DOI] [PubMed] [Google Scholar]
- 11.Volkmer BG, Nesslauer T, Rinnab L, Schradin T, Hautmann RE, Gottfried HW. Surgical intervention for complications of tension-free vaginal tape procedure. J Urol. 2003;169:570–574. doi: 10.1097/01.ju.0000046542.45062.37. [DOI] [PubMed] [Google Scholar]
- 12.Deng DY, Rutman M, Raz S, Rodriguez LV. Presentation and management of major complications of midurethral slings: Are complications under-reported? Neurourol Urodyn. 2007;26:46–52. doi: 10.1002/nau.20357. [DOI] [PubMed] [Google Scholar]
- 13.Irer B, Aslan G, Cimen S, Bozkurt O, Celebi I. Development of vesical calculi following tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:245–246. doi: 10.1007/s00192-004-1241-x. [DOI] [PubMed] [Google Scholar]
- 14.Kielb SJ, Clemens JQ. Endoscopic excision of intravesical tension-free vaginal tape with laparoscopic instrument assistance. J Urol. 2004;172:971. doi: 10.1097/01.ju.0000133899.82441.bf. [DOI] [PubMed] [Google Scholar]
- 15.Jorion JL. Endoscopic treatment of bladder perforation after tension-free vaginal tape procedure. J Urol. 2002;168:197. [PubMed] [Google Scholar]
- 16.Giri SK, Drumm J, Flood HD. Endoscopic holmium laser excision of intravesical tension-free vaginal tape and polypropylene suture after anti-incontinence procedures. J Urol. 2005;174:1306–1307. doi: 10.1097/01.ju.0000173926.04596.55. [DOI] [PubMed] [Google Scholar]
- 17.Frenkl TL, Rackley RR, Vasavada SP, Goldman HB. Management of iatrogenic foreign bodies of the bladder and urethra following pelvic floor surgery. Neurourol Urodyn. 2008;27:491–495. doi: 10.1002/nau.20558. [DOI] [PubMed] [Google Scholar]
- 18.Hodroff M, Portis A, Siegel SW. Endoscopic removal of intravesical polypropylene sling with the holmium laser. J Urol. 2004;172:1361–1362. doi: 10.1097/01.ju.0000139659.67173.e2. [DOI] [PubMed] [Google Scholar]
- 19.Feiner B, Auslender R, Mecz Y, Lissak A, Stein A, Abramov Y. Removal of an eroded transobturator tape from the bladder using laser cystolithotripsy and cystoscopic resection. Urology. 2009;73:681.e15–681.e16. doi: 10.1016/j.urology.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Doumouchtsis SK, Lee FY, Bramwell D, Fynes MM. Evaluation of holmium laser for managing mesh/suture complications of continence surgery. BJU Int. 2011;108:1472–1478. doi: 10.1111/j.1464-410X.2010.10012.x. [DOI] [PubMed] [Google Scholar]
- 21.Oh TH, Ryu DS. Transurethral resection of intravesical mesh after midurethral sling procedures. J Endourol. 2009;23:1333–1337. doi: 10.1089/end.2009.0098. [DOI] [PubMed] [Google Scholar]