Abstract
All diseases diagnosed in a primary healthcare clinic situated in Leogane, Haiti, were recorded prospectively during a 7-month period. Among the patients in this cohort, 2,821 of 6,631 (42.6%) presented with an infectious disease. The three most common syndromes among the patients presenting with infections were respiratory tract infections (33.5%), suspected sexually transmitted diseases—mostly among females with recurrent disease (18.1%)—and skin and soft tissue infections, including multiple cases of tinea capitis (12.8%). Of the 255 patients presenting with undifferentiated fever, 76 (29.8%) were diagnosed with falciparum malaria. Other vector-borne diseases included 13 cases of filariasis and 6 cases of dengue fever. Human immunodeficiency virus infection was diagnosed in 19 patients. Four cases of mumps were detected among unimmunized children. A large proportion of these infections are preventable. Concerted efforts should be made to create large-scale preventive medicine programs for various infectious diseases.
Introduction
In January of 2010, Haiti was devastated by an earthquake, the epicenter of which lay close to the town of Leogane, situated in the Ouest (West) Province of Haiti. Most of the town's buildings were destroyed, and vast tent encampments were created. The only functioning hospital was badly damaged. Subsequently, in November of 2010, the town suffered widespread flooding after Hurricane Tomas. More than 1 year after the earthquake, thousands of people are still living in crowded tent encampments in and surrounding Leogane. Electricity has not been restored, the roads and communication systems are still badly damaged, and a clean water supply is not yet available to all. The provision of healthcare to Haitians in this resource-limited environment depends heavily on multiple aid agencies, and even basic primary care is not readily accessible. This reality influenced the decision of an Israeli non-governmental organization to set up a primary healthcare clinic in Leogane rather than in the capital, where multiple aid organizations are already operating.
Harsh living conditions in improvised tent townships in the Leogane area may favor the spread of infections, such as the cholera epidemic that has been ravaging Haiti for more than 1 year. Similar rises in infectious conditions have been shown to follow major disasters.1 The aim of this article is to summarize our observation of infectious diseases commonly seen in this primary care setting in Haiti in the post-earthquake era.
Methods
The study was conducted in a newly established primary healthcare clinic in the West (Ouest) Province of Haiti. The clinic is situated in Leogane—a town with an estimated population of 200,000 situated 30 km west of Port-au-Prince. The clinic, staffed by nurses and doctors from Israel, Canada, and Haiti, has been operating on a daily basis since November of 2010. Treatment and medications were provided to patients free of charge for the first 100 days. Thereafter, a fee equivalent to $1 US per visit was instituted. This fee covered consultations, laboratory tests, and all medications. All patients were from the town itself or its immediate vicinity, and they sought medical advice without a medical referral.
Other medical facilities in Leogane included a field hospital set up by Médecins Sans Frontières (MSF), which treated mainly inpatients, and Saint Croix Hospital, which was severely damaged during the earthquake and again during the 2010 hurricane. Most laboratory tests were not available in any of the medical facilities in Leogane, and patients were often referred to Port-au-Prince. In Leogane itself, there were no other non-profit primary care clinics.
The clinic is outfitted with basic primary care equipment and rapid diagnostic tests (RDTs) for common infectious diseases. Malaria was diagnosed with the use of an RDT for detection of histidine-rich protein II (Paracheck Rapid Test; Orchid Biomedical Systems, Goa, India) in all patients with a history of compatible febrile illness. Dengue fever was diagnosed with the use of a rapid serologic test (Dengue IgG/IgM Cassette; Atlas Link Biotech Co., Beijing, China) in patients with undifferentiated fever. Additional laboratory or radiologic tests were not available routinely. Respiratory and gastrointestinal infections were diagnosed clinically. The diagnosis of probable sexually transmitted disease (STD) was based on a combination of compatible symptoms and signs and a recent history of unprotected sexual intercourse. STDs that were confirmed by RDTs included syphilis (Anti-Syphilis Serum Strip; Atlas Link Biotech Co., Beijing, China), and human immunodeficiency virus infection (HIV; anti-HIV 1/2 Cassette; Atlas Link Biotech Co., Beijing, China). Skin and soft tissue infections were diagnosed clinically, but a dermatologist was consulted online in case of diagnostic dilemmas. Demographic and clinical data on all patients were recorded prospectively.
Results
Over a period of 7 months (from November 1, 2010 to the end of May of 2011), 6,631 patients were treated in the clinic. The number of consultations per month is shown in Figure 1. Females constituted 69.2% of all patients. The mean age of patients was 28.2 ± 21.1 years; 2,142 patients (32%) were less than 18 years old.
Figure 1.
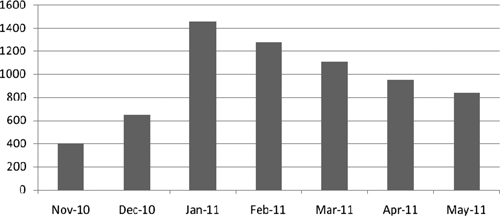
Frequency of all consultations according to months (N = 6,631) from November of 2010 to May of 2011. *The clinic was shut down for a few days in November of 2010 because of a hurricane and December of 2010 because of political unrest. An admission fee was introduced in February of 2011.
Among the patients in this cohort, 2,821 patients (42.6% of all patients) presented with an infectious disease. In addition to infections, patients sought medical advice mainly for gastrointestinal diseases (12.9%), cardiovascular problems (9.1%), pain syndromes (8.4%), and obstetric issues (5.6%) (Table 1).
Table 1.
Diseases by categories and age
| Disease category | Number of patients | Percent of all cases (%) | Average age ± standard deviation |
|---|---|---|---|
| Total | 6,631 | 100 | 28.2 ± 21.1 |
| Infectious diseases | 2,821 | 42.6 | 21.7 ± 15.4 |
| General | 913 | 13.8 | 25.2 ± 19.2 |
| Gastrointestinal diseases | 859 | 12.9 | 18.2 ± 18.0 |
| Cardiology | 603 | 9.1 | 57.7 ± 15.1 |
| Pain syndromes | 560 | 8.4 | 28.2 ± 21.2 |
| Obstetric/gynecologic conditions | 371 | 5.6 | 18.6 ± 15.1 |
| Dermatology | 163 | 2.5 | 18.6 ± 17.9 |
| Respiratory diseases | 97 | 1.5 | 27.2 ± 19.3 |
| Endocrinology | 86 | 1.3 | 50.6 ± 12.4 |
| Trauma and surgery | 100 | 1.5 | 28.9 ± 19.3 |
| Psychiatric conditions | 31 | 0.5 | 31.2 ± 11.3 |
| Neurologic conditions | 27 | 0.4 | 33.3 ± 19.1 |
Primary healthcare clinic, Leogane, Haiti.
Among the 2,821 patients with infections, the three most common syndromes included upper respiratory tract infections, suspected STDs, and skin and soft tissue infections (Figure 2).
Figure 2.
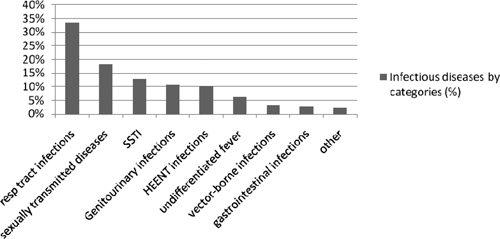
Infectious diseases of 2,821 patients by categories in the primary healthcare clinic, Leogane, Haiti. HEENT = head, eyes, ears, nose, and throat infections; Resp = respiratory; SSTI = skin and soft tissue infections.
Upper respiratory tract infections accounted for 30.7% of all infections. Most were considered viral in origin and were not treated with antimicrobials agents. Lower respiratory tract infections accounted for an additional 2.8% of all infections.
Probable STDs were diagnosed in 510 patients, accounting for 18.1% of all patients with infectious diseases. The majority of patients with probable STDs were female (475/510, 93%), with an average age of 26.7 ± 9.3 years. Most of these women had recurrent disease and had not been treated before concurrently with their sexual partners. Several women presented with STDs after they had been sexually assaulted.
Overall, 360 patients had skin and soft tissue infections (SSTIs), including tinea capitis and corporis (226 patients), bacterial skin infections such as cellulitis and impetigo (60 patients), skin and soft tissue abscesses (26 patients), fungal (20 patients), and other infections (28 patients). The majority of the patients with SSTIs were younger than 18 years old (225/360, 62.5%). Of note is the large number of patients with tinea capitis, many of whom are children living in the same orphanage.
A more detailed description of the epidemiological and clinical manifestations of the patients diagnosed with malaria in our clinic has been published elsewhere.2 During the study period, 255 patients presented with undifferentiated fever. Of these patients, 76 (29.8%) were diagnosed with falciparum malaria. Most patients with malaria were Haitians (73/76 patients); three additional cases of malaria were diagnosed in aid workers who had not taken the recommended chemoprophylaxis. No cases were diagnosed among aid workers who had been taking chloroquine prophylaxis. A thorough investigation showed that all cases of malaria were contracted in Leogane or its immediate vicinity. Malaria epidemiology seems to be seasonal, with the peak number of cases occurring from November to January and declining thereafter (Figure 3).
Figure 3.
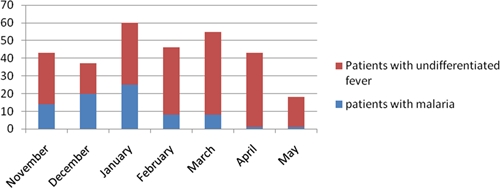
Number of patients with malaria and undifferentiated fever in Leogane, Haiti from November of 2010 to May of 2011.
Although on presentation, only 48 (63%) had a fever higher than 37.5°C, all malaria patients reported a febrile disease. Nearly all patients (74) were treated with chloroquine. Three patients (3.9%) presented for severe malaria. Two of these patients were transferred to a referral hospital; one aid worker with non-cardiogenic pulmonary edema was evacuated to the United States. Of note is the difficulty in obtaining medications for severe malaria through the publicly run pharmacies in Port-au-Prince.
Dengue fever was diagnosed in three Haitian patients and three foreign visitors. No cases of severe dengue were encountered. The diagnosis of dengue fever was made with an RDT for the detection of immunoglobulin (Ig) M and IgG antibodies. Because this test is likely to be falsely negative during the early phase of the disease, it was not performed in patients presenting with a fever lasting a few days only.
Thirteen patients were diagnosed clinically as having lymphatic filariasis. None of them had been treated for filariasis before. In a recent survey conducted over a 1-month period in our clinic, 96 adult males who attended the clinic for various reasons (not including suspected filariasis) were clinically screened, and five cases of hydrocele were found (5.2%), probably resulting from undiagnosed lymphatic filariasis (Schwartz E and others, unpublished data). The average age of the screened population was 31 years (range = 3–70 years).
Somewhat unexpectedly, only 80 patients presented with gastrointestinal infections. The majority of these patients (47/80, 58.7%) had a probable helminthic infection. Patients reported expulsion of worms in stool or through the mouth or nose, but laboratory confirmation was not available. Acute diarrheal illness occurred in 25 patients. Diarrhea, mostly chronic and without additional symptoms or signs, was noted in 92 more patients. These cases were not listed as infectious in origin. Despite the fact that a cholera outbreak is ongoing in Haiti, only three patients with suspected cholera presented to the clinic. These cases were referred to a Cholera Treatment Center set up by the Médecins Sans Frontières organization.
Tuberculosis was diagnosed in four patients, and HIV infection was diagnosed in 19 additional patients.
There was a cluster of four cases of children with mumps. All children lived in the same area of Leogane. Three of the children were unimmunized, whereas the vaccination status of one child was unclear. No cases of acute flaccid paralysis, human rabies, or suspected measles were found.
Discussion
Haiti was known to be the poorest nation in the Western Hemisphere even before the 2010 earthquake, and its healthcare system is the weakest in the region. In 2009, the British Foreign and Commonwealth Office estimated that the life expectancy in Haiti was 50.8 years for males and 52.4 years for females—far below the expectancy rates of any other country in the region.3 Haiti was a hot spot for vector-borne diseases like Plasmodium falciparum malaria and filariasis—diseases that had long been controlled outside the island of Hispaniola.4,5 The prevalence of human rabies was higher than in any other country of the Americas.6
Whether a change in the medical situation in Haiti has occurred in the post-earthquake era is hard to assess. This difficulty stems mainly from insufficient pre-earthquake epidemiological data. In addition, making accurate diagnoses is not always possible because of the lack of proper laboratory facilities. Furthermore, our clinic functions with limited laboratory resources. Diagnoses are based mainly on rapid diagnostic tests or a syndromic approach. Rapid diagnostic tests offer practical advantages. Namely, they do not require refrigeration and regular electricity, which is not available in Leogane and throughout much of Haiti. Despite these limitations, our findings offer some initial insights into the epidemiology of infectious diseases seen in a primary care clinic in Haiti.
Respiratory tract infections.
Respiratory tract infections were the most common infections diagnosed in our clinic. These findings are essentially identical to the findings reported by the National Sentinel Site Surveillance (NSSS) System that was launched in Haiti immediately after the earthquake.7 In the NSSS report published in 2010, acute respiratory infections accounted for 16.3% of all reportable conditions and 30.8% of all infections. A high incidence of respiratory tract infections after major disasters has been reported in the past, both in Haiti and elsewhere.8–11 A high incidence of respiratory tract infections more than 1 year after the earthquake can likely be explained by overcrowding in refugee camps.
STDs.
No mention was made of patients with STDs in the NSSS report.7 This report stands in sharp contrast to the data collected in our clinic, where 18.1% of all patients with infections presented with probable STDs. The diagnosis of probable STDs was made with a syndromic approach, albeit without laboratory confirmation because of the economic limitations imposed by the operation of a primary healthcare clinic run by volunteers. Rapid diagnostic tests that can be useful in such circumstances are lacking aside from RDTs for syphilis and HIV.
Even if there is some overdiagnosis of STDs because of the lack of laboratory confirmation, we argue that STDs are common in Haiti. Indeed, previous studies have shown that the prevalence of STDs among women of lower economic status reaches 40.1–47%.12,13
The low number of males presenting with STDs might be explained by economic limitations (e.g., difficulty in obtaining a day off work for visiting the clinic), cultural issues, and also, some overdiagnosis of STDs in females.
Most patients with probable STDs in our clinic were young females, many with recurrent disease. Few of these patients had been treated concomitantly with their sexual partners in the past. A national program concentrating on prevention of STDs and treatment of patients and their sexual partners is warranted. In addition, the diagnosis of STDs in rape victims highlights the importance of protecting vulnerable populations in Haiti.14
Vector-borne diseases.
It is possible that the breakdown of the infrastructure in the Leogane area after the earthquake and the flooding that followed Hurricane Tomas in 2010 caused an increase in the different vectors' breeding sites.
Malaria is the most common vector-borne disease seen in our clinic. We have recently published an article on malaria in Leogane.2 Although P. falciparum malaria is endemic in Haiti, epidemiological data from Haiti are scarce. Before the 2010 earthquake, the World Health Organization estimated the risk of malaria in most parts of Haiti to be low.15 We could not calculate the malaria incidence in the Leogane area, but the fact that malaria accounts for approximately 30% of all undifferentiated fever cases is alarming. It is unknown whether this finding holds true for other areas of Haiti as well. It is also unclear whether the high malaria incidence among febrile patients was underreported in the past or whether it is related to the deteriorating infrastructure of the area after the 2010 earthquake and Hurricane Tomas. The risk of malaria does not seem to be evenly distributed throughout the year. Most cases of malaria occurred between November and January, and nearly no cases were diagnosed in April and May (Figure 3). This observation is similar to previous reports.16 Severe malaria occurred in three patients (3.9%); two cases were diagnosed in Haitian children, and one case was an American aid worker. Parenteral chloroquine, quinine, and quinidine are not readily available in Haiti, and only donations of parenteral arthemether helped in the management of these patients. Visitors and aid workers would do well to use chemoprophylaxis according to existing guidelines,17 and indeed, no cases of malaria were diagnosed among aid workers in our organization who used chloroquine chemoprophylaxis.2
Only three Haitian patients were diagnosed with dengue fever. Three additional cases were identified in foreigners. Because all serotypes of the virus are endemic in Haiti and because the recently published seroprevalence of dengue in Haiti is high,18 it is likely that this finding represents a gross underestimation. Several explanations can be provided for the seemingly low occurrence of dengue fever. First, because the rash typically appears several days after the onset of fever, it is likely that many patients presenting with a systemic febrile illness were not suspected of having dengue fever. Second, because diagnosis of dengue fever was made with an RDT for the detection of IgM and IgG antibodies, it is likely that patients had initial false-negative results in the early phase of the disease. Getting patients to return to the clinic for additional testing when they are already recovering from their febrile illness is difficult. The high number of undiagnosed cases of undifferentiated fever occurring in the rainy season (Figure 3) may at least partly reflect undiagnosed cases of dengue fever and other vector-borne diseases. Third, the high seroprevalence of dengue fever in a recent survey might indicate that large parts of the local population are immune to dengue.18,19
One of the most important vector-borne diseases in Haiti is lymphatic filariasis caused by Wuchereria bancrofti. Although filariasis is a non-febrile and non–life-threatening disease, it is highly debilitating. Leogane is known to be an endemic area of filariasis.20 In our cohort, 13 patients were diagnosed with lymphatic filariasis, and none of them was previously diagnosed or treated. It is likely that, despite tremendous efforts to diagnose and treat the disease,21 many patients still remain untreated. Indeed, in a recent survey that was conducted in our clinic, five cases of hydrocele were found among 96 (5.2%) male patients who attended the clinic for various reasons (Schwartz E and others, unpublished data). This finding may reflect ongoing transmission.
Significant efforts to control the disease in Haiti were made in the pre-earthquake era.21 Our survey, albeit on a small scale, suggests that the breakdown of the infrastructure in the Leogane area after the 2010 earthquake and the flooding that followed Hurricane Tomas later in 2010 may have caused an increase in the vector's breeding sites.
Infections of the gastrointestinal tract.
The low number of patients presenting with gastrointestinal infections was unexpected. A Cholera Treatment Center (CTC) is operated by the MSF organization in Leogane. During a cholera outbreak, a clinical case definition, rather than laboratory confirmation, was recommended by the World Health Organization for the diagnosis of patients with cholera.22 Any patient over the age of 5 years who developed acute watery diarrhea was considered to have cholera according to these recommendations. Thus, it is likely that most patients with acute diarrheal syndromes were directly referred to the CTC, independent of whether they had cholera or not.
The classic presentation of typhoid fever is prolonged fever and severe abdominal symptoms, such as gastrointestinal hemorrhage or perforation apparent in the second or third week of the disease. The definite diagnosis of typhoid fever is based on blood (or stool) cultures, which were not available in our clinic or any other medical facility in Leogane and its vicinity. However, during the study period, no patients fitting this description were noted.
Helminthic infections were diagnosed only when the patient reported expulsion of a worm from either the anus or the mouth and nose. Thus, it is likely that our data represents a gross underestimation of the true incidence of such infections. Treatment with albendazole was provided to all patients at the clinic, regardless of diagnosis.
SSTIs.
Considering the living conditions and overcrowding in the various encampments as well as the Haitian tropical weather, the large number of patients with fungal and bacterial SSTIs was not unexpected. The large proportion of children among the patients with SSTI was also expected. Of note was a large proportion of patients with tinea capitis—typically, several children living in the same orphanage and treated only with topical antifungal therapy if at all. Systemic antifungal agents like fluconazole or grisofulvin, which are needed for the treatment of this condition, were only occasionally available through the publicly operated pharmacies in Port-au-Prince.
In conclusion, infections are the most common reason for patients to seek primary medical care in Leogane, Haiti, in the post-earthquake era. A large proportion of these infections are preventable by relatively simple measures. Infections of the respiratory tract are the most common conditions, possibly because of overcrowding in tent encampments. STDs were also very common, especially in young women who had never been treated concurrently with their partners and had recurrent episodes of STDs. Other important findings were the high proportion of patients with malaria among patients with undifferentiated fever, the multiple cases of filariasis, the relatively low number of dengue fever cases, the occurrence of vaccine-preventable diseases such as mumps, and the frequent diagnosis of tinea capitis, mainly in young children from lower socioeconomic status. Important medications, such as systemic antifungal drugs or intravenous therapy for severe malaria, were difficult to acquire in Haiti. Concerted efforts should be made to increase the availability of these medications.
Haiti needs an efficient, high-quality primary care system that is available to all; the data presented in this report may help create such a system. Along with strengthening the primary care system, concerted efforts should be made to create large-scale preventive medicine programs for various infectious diseases. The data collected in this study can be used when plans are drawn for setting up primary care clinics in post-earthquake Haiti.
ACKNOWLEDGMENTS
The authors thank all IsraAid clinic staff for their work, Dr. Ben Naafs for his online dermatologic consultations, and Dr. Belina Neuberger for her valuable editing remarks.
Footnotes
Authors' addresses: Ami Neuberger, IsraAid Primary Health Clinic, Leogane, Haiti and Unit of Infectious Diseases, Rambam Medical Center, Haifa, Israel, E-mail: a_neuberger@rambam.health.gov.il. Shiri Tenenboim and Eli Schwartz, IsraAid Primary Health Clinic, Leogane, Haiti and Center for Geographic Medicine and Tropical Diseases, Sheba Medical Center, Tel Hashomer and Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel, E-mails: shirite@gmail.com and Eli.schwartz@sheba.health.gov.il. Miri Golos, IsraAid Primary Health Clinic, Leogane, Haiti and Departments of Internal Medicine A and C, Sheba Medical Center, Tel Hashomer and Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel, E-mail: mirigolos@gmail.com. Racheli Pex and Spencer Vernet, IsraAid Primary Health Clinic, Leogane, Haiti, E-mails: pex.racheli@gmail.com and spenloveminouch@yahoo.fr. Yonah Krakowsky, Division of Urology, University of Toronto, Toronto, Canada, E-mail: yonahk@gmail.com. Marnina Urman, IsraAid Primary Health Clinic, Leogane, Haiti and Department of Obstetrics and Gynecology, Shaare Zedek Medical Center, Hebrew University Medical School, Jerusalem, Israel, E-mail: marnina@gmail.com.
References
- 1.Brennan RJ, Waldman RJ. The south Asian earthquake six months later—an ongoing crisis. N Engl J Med. 2006;354:1769–1771. doi: 10.1056/NEJMp068017. [DOI] [PubMed] [Google Scholar]
- 2.Neuberger A, Zaulan O, Tenenboim S, Vernet S, Pex R, Held K, Urman M, Garpenfeldt K, Schwartz E. Malaria among patients and aid workers consulting a primary healthcare centre in Leogane, Haiti, November 2010 to February 2011—a prospective observational study. Euro Surveill. 2011;16:19829. [PubMed] [Google Scholar]
- 3.United Kingdom Foreign and Commonwealth Office Country Profile, Haiti. 2009. http://www.fco.gov.uk/en/travel-and-living-abroad/travel-advice-by-country/country-profile/north-central-america/haiti?profile=all Available at. Accessed June 22, 2011.
- 4.Schneider MC, Aguilera XP, Barbosa da Silva Junior J, Ault SK, Najera P, Martinez J, Requejo R, Nicholls RS, Yadon Z, Silva JC, Leanes LF, Periago MR. Elimination of neglected diseases in Latin America and the Caribbean: a mapping of selected diseases. PLoS Negl Trop Dis. 2011;5:e964. doi: 10.1371/journal.pntd.0000964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Malaria—Great Exuma, Bahamas, May–June 2006. MMWR Morb Mortal Wkly Rep. 2006;55:1013–1016. [PubMed] [Google Scholar]
- 6.Schneider MC, Belotto A, Adé MP, Hendrickx S, Leanes LF, Rodrigues MJ, Medina G, Correa E. Current status of human rabies transmitted by dogs in Latin America. Cad Saude Publica. 2007;23:2049–2063. doi: 10.1590/s0102-311x2007000900013. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Launching a national surveillance system after an earthquake—Haiti, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:933–938. [PubMed] [Google Scholar]
- 8.Pan American Health Organization Haiti Health Cluster Bulletins—Earthquake, January 2010: Update, February 11, 2010. 2010. http://new.paho.org/disasters/index.php?option=com_content&task=view&id=1108&Itemid=1 Available at. Accessed June 15, 2011.
- 9.Robinson B, Alatas MF, Robertson A, Steer H. Natural disasters and the lung. Respirology. 2011;16:386–395. doi: 10.1111/j.1440-1843.2011.01923.x. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization Epidemic-prone disease surveillance and response after the tsunami in Aceh Province, Indonesia. Wkly Epidemiol Rec. 2005;80:160–164. [PubMed] [Google Scholar]
- 11.Lim JH, Yoon D, Jung G, Joo KW, Lee HC. Medical needs of tsunami disaster refugee camps. Fam Med. 2005;37:422–428. [PubMed] [Google Scholar]
- 12.Fitzgerald DW, Behets F, Caliendo A, Roberfroid D, Lucet C, Fitzgerald JW, Kuykens L. Economic hardship and sexually transmitted diseases in Haiti's rural Artibonite valley. Am J Trop Med Hyg. 2000;62:496–501. doi: 10.4269/ajtmh.2000.62.496. [DOI] [PubMed] [Google Scholar]
- 13.Behets FM, Desormeaux J, Joseph D, Adrien M, Coicou G, Dallabetta G, Hamilton HA, Moeng S, Davis H, Cohen MS. Control of sexually transmitted diseases in Haiti: results and implications of a baseline study among pregnant women living in Cité Soleil Shantytowns. J Infect Dis. 1995;172:764–771. doi: 10.1093/infdis/172.3.764. [DOI] [PubMed] [Google Scholar]
- 14.Kolbe AR, Hutson RA, Shannon H, Trzcinski E, Miles B, Levitz N, Puccio M, James L, Noel JR, Muggah R. Mortality, crime and access to basic needs before and after the Haiti earthquake: a random survey of Port-au-Prince households. Med Confl Surviv. 2010;26:281–297. doi: 10.1080/13623699.2010.535279. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Information Resource Centre Communicable Diseases. International Travel and Health. Country List: Vaccination Requirements and Malaria Situation. 2005. http://whqlibdoc.who.int/publications/2005/9241580364_country_list.pdf Available at. Accessed June 23, 2011.
- 16.Eisele TP, Keating J, Bennett A, Londono B, Johnson D, Lafontant C, Kroqstad DJ. Prevalence of Plasmodium falciparum infection in rainy season, Artibonite Valley, Haiti. Emerg Infect Dis. 2007;13:1494–1496. doi: 10.3201/eid1310.070567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Center for Disease Control and Prevention Health Information to Travelers to Haiti. 2010. http://wwwnc.cdc.gov/travel/destinations/haiti.htm Available at. Accessed June 23, 2011.
- 18.Rioth M, Beauharnais CA, Noel F, Ikizler MR, Mehta S, Zhu Y, Long CA, Pape JW, Wright PF. Serologic imprint of dengue virus in urban Haiti: characterization of humoral immunity to dengue in infants and young children. Am J Trop Med Hyg. 2011;84:630–636. doi: 10.4269/ajtmh.2011.10-0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Halstead SB, Streit TG, Lafontant JG, Putvatana R, Russell K, Sun W, Kanesa-Thasan N, Hayes CG, Watts DM. Haiti: absence of dengue hemorrhagic fever despite hyperendemic dengue virus transmission. Am J Trop Med Hyg. 2001;65:180–183. doi: 10.4269/ajtmh.2001.65.180. [DOI] [PubMed] [Google Scholar]
- 20.Beau de Rochars MV, Milord MD, St Jean Y, Désormeaux AM, Dorvil JJ, Lafontant JG, Addiss DG, Streit TG. Geographic distribution of lymphatic filariasis in Haiti. Am J Trop Med Hyg. 2004;71:598–601. [PubMed] [Google Scholar]
- 21.Talbot JT, Viall A, Direny A, de Rochars MB, Addiss D, Streit T, Mathieu E, Lammie PJ. Predictors of compliance in mass drug administration for the treatment and prevention of lymphatic filariasis in Leogane, Haiti. Am J Trop Med Hyg. 2008;78:283–288. [PubMed] [Google Scholar]
- 22.World Health Organization Prevention and Control of Cholera Outbreaks: WHO Policy and Recommendations. Global Task Force on Cholera Control. 2011. http://www.who.int/cholera/technical/prevention/control/en/index1.html Available at. Accessed June 15, 2011.


