Abstract
This study was conducted to evaluate the association of single serum total cholesterol (TC) measurement with cardiovascular diseases (CVD) deaths in Korean adults. The study subjects were taken from the multi-site collaborative dynamic prospective cohort for epidemiologic investigation on cancer risk in residents nearby nuclear power plants in Korea. A total of 12,740 adults aged 40 to 69 yr who underwent a mass screening examination were followed up from 1993 to 2008. Occurring CVD deaths were confirmed by the death certificates in the National Statistical Office, Korea. Groups with the lowest group having TC < 160 mg/dL as well as the highest group having >= 240 mg/dL were associated with higher CVD mortality in Cox proportional hazards analysis adjusting for age, sex, smoking and drinking status, body mass index, level of blood pressure, triglyceride and high density lipoprotein cholesterol. The distribution of adjusted hazard ratios showed the U-shaped curve. Based on the results of this study, caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk in Korean adults.
Keywords: Cholesterol, Cardiovascular Diseases, Mortality, Stroke, Cohort Studies
INTRODUCTION
Cardiovascular diseases (CVD) are the world's largest killers, claiming 17.1 million lives a year (1). As a paradigm shift was needed into the management of comprehensive CVD risk, WHO (2) has recommended total cholesterol (TC) as the only lipid parameter for CVD risk assessment of individuals detected to have hypertension, diabetes or smoking behavior in low and medium resource settings where it is both time-consuming and costly to measure TC, TG, LDL-C and HDL-C altogether. A single measurement of TC in middle aged retains its information in being associated with coronary heart disease (CHD) events and predicts them with similar or only slightly decreasing, strength for a long period of time (3, 4), it is confirmed that the magnitude of multivariate coefficients for serum cholesterol in predicting coronary events is similar across different populations, characterized by different cholesterol levels and different death rates from CHD (5). Thus, reducing high blood cholesterol, a risk factor for CVD events in people with and without a past history of CHD is an important goal of pharmacotherapy (6).
However, the relation of cholesterol to total mortality and non-CVD mortality varied by country and gender in contrast to CHD mortality (7). The shape of the relationship between total cholesterol and non-CHD mortality has been inconsistent (8). In addition, a Japanese study concluded that high cholesterol was not a risk factor for CVD mortality while low cholesterol was related to high mortality (9). The purpose was to study the association of a single serum cholesterol measurement with CVD deaths in Korean adults by a prospective cohort study.
MATERIALS AND METHODS
Cohort construction
The study participants were taken from the cohort for epidemiologic investigation on cancer risk in residents nearby nuclear power plants in Korea (10). Subjects were residents in Youngkwang, Wolsung, Kori, Uljin, Chungju, Yangpyong, and Haman County. This multi-sites collaborative dynamic prospective cohort was constructed between 1992 and 2005 with a total follow-up of 303,542 person-years in 36,176 subjects. Because nuclear power plants in Korea were mainly located in countryside, the enrollee of this cohort was represented in a population of rural district rather than of urban. All subjects provided written informed consent. And this study has approved by the institutional review board of Seoul National University College of Medicine (IRB No. C-0611-012-188).
The three exclusion criteria from the cohort were applied to construct the study participants: first, members without measurement of total cholesterol (TC) levels (n = 16,330); second, members aged under 40- or over 70 yr old (n = 5,718); last, members having previous history of cardiovascular diseases on entry (n = 1,388). Finally 12,740 subjects were selected as the study subjects.
Baseline demographic and clinical data were obtained from interviewer-administrated questionnaires. Weight and height were measured in wearing light clothing. Subjects were seated for blood-pressure measurement. Non-fasting blood specimens were drawn in order to determine total cholesterol (TC), triglyceride (TG), and high-density lipoprotein (HDL) cholesterol. Quality-control procedures were achieved in agreement with the Korean Association of Laboratory Quality Control.
Follow-up and Outcome Ascertainment
Deaths among study participants through December 31, 2008, were confirmed by linking the information to the death certificates in the Statistics Korea (11). The death from cardiovascular diseases was confirmed from abstractors' coded causes of death by the 'I00' to 'I69' in Korea Standard Classification of Cause of Death (KCD), 6th Revision (12). To conduct the subgroup analysis, deaths from heart diseases and stroke were defined by a combination of KCD codes 'I00' to 'I52', and 'I60' to 'I69', respectively.
Total person-years were calculated by determining the number of days from the entry, until the date of death from CVD, or the end of follow-up, 31 December 2008, after which the number of days was converted into years.
Data analysis
Subjects were divided into 4 groups based on the cutoff value of 160, 200, 240 mg/dL in TC level. The cutoff value of TC used was selected on the basis of past research (9) for comparing results, while the cut-points of TG and HDL were obtained from 25th, 50th, and 75th percentile in distribution. The second lowest group (160-199 mg/dL) in TC and TG was used as the reference group.
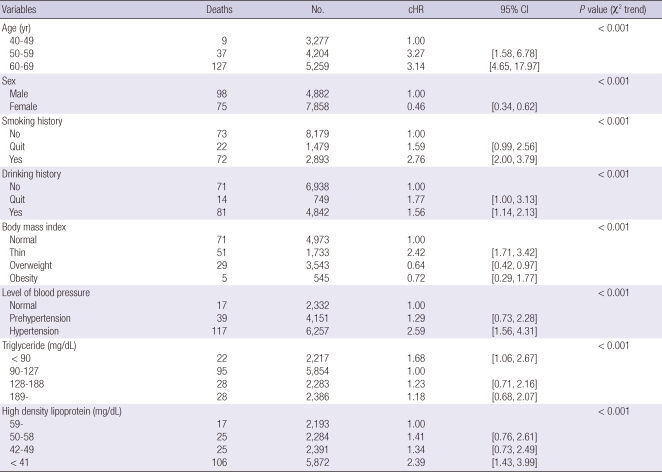
A potential confounder among the variables of the baseline information was defined as a variable showing a statistical significance based on the crude hazard ratios (cHR) of deaths from CVD. By this definition, the following eight potential confounders were chosen: age, sex, current smoking/drinking habit on entry, body mass index and distribution of blood pressure, as well as level of TG and HDL cholesterol (Table 1). Because TG and HDL cholesterol are highly correlated to TC, another model excluding TG and HDL was applied in multivariable analysis for considering over-adjustment.
Table 1.
The crude hazard ratio (cHR) with 95% confidence intervals (CIs) of baseline characteristics in death by cardiovascular diseases in the study participants (n = 12,740)*
*Excluding missing values.
Age at entry was categorized into 10-yr groups of 40-49, 50-59, and 60-69 yr old. The other confounding factors were categorized such as current smoking/drinking habit on entry (no/quit/yes), body mass index (BMI; thin, normal, overweight, and obesity) and distribution of blood pressure (normal, pre-hypertension, and hypertension). The BMI was categorized as less than 20.0, 20.0 to 24.9, 25.0 to 29.9, and 30.0 or more. The blood pressure was grouped by the classification in the seventh report of the Joint National Committee, 2003 (13).
To control the confounders, Cox's proportional-hazards regression was used to evaluate the association between the baseline cholesterol and death from CVD. Confidence intervals were obtained by the Wald method and all reported P values are two sided. The chi-square test for trend was used to evaluate linear trends. Analyses were conducted using SAS version 9 (14).
RESULTS
Baseline characteristics are presented in Table 1. In total 12,740 study participants, the average of age and BMI are 56.2 yr-old and 24.2 (kg/m2) for both sexes, respectively (SD 8.38 in age, 18.49 in BMI). During a follow-up of totally 73,064,487 person-years, 98 men and 75 women died from CVD. Smoking history, drinking history, high blood pressure, and HDL cholesterol have a linear trend with statistical significance. BMI and TC cholesterol show the U-shaped curve in the risk of death from CVD (Table 1).
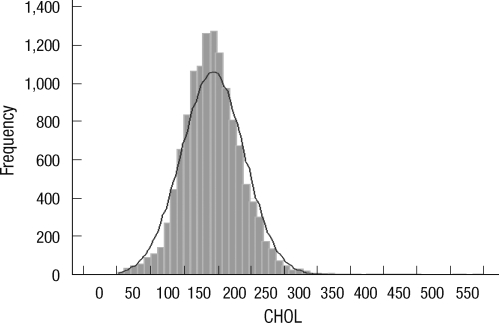
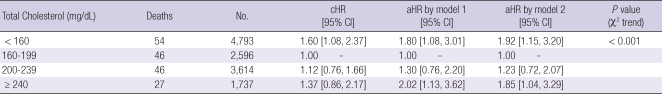
Fig. 1 displays the distribution of TC with 194 mg/dL in mean and 47.2 in SD. Table 2 indicates that the lowest group having TC < 160 mg/dL as well as the highest group having > = 240 mg/dL are associated with higher CVD mortality in Cox proportional hazards analysis adjusting for age, sex, smoking and drinking status, body mass index, level of blood pressure, TG and HDL cholesterol. Even if excluding TG and HDL cholesterol for considering over-adjustment (model 2 in Table 2), the trends as well as statistical significances were sustained.
Fig. 1.
Distribution of total cholesterol levels in study participants.
Table 2.
The crude and adjusted hazard ratios (cHR, aHR) with 95% confidence intervals (CIs) of total cholesterol in death by cardiovascular diseases in the study participants (n = 12,740)
*model 1 (adjusted for age, sex, smoking and drinking history, body mass index, level of blood pressure, triglyceride, high density lipoprotein) and model 2 (adjusted for age, sex, smoking and drinking history, body mass index, and level of blood pressure).
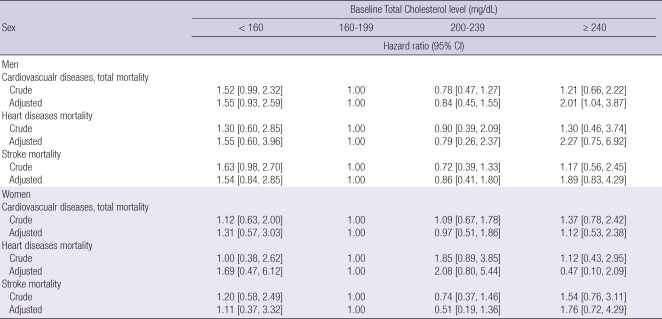
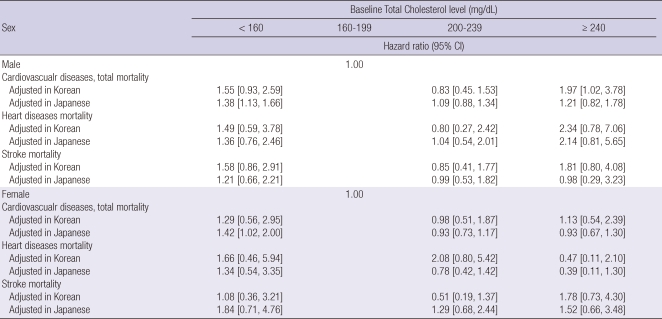
Table 3 shows HRs and 95% CIs for CVD mortality by cholesterol category. The crude and multivariate-adjusted HRs are grouped by sex. While the distribution of adjusted HRs shows the U-shaped curve, the adjusted HRs of the lowest cholesterol group (< 160 mg/mL) in a risk of CVD death are 1.55 (95% CI, 0.93-2.59) for men and 1.31 (0.57-3.03) for women. In the highest cholesterol group (≥ 240 mg/dL), the adjusted HR in men only has the statistical significance (aHR 2.01, 95% CI 1.04-3.87). When a subgroup analysis in mortality from heart disease and stroke has conducted, all adjusted HRs by cholesterol groups and both sexes do not show a statistical significance, in spite of keeping the U-shaped distribution.
Table 3.
The crude and adjusted* hazard ratios (cHR, aHR) of total cholesterol level in the cardiovascualr mortalities by sex
*adjusted for age, smoking and drinking history, body mass index, level of blood pressure, high density lipoprotein cholesterol, and triglyceride.
DISCUSSION
CVD encompasses a wide range of disease including ischemic heart disease, coronary heart disease (e.g. heart attack), cerebrovascular disease (e.g. stroke), raised blood pressure, hypertension, rheumatic heart disease and heart failure (6). As CVD is ranked as the number one cause of mortality and is a major cause of morbidity world wide (1), CVD imposes high social costs, including impaired quality of life and reduced economic activity, and accounts for a large share of health service resources (15).
In the general population, the relationship between hyperlipidemia (dyslipidemia) and CVD (predominantly CAD) is well established (16) and there are proven benefits of lipid-lowering with statins (6). While this study has several strengths, including a prospective design, large sample size, prolonged duration of follow-up, a large number of deaths, and actually complete mortality follow-up, the distribution of multivariable-adjusted HRs shows the U-shaped curve in Korean adults. Especially, the fact that low cholesterol was related to high mortality of CVD is as same as that of a Japanese study (9) in Table 4.
Table 4.
Comparison of adjusted* hazard ratios (aRR) of total cholesterol level in the cardiovascualr mortalities by sex between Korean and Japanese people [Ref: 9]
*adjusted for age, smoking and drinking history, body mass index, level of blood pressure, and high density lipoprotein cholesterol.
Similar inverse, 'J' or 'U'-shaped relationships between lipid levels and all cause mortality have been reported in other populations and are thought to reflect a high prevalence of co-morbid disease in patients with low cholesterol levels (16, 17). In the Honolulu Heart Study of Japanese-Americans (18), low serum cholesterol was associated with increased mortality, but only among individuals with the risk factors of smoking, high alcohol consumption, and untreated hypertension. In other words, the association is not invariant, but appears to vary across populations of different social or lifestyle characteristics (7).
Although the increase in mortality at low levels of TC was explained by chance, regression dilution bias, competing risks, cause-effect, effect-cause, and residual confounding such as smoking (17), the terms of 'reverse epidemiology' and 'obesity paradox' (19, 20) in marked contrast to the effects of TC or obesity on mortality in the general population, especially the Framingham paradigm (21), have been proposed. Associations compatible with the concept of "reverse epidemiology" have been described in several other chronic conditions such as end-stage renal disease, malignancies, chronic obstructive lung disease, AIDS as well as in the elderly (22). As same as the results of this study, Casiglia et al. (23) reported that the higher the TC levels, the lower mortality in the elderly. In addition, Strandberg et al. (24) suggested that low serum cholesterol level in midlife predicted not only better survival but also better physical function and quality of life (QOL) in old age.
Interestingly, Table 3 showed that the adjusted HR of heart disease mortality was in the opposite direction between men and women, especially in TC over 240 mg/dL (2.27 in men vs 0.47 in women). Japanese in the same level of TC in Table 4 also showed the same fact (2.14 in men vs 0.39 in women). While the CVD mortality in men are generally higher than in women, further studies for explaining this phenomenon will be needed.
The fact that only the multivariable-adjusted HR in men has the statistical significance should be interpreted carefully because this study has a number of limitations. First limitation is that results were based on a one-time measurement of serum lipids. In longitudinal studies the use of baseline measurements only may underestimate the associations between usual risk factors and CVD mortality due to regression dilution effects (25). Second limitation is that TC levels in this study were measured in the non-fasting state. Although similar results were obtained when analyses were repeated with non-fasting serum (26), subjects would be grouped into higher TC level. Based on this fact, calculated HRs would be assumed as under-estimated with toward the null. Third limitation is the issue of reverse-causality because some underlying diseases could influence the level of lipid. To controlling this bias, authors applied to exclude members having previous history of cardiovascular disease on entry. Last limitation is that the "healthy peopler" would have a higher chance to register as a cohort participant in general population (27). The effect on mortality might have been slightly underestimated by the increased level of TC during follow-up.
CVD is multi-factorial in its causation and lifestyle changes are the basis of any treatment strategy, with patients often requiring behavioral counseling (6). Considering reductions in CVD mortality with statins, there have still been controversies regarding the truly long-term prognostic value of low cholesterol on CVD mortality, especially in older individuals (5, 28). Based on the results of this study, caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk.
ACKNOWLEDGMENTS
The authors thank the investigators of the report titled as "Epidemiological Investigation on Cancer Risk among Radiation Workers in Nuclear Power Plants and Residents nearby Nuclear Power Plants in Korea"
Footnotes
This study was funded by a grant from Ministry of Education, Science and Technology (MEST No. 2010-0000986), Republic of Korea.
References
- 1.Cardiovascular disease. WHO. [accessed on 31 July 2011]. Available at http://www.who.int/cardiovascular_diseases/en/
- 2.Integrated management of cardiovascular risk. WHO. [accessed on 31 July 2011]. Available at http://www.who.int/cardiovascular_diseases/media/en/635.pdf.
- 3.Menotti A, Lanti M. Coronary risk factors predicting early and late coronary deaths. Heart. 2003;89:19–24. doi: 10.1136/heart.89.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menotti A, Giampaoli S. A single risk factor measurement predicts 35-year mortality from cardiovascular disease. G Ital Cardiol. 1998;28:1354–1362. [PubMed] [Google Scholar]
- 5.Menotti A, Lanti M, Kromhout D, Kafatos A, Nedeljkovic S, Nissinen A. Short and long term association of a single serum cholesterol measurement in middle-aged men in prediction of fatal coronary and other cardiovascular events: a cross-cultural comparison through Europe. Eur J Epidemiol. 2005;20:597–604. doi: 10.1007/s10654-005-7918-8. [DOI] [PubMed] [Google Scholar]
- 6.Taylor F, Ward K, Moore TH, Burke M, Davey Smith G, Casas JP, Ebrahim S. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;(1):CD004816. doi: 10.1002/14651858.CD004816.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai J, Pajak A, Li Y, Shestov D, Davis CE, Rywik S, Li Y, Deev A, Tyroler HA. Total cholesterol and mortality in China, Poland, Russia, and the US. Ann Epidemiol. 2004;14:399–408. doi: 10.1016/j.annepidem.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Simes RJ. Low cholesterol and risk of non-coronary mortality. Aust N Z J Med. 1994;24:113–119. doi: 10.1111/j.1445-5994.1994.tb04446.x. [DOI] [PubMed] [Google Scholar]
- 9.Nago N, Ishikawa S, Goto T, Kayaba K. Low cholesterol is associated with mortality from stroke, heart disease, and cancer: the Jichi Medical School Cohort Study. J Epidemiol. 2011;21:67–74. doi: 10.2188/jea.JE20100065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahn YO, Lee MC, Yoo KY, Chung JK, Park BJ, Li ZM, Choi JS, Lee CE, Lee DH, Lim HS, Choi BY, Chang SH, Oh JK, Cha CY, Chung HW. Epidemiological Investigation on Cancer Risk among Radiation Workers in Nuclear Power Plants and Residents nearby Nuclear Power Plants in Korea. 2007.3-2011.2. Ministry of Education, Science and Technology (MEST No. 2010-0000986) [Google Scholar]
- 11.Korean Statistical Information Service. The Statistics Korea. [accessed on 31 July 2011]. Available at http://www.kosis.kr/
- 12.Korea Standard Classification of Cause of Death. The Statistics Korea. [accessed on 31 July 2011]. Available at http://www.kostat.go.kr/portal/english/news/1/8/index.board?bmode=read&aSeq=67396.
- 13.The Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) National Heart Lung and Blood Institute. [accessed on 31 July 2011]. Available at http://www.nhlbi.nih.gov/guidelines/hypertension/jnc8/index.htm. [PubMed]
- 14.SAS software. [accessed on 31 July 2011]. Available at http://www.sas.com/
- 15.Gaziano TA. Reducing the growing burden of cardiovascular disease in the developing world. Health Aff (Millwood) 2007;26:13–24. doi: 10.1377/hlthaff.26.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wan RK, Mark PB, Jardine AG. The cholesterol paradox is flawed: cholesterol must be lowered in dialysis patients. Semin Dial. 2007;20:504–509. doi: 10.1111/j.1525-139X.2007.00359.x. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs D, Blackburn H, Higgins M, Reed D, Iso H, McMillan G, Neaton J, Nelson J, Potter J, Rifkind B. Report of the Conference on Low Blood Cholesterol: Mortality Associations. Circulation. 1992;86:1046–1060. doi: 10.1161/01.cir.86.3.1046. [DOI] [PubMed] [Google Scholar]
- 18.Iribarren C, Reed DM, Burchfiel CM, Dwyer JH. Serum total cholesterol and mortality. Confounding factors and risk modification in Japanese-American men. JAMA. 1995;273:1926–1932. [PubMed] [Google Scholar]
- 19.Speakman JR, Westerterp KR. Reverse epidemiology, obesity and mortality in chronic kidney disease: modelling mortality expectations using energetics. Blood Purif. 2010;29:150–157. doi: 10.1159/000245642. [DOI] [PubMed] [Google Scholar]
- 20.Arena R, Lavie CJ. The obesity paradox and outcome in heart failure: is excess bodyweight truly protective? Future Cardiol. 2010;6:1–6. doi: 10.2217/fca.09.158. [DOI] [PubMed] [Google Scholar]
- 21.Kalantar-Zadeh K. What is so bad about reverse epidemiology anyway? Semin Dial. 2007;20:593–601. doi: 10.1111/j.1525-139X.2007.00360.x. [DOI] [PubMed] [Google Scholar]
- 22.Güder G, Frantz S, Bauersachs J, Allolio B, Wanner C, Koller MT, Ertl G, Angermann CE, Störk S. Reverse epidemiology in systolic and nonsystolic heart failure: cumulative prognostic benefit of classical cardiovascular risk factors. Circ Heart Fail. 2009;2:563–571. doi: 10.1161/CIRCHEARTFAILURE.108.825059. [DOI] [PubMed] [Google Scholar]
- 23.Casiglia E, Mazza A, Tikhonoff V, Scarpa R, Schiavon L, Pessina AC. Total cholesterol and mortality in the elderly. J Intern Med. 2003;254:353–362. doi: 10.1046/j.1365-2796.2003.01200.x. [DOI] [PubMed] [Google Scholar]
- 24.Strandberg TE, Strandberg A, Rantanen K, Salomaa VV, Pitkälä K, Miettinen TA. Low cholesterol, mortality, and quality of life in old age during a 39-year follow-up. J Am Coll Cardiol. 2004;44:1002–1008. doi: 10.1016/j.jacc.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 25.Clarke R, Lewington S, Youngman L, Sherliker P, Peto R, Collins R. Underestimation of the importance of blood pressure and cholesterol for coronary heart disease mortality in old age. Eur Heart J. 2002;23:286–293. doi: 10.1053/euhj.2001.2781. [DOI] [PubMed] [Google Scholar]
- 26.Liu Y, Coresh J, Eustace JA, Longenecker JC, Jaar B, Fink NE, Tracy RP, Powe NR, Klag MJ. Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA. 2004;291:451–459. doi: 10.1001/jama.291.4.451. [DOI] [PubMed] [Google Scholar]
- 27.Clarke R, Emberson J, Fletcher A, Breeze E, Marmot M, Shipley MJ. Life expectancy in relation to cardiovascular risk factors: 38 year follow-up of 19,000 men in the Whitehall study. BMJ. 2009;339:b3513. doi: 10.1136/bmj.b3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manolio TA, Pearson TA, Wenger NK, Barrett-Connor E, Payne GH, Harlan WR. Cholesterol and heart disease in older persons and women. Review of an NHLBI workshop. Ann Epidemiol. 1992;2:161–176. doi: 10.1016/1047-2797(92)90051-q. [DOI] [PubMed] [Google Scholar]