Abstract
Lymphocytic choriomeningitis virus (LCMV) exhibits natural tropism for dendritic cells and represents the prototypic infection that elicits protective CD8+ T cell (cytotoxic T lymphocyte (CTL)) immunity. Here we have harnessed the immunobiology of this arenavirus for vaccine delivery. By using producer cells constitutively synthesizing the viral glycoprotein (GP), it was possible to replace the gene encoding LCMV GP with vaccine antigens to create replication-defective vaccine vectors. These rLCMV vaccines elicited CTL responses that were equivalent to or greater than those elicited by recombinant adenovirus 5 or recombinant vaccinia virus in their magnitude and cytokine profiles, and they exhibited more effective protection in several models. In contrast to recombinant adenovirus 5, rLCMV failed to elicit vector-specific antibody immunity, which facilitated re-administration of the same vector for booster vaccination. In addition, rLCMV elicited T helper type 1 CD4+ T cell responses and protective neutralizing antibodies to vaccine antigens. These features, together with low seroprevalence in humans, suggest that rLCMV may show utility as a vaccine platform against infectious diseases and cancer.
Vaccines represent one of the most successful interventions in modern medicine, having led to the control of many devastating infectious diseases and recently also to the prevention of cervical cancer. Recombinant DNA technology and bioengineering have made it possible to exploit viral vectors for optimized vaccine delivery. Attenuated or replication-incompetent viruses such as modified vaccinia virus Ankara and recombinant adenovirus 5 are genetically modified to express a vaccine antigen of interest.
Many vectors have limitations, and their ability to counter infection by HIV, hepatitis C virus and tuberculosis or treat tumors remains uncertain. The induction of protective and long-lived cytotoxic T lymphocytes (CTLs) is an unmet yet important goal of vaccination against many of these diseases, which have a considerable effect on human health. Poxvirus-based vectors, for example, effectively induce multifunctional CTL responses1, but they exhibit a limited ability to elicit CTL responses of high magnitude2. Conversely, recombinant adenovirus (rAd)-based vaccines stimulate high-frequency responses that tend to be less multifunctional3. Moreover, a significant proportion of the global population carries adenovirus 5–neutralizing antibodies from natural infection, which can affect vector immuno-genicity4,5. Even in the absence of preexisting immunity, vaccination with rAd- or poxvirus-based vaccines elicits potent vector-specific antibody immunity, which interferes with homologous boosting5. Thus, there remains a need to develop viral vectors that elicit effective T cell immunity without concomitant induction of antibodies that block vector re-administration.
The prototypic arenavirus lymphocytic choriomeningitis virus (LCMV) contains a bisegmented negative-strand RNA genome encoding the viral proteins glycoprotein (LCMV-GP), nucleoprotein (NP), Z and L in an ambisense strategy6 (Fig. 1a). LCMV-GP mediates receptor binding and cell entry and represents the only target for LCMV-neutralizing antibodies6. LCMV-induced T cell responses are broad and long-lived7, and LCMV infection has been widely studied as a model of CTL-mediated protection. The neutralizing antibody response to LCMV is extraordinarily weak, and convalescent serum fails to prevent re-infection6,8. These characteristics suggested that modified LCMV might serve as a vector for the induction of CTL immunity. Recently, it has become possible to manipulate the LCMV genome by recombinant cDNA technology9,10. Here we report on a molecular strategy for rendering the virus replication incompetent to confer an acceptable safety profile while allowing the incorporation of diverse antigens that can confer protection against infections and cancers.
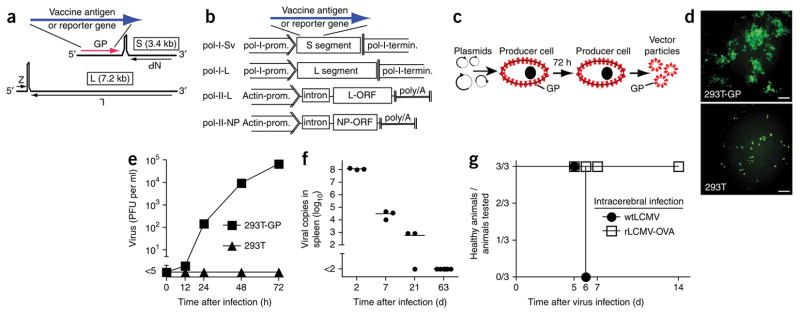
Figure 1.
Generation of rLCMV vectors, replication in cultured cells and rapid elimination and lack of pathogenicity in vivo. (a) Wild-type LCMV with its two genome segments (S and L) and the four open reading frames (ORFs). Substitution of GP for a vaccine antigen or reporter gene creates the rLCMV vectors. (b) Expression cassettes of plasmids used for the recovery of rLCMV vectors. In pol-I-Sv and pol-I-L10, the mouse polymerase I promoter (pol-I-prom.) and terminator (pol-I-termin.) drive intracellular expression of the LCMV vector S segment and L segment, respectively; pol-II-L10 and pol-II-NP10 express the respective viral proteins under control of an actin promoter (Actin-prom.)-driven expression cassette with intron and polyadenylation (poly(A)) signal. ORF, open reading frame. (c) Process to recover rLCMV vectors in producer cells. LCMV-GP protein (GP) on the surface of producer cells is incorporated into vector particles. (d) Fluorescence microscopy of GFP expression in 293T cells and GP-expressing 293T cells (293T-GP) infected for 48 h with rLCMV-GFP at a multiplicity of infection of 0.05. Scale bars, 100 μm. (e) Infectious progeny particles in supernatants of the 293T cells and GP-expressing 293T cells in d at 0–72 h after infection. Data are representative of three individual culture wells (mean ± s.e.m.). (f) Real-time RT-PCR analysis of vector S segment copies, measured in total RNA from spleen of mice vaccinated with rLCMV-GFP. Each symbol represents an individual mouse; small horizontal lines indicate the mean. (f) Disease development in mice infected intracerebrally with wild-type LCMV or rLCMV-OVA (three mice per group). Animals displaying clinical signs of lymphocytic choriomeningitis were killed in accordance with the Swiss law for animal protection.
RESULTS
Generation of replication-defective rLCMV vectors
To generate replication-deficient LCMV (rLCMV) vectors, we hypothesized that the viral GP open reading frame could be replaced by a gene encoding a vaccine antigen (Fig. 1a). We generated rLCMV vectors in which GP was deleted using a four-plasmid co-transfection system previously used to generate wild-type LCMV10. The short (S) and long (L) vector RNA genome segments were expressed intra-cellularly from plasmid expression vectors under control of an RNA polymerase I promoter and terminator (Fig. 1b). The minimal viral trans-acting factors (NP and L) were co-expressed from an RNA polymerase II promoter in additional plasmids (Fig. 1b). We used these four plasmids for transient transfection of BHK-21 cells stably transfected with an LCMV-GP expression vector (‘producer cells’; Fig. 1c). In these cells, the GP-deficient viral genomes were complemented in trans and gave rise to vectors whose RNA could be amplified and expressed in target cells, but they could not give rise to a spreading virus and propagate infection.
To confirm expression of the heterologous gene, we generated an rLCMV with the green fluorescent protein (GFP) reporter gene in place of LCMV-GP (rLCMV-GFP). Infection of normal BHK-21 or 293T cells with rLCMV-GFP yielded individual fluorescent cells that did not increase in number over time, whereas passage of GP-expressing BHK-21 or 293T producer cells yielded expanding fluorescent foci indicative of viral propagation (Fig. 1d and data not shown). This finding suggested that rLCMV particles formed in normal cells were GP deficient and replication incompetent, as expected. The growth curves of rLCMV-GFP confirmed the presence of vector in the supernatants of producer cells but not those of normal cells (Fig. 1e). In C57BL/6 mice inoculated intravenously with rLCMV-GFP, viral RNA copies in spleen declined rapidly and early, and within 21 d, they approached the limit of detection (Fig. 1f). To determine whether this vector induced disease in the central nervous system, we injected an rLCMV vector expressing ovalbumin (rLCMV-OVA) intracerebrally. This vector failed to elicit clinical signs of chorio-meningitis, whereas wild-type LCMV uniformly caused fatal disease (Fig. 1g). Mice with a combined genetic deficiency in type I and type II interferon receptors (Ifnar1−/−Ifngr−/−; called ‘Ifnagr−/−’ here) are uniquely permissive for LCMV, and Ifnagr−/− mice have therefore been used to detect very low-level LCMV replication11. We inoculated Ifnagr−/− mice with rLCMV-GFP and killed them 2, 7 or 21 d later. We sampled spleen, liver, lung, kidney and brain tissues without detecting infectivity at any time point (Supplementary Fig. 1a), which further documented that the rLCMV vectors were replication incompetent in vivo. The rLCMV vector also did not inhibit CTL or antibody responses to vesicular stomatitis virus (VSV; Supplementary Fig. 1b), which indicated that rLCMV vectors did not adversely affect general immunocompetence.
rLCMV vectors elicit potent CD8+ T cell responses
To characterize the immunogenicity of proteins encoded by rLCMV, we injected increasing doses of rLCMV-OVA or rAd vector expressing OVA (rAd-OVA) into C57BL/6 mice and assessed CD8+ T cell frequencies specific for OVA (SIINFEKL epitope) in the peripheral blood after 28 d. At lower vector doses of 3 × 102 or 3 × 104 plaque-forming units (PFU), rLCMV-OVA elicited higher frequencies of specific CD8+ T cells than did rAd-OVA, whereas at higher doses of 3 × 105 or 3 × 107 PFU, the responses were similar (Fig. 2a). A further increase in dose was technically possible only for rAd-OVA and resulted in exhaustion of T cell responses (Fig. 2a, 2.5 × 108 PFU), similar to previous reports12. An rLCMV vector expressing the HLA-A2.1-restricted CD8+ T cell epitope MelanA26–35(27L) (rLCMV–MelanA26–35(27L)) stimulated vigorous responses in HLA-A2.1-transgenic mice (Supplementary Fig. 2), which demonstrated that rLCMV can trigger responses of a clinically relevant specificity. The route of vector administration may affect immune responses. We used an intravenous route of immunization here, but responses of similar magnitude have been observed after intradermal, subcutaneous, intramuscular or intraperitoneal administration of rLCMV vectors (Supplementary Fig. 3 and data not shown). CTL induction by rLCMV-OVA was abolished by ultraviolet irradiation of vector (data not shown), which indicated that its immunogenicity depended on gene expression in vivo.
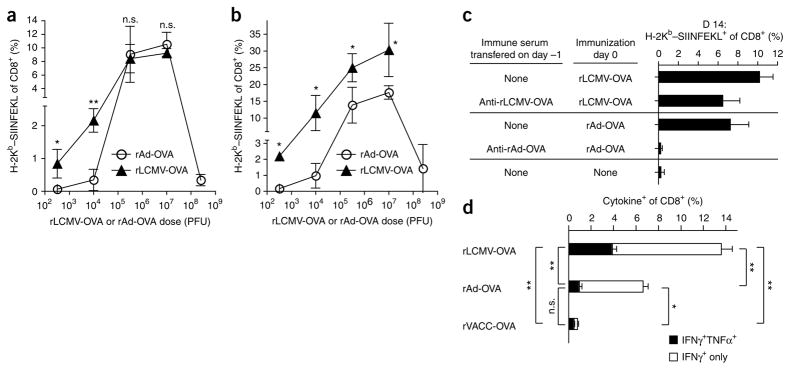
Figure 2.
The rLCMV vectors elicit CD8+ T cell responses of high frequency and functionality that are efficiently amplified in homologous prime-boost vaccination. (a,b) SIINFEKL-specific CD8+ T cell frequencies in the blood of mice vaccinated (primed) with rAd-OVA or rLCMV-OVA (dose, horizontal axis) on day 0 and boosted with the same vector-dose combination on day 38, assessed on day 28 after vaccination (a) and 7 d after boost (b). (c) SIINFEKL-specific CD8+ T cell frequencies in peripheral blood: serum (500 μl) from mice vaccinated with rLCMV-OVA or rAd-OVA 4 weeks previously was transferred into naive mice; 1 d after transfer, both groups and controls without serum transfer were vaccinated with the same two vectors, and T cell frequencies were determined 14 d later. Data are representative of three mice per group (mean ± s.d.). (d) Intracellular cytokine assay of SIINFEKL-specific CD8+ T cells producing IFN-γ alone (IFN-γ+ only) or both IFN-γ and TNF-α (IFN-γ+TNF-α+) in spleen, assessed on day 14 after vaccination with rLCMV-OVA, rAd-OVA or VACC-OVA. Data are representative of three to six mice per group (mean ± s.e.m.). P values of less than 0.05 (*) were considered statistically significant, and P values of less than 0.01 (**) were considered highly significant.
When rLCMV- and rAd-induced CTL responses were boosted with homologous vector on day 38, rLCMV-OVA elicited significantly higher specific CD8+ T cell frequencies than did rAd-OVA at all doses (Fig. 2b). The relative increase in specific CD8+ T cell frequency after boosting was particularly evident at lower doses but was also observed at standard doses and was higher for rLCMV-OVA than for rAd-OVA (rLCMV-OVA, 2.46-fold ± 0.54-fold; rAd-OVA, 1.58-fold ± 0.33-fold (mean ± s.d. of three experiments); P < 0.001; data not shown). Furthermore, we found that three administrations of rLCMV-OVA at monthly intervals maintained OVA-specific CD8+ T cell frequencies at ~3–4% of total CD8 T+ cells 276 d after the final immunization (Supplementary Fig. 4a). We established the functionality of such memory cells in an in vivo cytotoxicity assay on day 168 after the third immunization. Transfusion of syngenic splenocytes incubated with the OVA-derived CTL peptide SIINFEKL resulted in almost complete rejection of these cells within 24 h, whereas control cells without peptide persisted in the circulation (Supplementary Fig. 4b). More than 80% of rLCMV-OVA-induced memory CTLs had high expression of the activation marker CD44. About half were KLRG-1+, 40% were positive for the interleukin 7 (IL-7) receptor (CD127+) and 15% were CD62L+ central memory cells 45 d after a single immunization (Supplementary Fig. 2c). By day 196 after boosting, over 90% had become positive for the IL-7 receptor, and the fraction of CD62L+ central memory cells had increased to slightly over 30%.
Unlike antibodies to adenovirus 5 (ref. 5), antibodies to LCMV have a limited capacity to prevent reinfection6,8, a property that could have explained the superior performance of rLCMV-OVA in homologous prime-boost immunizations (Fig. 2b). To test this hypothesis, we passively transferred serum from rLCMV-OVA-immunized mice into naive mice. After subsequent immunization with rLCMV-OVA, the CD8+ T cell response was similar to or only moderately lower than that of control mice that received naive serum (Fig. 2c). In contrast, passive transfer of rAd-OVA-immune serum markedly decreased the specific CD8+ T cell response after rAd-OVA immunization, consistent with previous studies of preexisting immunity to adenovirus 5 (ref. 5). We obtained analogous results with immune serum collected 100 d after the last of three monthly immunizations with rLCMV-OVA or rAd-OVA (Supplementary Fig. 5), which confirmed that antibodies with the capacity to block rLCMV vector immunogenicity were inefficiently induced.
To evaluate the functionality of rLCMV-induced CTLs, we measured OVA-specific interferon-γ (IFN-γ)-secreting CD8+ T cells and CD8+ T cells producing both IFN-γ and tumor necrosis factor-α (TNF-α) in the spleen. We found that rLCMV-OVA elicited responses at higher frequencies than did immunization with rAd-OVA or recombinant vaccinia virus expressing OVA (VACC-OVA, Fig. 2d), which attested to the quality of rLCMV-induced CTLs.
Induction of CD4+ T cells and protective antibodies
To examine CD4+ T cells and antibody responses, we generated an rLCMV vector expressing a defective form of the VSV G envelope glycoprotein (rLCMV-INDG61), in which the immunodominant I-Ab-restricted epitope of LCMV-GP (GP61) was inserted in the ectodomain of the VSV G envelope glycoprotein. We labeled transgenic CD4+ T cells specific for GP61 (SMARTA1 T cells13) with the fluorescent dye CFSE and transferred the cells into naive C57BL/6 recipients. Administration of rLCMV-INDG61 stimulated rapid cell division evident in the dilution of CFSE on 98% of the SMARTA1 CD4+ T cells within 3 d of vaccination (Fig. 3a). Similarly, adoptively transferred GP33-specific CD8+ T cells from T cell receptor (TCR)-transgenic mice underwent rapid cell division after immunization with rLCMV (Supplementary Fig. 6). After initial population expansion, rLCMV-INDG61-activated SMARTA1 T cells slowly decreased in frequency during the observation period of 2 months, similar to CD4+ T cells after infection with wild-type LCMV7,13 (Fig. 3b). When SMARTA1 CD4+ T cells were restimulated 9 d after rLCMV-INDG61 vaccination, >95% of the cells synthesized TNF-α and many also co-expressed IFN-γ (Fig. 3c, left), whereas secretion of IL-4 and IL-10 was minimally detectable (Fig. 3c, right), indicative of T helper type 1 polarization in rLCMV-triggered CD4+ T cell responses13.
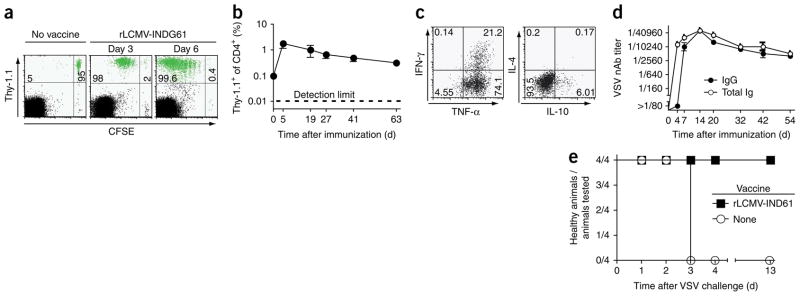
Figure 3.
The rLCMV vectors trigger rapid proliferation, T helper type 1 differentiation and memory formation of CD4+ T cells and elicit durable neutralizing antibody responses to vaccine antigen. (a) Proliferation (assessed as CFSE dilution) in blood of naive syngeneic recipients given CFSE-labeled SMARTA TCR-transgenic splenocytes carrying the Thy-1.1 marker, then vaccinated with rLCMV-INDG61 or left unvaccinated (No vaccine), assessed on days 3 and 6. Green indicates transferred epitope-specific (Thy-1.1+) cells. (b,c) Frequency of SMARTA1 CD4+ T cells in peripheral blood over time (b) and cytokine profile of SMARTA1 CD4+ T cells after restimulation with phorbol 12-myristate 13-acetate and ionomycin on day 9 (c), assessed for cells from the mice in a. (d) VSV-neutralizing titers of total immunoglobulin (Total Ig) and immunoglobulin G (IgG) in serum of C57BL/6 mice vaccinated with rLCMV-INDG61. nAb, neutralizing antibody. Data are representative of three to six mice per group (b,d; mean ± s.e.m.). (e) Disease development in type I interferon receptor–deficient mice vaccinated with rLCMV-INDG61 or left untreated, then challenged intravenously with 2 × 106 PFU VSV 4 weeks later (four mice per group). Animals with terminal myeloencephalitis were killed.
Immunization with rLCMV-INDG61 also stimulated a potent neutralizing antibody response to VSV that reached titers of ~1:10,000 within 4 d (Fig. 3d). Isotype class switching to immunoglobulin G was evident 7 d after vaccination, which reflected efficient CD4+ T cell help. Titers in the range of 1:5,000 were maintained throughout the observation period of 54 d, which demonstrated the durability of this antibody response after rLCMV vaccination. We confirmed the protective capacity of rLCMV-induced antibodies in mice deficient in type I interferon receptors. Immunization with rLCMV-INDG61 protected these mice against challenge with 2 × 106 PFU VSV (>10,000-fold the 50% lethal dose14), whereas non-immune controls rapidly developed terminal myeloencephalitis (Fig. 3e).
Efficacy and longevity of rLCMV-induced CTL responses
We next examined the protective capacity of rLCMV-induced CTL immunity. We vaccinated C57BL/6 mice with rLCMV-OVA, rAd-OVA or VACC-OVA, challenged them with recombinant Listeria monocytogenes expressing OVA (rLM-OVA15) on day 16 after immunization and measured bacterial titers in the liver 3 d later16. Immunization with rLCMV-OVA or rAd-OVA resulted in bacterial titers that were nearly undetectable. In contrast, immunization with VACC-OVA failed to confer protection (Fig. 4a). When we challenged the mice 58 d after a single vaccination or 200 d after prime-boost immunization, we obtained similar results, which confirmed the durability of protection of rLCMV-OVA and rAd-OVA. This protection was produced in a dose-response manner. When we challenged the mice either 18 d after single immunization or 200 d after prime-boost vaccination, rLCMV-OVA afforded antibacterial protection at doses 30- to 1,000-fold lower than those of rAd-OVA (Supplementary Fig. 7a–b).
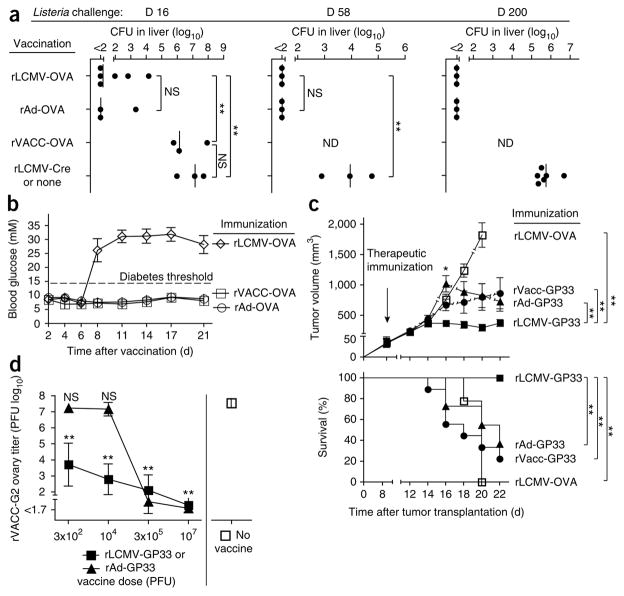
Figure 4.
Efficacy and protective capacity of rLCMV-induced CTL responses. (a) Bacterial titers in the livers of C57BL/6 mice vaccinated with rLCMV-OVA, rAd-OVA or VACC-OVA, then challenged with rLM-OVA 16 or 58 d after single immunization or 200 d after homologous prime-boost vaccination (days 0 and 38); titers were measured 3 d after challenge. Immunization with rLCMV-Cre (challenge on day 16 or 58) and no immunization (challenge on day 200) serve as controls. Each symbol represents an individual mouse; small vertical lines indicate the mean. (b) Blood glucose concentrations of RIP-OVA-transgenic mice transfused with 1 × 103 OT-I TCR-transgenic splenocytes on day -1 and immunized with rLCMV-OVA, VACC-OVA or rAd-OVA on day 0. Data are from one representative of two experiments (mean ± s.e.m. of three to six mice). (c) Tumor volume and survival of C57BL/6 mice injected subcutaneously in both flanks with 5 × 105 B16.F10 melanoma cells expressing the CTL epitope GP33 (ref. 19); 8 d later, tumor masses were palpable, and rLCMV-GP33, rAd-GP33 or VACC-GP33 was given for immunotherapy. Immunization with rLCMV-OVA serves as a control. Tumor volume was calculated by the formula V = π × abc/6, where a, b and c are the orthogonal diameters. For survival analysis, death and humane endpoints (tumor volume, tumor exulceration, cachexia) were counted as events. Broken lines (top) indicate loss of mice to follow-up (bottom), which caused a bias toward smaller tumors at subsequent time points. Data are representative of initially 18–22 tumors from 9–11 mice per group (mean ± s.e.m.). (d) Viral titers in the ovaries of C57BL/6 mice vaccinated with rLCMV-GP33 or rAd-GP33 (dose, horizontal axis) or left untreated, then given 2 × 106 PFU of VACC-G2 intraperitoneally 18 d later and killed 6 d later. Statistical analysis identifies groups that differ significantly from unvaccinated controls. Data are representative of five mice (mean ± s.d.). P values of less than 0.01 (**) were considered highly significant.
Next we assessed the cytolytic efficacy of rLCMV-, rAd- and VACC-induced CTLs in solid tissues. RIP-OVA mice express OVA antigen in pancreatic islet cells17 and exhibit central tolerance to OVA, but adoptively transferred OVA-specific TCR-transgenic CD8+ T cells (OT-I cells18) can destroy pancreatic beta cells and cause diabetes if appropriately stimulated by OVA-specific vaccination. We gave RIP-OVA mice 1 × 103 OT-I splenocytes (~1 × 102 OVA-specific CD8+ T cells) and then immunized the mice with rLCMV-OVA, rAd-OVA or VACC-OVA (Fig. 4b). In two independent experiments, rLCMV-OVA-immunized mice uniformly exhibited loss of glucose control (nine of nine mice), whereas VACC-OVA-immunized mice (one of six mice) and rAd-OVA-immunized mice (none of six mice) remained mostly unaffected. This finding demonstrated that rLCMV was more effective than rAd and VACC in stimulating specific CTLs that destroyed antigen-expressing cells in solid tissue.
To test the capacity of rLCMV vectors to promote CTL-mediated rejection of peripheral solid tumors, we injected B16.F10 melanoma cells expressing the CTL epitope GP33 subcutaneously into the flank of C57BL/6 mice19. Eight days later, tumor masses were palpable, and we treated mice with rLCMV-, rAd- or VACC-based vectors expressing the GP33 epitope (rLCMV-GP33, rAd-GP33 or VACC-GP33, respectively) and used rLCMV-OVA as a negative control. Within 8 d of injection, the tumor masses were significantly smaller in rLCMV-GP33-treated mice than in all other groups (Fig. 4c, top). Further, all 11 rLCMV-GP33-treated mice survived until day 22 (14 d after immunotherapy; termination of the experiment), with tumors shrinking or stabilizing. In contrast, most mice vaccinated with rAd-GP33 or VACC-GP33 or with the rLCMV-OVA control had died or reached the endpoint criteria of tumor volume (Fig. 4c, bottom).
We used a vaccinia virus challenge to assess the ability of rLCMV to confer antiviral protection. We immunized C57BL/6 mice with increasing doses of rLCMV-GP33 or rAd-GP33. Then, 18 d later, we challenged the mice intraperitoneally with the recombinant vaccinia virus VACC-G2 expressing full-length LCMV-GP (containing GP33) and measured VACC-G2 titers in the ovaries 6 d after challenge. Even at the lowest vaccine dose, VACC-G2 titers in rLCMV-GP33- immunized mice were three orders of magnitude lower than those of non-immune control mice (Fig. 4d). Vaccination with rAd-GP33 also conferred protection but required doses of ≥3 × 105 PFU, 1000-fold higher than the minimal protective dose of rLCMV-GP33.
rLCMV vectors target and activate dendritic cells in vivo
The targeting and activation of dendritic cells (DCs) is key for CTL induction20,21, and wild-type LCMV exhibits tropism for DCs22. To understand the mechanism by which rLCMV vectors might elicit adaptive immune responses, we studied the cellular tropism of an rLCMV expressing Cre recombinase (rLCMV-Cre). After injection of rLCMV-Cre into transgenic reporter mice23, Cre-mediated removal of a loxP-flanked transcription stop signal allowed expression of an actin promoter-driven GFP. Flow cytometry of GFP+ cells identified about 5 × 103 rLCMV-Cre-infected DCs per spleen, in contrast to around 200 fluorescent macrophages, T cells and B cells (Fig. 5a). This indicated that rLCMV vectors showed a tropism for DCs, similar to wild-type LCMV22. DCs infected with rLCMV-Cre (GFP+) exhibited higher surface levels of CD86 than did uninfected (GFP−) DCs in the same mice (Fig. 5b; mean fluorescence indices, 15.5 ± 2.7 (GFP+) versus 5.3 ± 0.4 (GFP−); P < 0.001), and the latter were similar to DCs in mice that received rLCMV-OVA control (mean fluorescence index, 4.6 ± 0.2; P = 0.14), which suggested that rLCMV vectors activated mainly infected DCs. To analyze DC activation by rLCMV further, we used the transgenic mouse model ST33 (ref. 21), which expresses GP33 after intracellular expression of Cre. Expression of GP33 in resting ST33 DCs triggers specific CD8+ T cell tolerance, whereas GP33 expression in activated DCs results in CD8+ T cell priming21. Administration of rLCMV-Cre in ST33 mice resulted in 0.8% GP33-specific CD8+ T cells on day 10 and day 27, and this was absent in ST33 mice inoculated with rLCMV-OVA (Fig. 5c). Subsequent challenge with VACC-G2 triggered a rapid population expansion of the GP33-specific CTLs that produced IFN-γ upon in vitro restimulation. These data confirmed that rLCMV not only targeted DCs but also functionally activated them in vivo.
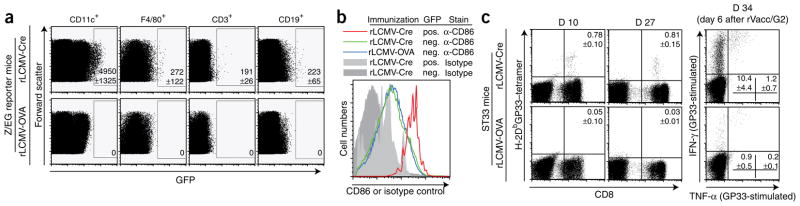
Figure 5.
The rLCMV vectors target and activate DCs. (a) Flow cytometry of GFP expression in DCs (CD11c+), macrophages (F4/80+), T cells (CD3+) and B cells (CD19+) in Z/EG transgenic reporter mice 3 d after vaccination with rLCMV-Cre or rLCMV-OVA (control vector). Numbers in outlined areas indicate total number of fluorescent cells per spleen (mean ± s.e.m.); gates were set such that no positive cells were recorded for mice vaccinated with rLCMV-OVA. Data are representative of four Z/EG mice per group. (b) CD86 surface expression on CD11c+ DC populations from the mice in a, identified as GFP+ (pos.) or GFP− (neg.) and stained with antibody to CD86 (α-CD86) or isotype-matched control antibody (Isotype). (c) GP33-specific CD8+ T cell frequencies in blood of ST33 mice vaccinated with rLCMV-Cre or rLCMV-OVA control vector, assessed by major histocompatibility complex class I (H-2Db) tetramer staining on days 10 and 27 after vaccination (left), and GP33-specific recall responses in spleen after mice were challenged with VACC-G2 on day 28 of the experiment, assessed 6 d later by intracellular cytokine assay. Numbers in plots indicate percent tetramer-positive CD8+ T cells (left; top right quadrant) or percent IFN-γ+ CD8+ T cells (right; top left quadrant) or IFN-γ+TNF-α+ CD8+ T cells (right; top right quadrant). Data are from one representative of two similar experiments (mean ± s.d. of three to four mice per group).
When rLCMV vectors were incubated with human peripheral blood mononuclear cells (PBMCs) in vitro, they infected over 60% of myeloid DCs, plasmacytoid DCs and monocytes, compared with less than 2% of B cells, CD4+ and CD8+ T cells (Supplementary Fig. 8a), which resembled the vector tropism in mice (Fig. 5a). Infection of human myeloid DCs also increased expression of the activation marker CD86 (Supplementary Fig. 8b). Finally, incubation of PBMCs from human melanoma patients with rLCMV–MelanA26–35(27L) in vitro stimulated a substantial HLA-A★0201-restricted MelanA26–35(27L)-specific CD8+ T cell response (Supplementary Fig. 8c), which exceeded the response triggered by MelanA26–35(27L) peptide. These experimental observations indicate that rLCMV will be immunogenic in humans.
DISCUSSION
The properties of rLCMV suggest that it holds promise as a vector for vaccination and immunotherapy in infectious diseases and cancer. Its desirable features stem mainly from three properties: (i) its ability to target and functionally activate DCs, (ii) its stimulation of potent CD8+ T cell responses and (iii) its relative insensitivity to antibody neutralization and thus its efficacy in homologous prime-boost vaccination. A cardinal aspect of rLCMV immunogenicity is its targeting to DCs, followed by activation of these cells20, which is probably responsible for the potent CTL induction. The ability of rLCMV-immunized mice to respond to homologous boosting reflects the poor induction of neutralizing antibodies, an intrinsic feature of the LCMV envelope glycoprotein8. In addition, the limited number of rLCMV vector particles administered for vaccination here provided relatively low amounts of LCMV-GP, and exposure of the immune system to LCMV-GP was of short duration. The gene encoding LCMV-GP is absent from rLCMV vectors, and the vaccine cannot produce further LCMV-GP in vivo to trigger GP-specific neutralizing antibody responses. Moreover, even antibodies that potently neutralize LCMV in vitro exhibit only a limited capacity to interfere with T cell induction in vivo24. Together these considerations probably explain why even multiple administrations of rLCMV over prolonged periods of time have failed to elicit antibodies that interfere with vector immunogenicity. In addition to the limited interference by preexisting humoral immunity, all the existing evidence suggests that human seroprevalence to LCMV is generally below 5% (refs. 25–28). In contrast, high-titer protective neutralizing antibody responses are generated to the transgene encoded by the vector, which indicates its likely utility as a vaccine vector in humans. Wild-type LCMV can replicate and cause disease in immunosuppressed transplant recipients29. The lack of rLCMV replication suggests therefore that these vectors will provide a suitable safety profile for further development in humans.
Possible applications for rLCMV include protective vaccines, for example, against HIV, hepatitis C virus, tuberculosis and malaria, as well as cancer immunotherapy. Preliminary data in mice suggest that rLCMV vectors elicit CD8+ T cell responses to HIV antigens at high frequency and functionality (L.F. and G.J.N., unpublished data). Future studies should determine whether rLCMV vectors are particularly advantageous in eliciting CD8+ T cell responses to self antigens on tumors, in which immunotherapy can be compromised by T cell tolerance.
The choice of an optimal vaccine vector depends on both the properties of the vector and the mechanisms of protection for specific diseases. Additional parameters, including ease of storage, large-scale manufacturing, cost effectiveness and the size of the gene payload, can be limiting and remain to be determined for rLCMV. We have generated rLCMV vectors carrying foreign genes up to 2.6 kilobases in size without technical difficulties. If size limits for inserts existed, multiple vectors carrying individual antigens could be combined in a single vaccine, as successfully performed with recombinant adeno-virus 5–based vectors30. Given all of these observations, rLCMV represents an attractive vector for stimulating both cellular and humoral immunity. Thus, it provides a platform that may be used to prevent or treat malignant and infectious diseases for which existing vaccination strategies have yet to confer protection.
METHODS
Methods and any associated references are available in the online version of the paper at http://www.nature.com/naturemedicine/.
Supplementary Material
Acknowledgments
We thank H. Hengartner and R. Zinkernagel for critical comments, suggestions, discussions and long-term support; E. Horvath for technical assistance; S.A. Rosenberg and J.R. Wunderlich for samples from patients with melanoma; M. Roederer and K. Foulds for reagents and flow cytometry support; A. Oxenius, R. Spörri and N. Joller for providing access to their flow cytometry facility; A. Pegu, R. Roychoudhuri and C. Cheng for discussions and advice on human DC cultures; D. von Laer (Georg-Speyer-Haus) for plasmid M369 and GP-expressing 293T cells; H. Shen (University of Pennsylvania School of Medicine) for rLM-OVA; M. Groettrup (University of Constance) for VACC-OVA, originally generated by J. Yewdell (National Institute of Allergy and Infectious Diseases); and R. Schirmbeck (University of Ulm) for StT-OVA-G cDNA. L.F. was supported by a fellowship of the Schweizerische Stiftung für medizinisch-biologische Stipendien. A.N.H. is a fellow of GRAKO1121 of the German Research Foundation. M.L. is a Lichtenberg fellow funded by the Volkswagen Foundation. A.B. was supported by a PhD scholarship of the Boehringer Ingelheim Fonds and by a post-doctoral fellowship of the Roche Research Foundation. D.D.P. holds a stipendiary professorship of the Swiss National Science Foundation (PP00A-114913) and was supported by grant 3100A0-104067/1 of the Swiss National Science Foundation.
Footnotes
Supplementary information is available on the Nature Medicine website.
AUTHOR CONTRIBUTIONS
L.F., A.N.H., A.B., A.V., C.C., M.F., L.G., S.J., F.K. and D.D.P. performed experiments; L.F., A.N.H., A.B., A.V., C.C., L.G., P.-H.L., C.-A.S., N.P.R., M.L., A.F.O., G.J.N. and D.D.P. designed experiments; S.K., M.v.d.B., A.R. and F.L. contributed reagents; and L.F., G.J.N. and D.D.P. wrote the manuscript.
COMPETING INTERESTS STATEMENT
The authors declare competing financial interests: details accompany the full-text HTML version of the paper at http://www.nature.com/naturemedicine/.
Reprints and permissions information is available online at http://npg.nature.com/reprintsandpermissions/.
References
- 1.Harari A, et al. An HIV-1 clade C DNA prime, NYVAC boost vaccine regimen induces reliable, polyfunctional, and long-lasting T cell responses. J Exp Med. 2008;205:63–77. doi: 10.1084/jem.20071331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peters BS, et al. Studies of a prophylactic HIV-1 vaccine candidate based on modified vaccinia virus Ankara (MVA) with and without DNA priming: effects of dosage and route on safety and immunogenicity. Vaccine. 2007;25:2120–2127. doi: 10.1016/j.vaccine.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Darrah PA, et al. Multifunctional TH1 cells define a correlate of vaccine-mediated protection against Leishmania major. Nat Med. 2007;13:843–850. doi: 10.1038/nm1592. [DOI] [PubMed] [Google Scholar]
- 4.Kostense S, et al. Adenovirus types 5 and 35 seroprevalence in AIDS risk groups supports type 35 as a vaccine vector. AIDS. 2004;18:1213–1216. doi: 10.1097/00002030-200405210-00019. [DOI] [PubMed] [Google Scholar]
- 5.Roberts DM, et al. Hexon-chimaeric adenovirus serotype 5 vectors circumvent pre-existing anti-vector immunity. Nature. 2006;441:239–243. doi: 10.1038/nature04721. [DOI] [PubMed] [Google Scholar]
- 6.Buchmeier MJ, Bowen MD, Peters CJ. Arenaviridae: The viruses and their replication. In: Knipe DM, Howley PM, editors. Fields Virology. Lippincott Williams & Wilkins; Philadelphia, Pennsylvania: 2001. pp. 1635–1668. [Google Scholar]
- 7.Homann D, Teyton L, Oldstone MB. Differential regulation of antiviral T-cell immunity results in stable CD8+ but declining CD4+ T-cell memory. Nat Med. 2001;7:913–919. doi: 10.1038/90950. [DOI] [PubMed] [Google Scholar]
- 8.Pinschewer DD, et al. Kinetics of protective antibodies are determined by the viral surface antigen. J Clin Invest. 2004;114:988–993. doi: 10.1172/JCI22374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinschewer DD, Perez M, Sanchez AB, de la Torre JC. Recombinant lymphocytic choriomeningitis virus expressing vesicular stomatitis virus glycoprotein. Proc Natl Acad Sci USA. 2003;100:7895–7900. doi: 10.1073/pnas.1332709100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flatz L, Bergthaler A, de la Torre JC, Pinschewer DD. Recovery of an arenavirus entirely from RNA polymerase I/II-driven cDNA. Proc Natl Acad Sci USA. 2006;103:4663–4668. doi: 10.1073/pnas.0600652103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ciurea A, et al. Persistence of lymphocytic choriomeningitis virus at very low levels in immune mice. Proc Natl Acad Sci USA. 1999;96:11964–11969. doi: 10.1073/pnas.96.21.11964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krebs P, Scandella E, Odermatt B, Ludewig B. Rapid functional exhaustion and deletion of CTL following immunization with recombinant adenovirus. J Immunol. 2005;174:4559–4566. doi: 10.4049/jimmunol.174.8.4559. [DOI] [PubMed] [Google Scholar]
- 13.Lohning M, et al. Long-lived virus-reactive memory T cells generated from purified cytokine-secreting T helper type 1 and type 2 effectors. J Exp Med. 2008;205:53–61. doi: 10.1084/jem.20071855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steinhoff U, et al. Antiviral protection by vesicular stomatitis virus-specific antibodies in alpha/beta interferon receptor-deficient mice. J Virol. 1995;69:2153–2158. doi: 10.1128/jvi.69.4.2153-2158.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pope C, et al. Organ-specific regulation of the CD8 T cell response to Listeria monocytogenes infection. J Immunol. 2001;166:3402–3409. doi: 10.4049/jimmunol.166.5.3402. [DOI] [PubMed] [Google Scholar]
- 16.Jensen ER, Shen H, Wettstein FO, Ahmed R, Miller JF. Recombinant Listeria monocytogenes as a live vaccine vehicle and a probe for studying cell-mediated immunity. Immunol Rev. 1997;158:147–157. doi: 10.1111/j.1600-065x.1997.tb01001.x. [DOI] [PubMed] [Google Scholar]
- 17.Kurts C, et al. CD8 T cell ignorance or tolerance to islet antigens depends on antigen dose. Proc Natl Acad Sci USA. 1999;96:12703–12707. doi: 10.1073/pnas.96.22.12703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hogquist KA, et al. T cell receptor antagonist peptides induce positive selection. Cell. 1994;76:17–27. doi: 10.1016/0092-8674(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 19.Prevost-Blondel A, et al. Tumor-infiltrating lymphocytes exhibiting high ex vivo cytolytic activity fail to prevent murine melanoma tumor growth in vivo. J Immunol. 1998;161:2187–2194. [PubMed] [Google Scholar]
- 20.Steinman RM. Dendritic cells: versatile controllers of the immune system. Nat Med. 2007;13:1155–1159. doi: 10.1038/nm1643. [DOI] [PubMed] [Google Scholar]
- 21.Probst HC, Lagnel J, Kollias G, van den Broek M. Inducible transgenic mice reveal resting dendritic cells as potent inducers of CD8+ T cell tolerance. Immunity. 2003;18:713–720. doi: 10.1016/s1074-7613(03)00120-1. [DOI] [PubMed] [Google Scholar]
- 22.Sevilla N, et al. Immunosuppression and resultant viral persistence by specific viral targeting of dendritic cells. J Exp Med. 2000;192:1249–1260. doi: 10.1084/jem.192.9.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novak A, Guo C, Yang W, Nagy A, Lobe CG. Z/EG, a double reporter mouse line that expresses enhanced green fluorescent protein upon Cre-mediated excision. Genesis. 2000;28:147–155. [PubMed] [Google Scholar]
- 24.Seiler P, et al. Induction of protective cytotoxic T cell responses in the presence of high titers of virus-neutralizing antibodies: implications for passive and active immunization. J Exp Med. 1998;187:649–654. doi: 10.1084/jem.187.4.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Lamballerie X, Fulhorst CF, Charrel RN. Prevalence of antibodies to lymphocytic choriomeningitis virus in blood donors in southeastern France. Transfusion. 2007;47:172–173. doi: 10.1111/j.1537-2995.2007.01081.x. [DOI] [PubMed] [Google Scholar]
- 26.Lledo L, Gegundez MI, Saz JV, Bahamontes N, Beltran M. Lymphocytic choriomeningitis virus infection in a province of Spain: analysis of sera from the general population and wild rodents. J Med Virol. 2003;70:273–275. doi: 10.1002/jmv.10389. [DOI] [PubMed] [Google Scholar]
- 27.Elbers AR, et al. Low prevalence of antibodies against the zoonotic agents Brucella abortus, Leptospira spp. Streptococcus suis serotype II, hantavirus, and lymphocytic choriomeningitis virus among veterinarians and pig farmers in the southern part of The Netherlands. Vet Q. 1999;21:50–54. doi: 10.1080/01652176.1999.9694991. [DOI] [PubMed] [Google Scholar]
- 28.Stephensen CB, et al. Prevalence of serum antibodies against lymphocytic choriomeningitis virus in selected populations from two U.S. cities. J Med Virol. 1992;38:27–31. doi: 10.1002/jmv.1890380107. [DOI] [PubMed] [Google Scholar]
- 29.Fischer SA, et al. Transmission of lymphocytic choriomeningitis virus by organ transplantation. N Engl J Med. 2006;354:2235–2249. doi: 10.1056/NEJMoa053240. [DOI] [PubMed] [Google Scholar]
- 30.Seaman MS, et al. Multiclade human immunodeficiency virus type 1 envelope immunogens elicit broad cellular and humoral immunity in rhesus monkeys. J Virol. 2005;79:2956–2963. doi: 10.1128/JVI.79.5.2956-2963.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.