Abstract
Heparin-induced thrombocytopenia (HIT) is an immune-mediated clinical syndrome of thrombocytopenia and thrombosis occurring after exposure to heparin. HIT most commonly occurs after exposure to unfractionated heparin but has also been reported with low-molecular-weight heparin. To date, there have been very few reports of HIT with the pentasaccharide fondaparinux, and some have proposed fondaparinux as a treatment for HIT. This article presents two cases of HIT associated with fondaparinux use.
Heparin-induced thrombocytopenia (HIT) is a prothrombotic condition associated with characteristic platelet-activating antibodies occurring after exposure to heparin (1). These IgG subclass antibodies recognize complexes of heparin and platelet factor 4 (PF4) and result in a clinical syndrome of thrombocytopenia and thrombosis, typically occurring 5 to 10 days after exposure to heparin. The syndrome is most commonly associated with the use of unfractionated heparin (UFH), with a much lower incidence reported with low-molecular-weight heparin (LMWH) (2, 3).
Fondaparinux (Arixtra) is a synthetic sulfated pentasaccharide that inhibits factor Xa indirectly by binding to antithrombin III. In postoperative orthopedic patients, it has been shown to be effective in the prevention of deep-venous thrombosis (DVT) (4), as well as the treatment of acute DVT and pulmonary embolus (5, 6). Antibodies to PF4/heparin develop in postoperative orthopedic patients receiving fondaparinux at a rate similar to those receiving enoxaparin, but none reacted with PF4/fondaparinux (3). Fondaparinux is likely unable to react with PF4 to generate ternary immune complexes to provide platelet activation. The risk of HIT is thought to be negligible with this medication, as it has even been proposed as a useful alternate anticoagulant in HIT (7, 8). There have been, however, a few case reports of HIT associated with fondaparinux use (9, 10). We describe two cases of HIT associated with fondaparinux that occurred in the postoperative setting after knee replacement.
CASE 1
A 47-year-old man with osteoarthritis underwent left total knee replacement at Baylor University Medical Center. He had no history of previous heparin exposure, and no heparin was given preoperatively or intraoperatively. His preoperative platelet count was 269 × 109/L. Beginning on postoperative day 1, he received prophylactic fondaparinux 2.5 mg subcutaneously daily and was discharged home on day 3 to complete fondaparinux for a total of 9 days.
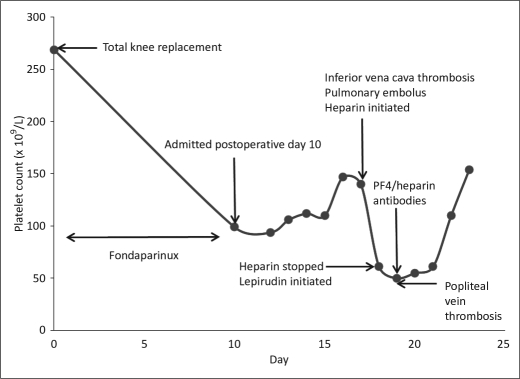
On the 10th postoperative day, he presented to the emergency department with decreased appetite, abdominal distention, left knee pain, and a temperature of 103°F. His final dose of fondaparinux was given the day prior to admission. At admission, his platelet count was 99 × 109/L, and he was initially believed to have sepsis secondary to postoperative joint infection. With antibiotics, his platelet count slowly increased to 147 × 109/L over the first 6 hospital days, and he received no heparin or LMWH during this time. An abdominal ultrasound on hospital day 7 to evaluate persistent abdominal pain and distention revealed an occlusive thrombus of his inferior vena cava. Magnetic resonance imaging of the abdomen also revealed bilateral adrenal hemorrhage. An UFH drip was subsequently started, and his platelet count fell precipitously from 140 × 109/L to a nadir of 50 × 109/L over a 24-hour period. He was also found to have an acute pulmonary embolus and left popliteal vein DVT over this interval (Figure 1).
Figure 1.
Clinical course of patient 1 with fondaparinux-associated heparin-induced thrombocytopenia.
His anti-PF4/heparin enzyme immunoassay, which was drawn approximately 8 hours after beginning UFH, was positive at an optical density of 2.807 units (normal value, <0.40). This positive result was confirmed with high-dose heparin neutralization studies. Testing for antiphospholipid antibodies as well as other hypercoagulable states was negative. Heparin was stopped, and alternate anticoagulation with lepirudin was initiated. His platelet count normalized over the next week. Warfarin was eventually started, and the patient was discharged home in good condition.
CASE 2
A 63-year-old man with osteoarthritis underwent a right total knee replacement at Baylor University Medical Center. No heparin was given preoperatively or intraoperatively. His preoperative platelet count was 376 × 109/L. Fondaparinux at 2.5 mg subcutaneously daily was started on postoperative day 1, and he was discharged on day 5 to continue the anticoagulant.
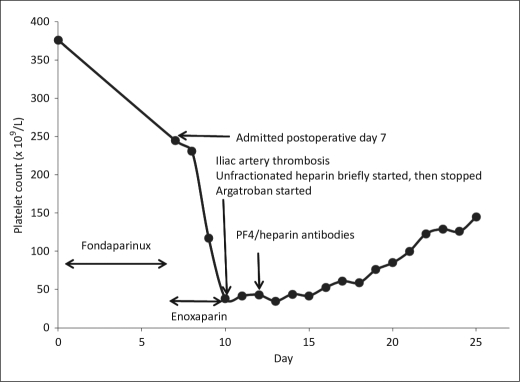
He was readmitted on postoperative day 7, while still taking fondaparinux, with nausea, vomiting, and abdominal pain. His platelet count was 240 × 109/L upon admission. A computed tomography (CT) scan of his abdomen and pelvis only showed findings of duodenal enteritis. He was placed on enoxaparin 40 mg subcutaneously daily at admission. His abdominal symptoms slowly improved; however, on hospital day 4, he developed acute right lower extremity pain and paralysis with physical exam findings consistent with acute right lower extremity ischemia. A UFH drip was started at this time and given for approximately 5 hours. A CT angiogram of the aorta confirmed complete occlusion of the right distal common iliac artery, as well as splenic and left renal infarcts. He underwent right common iliac embolectomy the same day. His platelet count, which had decreased to 117 × 109/L the day prior to the thrombotic event, had decreased to 38 × 109/L at the time of surgery (Figure 2).
Figure 2.
Clinical course of patient 2 with fondaparinux-associated heparin-induced thrombocytopenia.
Given his acute arterial thrombosis and decline in platelets, a strong clinical suspicion for HIT was maintained. His anti-PF4/heparin enzyme immunoassay was positive at an optical density of 3.081 units (normal value, <0.40), and this result was confirmed with high-dose heparin neutralization. All heparin was discontinued and alternate anticoagulation with argatroban was initiated. Over the next 2 weeks, his platelet count rose to normal levels. Warfarin was eventually started, and the patient was discharged home in good condition.
DISCUSSION
These cases demonstrate HIT associated with fondaparinux in two patients undergoing knee replacement. In each case, there was no documented use of heparin preoperatively or intraoperatively, without documentation of incidental exposure to UFH with arterial lines, central venous lines, or cell saver devices. Both patients initially had uneventful postoperative courses following knee replacement; however, both were readmitted to the hospital after discharge. In each case, acute thrombosis was documented with a rapid decline in platelet count, which improved with direct thrombin inhibitor therapy.
Fondaparinux has been shown to be associated with the formation of anti-PF4/heparin antibodies in postoperative orthopedic patients (3). These antibodies cannot be distinguished from those generated from LMWH. Other studies have shown that these anti-PF4/heparin antibodies fail to react against PF4 in the presence of fondaparinux, making a clinical syndrome of HIT associated with fondaparinux unlikely (11). However, a few other cases of HIT associated with fondaparinux have been reported. Warkentin et al reported a case similar to ours of a young woman developing fondaparinux-associated HIT after bilateral knee replacement. She developed bilateral adrenal hemorrhage with DVT on postoperative day 7, with her platelet count decreasing to 39 × 109/L (9).
Our cases bolster the observation that, on rare occasions, fondaparinux is associated with HIT. Each case had highly characteristic clinical findings for HIT, including bilateral adrenal hemorrhagic necrosis and inferior vena cava thrombosis in case 1 and acute lower extremity artery occlusion in case 2. Also, both patients demonstrated a drastic decline in platelet count after UFH or enoxaparin was initiated. Each case also demonstrated strongly positive assays for anti-PF4/heparin antibodies and normalization of platelet counts with direct thrombin inhibitor therapy.
These cases highlight two separate potential mechanisms for fondaparinux-induced HIT. The first case likely represents a more rare case of classic HIT related to fondaparinux. Thrombocytopenia and thrombosis developed during a 10-day course of fondaparinux treatment prior to hospitalization and any exposure to heparin. In the second case, however, the patient did receive three daily prophylactic doses of enoxaparin after admission, with platelet counts only decreasing after enoxaparin administration. It seems plausible that anti-PF4/heparin antibodies generated through previous exposure to fondaparinux resulted in a clinical syndrome of HIT. The rapidity of thrombocytopenia with thrombosis suggests an anamnestic response to preformed anti-PF4/heparin antibodies upon exposure to enoxaparin.
Finally, cases of “spontaneous HIT” have been reported, in which acute infectious/inflammatory events seem to generate platelet-activating anti-PF4/heparin antibodies (12, 13). Given the case reports associated with knee arthroplasty, it is unclear if the perioperative environment of inflammation resulting from this type of surgery might further potentiate generation of anti-PF4/heparin antibodies in conjunction with fondaparinux. These two cases highlight the complex nature of the pathophysiology of an important clinical syndrome, which seems to be associated with fondaparinux on rare occasions.
References
- 1.Warkentin TE, Kelton JG. Delayed-onset heparin-induced thrombocytopenia and thrombosis. Ann Intern Med. 2001;135(7):502–506. doi: 10.7326/0003-4819-135-7-200110020-00009. [DOI] [PubMed] [Google Scholar]
- 2.Prandoni P, Siragusa S, Girolami B, Fabris F, BELZONI Investigators Group The incidence of heparin-induced thrombocytopenia in medical patients treated with low-molecular-weight heparin: a prospective cohort study. Blood. 2005;106(9):3049–3054. doi: 10.1182/blood-2005-03-0912. [DOI] [PubMed] [Google Scholar]
- 3.Warkentin TE, Cook RJ, Marder VJ, Sheppard JA, Moore JC, Eriksson BI, Greinacher A, Kelton JG. Anti-platelet factor 4/heparin antibodies in orthopedic surgery patients receiving antithrombotic prophylaxis with fondaparinux or enoxaparin. Blood. 2005;106(12):3791–3796. doi: 10.1182/blood-2005-05-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turpie AG, Bauer KA, Eriksson BI, Lassen MR. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162(16):1833–1840. doi: 10.1001/archinte.162.16.1833. [DOI] [PubMed] [Google Scholar]
- 5.Büller HR, Davidson BL, Decousus H, Gallus A, Gent M, Piovella F, Prins MH, Raskob G, Segers AE, Cariou R, Leeuwenkamp O, Lensing AW, Matisse Investigators Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004;140(11):867–873. doi: 10.7326/0003-4819-140-11-200406010-00007. [DOI] [PubMed] [Google Scholar]
- 6.Büller HR, Davidson BL, Decousus H, Gallus A, Gent M, Piovella F, Prins MH, Raskob G, van den Berg-Segers AE, Cariou R, Leeuwenkamp O, Lensing AW, Matisse Investigators Subcutaneous fondaparinux versus intravenous unfractionated heparin in the initial treatment of pulmonary embolism. N Engl J Med. 2003;349(18):1695–1702. doi: 10.1056/NEJMoa035451. [DOI] [PubMed] [Google Scholar]
- 7.Kuo KH, Kovacs MJ. Fondaparinux: a potential new therapy for HIT. Hematology. 2005;10(4):271–275. doi: 10.1080/10245330500093492. [DOI] [PubMed] [Google Scholar]
- 8.Blackmer AB, Oertel MD, Valgus JM. Fondaparinux and the management of heparin-induced thrombocytopenia: the journey continues. Ann Pharmacother. 2009;43(10):1636–1646. doi: 10.1345/aph.1M136. [DOI] [PubMed] [Google Scholar]
- 9.Warkentin TE, Maurer BT, Aster RH. Heparin-induced thrombocytopenia associated with fondaparinux. N Engl J Med. 2007;356(25):2653–2655. doi: 10.1056/NEJMc070346. [DOI] [PubMed] [Google Scholar]
- 10.Rota E, Bazzan M, Fantino G. Fondaparinux-related thrombocytopenia in a previous low-molecular-weight heparin (LMWH)-induced heparin-induced thrombocytopenia (HIT) Thromb Haemost. 2008;99(4):779–781. doi: 10.1160/TH07-09-0573. [DOI] [PubMed] [Google Scholar]
- 11.Savi P, Chong BH, Greinacher A, Gruel Y, Kelton JG, Warkentin TE, Eichler P, Meuleman D, Petitou M, Herault JP, Cariou R, Herbert JM. Effect of fondaparinux on platelet activation in the presence of heparin-dependent antibodies: a blinded comparative multicenter study with unfractionated heparin. Blood. 2005;105(1):139–144. doi: 10.1182/blood-2004-05-2010. [DOI] [PubMed] [Google Scholar]
- 12.Warkentin TE, Makris M, Jay RM, Kelton JG. A spontaneous prothrombotic disorder resembling heparin-induced thrombocytopenia. Am J Med. 2008;121(7):632–636. doi: 10.1016/j.amjmed.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Pruthi RK, Daniels PR, Nambudiri GS, Warkentin TE. Heparin-induced thrombocytopenia (HIT) during postoperative warfarin thromboprophylaxis: a second example of postorthopedic surgery ‘spontaneous’ HIT. J Thromb Haemost. 2009;7(3):499–501. doi: 10.1111/j.1538-7836.2008.03263.x. [DOI] [PubMed] [Google Scholar]