Abstract
Haiti's Ministry of Public Health and Population collaborated with global partners to enhance malaria surveillance in two disaster-affected areas within 3 months of the January 2010 earthquake. Data were collected between March 4 and April 9, 2010 by mobile medical teams. Malaria rapid diagnostic tests (RDTs) were used for case confirmation. A convenience sample of 1,629 consecutive suspected malaria patients was included. Of these patients, 1,564 (96%) patients had malaria RDTs performed, and 317 (20.3%) patients were positive. Of the 317 case-patients with a positive RDT, 278 (87.7%) received chloroquine, 8 (2.5%) received quinine, and 31 (9.8%) had no antimalarial treatment recorded. Our experience shows that mobile medical teams trained in the use of malaria RDTs had a high rate of testing suspected malaria cases and that the majority of patients with positive RDTs received appropriate antimalarial treatment. Malaria RDTs were useful in the post-disaster setting where logistical and technical constraints limited the use of microscopy.
Introduction
The Republic of Haiti shares the island of Hispaniola with the Dominican Republic and is located approximately 600 miles southeast of the continental United States. Haiti is one of the poorest countries in the Western Hemisphere, with a 2010 Human Development Index ranking 145th in the world.1 On January 12, 2010, a 7.0-magnitude earthquake struck Haiti, with the epicenter approximately 10 miles west of the capital city of Port-au-Prince (Figure 1). An estimated 1.3 million people, or approximately 14% of the total population, live in the 10 communes that experienced the greatest earthquake intensity.2 Throughout much of the earthquake-affected zone, there was extensive destruction of healthcare facilities and public health infrastructure as well as displacement and loss of many healthcare providers.
Figure 1.
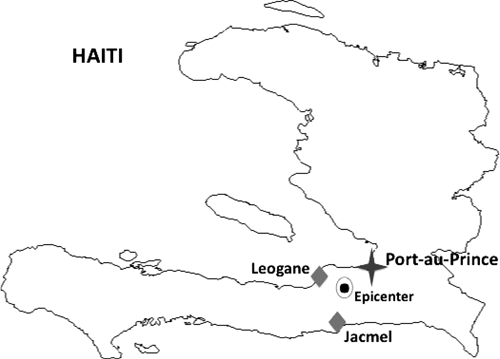
Map of Haiti showing the locations of Port-au-Prince, Léogâne, and Jacmel and the epicenter of the January 12, 2010 earthquake.
In the months after the earthquake, most of the displaced population was living outdoors or in temporary shelters, putting them at increased risk for acquiring malaria. Hispaniola is currently the only Caribbean island with endemic Plasmodium falciparum malaria. The principle vector is Anopheles albimanus, which frequently bites outdoors. Unlike much of the rest of the malaria-endemic world, P. falciparum in Haiti remains sensitive to treatment with chloroquine. The Pan American Health Organization (PAHO) has estimated that as many as 250,000 cases of malaria occur annually in Haiti, but data for laboratory-confirmed malaria cases have not been consistently available.3
In response to the January of 2010 earthquake, the Haitian Ministry of Health and Population (MSPP), in collaboration with the US Centers for Disease Control and Prevention (CDC) and non-governmental organization (NGO) partners, established infectious disease surveillance for a variety of conditions, including malaria.4 However, the surveillance systems were not yet reporting confirmed malaria cases, only suspected cases. The objective of this malaria survey was to rapidly obtain laboratory-confirmed malaria prevalence in persons presenting with fever to mobile or fixed health facilities in disaster-affected areas, identify areas of increased transmission, and monitor treatment provided. This manuscript describes this malaria survey in two of the earthquake-affected areas within the first 3 months after the disaster.
Materials and Methods
Before the earthquake, in accordance with Haiti's national policy, microscopy was the only acceptable diagnostic method for confirming malaria infection, and the existing routine surveillance system included regional monthly reporting of microscopy-confirmed malaria cases by health facilities to the MSPP. Malaria rapid diagnostic tests (RDTs) were not part of the national malaria control strategy. In the earthquake-affected zone, much of the infrastructure required for maintaining malaria microscopy capacity and surveillance was either destroyed or not readily implementable in the emergency response setting. As a result, the MSPP allowed the use of malaria RDTs during a 90-day period immediately after the earthquake from January 12 to April 12, 2010.
This post-earthquake malaria survey was established in the communities of Léogâne and Jacmel (Figure 1). These sites were selected by the MSPP based on the combination of extensive destruction from the earthquake, resulting in a high percentage of the population being displaced, and the historically high prevalence of malaria in these areas before the earthquake. Léogâne (population = 135,000) is located 18 miles west of Port-au-Prince, and Jacmel (population = 138,000) is 25 miles south of Port-au-Prince along the southern coast.5,6
Data were collected between March 4 and April 9, 2010 by mobile medical teams from Save the Children, a large international NGO that has been working in Haiti since 1978, and at the time, it had approximately 800 staff in the country. In Léogâne, there were six medical teams responsible for 26 clinical sites. Most sites were staffed one time per week, with a few staffed two times per week. In Jacmel, there were 11 medical teams responsible for 45 clinical sites, with each site staffed one time per week. The day of the week when the clinic was staffed was on a rotating basis from Monday to Saturday. Each team consisted of Haitian clinicians, including one physician, two nurses, one midwife, one nutritionist, and a community health worker.
To be included in the malaria survey, patients were considered suspected malaria cases based on clinical symptoms or if determined to have a fever without an obvious source after being evaluated by the medical team. For each suspected malaria patient, the age, sex, address or current living location, pregnancy status, history of fever, and measured oral temperature were recorded at the time of the clinic visit on a standardized data collection form. Additionally, if a malaria RDT was performed, the result was recorded. The final diagnosis was left for the clinician to determine based on history, presentation, and RDT results. The final diagnosis was also recorded, and in the case of suspected and confirmed malaria, the type of antimalarial and antipyretic medication given, if any, was documented.
Before data collection, medical team members received training in the diagnosis and treatment of malaria, including the use of malaria RDTs. Teams were supplied with CareStart Malaria HRP2 (Pf) RDTs (AccessBio, Inc., Monmouth Junction, NJ), which detect the histidine-rich protein 2 antigen expressed by P. falciparum, related supplies, including gloves, lancets, alcohol swabs, capillary tubes for blood transfer, sharps disposal containers, and visual aids about malaria and proper RDT use, and surveillance data collection forms for the duration of the surveillance period.
Results
Between March 4 and April 9, 2010, 1,629 consecutive suspected malaria patients were included. Of these 1,629 patients, 1,564 (96%) had malaria RDTs performed, and 317 (20.3%) had a positive result. The overall total number of patients seen, including those patients with diagnoses other than suspected malaria, was not available.
The 317 patients with a positive RDT included 142 (44.8%) females and 175 (55.2%) males. Of these 317 case-patients, 26 (8.2%) were less than 5 years of age, 87 (27.4%) were between 5 and 14 years of age, and 194 (61.2%) were 15 years of age or older. In 10 (3.2%) patients, no age was documented. There were 97 (30.6%) female case-patients between 15 and 49 years of age, of which 11 (3.5%) reported being pregnant.
Finally, of the 317 case-patients with a positive RDT, 278 (87.7%) received chloroquine, 8 (2.5%) received quinine, and 31 (9.8%) had no antimalarial treatment recorded. In addition, of the 1,247 case-patients with a negative RDT, 269 (21.5%) received an antimalarial despite the negative result.
Discussion
Assessing the malaria prevalence among patients seeking care in post-earthquake Haiti presented several challenges. Similar to other complex humanitarian emergencies, the situation in Haiti immediately after the earthquake was a dynamic and chaotic environment. The lack of coordination and presence of logistical challenges combined with mobile populations and a constantly changing network of healthcare facilities and providers made accurate and timely surveillance difficult. One major challenge was how to accomplish accurate case confirmation in the setting of insufficient capacity for malaria microscopy. In response, the MSPP had allowed the use of malaria RDTs for case confirmation during the 90-day period directly after the earthquake. No specific brands were endorsed for this temporary period; however, the choice of RDT for this study was based on product availability and World Health Organization recommendations.7
Despite the limited history of RDT use in Haiti, our experience shows that mobile medical teams trained in the use of malaria RDTs and provided with the necessary supplies had a high rate of testing suspected malaria cases. In addition, a majority of patients with positive RDTs were treated with an antimalarial drug. These results support the use of malaria RDTs in the post-disaster setting, particularly when logistical and technical constraints limit the use of microscopy. Of note, a substantial number of patients with negative RDTs were also treated with an antimalarial. There are many potential reasons for this observation, including clinicians' unfamiliarity or lack of trust of the RDT, clinicians' desire to provide some treatment, or clinicians' tendency to err on the side of overtreatment. This problem should be anticipated and addressed with complementary training around test result-based treatment and management of non-malaria fevers. Information about the reasons patients with a negative RDT were treated with an antimalarial was not collected in our study but is an important question for future investigation.
Because RDTs had not been a component of Haiti's national malaria control strategy, there were initial concerns about the potential for poor RDT sensitivity for Haiti's relatively low transmission level, future sustainability, appropriate RDT use and storage, and lack of clarity about what would happen after the 90-day period. To address these concerns, the MSPP in collaboration with CDC conducted a field assessment of two malaria RDTs commonly being used, comparing their performance to expert microscopy in real world field conditions. Based on this field assessment and rigorous, published laboratory evaluations of commercially available RDTs, the MSPP ultimately selected three malaria RDT products to adopt as part of the national malaria control strategy in July of 2010.8 Although an existing policy on RDTs was not in place before this time, the MSPP used the opportunity not only to address the short-term surveillance needs post-earthquake but also to lay the foundation for a longer-term vision and strategy that could increase the country's diagnostic capacity for malaria.
Other major challenges for conducting this study included how to identify a representative sample of the earthquake-affected population and collect accurate and timely demographic information, despite the population's inconsistent availability and access to functioning healthcare facilities. In addition, because the earthquake destroyed much of the infrastructure, the majority of healthcare facilities operating in or near the camps were recently established, temporary facilities run by NGOs. Although many of these facilities were registered with the United Nations Health Cluster, in the months immediately after the earthquake, not all were registered. Thus, at that time, there was no comprehensive list of healthcare facilities, their capabilities, and the population or area that they served. Given these challenges, we recruited among the known network of large NGOs, but many did not follow-up with data collection and submission because of competing responsibilities and changing staff. Save the Children mobile teams viewed the data collection as useful to their performance and were the only NGO teams that collected data consistently throughout the time of our study.
During the survey period, 96% of 1,629 suspected malaria patients had malaria RDTs performed, with an overall positivity rate of 20.3%. Our results suggest that malaria is an important health problem in the displaced population in Jacmel and Léogâne, possibly worsened by living outdoors or in temporary shelters. In a retrospective study of malaria cases between 1975 and 1997 done at Bon Samaritan Hospital in the Limbé Valley located in northeastern Haiti, 50% of malaria cases occurred during two peak transmission seasons, one in the summer between June and July and one in the winter between December and January.9 A comparison of this investigation with our study suggests that the incidence of malaria was expected to increase, because our study was conducted immediately after the earthquake and before the peak transmission season. A later study at one health center in Léogâne, conducted during peak transmission season, reported an RDT positivity rate of 46.9% among 130 patients presenting with undifferentiated fever.10
In post-earthquake Haiti and similar complex humanitarian emergencies, it is important to have accurate malaria diagnostics available to all healthcare facilities in operation. Many of the NGO-established facilities had not routinely used microscopy before the earthquake, and for those facilities that did use microscopy, many lost that capacity with the earthquake. The experience in Haiti supports the use of malaria RDTs as an alternative to microscopy in the post-disaster setting to improve the accuracy and completeness of malaria surveillance. RDTs may also increase the proportion of suspected malaria cases that receive laboratory confirmation by extending diagnostic capacity to settings that cannot support microscopy. The specific RDTs used should be chosen carefully, be appropriate for the particular setting, and be consistent with the country's national policy for malaria diagnostics. In addition, training in their use and quality assurance should be provided. Even before the earthquake, microscopy use was limited in Haiti because of a lack of equipment and trained personnel, especially in the rural parts of the country. Because malaria RDTs require less training and equipment, they are likely to play an important role not only during the immediate relief efforts but beyond as well.
Footnotes
Authors' addresses: David Townes, Laurence Slutsker, and Michelle Chang, Malaria Branch, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, GA, E-mails: townesd@uw.edu, lms5@cdc.gov, and aup6@cdc.gov. Alexandre Existe and Jacques Boncy, National Public Health Laboratory, Ministry of Health and Population, Port-au-Prince, Haiti, E-mails: Alexandre.existe@gmail.com and Jboncy2001@yahoo.fr. Roc Magloire, Department of Epidemiology and Laboratory Research, Ministry of Health and Population, Port-au-Prince, Haiti, E-mail: Corgamsa368@hotmail.com. Jean-Francois Vely, National Malaria Control Program, Ministry of Health and Population, Port-au-Prince, Haiti. Ribka Amsalu, Save the Children, E-mail: ramsalu@savechildren.org. Marleen De Tavernier, Save the Children, Jacmel, Haiti, E-mail: mtavernier@savechildren.org. James Muigai, Save the Children, Léogâne, Haiti, E-mail: jmungai@savechildren.org. Sarah Hoibak and Michael Albert, The MENTOR Initiative, La Prade, France, E-mails: sarahhoibak@hotmail.com and michael.a.albert@gmail.com. Meredith McMorrow and S. Patrick Kachur, Malaria Branch, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, GA, and United States Public Health Service, E-mails: bwe3@cdc.gov and spk0@cdc.gov.
References
- 1.United Nations Development Programme. 2011. http://hdr.undp.org/en/statistics/ Available at. Accessed March 20.
- 2.US Census Bureau. 2011. http://www.census.gov/newsroom/emergencies/earthquake_in_haiti.html Available at. Accessed June 23.
- 3.Pan American Health Organization (PAHO) 2011. http://www.paho.org/english/sha/prflhai.htm Available at. Accessed March 20.
- 4.Magloire R, Mung K, Cookson ST, Tappero J, Barzilay E, Dominguez K, Dubray C, Lindblade K, Jentes ES, Willis M, Tohme RA, Sprecher AG, El Bcheraoui C, Walldorf JA. Rapid establishment of an internally displaced persons disease surveillance system after an earthquake—Haiti, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:939–945. [PubMed] [Google Scholar]
- 5.GeoNames. 2011. http://www.geonames.org/search.html?q=jacmel%2C+haiti&country= Available at. Accessed March 20.
- 6.Wikipedia. 2011. http://en.wikipedia.org/wiki/List_of_populated_places_affected_by_the_2010_Haiti_earthquake Available at. Accessed March 20.
- 7.World Health Organization Information Note on Recommended Selection Criteria for Procurement of Malaria Rapid Diagnostic Tests (RDTs), Global Malaria Programme, World Health Organization, September 16, 2010. 2010. 2011. http://www.theglobalfund.org/documents/psm/PSM_RDTSelection_Criteria_en/ Available at. Accessed March 20.
- 8.Existe A, Freeman N, Boncy J, Magloire R, Vely J-F, Chang M, Bishop H, Macedo de Oliverira A, McMorrow M, Dasilva A, Barnwell J, Slutsker L, Townes D. Rapid diagnostic tests for malaria—Haiti, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:1372–1373. [PubMed] [Google Scholar]
- 9.Vanderwal T, Paulton R. Malaria in the Limbe River Valley in northern Haiti: a hospital-based retrospective study, 1975–1997. Rev Panam Salud Publica. 2000;7:162–167. doi: 10.1590/s1020-49892000000300004. [DOI] [PubMed] [Google Scholar]
- 10.Neuberger A, Zaulan O, Tenenboim S, Vernet S, Pex R, Held K, Urman M, Garpenfeldt K, Schwartz E. Malaria among patients and aid workers consulting a primary healthcare centre in Leogane, Haiti, November 2010 to February 2011—a prospective observational study. Euro Surveill. 2011;16:19829. [PubMed] [Google Scholar]


