Abstract
From 2004 to 2009, the number of malaria cases reported in Haiti increased nearly fivefold. The effect of the 2010 earthquake and its aftermath on malaria transmission in Haiti is not known. Imported malaria cases in the United States acquired in Haiti tripled from 2009 to 2010, likely reflecting both the increased number of travelers arriving from Haiti and the increased risk of acquiring malaria infection in Haiti. The demographics of travelers and the proportion of severe cases are similar to those statistics reported in previous years. Non-adherence to malaria chemoprophylaxis remains a nearly universal modifiable risk factor among these cases.
Malaria remains endemic in Haiti. Nearly all reported cases of malaria in Haiti are caused by Plasmodium falciparum, the species that is most likely to cause severe disease and is responsible for most malaria deaths globally.1 Fewer than 5% of cases are caused by P. malariae, a species that usually causes milder infections.2 Currently, P. falciparum infections acquired in Haiti remain responsive to chloroquine therapy, despite reports of molecular markers among a small number of P. falciparum isolates that are associated with chloroquine resistance.3 The effect of the 7.0-magnitude earthquake on January 12, 2010 on malaria transmission is still not known, but there had already been an increase in the number of confirmed malaria cases reported in Haiti from 10,802 in 2004 to 49,535 in 2009.4 Surveillance data for 2010 are not yet available. The primary malaria vector in Haiti is Anopheles albimanus, which prefers to bite outdoors.5 Given the increased exposure to mosquitoes of displaced persons living in temporary shelters and the disruptions in health services after the earthquake, it is likely that the number of reported malaria cases in 2010 will be higher than in 2009. Additionally, the number of aid workers present in Haiti dramatically increased after the earthquake, increasing the number of persons with mosquito exposures and importation of malaria to non-endemic countries.6 In February of 2010, a report of 11 malaria cases diagnosed and treated in the United States but acquired in Haiti in the month after the earthquake was issued to remind US travelers to Haiti to comply with chemoprophylaxis guidelines and use other mosquito avoidance measures to prevent malaria infection.7 This report summarizes currently available data on all reported imported malaria cases in the United States acquired in Haiti in recent years.
Thirty-four cases of P. falciparum malaria acquired in Haiti were reported to the US Centers for Disease Control and Prevention (CDC) through the National Malaria Surveillance System (NMSS) in 2007; 19 cases were reported in 2008, and 58 cases were reported in 2009. In 2010, the NMSS captured 170 cases of malaria acquired in Haiti (Figure 1). The average age of the 170 travelers who acquired malaria in Haiti in 2010 was 42 years: the youngest was a 2-year-old Haitian adoptee and the oldest was a 92-year-old aid worker. The average duration of time in Haiti for the 131 US resident malaria case-patients in 2010 was 32 days (range = 2–240 days).
Figure 1.
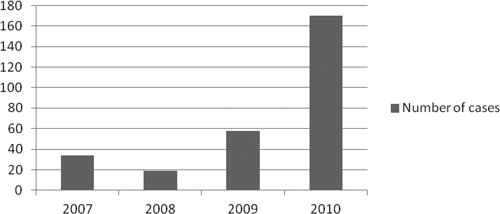
The number of imported malaria cases in the U.S. acquired in Haiti from 2007–2010.
Of the 170 cases, 131 cases were US residents, and at least 27 (16%) of these case-patients visited Haiti as aid workers. Eighty-nine (52%) were visiting friends and relatives (VFRs), two (1%) were business travelers, and thirteen (8%) had unknown reasons for travel. Thirty-two (19%) of the case-patients were Haitian residents visiting the United States, one-half of whom were refugees. Of the remaining seven case-patients, three were residents of countries other than the United States or Haiti, and four had unknown residency status. Compared with 2009, the proportion of cases that were aid workers who acquired malaria in Haiti has increased from 9% to 16%. However, the proportion of imported cases among Haitian residents and VFRs is similar: 73% in 2009 and 71% in 2010.
Of the 170 cases reported to NMSS, the 32 residents of Haiti would not have been expected to take malaria prophylaxis. Among the 131 known US resident case-patients, only 4 (3%) reported adherence to a recommended malaria prophylaxis regimen in accordance with CDC guidelines. The remaining case-patients either did not take prophylaxis at all (N = 113) or did not take it properly (N = 11; i.e., skipped doses or prematurely stopped chemoprophylaxis). Adherence data are missing for three cases. The prescribed medication is known for 13 of 18 US resident case-patients who reported taking chemoprophylaxis. Ten were prescribed daily doxycycline (77%), and three were prescribed weekly chloroquine (23%). Of the four patients who adhered to their chemoprophylaxis regimen, two reported taking doxycycline, and two reported taking chloroquine. Similarly, in 2009, only three (5%) of the US resident case-patients who acquired malaria in Haiti reported taking malaria prophylaxis, all with chloroquine. Two of these three patients reported full adherence, and one patient had unknown adherence. In 2007 and 2008, no US resident case-patients who acquired malaria in Haiti reported taking chemoprophylaxis.
Twenty-six (15%) cases of malaria acquired in Haiti in 2010 were considered severe malaria because of either high-density parasitemia (> 5% of red blood cells parasitized) or other complications. The most common complications among those patients with severe disease were acute respiratory distress syndrome (N = 8), renal insufficiency (N = 8), and cerebral malaria (N = 7). Only 11 (42%) of these patients received parenteral therapy (7 with intravenous [IV] quinidine and 4 with IV artesunate), although any case classified as severe should have received parenteral treatment.8 Fortunately, the remaining cases responded to oral antimalarial therapy. Among these 26 severely ill case-patients, there were 13 (50%) US resident VFR travelers, 6 (23%) Haitians visiting the United States, 4 (19%) aid workers, 1 (4%) business traveler, and 2 (8%) with unknown reasons for travel. Similarly, in 2009, 9 (15%) of 58 cases of malaria acquired in Haiti were classified as severe, and at least 7 of these cases (78%) were VFRs or Haitian residents. The proportion of severe cases in 2008 (N = 2) and 2007 (N = 6) were comparable (10% and 18%, respectively). There have been no reported fatalities from malaria in travelers from Haiti in the last 4 years.
Because Haiti borders the Dominican Republic (D.R.) on the island of Hispaniola, malaria trends in the D.R. and imported cases to the United States are described here for comparison. Confirmed malaria cases in the D.R. have decreased from 2,353 cases in 2004 to 1,643 cases in 2009.4 Surveillance data from 2010 are not yet available. Eleven cases of malaria imported to the United States from the D.R. were reported in 2007, zero cases were reported in 2008, and four cases were reported in 2009. In 2010, the number of imported cases of malaria from the D.R. remained low, with only six uncomplicated cases reported.
The number of malaria cases reported through national surveillance systems in Haiti increased from 2004 to 2009, and this trend is expected to continue in 2010. Before the earthquake, lack of funding and limited personnel prevented the Haitian Ministry of Public Health and Population from implementing malaria control measures and likely contributed to the increase in reported cases of malaria since 2004. Since the January of 2010 earthquake, improved surveillance and testing methods, increased exposure of displaced populations because of inadequate shelter, changes in access to healthcare, and increased mosquito breeding areas because of environmental destruction may all contribute to greater numbers of reported malaria cases. The fact that similar increases are not being reported from the D.R. suggests that inadequate shelter, environmental factors, and poor public health infrastructure may, indeed, be accountable for the rise of malaria infections in Haiti rather than ecological factors, such as increased rainfall or changes in vector populations.
The number of cases of imported malaria from Haiti dramatically increased in 2010 compared with 2007–2009. This increase may be attributable to a greater number of travelers visiting Haiti from the United States or an increased risk of acquiring malaria associated with travel to Haiti. Although the proportion of imported malaria case-patients who were aid workers acquiring malaria in Haiti increased in 2010, the majority of imported cases remained among VFRs and Haitian residents visiting the United States. Additionally, the proportion of severe cases remains similar to previous years and occurred mostly in VFRs and Haitian residents, suggesting that visitors should not expect acquired immunity to prevent severe illness.
Non-compliance with malaria chemoprophylaxis remains a modifiable risk factor shared by nearly all US residents who acquired malaria in Haiti from 2007 to 2010. It is likely that the increased number of aid workers visiting Haiti in 2010 contributed to the increase in imported malaria cases, given that they probably worked outdoors in internally displaced persons (IDP) camps and thus, were more likely to be exposed to mosquitoes. US resident VFRs continue to experience severe malaria and should be counseled to take malaria chemoprophylaxis when visiting Haiti. Malaria chemoprophylaxis is highly effective at preventing malaria, but no regimen provides complete protection. Therefore, mosquito avoidance measures are also recommended.
This report emphasizes that the risk of acquiring malaria in Haiti is substantial, and all US residents visiting Haiti should comply with an appropriate malaria chemoprophylaxis regimen. Clinicians should note that all cases of severe malaria in the United States should be treated with IV quinidine or IV artesunate. All travelers to Haiti should consult a travel medicine physician or other experienced healthcare professional for advice regarding immunizations, malaria chemoprophylaxis, and mosquito avoidance measures before visiting Haiti. Travelers and healthcare providers can also find up to date information about CDC recommendations for travelers at www.cdc.gov/travel.
Footnotes
Authors' addresses: Aarti Agarwal, Meredith McMorrow, and Paul M. Arguin, Division of Parasitic Diseases and Malaria, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, GA, E-mails: iyj8@cdc.gov, bwe3@cdc.gov, and pma0@cdc.gov.
References
- 1.World Health Organization Malaria Fact Sheet No. 94. 2010. http://www.who.int/mediacentre/factsheets/fs094/en/index.html Available at. Accessed May 6, 2011.
- 2.Lindo JF, Bryce JH, Ducasse MB, Howitt C, Barrett DM, Lorenzo Morales J, Ord R, Burke M, Chiodini PL, Sutherland CJ. Plasmodium malariae in Haitian refugees, Jamaica. Emerg Infect Dis. 2007;13:931–933. doi: 10.3201/eid1306.061227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Londono BL, Eisele TP, Keating J, Bennett A, Chattopadhyay C, Heyliger G, Mack B, Rawson I, Vely JF, Désinor O, Krogstad DJ. Chloroquine-resistant haplotype Plasmodium falciparum parasites, Haiti. Emerg Infect Dis. 2009;15:735–740. doi: 10.3201/eid1505.081063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pan American Health Organization Malaria Surveillance Indicators. 2010. http://ais.paho.org/phip/viz/malaria_surv_indicators_popup.asp Available at. Accessed September 26, 2011.
- 5.PAHO-Pan American Health Organization . Biology and Ecology of Anopheles albimanus Wiedemann in Central America, Technical Paper 43. Washington, DC: Pan American Health Organization; 1996. [Google Scholar]
- 6.Romo R. Responding to a Crisis: The Harsh Realities for Aid Workers in Haiti. 2010. http://www.cnn.com/2010/HEALTH/01/29/haiti.relief.workers/index.html?iref=allsearch CNN. Available at. [Google Scholar]
- 7.Centers for Disease Control and Prevention Malaria acquired in Haiti—2010. MMWR Morb Mortal Wkly Rep. 2010;59:217–219. [PubMed] [Google Scholar]
- 8.Griffith KS, Lewis LS, Mali S, Parise ME. Treatment of malaria in the United States. JAMA. 2007;297:2264–2277. doi: 10.1001/jama.297.20.2264. [DOI] [PubMed] [Google Scholar]


